Impact of an Intervention with Wii Video Games on the Autonomy of Activities of Daily Living and Psychological–Cognitive Components in the Institutionalized Elderly
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design: Participants
2.2. Procedure: Data Collection
2.3. Main Outcomes: Instruments
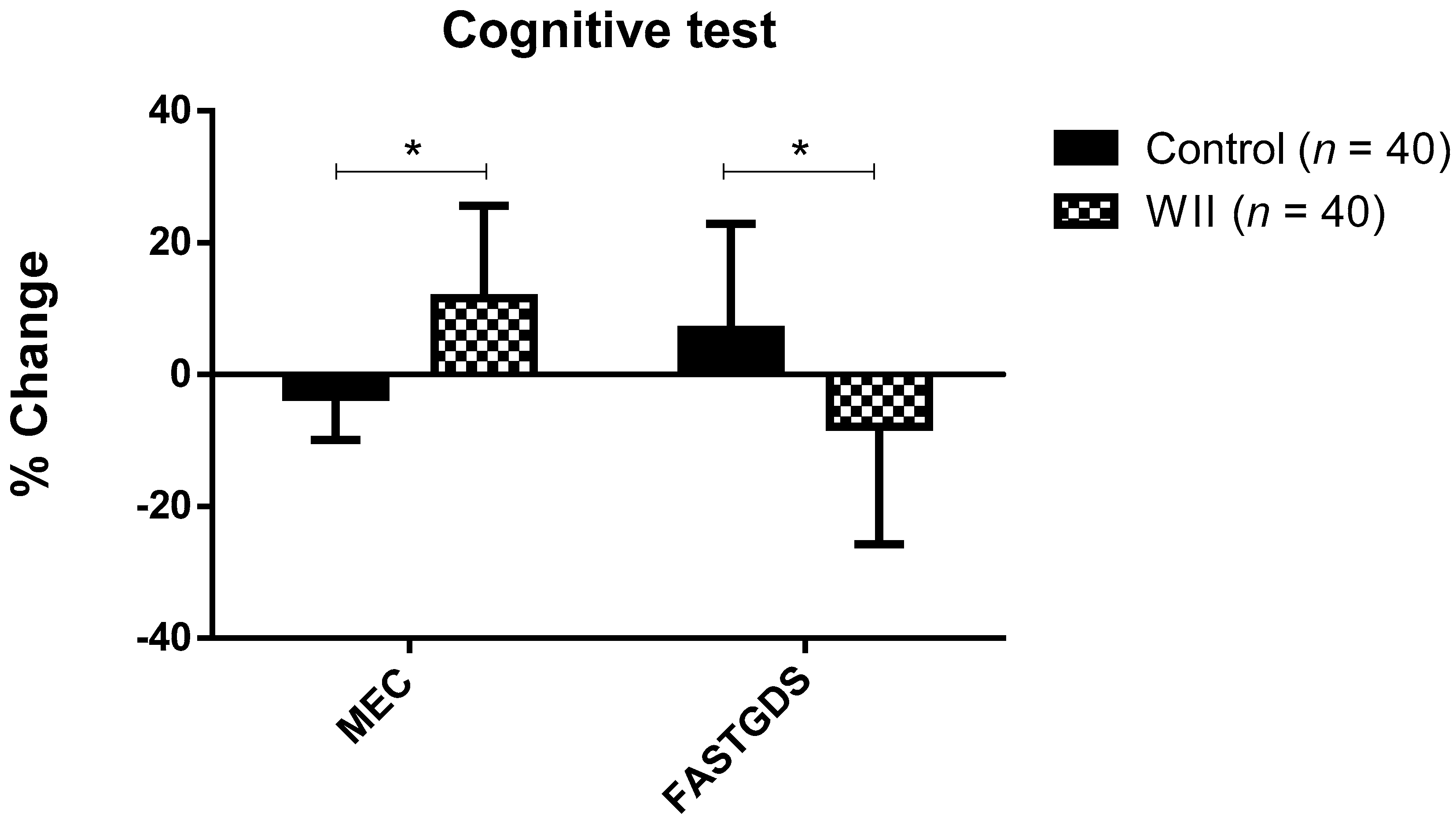
- Cognitive assessment: the cognitive status of the participants was evaluated using the MCE. This is an adapted and validated version for the Spanish population of the “Mini-Mental State Examination” [27]. In this study, the 30-point version was used, instead of the 35-point version, since it has been the most widely used internationally and allows comparisons with other investigations. The test-retest reliability is 0.89, while the inter-rater reliability is 0.82. Through 11 items, this test assesses the essential cognitive functions of the participants: orientation, registration, attention and concentration, fixation and short-term memory, language, calculation, memory, nomination, repetition, compression, reading, writing, and drawing [28]. The score obtained ranges from 1 to 30; values lower than 10 indicate severe cognitive damage, values between 11 and 20 moderate cognitive damage, values between 21 and 26 mild cognitive damage, and values higher than 27 normal cognitive status.The Global Deterioration Scale (GDS) was also used, which allows professionals and caregivers to measure and record the cognitive, behavioral, and functional impairment of patients [29]. This scale classifies deterioration into seven stages, where 1 corresponds to the absence of deterioration and 7 to the most severe deterioration. Stage 4 or mild deterioration is characterized by patients who require help with complex tasks such as managing finances, planning a dinner, and so forth. In stage 5, or moderate deterioration, patients need help to choose adequate clothing. In stage 6, or moderately severe deterioration, patients need help to dress and bathe, and they begin to experience urinary and fecal incontinence. Although the MCE scale is already a sufficient tool, complementing its use with the GDS is useful because this tool provides information on behavioral deterioration and dependent status, and also relates the person’s cognitive status with their score on the MCE. Each stage of the GDS is related to a score of the MCE, so if a person improves or worsens, changes on his score in MCE and GDS stage can reflect this [30].
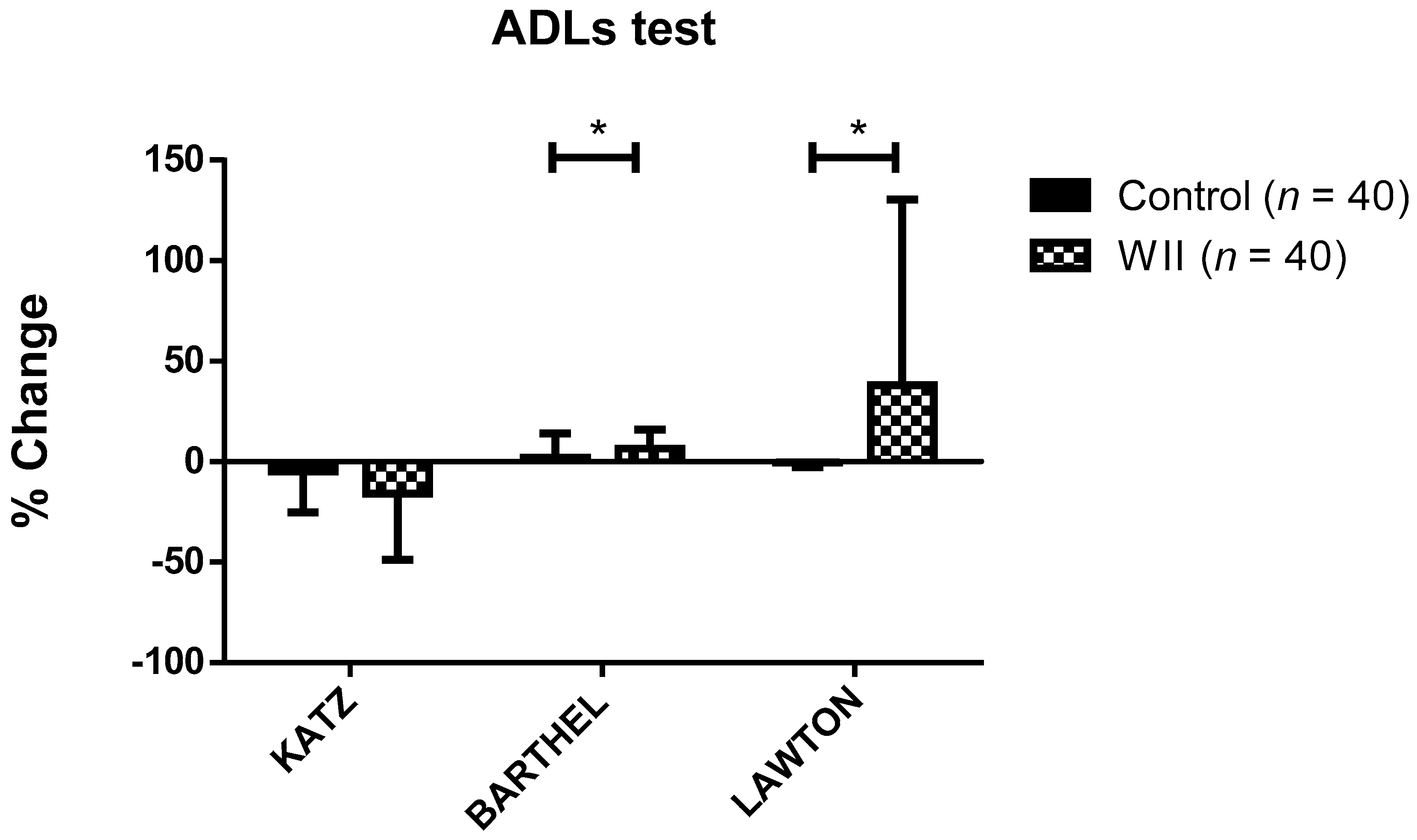
- Functional assessment: to assess the basic ADLs, the Katz Index of Independence in Activities of Daily Living was used [31]. This index assesses six basic functions in terms of dependency or independence: bathing, dressing, toileting, transferring, continence, and feeding. Its assessment is based on the direct observation of the patient by health personnel during their stay in a center, and/or by direct questioning with the patient, caregivers, or a family member by health personnel. The ability to perform each of the tasks is valued at 0, while disability is valued at 1. Therefore, the higher the score, the greater the dependency. It is an effective indicator of active life expectancy, since the higher the score, the lower the active life expectancy. It is an indicator poorly sensitive to small changes in ADL performance [32].To complement the assessment of basic ADLs, the Barthel Index [33] was also used. Both scales were included in the research to determine the AVDS of a patient because, while the Katz scale measures rapid changes (acute context), the Barthel scale is more conducive to the long-term assessment [34]. This index assesses the level of independence of the patient in some basic ADLs, such as feeding, bathing, grooming, dressing, bowel control, bladder control, toilet use, transferring (bed to chair and back), and mobility on level surfaces or stairs. The evaluator assigns different scores and weights according to the patient’s ability to perform the different activities. The score obtained ranges from 1 to 100, with intervals of 5 points; values closer to 0 indicate higher levels of dependency, and values closer to 100 more independence [33,35].The evaluation was carried out by an occupational therapist, accompanied by the auxiliary reference staff and the residential center occupational therapist. In this case, there was no interview with any family members, since the information from two different professionals was sufficient and included the nursing assistant who assists users in ADLs, and the occupational therapist who oversees evaluation and stimulation of the AVDs of the users.The ability to carry out instrumental ADLs was assessed using the Lawton and Brody index [36]. This index assesses eight instrumental activities, such as the ability to use a telephone, shopping, food preparation, housekeeping, laundry, mode of transportation, responsibility for own medications, and ability to handle finances. Those people with an inability to perform one or more activities are considered dependent to different degrees. Each area is scored according to the description that best corresponds with it, assigning a maximum of 1 point and a minimum of 0 points. The maximum dependence would be reflected by a score of 0 points, while a score of 8 points would express the total independence of the patient.
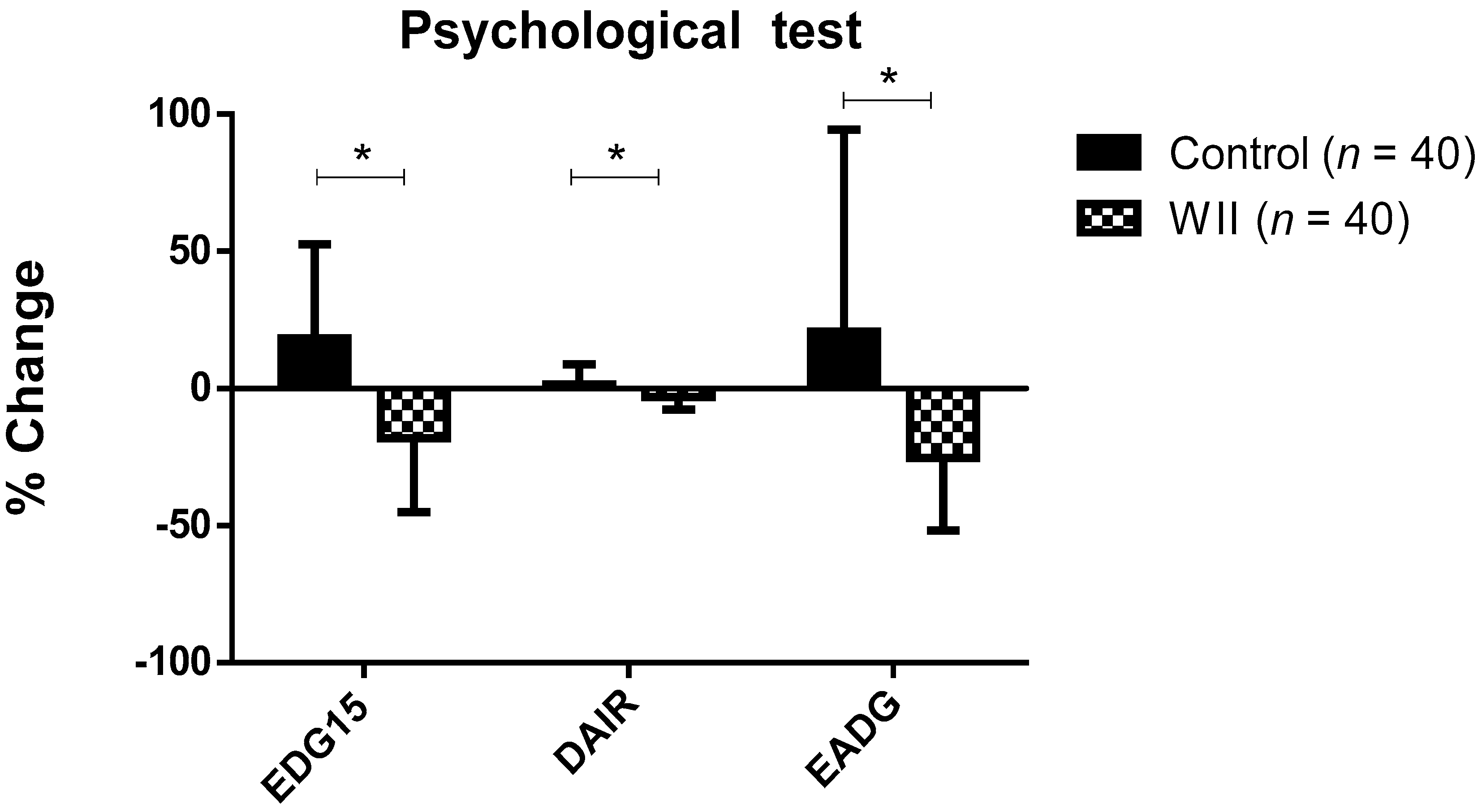
- Psychological evaluation: the Dementia Apathy Interview and Rating (DAIR) was used to assess the level of apathy of the participants. This questionnaire, which includes 14 items, was administered to a knowledgeable caregiver who had to indicate how often the patient had suffered the content of the sentence over the past month, using a four point scales: 0—no or almost never; 1—sometimes; 2—very often; 3—yes or almost always. The total score is obtained by adding the score obtained in each of the completed items and dividing it by the number of completed items. Higher scores on this scale represent greater severity of apathy. The DAIR is a reliable assessment with high internal consistency (α = 0.89) [37].The Yesavage scale for Geriatric Depression (EGD-15) was used to assess the presence of depressive symptoms [38,39]. This scale explores only the cognitive symptoms of a major depressive episode, with a dichotomous response pattern to facilitate the responses of the person evaluated. There is a short version of 15 items, with an internal consistency that ranges between 0.76 and 0.89. The cut-off points are: 0–5: normal; 6–10: moderate depression; >10: severe depression.
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Bolandzadeh, N.; Kording, K.; Salowitz, N.; Davis, J.C.; Hsu, L.; Chan, A.; Sharma, D.; Blohm, G.; Liu-Ambrose, T. Predicting Cognitive function from clinical measures of physical function and health status in older adults. PLoS ONE 2015, 10, e0119075. [Google Scholar] [CrossRef]
- Razani, J.; Casas, R.; Wong, J.T.; Lu, P.; Alessi, C.; Josephson, K. Relationship between executive functioning and activities of daily living in patients with relatively mild dementia. Appl. Neuropsychol. 2007, 14, 208–214. [Google Scholar] [CrossRef] [PubMed]
- Agüero-Torres, H.; Thomas, V.S.; Winblad, B.; Fratiglioni, L. The impact of somatic and cognitive disorders on the functional status of the elderly. J. Clin. Epidemiol. 2002, 55, 1007–1012. [Google Scholar] [CrossRef]
- Paixão, C.; Reichenheim, M.E. A review of functional status evaluation instruments in the elderly. Cadernos Saude Publica 2005, 21, 7–19. [Google Scholar] [CrossRef][Green Version]
- Sanchez, M.A.S.; Correa, P.C.R.; Lourenço, R.A. Cross-cultural adaptation of the “functional activities questionnaire—FAQ” for use in Brazil. Dement. Neuropsychol. 2011, 5, 322–327. [Google Scholar] [CrossRef] [PubMed]
- Gühne, U.; Angermeyer, M.C.; Riedel-Heller, S. Is mortality increased in mildly cognitively impaired individuals? Dement. Geriatr. Cogn. Disord. 2006, 21, 403–410. [Google Scholar] [CrossRef]
- Black, S.A.; Rush, R.D. Cognitive and functional decline in adults aged 75 and older. J. Am. Geriatr. Soc. 2002, 50, 1978–1986. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, A.; Savill-Smith, C. The Use of Computer and Video Games for Learning: A Review of the Literature, 3rd ed.; Learning and Skills Development Agency: London, UK, 2004; pp. 1–84. [Google Scholar]
- Gee, J.P. Good Video Games Plus Good Learning, 1st ed.; Peter Lang Publishing: New York, NY, USA, 2007; pp. 1–194. [Google Scholar]
- Ben-Sadoun, G.; Sacco, G.; Manera, V.; Bourgeois, J.; König, A.; Foulon, P.; Fosty, B.; Bremond, F.; D’Arripe-Longueville, F.; Robert, P. Physical and Cognitive stimulation using an exergame in subjects with normal aging, mild and moderate cognitive impairment. J. Alzheimer’s Dis. 2016, 53, 1299–1314. [Google Scholar] [CrossRef]
- Eggenberger, P.; Wolf, M.; Schumann, M.; De Bruin, E.D. Exergame and balance training modulate prefrontal brain activity during walking and enhance executive function in older adults. Front. Aging Neurosci. 2016, 8, 66. [Google Scholar] [CrossRef] [PubMed]
- Hill, N.T.; Mowszowski, L.; Naismith, S.L.; Chadwick, V.L.; Valenzuela, M.; Lampit, A. Computerized cognitive training in older adults with mild cognitive impairment or dementia: A systematic review and meta-analysis. Am. J. Psychiatry 2017, 174, 329–340. [Google Scholar] [CrossRef]
- Arvanitakis, Z.; Capuano, A.W.; Leurgans, S.E.; Bennett, D.A.; Schneider, J.A. Relation of cerebral vessel disease to Alzheimer’s disease dementia and cognitive function in elderly people: A cross-sectional study. Lancet Neurol. 2016, 15, 934–943. [Google Scholar] [CrossRef]
- Kim, K.; Choi, B.; Lim, W. The efficacy of virtual reality assisted versus traditional rehabilitation intervention on individuals with functional ankle instability: A pilot randomized controlled trial. Disabil. Rehabil. Assist. Technol. 2018, 14, 276–280. [Google Scholar] [CrossRef] [PubMed]
- Donath, L.; Rössler, R.; Faude, O. Effects of virtual reality training (exergaming) compared to alternative exercise training and passive control on standing balance and functional mobility in healthy community-dwelling seniors: A meta-analytical review. Sports Med. 2016, 46, 1293–1309. [Google Scholar] [CrossRef] [PubMed]
- Şimşek, T.T.; Çekok, K. The effects of Nintendo WiiTM-based balance and upper extremity training on activities of daily living and quality of life in patients with sub-acute stroke: A randomized controlled study. Int. J. Neurosci. 2015, 126, 1061–1070. [Google Scholar] [CrossRef] [PubMed]
- Uysal, S.A.; Baltaci, G. Effects of Nintendo Wii™ training on occupational performance, balance, and daily living activities in children with spastic hemiplegic cerebral palsy: A single-blind and randomized trial. Games Health J. 2016, 5, 311–317. [Google Scholar] [CrossRef]
- Moon, J.; Jung, J.; Cho, H. Effects of balance training using a Wii Fit balance board on balance, gait and activities of daily living in patients with parkinson disease: A pilot randomized controlled trial. Med. Leg Update 2020, 20, 1799–1803. [Google Scholar] [CrossRef]
- Monteiro, R.; Da Silva, L.; De Tarso, P.; Pinheiro, M.; Rodrigues, E.; Mendes, A.; Lage, M.; Engedal, K. Acute effects of exergames on cognitive function of institutionalized older persons: A single-blinded, randomized and controlled pilot study. Aging Clin. Exp. Res. 2017, 387–394. [Google Scholar] [CrossRef]
- Santamaría, K.G.; Fonseca, A.S.; Moncada Jiménez, J.; Solano Mora, L.C. Balance, attention and concentration improvements following an exergame training program in elderly. Retos 2017, 33, 102–105. [Google Scholar] [CrossRef]
- Chesler, J.; McLaren, S.; Klein, B.; Watson, S. The effects of playing Nintendo Wii on depression, sense of belonging and social support in Australian aged care residents: A protocol study of a mixed methods intervention trial. BMC Geriatr. 2015, 15, 106. [Google Scholar] [CrossRef]
- Ritchie, K.; Artero, S.; Touchon, J. Classification criteria for mild cognitive impairment. Neurology 2001, 56, 37–42. [Google Scholar] [CrossRef]
- Millán-Calenti, J.C.; Tubío, J.; Pita-Fernández, S.; González-Abraldes, I.; Lorenzo, T.; Maseda, A. Prevalence of cognitive impairment: Effects of level of education, age, sex and associated factors. Dement. Geriatr. Cogn. Disord. 2009, 28, 455–460. [Google Scholar] [CrossRef]
- Millán-Calenti, J.C.; Tubío, J.; Pita-Fernández, S.; González-Abraldes, I.; Lorenzo, T.; Fernández-Arruty, T.; Maseda, A. Prevalence of functional disability in activities of daily living (ADL), instrumental activities of daily living (IADL) and associated factors, as predictors of morbidity and mortality. Arch. Gerontol. Geriatr. 2010, 50, 306–310. [Google Scholar] [CrossRef]
- Franco, M. Desempeño ocupacional, bienestar psicológico y sentido de la vida en personas institucionalizadas. Estudio preliminar. Rev. Psicol. Salud 2018, 6, 87–123. [Google Scholar] [CrossRef]
- Custodia, N.; Herrera, E.; Lira, D.; Montesinos, R.; Linares, J.; Bendezú, L. Mild cognitive impairment: Where does normal ageing end and where dementia begins? Rev. Fac. Med. 2012, 73, 322–330. [Google Scholar]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatry Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- López, J.; Martí, A. Instituto de Medicina Legal de Cataluña, Mini-examen cognoscitivo (MCE). Rev. Esp. Med. Leg. 2011, 37, 122–127. [Google Scholar]
- Reisberg, B.; Ferris, S.; Franssen, E. An ordinal functional assessment tool for Alzheimer’s-type dementia. Psychiatry Serv. 1985, 36, 593–595. [Google Scholar] [CrossRef] [PubMed]
- Beobide, I.; Ferro, A.; Miró, B.; Martínez, S.; Genua, M.I. The impact of automation on the safety of drug dispensing in nursing homes. Farm. Hosp. 2018, 42, 141–146. [Google Scholar] [CrossRef]
- Katz, S.; Ford, A.B.; Moskowitz, R.W.; Jackson, B.A.; Jaffe, M.W. Studies of illness in the age: The index of adl, a standarized measure of biological and psychosocial function. JAMA 1963, 185, 914–919. [Google Scholar] [CrossRef]
- Silva, G.D.S.F.D.; Bergamaschine, R.; Rosa, M.; Melo, C.; Miranda, R.; Filho, M.B. Avaliação do nível de atividade física de estudantes de graduação das áreas saúde/biológica. Rev. Bras. Med. Esporte 2007, 13, 39–42. [Google Scholar] [CrossRef][Green Version]
- Mahoney, F.I.; Barthel, D.W. Functional evaluation: The Barthel Index. Md. State Med. J. 1965, 14, 61–65. [Google Scholar] [PubMed]
- Hartigan, I. A comparative review of the Katz ADL and the Barthel Index in assessing the activities of daily living of older people. Int. J. Older People Nurs. 2007, 2, 204–212. [Google Scholar] [CrossRef]
- Mahoney, F.I.; Wood, O.H.; Barthel, D.W. Rehabilitation of chronically Ill patients: The Influence of complications on the final Goal. South. Med. J. 1958, 51, 605–609. [Google Scholar] [CrossRef]
- Lawton, M.P.; Brody, E.M. Assessment of older people: Self-maintaining and instrumental activities of daily living. Gerontologist 1969, 9, 179–186. [Google Scholar] [CrossRef] [PubMed]
- Strauss, E.; Sperry, S. An informant-based assessment of apathy in Alzheimer disease. Cogn. Behav. Neurol. 2002, 15, 176–183. [Google Scholar]
- Incalzi, R.A.; Cesari, M.; Pedone, C.; Carbonin, P.U. Construct validity of the 15-Item geriatric depression scale in older medical inpatients. J. Geriatr. Psychiatry Neurol. 2003, 16, 23–28. [Google Scholar] [CrossRef]
- Gómez, C.; Campo, A. Escala de yesavage para depresión geriátrica (GDS-15 y GDS-5): Estudio de la consistencia Interna y estructura factorial. Univ. Psychol. 2011, 10, 735–743. (In Spanish) [Google Scholar] [CrossRef]
- Goldberg, D.; Bridges, K.; Duncan-Jones, P.; Grayson, D. Detecting anxiety and depression in general medical settings. BMJ 1988, 297, 897–899. [Google Scholar] [CrossRef]
- Ferguson, C.J. An effect size primer: A guide for clinicians and researchers. Prof. Psychol. Res. Pract. 2009, 40, 532–538. [Google Scholar] [CrossRef]
- Harada, C.N.; Love, M.C.; Triebel, K.L. Normal cognitive aging. Clin. Geriatr. Med. 2013, 29, 737–752. [Google Scholar] [CrossRef]
- Lipnicki, D.M.; Makkar, S.R.; Crawford, J.D.; Thalamuthu, A.; Kochan, N.A.; Lima-Costa, M.F.; Castro-Costa, E.; Ferri, C.P.; Brayne, C.; Stephan, B.; et al. Determinants of cognitive performance and decline in 20 diverse ethno-regional groups: A COSMIC collaboration cohort study. PLoS Med. 2019, 16, e1002853. [Google Scholar] [CrossRef] [PubMed]
- Adcock, M.; Fankhauser, M.; Post, J.; Lutz, K.; Zizlsperger, L.; Luft, A.R.; Guimarães, V.; Schättin, A.; De Bruin, E.D. Effects of an in-home multicomponent exergame training on physical functions, cognition, and brain volume of older adults: A randomized controlled trial. Front. Med. 2020, 6, 321. [Google Scholar] [CrossRef] [PubMed]
- Wiloth, S.; Lemke, N.; Werner, C.; Hauer, K. Validation of a computerized, game-based assessment strategy to measure training effects on motor-cognitive functions in people with dementia. JMIR Serious Games 2016, 4, e12. [Google Scholar] [CrossRef] [PubMed]
- Van Santen, J.; Dröes, R.-M.; Holstege, M.; Henkemans, O.B.; Van Rijn, A.; De Vries, R.; Van Straten, A.; Meiland, F. Effects of exergaming in people with dementia: Results of a systematic literature review. J. Alzheimer’s Dis. 2018, 63, 741–760. [Google Scholar] [CrossRef]
- Chan, C.; Ngai, E.; Leung, P.; Wong, S. Effect of the adapted virtual reality cognitive training program among chinese older adults with chronic schizophrenia: A pilot study. Int. J. Geriatr. Psychiatry 2009, 25, 643–649. [Google Scholar] [CrossRef] [PubMed]
- Cicek, A.; Ozdincler, A.R.; Tarakci, E. Interactive video game-based approaches improve mobility and mood in older adults: A nonrandomized, controlled trial. J. Bodyw. Mov. Ther. 2020, 24, 252–259. [Google Scholar] [CrossRef]
- Li, J.; Theng, Y.-L.; Foo, S.; Xu, X. Exergames vs. traditional exercise: Investigating the influencing mechanism of platform effect on subthreshold depression among older adults. Aging Ment. Health 2017, 22, 1634–1641. [Google Scholar] [CrossRef]
- Contreras, K.; Cubillos, R.; Hernández, O.; Reveco, C.; Santis, N. Virtual rehabilitation in occupational therapy intervention. Rev. Child Radiol. 2014, 14, 205. [Google Scholar]
- Castellano, J.; Hurtado, M.D.; Contreras, M.I. Mantenimiento de Roles Ocupacionales en el Envejecimiento. In Cuidados, Aspectos Psicológicos y Actividad Física en Relación con la Salud, 1st ed.; Pérez-Fuentes, M.C., Molero Jurado, M., Gázquez Linares, J.J., Barragán Martín, A.B., Martos Martínez, A., Pérez Esteban, M.D., Eds.; Asociación Universitaria de Educación y Psicología: Madrid, Spain, 2016; Volume 2, pp. 9–14. [Google Scholar]
- Clement-Carbonell, V.; Ferrer-Cascales, R.; Ruiz-Robledillo, N.; Rubio-Aparicio, M.; Portilla-Tamarit, I.; Cabañero-Martínez, M.J. Differences in autonomy and health-related quality of life between resilient and non-resilient individuals with mild cognitive impairment. Int. J. Environ. Res. Public Health 2019, 16, 2317. [Google Scholar] [CrossRef]

| Control (n = 40) | Wii (n = 40) | p | η2 p | Statistical Power |
|---|---|---|---|---|
| Age (Years) | ||||
| 83.25 ± 8.78 | 85.05 ± 8.63 | 0.285 | 0.015 | 0.186 |
| Body mass (kg) | ||||
| 76.35 ± 13.54 | 74.60 ± 13.01 | 0.927 | 0.000 | 0.051 |
| Waist circumference (cm) | ||||
| 96.73 ± 14.47 | 96.97 ± 14.74 | 0.645 | 0.003 | 0.074 |
| Arm circumference (cm) | ||||
| 31.18 ± 37.99 | 31.25 ± 37.99 | 0.579 | 0.004 | 0.085 |
| Leg circumference (cm) | ||||
| 49.86 ± 11.34 | 49.65 ± 12.37 | 0.858 | 0.000 | 0.032 |
| Control (n = 40) | Wii (n = 40) | p-Value (t×G) | η2 p | Statistical Power | |
|---|---|---|---|---|---|
| Katz index | |||||
| T1 | 1.23 ± 1.29 | 0.95 ± 1.37 | 0.028 | 0.051 | 0.303 |
| T2 | 1.30 ± 1.20 | 0.82 ± 1.19 * and | |||
| Barthel index | |||||
| T1 | 68.10 ± 20.75 | 75.30 ± 16.69 | 0.025 | 0.064 | 0.614 |
| T2 | 68.88 ± 21.36 | 79.25 ± 14.17 * and | |||
| Lawton and Brody index | |||||
| T1 | 5.88 ± 1.81 | 5.25 ± 2.44 | <0.001 | 0.161 | 0.964 |
| T2 | 5.85 ± 1.81 | 5.90 ± 1.81 * | |||
| Control (n = 40) | Wii (n = 40) | p-Value (t×G) | η2 p | Statistical Power | |
|---|---|---|---|---|---|
| MCE | |||||
| T1 | 23.10 ± 5.73 | 21.28 ± 5.78 | <0.001 | 0.369 | 1.000 |
| T2 | 22.40 ± 6.00 * | 23.32 ± 5.50 * | |||
| FAST-GDS | |||||
| T1 | 2.82 ± 1.36 | 3.20 ± 1.24 | <0.001 | 0.181 | 0.982 |
| T2 | 3.00 ± 1.43 * | 2.97 ± 1.31 * | |||
| Control (n = 40) | Wii (n = 40) | p-Value (txG) | η2 p | Statistical Power | |
|---|---|---|---|---|---|
| EDG-15 | |||||
| T1 | 4.35 ± 2.80 | 5.85 ± 3.50 | <0.001 | 0.335 | 1.000 |
| T2 | 5.08 ± 3.15 * | 4.55 ± 2.84 * | |||
| DAIR | |||||
| T1 | 1.33 ± 0.26 | 1.42 ± 0.27 | <0.001 | 0.180 | 0.980 |
| T2 | 1.34 ± 0.25 * | 1.37 ± 0.27 * | |||
| EADG | |||||
| T1 | 3.47 ± 2.31 | 4.07 ± 2.63 | <0.001 | 0.212 | 0.0994 |
| T2 | 3.78 ± 2.48 | 3.08 ± 2.14 * | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jahouh, M.; González-Bernal, J.J.; González-Santos, J.; Fernández-Lázaro, D.; Soto-Cámara, R.; Mielgo-Ayuso, J. Impact of an Intervention with Wii Video Games on the Autonomy of Activities of Daily Living and Psychological–Cognitive Components in the Institutionalized Elderly. Int. J. Environ. Res. Public Health 2021, 18, 1570. https://doi.org/10.3390/ijerph18041570
Jahouh M, González-Bernal JJ, González-Santos J, Fernández-Lázaro D, Soto-Cámara R, Mielgo-Ayuso J. Impact of an Intervention with Wii Video Games on the Autonomy of Activities of Daily Living and Psychological–Cognitive Components in the Institutionalized Elderly. International Journal of Environmental Research and Public Health. 2021; 18(4):1570. https://doi.org/10.3390/ijerph18041570
Chicago/Turabian StyleJahouh, Maha, Jerónimo J. González-Bernal, Josefa González-Santos, Diego Fernández-Lázaro, Raúl Soto-Cámara, and Juan Mielgo-Ayuso. 2021. "Impact of an Intervention with Wii Video Games on the Autonomy of Activities of Daily Living and Psychological–Cognitive Components in the Institutionalized Elderly" International Journal of Environmental Research and Public Health 18, no. 4: 1570. https://doi.org/10.3390/ijerph18041570
APA StyleJahouh, M., González-Bernal, J. J., González-Santos, J., Fernández-Lázaro, D., Soto-Cámara, R., & Mielgo-Ayuso, J. (2021). Impact of an Intervention with Wii Video Games on the Autonomy of Activities of Daily Living and Psychological–Cognitive Components in the Institutionalized Elderly. International Journal of Environmental Research and Public Health, 18(4), 1570. https://doi.org/10.3390/ijerph18041570










