The Prevalence of Peripheral Erythrophagocytosis in Pediatric Immune-Mediated Hemolytic Anemia
Abstract
1. Introduction
2. Materials and Methods
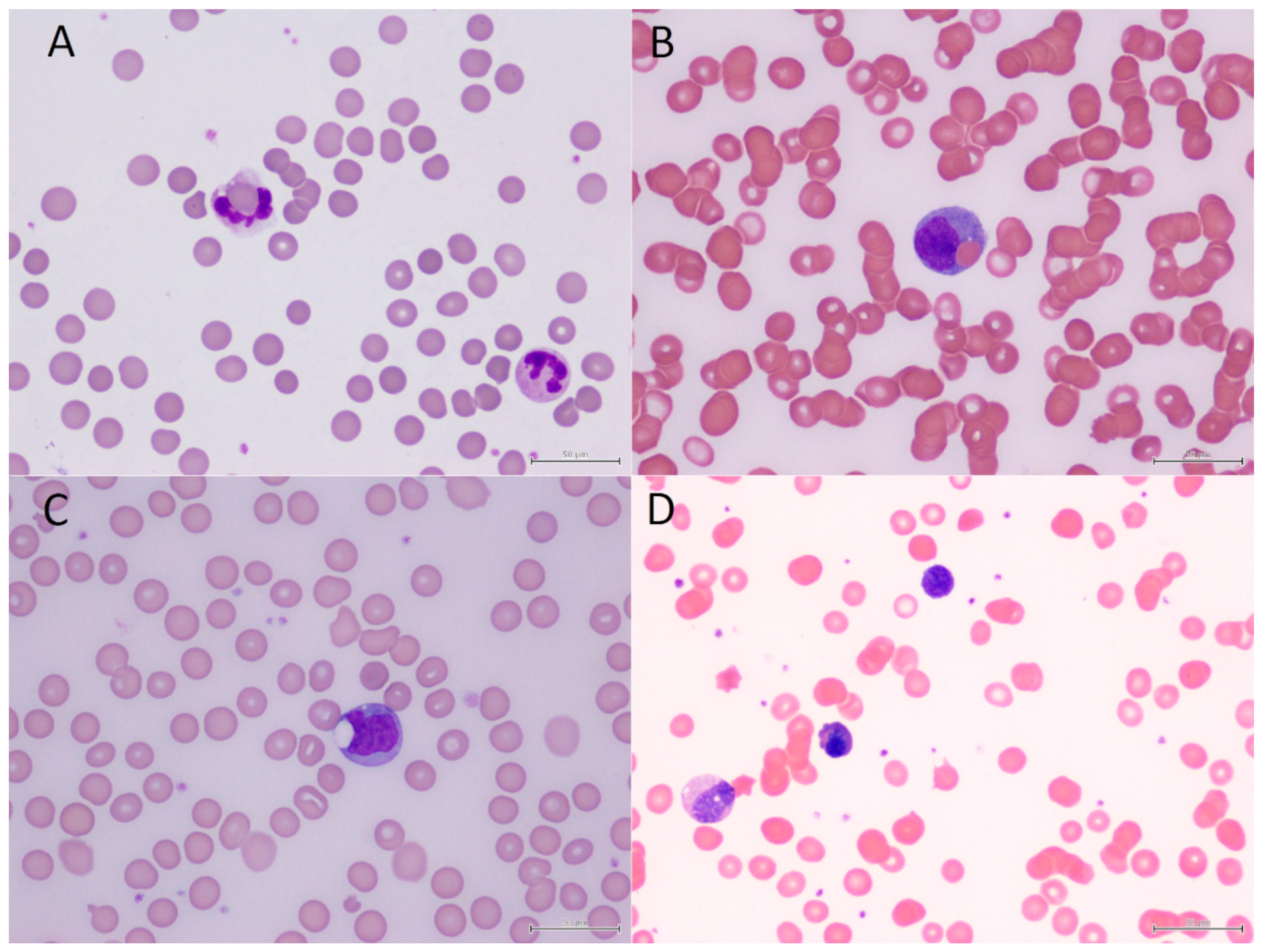
3. Results
4. Discussion
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ladogana, S.; Maruzzi, M.; Samperi, P.; Perrotta, S.; Del Vecchio, G.C.; Notarangelo, L.D.; Farruggia, P.; Verzegnassi, F.; Masera, N.; Saracco, P.; et al. Diagnosis and management of newly diagnosed childhood autoimmune hemolytic anemia. Recommendations from the Red Cell Study Group of the Paediatric Haemato-Oncology Italian Association. Blood Transfus. 2017, 15, 259–267. [Google Scholar] [PubMed]
- Ware, R.E. Autoimmune hemolytic anemia (AIHA) in children: Classification, clinical features, and diagnosis. In UpToDate; Connor, R.F., Ed.; Wolters Kluwer: Alphen aan den Rijn, The Netherlands, 2024. [Google Scholar]
- Lu, Y.; Huang, X.M. Autoimmune hemolytic anemia as an initial presentation in children with systemic lupus erythematosus: Two case reports. J. Int. Med. Res. 2022, 50, 3000605221115390. [Google Scholar] [CrossRef] [PubMed]
- Mantadakis, E.; Farmaki, E. Natural history, pathogenesis, and treatment of Evans syndrome in children. J. Pediatr. Hematol. Oncol. 2017, 39, 413–419. [Google Scholar] [CrossRef] [PubMed]
- Leach, M.; Bain, B.J. Chapter 88: Spherocytic red cell disorders. In Haematology: From the Image to the Diagnosis; John Wiley & Sons Ltd.: Oxford, UK, 2022; pp. 178–179. [Google Scholar]
- Kuwata, K.; Yamada, S.; Kinuwaki, E.; Naito, M.; Mitsuya, H. Peripheral hemophagocytosis: An early indicator of advanced systemic inflammatory response syndrome/hemophagocytic syndrome. Shock 2006, 25, 344–350. [Google Scholar] [CrossRef]
- Islam, M.D.; Chia, L. Hyperhemolysis syndrome in a patient with sickle cell disease with erythrophagocytosis in peripheral blood. Eur. J. Haematol. 2010, 84, 188. [Google Scholar] [CrossRef]
- Matson, D.R.; Matkovic, E. Peripheral erythrophagocytosis in paroxysmal cold hemaglobinuria. Blood 2023, 141, 1233. [Google Scholar] [CrossRef]
- Amelirad, A.; Modaresi, P.; Soltani, H. Neutrophilic erythrophagocytosis in myelodysplastic syndrome and cold agglutinin disease co-occurrence. Clin. Case Rep. 2023, 11, e06828. [Google Scholar] [CrossRef]
- Pervais, O.; Louka, E.; Willan, J. Neutrophilic erythrophagocytosis in a child with paroxysmal cold haemoglobinuria. EJHaem 2022, 3, 1394–1395. [Google Scholar] [CrossRef]
- Eldar, D.; Ganzel, C. Erythrophagocytosis in a young adult with Mycoplasma pneumoniae-induced paroxysmal cold hemoglobinuria. Blood 2021, 137, 1432. [Google Scholar] [CrossRef]
- Grech, M.; Camellieri, D.J. Erythrophagocytosis on the peripheral blood smear. Blood 2019, 133, 285. [Google Scholar] [CrossRef]
- Lee, J.H. A rare case of erythrophagocytosis by neutrophils on the peripheral blood smear. Blood Res. 2017, 52, 74–75. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Reddivalla, N. Florid erythrophagocytosis by neutrophils in peripheral blood. Blood 2016, 128, 739. [Google Scholar] [CrossRef] [PubMed]
- Chandrashekar, V.; Soni, M. Florid erythrophagocytosis on the peripheral blood smear. J. Lab. Physicians 2012, 4, 59–61. [Google Scholar] [PubMed]
- Wong, A.K.; Said, J. Erythrophagocytosis by neutrophils. Blood 2011, 117, 753. [Google Scholar]
- Lobreglio, G.; Valacca, A. Erythrophagocytosis. N. Engl. J. Med. 2001, 344, 897. [Google Scholar] [CrossRef]
- Depcik-Smith, N.D.; Escobar, M.A.; Ma, A.D.; Brecher, M.E. RBC rosetting and erythrophagocytosis in adult paroxysmal cold hemoglobinuria. Transfusion 2001, 41, 163. [Google Scholar] [CrossRef]
- Bolton-Maggs, P.H.B.; Langer, J.C.; Iolascon, A.; Tittensor, P.; King, M.J. Guidelines for the diagnosis and management of hereditary spherocytosis—2011 update. Br. J. Haematol. 2012, 156, 37–49. [Google Scholar] [CrossRef]
- Lee, A.C. Peripheral haemophagocytosis: A paediatric series. Br. J. Haematol. 2020, 191, 294–297. [Google Scholar] [CrossRef]
- Chong, J.H.; Isa, M.S.; Koh, M.J.; Lee, A.C. Cutaneous cytomegalovirus mimicking mpox in an immunocompromised infant. Arch. Dis. Child. 2024. online ahead of print. [Google Scholar] [CrossRef]
- Hadjiaggelidou, C.; Douganiotis, G.; Tsirou, K.; Verrou, E.; Triantafyllou, T.; Keramidioti, K.; Konstantinidou, P.; Katodritou, E. A rare case of autoimmune hemolytic anemia during venetoclax therapy for relapsed chronic lymphocytic leukemia. Leuk. Lymphoma 2021, 62, 3054–3056. [Google Scholar] [CrossRef]
- Aladjidi, N.; Jutand, M.A.; Beaubois, C.; Fernandes, H.; Jeanpetit, J.; Coureau, G.; Gilleron, V.; Kostrzewa, A.; Lauroua, P.; Jeanne, M.; et al. Reliable assessment of the incidence of childhood autoimmune hemolytic anemia. Pediatr. Blood Cancer 2017, 64, e26683. [Google Scholar] [CrossRef]
- Bansal, M.G.; Crane, M.G. Chapter 3. Hypochromic and hemolytic anemias. In Atlas of Diagnostic Hematology; Salama, M., Teruya-Feldstein, J., Kremyanskaya, M., Eds.; Elsevier: Philadelphia, PA, USA, 2021; pp. 22–46. [Google Scholar]
- Fan, J.; He, H.; Zhao, W.; Wang, Y.; Lu, J.; Li, J.; Li, J.; Xiao, P.; Lu, Y.; Chai, Y.; et al. Clinical features and treatment outcomes of childhood autoimmune hemolytic anemia: A retrospective analysis of 68 cases. J. Pediatr. Hematol. Oncol. 2016, 38, e50–e55. [Google Scholar] [CrossRef] [PubMed]
- Kar, S.; Kumar, C.G.D.; Kar, R.; Basavarajegowda, A. Autoimmune hemolytic anemia in children: Clinical profile and outcome. Indian J. Pediatr. 2024, 91, 143–148. [Google Scholar] [CrossRef] [PubMed]
- Gammal, R.S.; Pirmohamed, M.; Somogyi, A.A.; Morris, S.A.; Formea, C.M.; Elchynski, A.L.; Oshikoya, K.A.; McLeod, H.L.; Haidar, C.E.; Whirl-Carrillo, M.; et al. Expanded clinical pharmacogenetics implementation consortium guideline for medication use in the context of G6PD genotype. Clin. Pharmacol. Ther. 2023, 113, 973–985. [Google Scholar] [CrossRef] [PubMed]
- Loffler, H.; Rastetter, J.; Haferlach, T. Chapter 4. Blood and bone marrow. In Atlas of Clinical Hematology; Springer: Berlin, Germany, 2005; pp. 28–291. [Google Scholar]
- Garratty, G. Erythrophagocytosis on the peripheral blood smear and paroxysmal cold hemoglobinuria. Transfusion 2001, 41, 1073. [Google Scholar] [CrossRef]
- Ravelli, A.; Davi, S.; Minoia, F.; Martini, A.; Cron, R.Q. Macrophage activation syndrome. Hematol. Oncol. Clin. N. Am. 2015, 29, 927–941. [Google Scholar] [CrossRef]
- Filipovich, A.H.; Chandrakasan, S. Pathogenesis of hemophagocytic lymphohistiocytosis. Hematol. Oncol. Clin. N. Am. 2015, 29, 895–902. [Google Scholar] [CrossRef]
- Lee, A.C.; Ee, K.; Tan, N. Peripheral hemophagocytosis: A rapid clue to severe sepsis and hemophagocytic lymphohistiocyotsis. Pediatr. Neonatol. 2019, 60, 108–109. [Google Scholar] [CrossRef]
| Case | Sex/Age | Pre-Existing Conditions | Concurrent Diagnoses | Hb | Bilirubin | DAT | Cold Aggl. | ANA | Remarks |
|---|---|---|---|---|---|---|---|---|---|
| Absence of peripheral erythrophagocytosis | |||||||||
| 1 | M/16.6 | MDS | Pneumonia | 6.5 | 8 | - | + 1:256 | - | Responded to prednisolone treatment |
| 2 | F/2.5 | Nil | Pneumonia | 5.9 | 6 | - | + 1:1024 | ND | Resolved after transfusion and antibiotic treatment |
| 3 | F/8.6 | Nil | SLE/Evans syndrome | 8.1 | 32 | + (poly) | + 1:512 | + | - |
| 4 | M/5.4 | HS | URI, Mycoplasma infection | 5.1 | 26 | - | + 1:64 | ND | Resolved after transfusion and antibiotic treatment |
| 5 | F/5.9 | Nil | EBV-IM | 5.6 | 11 | + (poly) | ND | - | Resolved after transfusion and corticosteroid treatment |
| 6 | M/15.1 | Nil | Nil | 2.5 | ND | + (IgG and C3) | ND | - | Resolved after transfusion and corticosteroid treatment |
| 7 | M/1.2 | Nil | WAS, EBV and CMV co-infection | 6.6 | 22 | + (IgG) | ND | ND | Partial response after IVIG |
| Presence of peripheral erythrophagocytosis | |||||||||
| 8 | M/2.5 | Nil | Pneumonia, hRV/EV infection | 4.8 | 69 | + (poly) | - | + | Resolved after transfusion and single dose of IVIG |
| 9 | F/3.8 | Neuroblastoma | HSCT | 6.1 | 30 | + (poly) | ND | ND | Resolved after transfusion and single dose of IVIG |
| 10 | M/6.2 | G6PD deficiency | Pneumonia, Mycoplasma infection | 7.8 | 24 | + (poly) | + 1:64 | ND | Resolved after single dose of IVIG |
| 11 | M/12.4 | AML | Venetoclax therapy | 7.3 | 40 | + (IgG) | ND | + | Succumbed from refractory leukemia |
| 12 | M/0.8 | Chronic neutropenia | Pneumonia, Mycoplasma infection | 7.9 | 3 | + (poly) | ND | - | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, A.C.-w. The Prevalence of Peripheral Erythrophagocytosis in Pediatric Immune-Mediated Hemolytic Anemia. Hematol. Rep. 2025, 17, 4. https://doi.org/10.3390/hematolrep17010004
Lee AC-w. The Prevalence of Peripheral Erythrophagocytosis in Pediatric Immune-Mediated Hemolytic Anemia. Hematology Reports. 2025; 17(1):4. https://doi.org/10.3390/hematolrep17010004
Chicago/Turabian StyleLee, Anselm Chi-wai. 2025. "The Prevalence of Peripheral Erythrophagocytosis in Pediatric Immune-Mediated Hemolytic Anemia" Hematology Reports 17, no. 1: 4. https://doi.org/10.3390/hematolrep17010004
APA StyleLee, A. C.-w. (2025). The Prevalence of Peripheral Erythrophagocytosis in Pediatric Immune-Mediated Hemolytic Anemia. Hematology Reports, 17(1), 4. https://doi.org/10.3390/hematolrep17010004






