Machine Learning-Powered Smart Healthcare Systems in the Era of Big Data: Applications, Diagnostic Insights, Challenges, and Ethical Implications
Abstract
1. Introduction
Previous Reviews and Research Landscape
2. Methodology
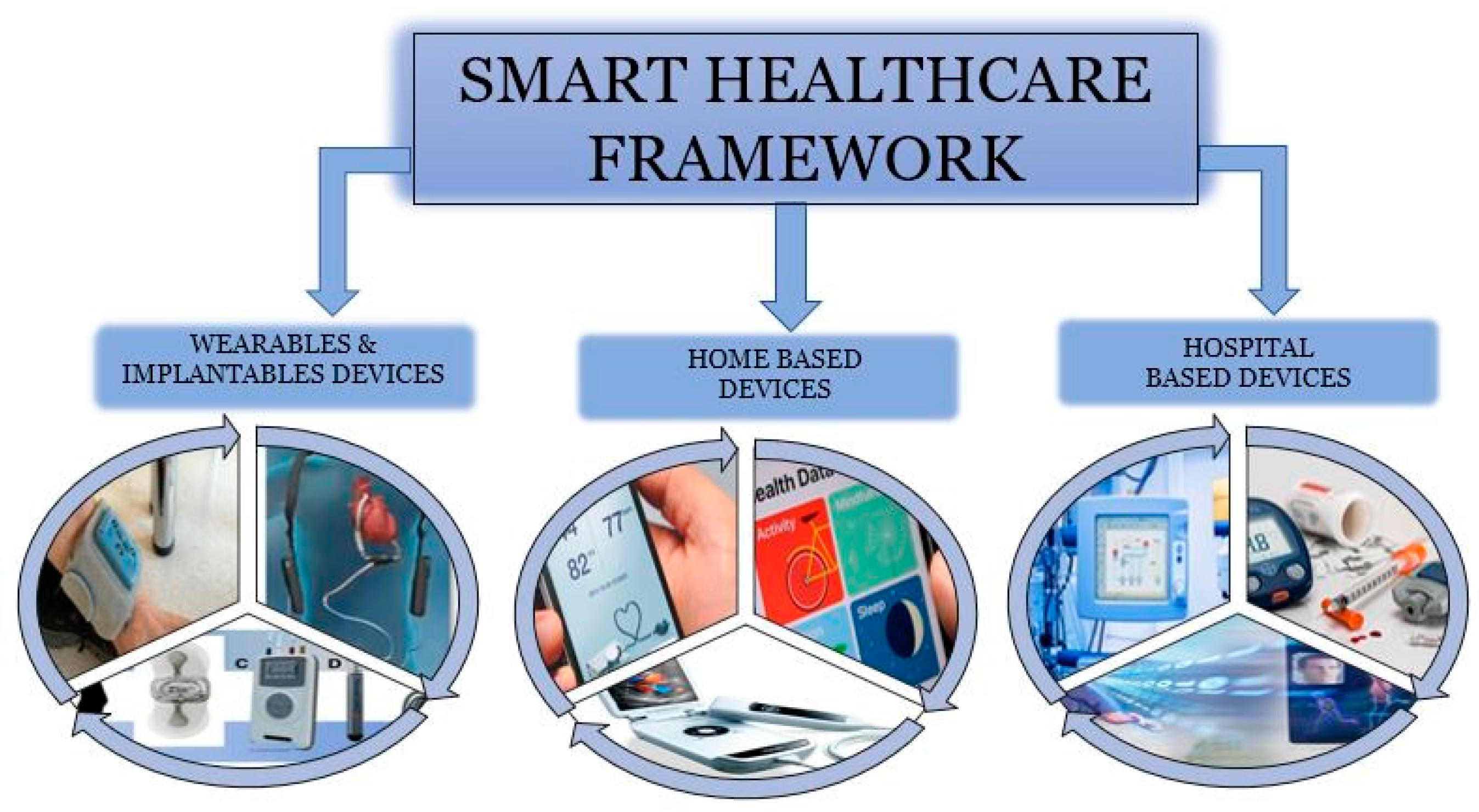
3. Smart Healthcare Systems
3.1. Smart Healthcare Framework
3.1.1. Wearables IoT Devices
- A biker employing a vital sign system, specifically a wristband, is involved in an accident. The body sensor network detects the fall, which transmits an alarm to the city’s infrastructure. The technology replies by evaluating road congestion and dispatching ambulances through the most direct route. Furthermore, municipal traffic signals are automatically modified to shorten the time the ambulances take to reach the rider.
- Fitbit Inspire, a wearable fitness band, records all-day activity, relaxation, calorie counting, and breathing rate, among other things, and shows the results on an Android smartphone while storing the cloud to help the user achieve his or her chosen fitness goal. Google Fit, Fitbit Coach, Nike Training Club, Runtastic, and other mobile phone overall fitness applications track wellness and exercise regimens for individual requirements.
3.1.2. Home-Based IoT Devices
- Glycaemic monitoring apps supervise the patient’s glucose level. They can undertake a variety of actions relying just on the app, such as measuring the information in the device and/or the infrastructure as a service, displaying on connected phones, notifying caregivers, advising the general practitioner, and tracking to the health insurer, among other things.
- Electrocardiogram and cardiovascular monitoring applications use ECG, heart rate readings, and basic pattern recognition to follow the heart’s electrical activity. Depending on the app’s circumstances, they can forecast some fundamental problems, such as arrhythmias and cardiac ischemia, and notify people, clinicians, and caretakers.
3.1.3. Hospital-Based IoT Devices
- Concentrating on sensor technologies for health checks and appraisal techniques in the home and neighborhood atmospheres to minimize direct stress on healthcare environments and convert it to a digital dissemination of knowledge.
- Transforming the pharmaceutical procedure from a reaction to a proactive risk management strategy can dramatically reduce hospitalization costs for acute occurrences.
- Enhancing the personalized recommendations of the health and care system so that private citizens can supervise and recognize their potential risk characterization, preventive medicine intervention, and diagnosis, allowing patients to stay independent while being cared for, which has a strong positive influence on their psychological makeup and, as a result, their health status.
- Facilitating improved clinical maintenance and permitting the health service to prioritize sick people in the greatest need properly.
- Assisting self-care clinical techniques to observe health status and other varied metrics, in which these data are exchanged with a physician to conduct a diagnosis, either in person or by teleconsultation. Likewise, for mild conditions such as influenza, diagnosis can sometimes be computerized.
- Maximizing moment-in-time testing by lowering diagnostic time by eliminating the need to transfer specimens elsewhere to be analyzed. Computerized monitoring using blood pressure cuffs and electronic thermometers, for example, can assist the doctor in reviewing a medical history as statistics have been taken.
4. Machine Learning and Big Data Applications in Smart Healthcare Diagnostics
4.1. Overview of Machine Learning
4.2. Big Data in Smart Healthcare
4.3. Convergence of Machine Learning and Big Data
5. Machine Learning for Voluminous Healthcare Data: Real-World Case Studies
5.1. Real World Case Studies
5.1.1. UK Biobank: Advancing Global Medical Research
5.1.2. NVIDIA and GE HealthCare: Transforming Diagnostic Imaging
5.1.3. Healthcare Platform Utilizing Big Data Analytics (BDA)
5.1.4. Big Data in Oncology Drug Development
5.1.5. Oncora Medical: Streamlining Oncology Workflows
5.1.6. IQVIA’s NLP Data Factory for Population Health
5.1.7. Digital Health Platform in Colombia
5.1.8. BigQuery ML for Diabetes Prediction
5.1.9. HealthEdge: Predicting Type 2 Diabetes
5.1.10. AI Predicting 10-Year Heart Disease Risk
5.2. ML-Driven Innovations in Disease Diagnosis and Early Detection
5.2.1. Medical Imaging and Radiology
5.2.2. Natural Language Processing in Clinical Text
5.2.3. Large Language Models (LLMs) in Healthcare
5.2.4. Wearable Devices and Continuous Monitoring
5.2.5. Neurodegenerative Diseases and Early Detection
5.2.6. Integration and Future Prospects
6. Major Challenges Faced in Processing Huge Healthcare Data
6.1. Data Challenges
- Volume: The sheer quantity of data generated by organizations, often reaching hundreds of terabytes or even petabytes, stems from routine business operations and regulatory obligations. In the healthcare domain, this data proliferation quickly leads to saturation, wherein the proportion of actionable or relevant information diminishes. This phenomenon gives rise to what is termed the “blind zone”: a segment of data characterized by unknown or unexamined facts that may be either inconsequential or critically informative.
- Variety: The exponential growth of sensor technologies, IoT devices, and diverse communication platforms has resulted in a highly heterogeneous data landscape. Data today spans structured formats (e.g., relational databases), semi-structured formats (e.g., XML or JSON with identifiable markers but lacking a rigid schema), and unstructured formats (e.g., textual data, multimedia, and user-generated content from websites and social media). This diversity presents formidable challenges for integration, storage, and analysis across systems.
- Velocity: The velocity dimension refers to the rapid rate at which data is generated, transmitted, and analyzed. Modern data streams require real-time or near-real-time processing due to their ephemeral value. In contexts such as healthcare, where clinical decisions are time-sensitive, the inability to process high-speed data flows in transit can result in missed opportunities for timely interventions.
- Veracity: Veracity pertains to the reliability, accuracy, and quality of data. Issues such as misinformation, incomplete records, and noise complicate the extraction of meaningful insights. Given the scale of big data, ensuring data veracity becomes a significant hurdle, particularly in fields like healthcare, where analytical precision is paramount. Compounding this issue is the shortage of highly skilled data scientists, professionals adept in data mining, transformation, interpretation, and innovation, whose expertise is often prohibitively expensive and challenging to retain.
- Volatility: Volatility describes the degree to which data can be deemed reliable over time and the duration for which it remains relevant or valid within a system. In an era increasingly reliant on data-driven insights, understanding the temporal sensitivity of data, when it becomes obsolete, is essential for maintaining the integrity and usefulness of information used in decision-making processes.
6.2. Process Challenges
6.3. Management Challenges
7. Existing ML-Based Big Data Solutions in Managing Healthcare Data
7.1. Diagnosis and Treatment
7.2. Medical Imaging
7.3. Drug Discovery and Development
Limitations of ML in Late-Stage Drug Development
7.4. Natural Language Processing of Medical Records
7.5. ML Applications in Prognosis
7.6. ML for Medical Time Analysis
7.7. Prediction of Future Illness Symptoms
8. Ethical Considerations in AI-Driven Smart Healthcare
- Data Privacy and Security: A primary ethical concern involves the privacy and security of patient data. Smart healthcare platforms routinely collect vast volumes of sensitive information from sources such as IoT devices deployed in operating theatres, EHRs, and genomic databases. Safeguarding this data against breaches, misuse, or unauthorized access is not only a legal mandate but also an ethical imperative. In alignment with principles of fair data sharing, emerging technologies, such as blockchain, differential privacy, and secure federated learning, are being increasingly adopted to protect patient data while still enabling its utility for clinical insight generation and ML model development.
- Consent and Transparency: A further ethical challenge arises from issues of consent and transparency. The deployment of black-box ML systems often impedes comprehension of decision-making processes by both patients and clinicians. Explainability must, therefore, be prioritized in the design of ethical AI, particularly in healthcare settings where model outputs may inform critical, high-stakes decisions. Patients should be adequately informed about the use of their data, the risks involved, and their rights regarding contesting or overriding automated decisions.
- Algorithmic Accountability: Equally crucial is the matter of algorithmic accountability. As AI systems become integral to decision-making in diagnosis, treatment planning, and resource allocation, mechanisms for tracing errors, identifying points of failure, and assigning accountability must be clearly established. Health systems must avoid uncritical adoption of these tools in the absence of robust governance frameworks, domain expertise, and risk mitigation strategies to prevent unintended harm.
- Economic Disparity and Access Limitations: AI-powered healthcare tools often entail high implementation and maintenance costs, disproportionately benefiting wealthier individuals and institutions. This economic imbalance risks widening existing disparities in care quality and health outcomes, particularly in under-resourced settings where financial barriers limit access to advanced diagnostics and AI-supported clinical tools.
- Bias in AI Performance Evaluation: Many AI solutions are developed, validated, and promoted by the same entities, raising concerns regarding inflated performance claims and commercial bias. Clinical robustness should be ensured through independent third-party audits, stringent regulatory oversight, and the use of open, transparent benchmarking methodologies.
- Biases in Historical Healthcare Data: The datasets used to train ML models often reflect historical inequities in healthcare delivery. Consequently, models trained on such data risk perpetuating discriminatory outcomes across race, gender, or socioeconomic status. Ensuring fairness requires rigorous auditing of training datasets, inclusive representation during model design, and continuous model updates to align predictions with equitable health outcomes.
9. Future Research Direction
- Privacy and Security
- Scalability and Infrastructure
- Explainability and Clinical Integration
10. Conclusions
- Diagnostic accuracy of 95%+ is achieved by ML-integrated platforms, comparable to conventional manual-inspection methods [86].
- Big data-enabled AI diagnostic systems have achieved cost reductions of up to 20%, primarily by minimizing unnecessary testing and streamlining decision workflows [82].
- AI-powered imaging systems developed by NVIDIA and GE HealthCare have been successfully deployed for automated X-ray and ultrasound assessments, improving diagnostic efficiency and expanding access globally [86].
- Oncora Medical is advancing the development of ML algorithms and BDA to establish a standardized and automated solution for oncology treatment planning. The platform aggregates patient-specific clinical data, including tumor genetic profiles, medical histories, imaging results, and prior treatment responses, to assist clinicians in efficiently generating personalized therapy recommendations. This automated approach significantly reduces the interval between diagnosis and the initiation of treatment, thereby enhancing patient outcomes through the provision of timely, precise, and individualized cancer care.
- The UK Biobank uses ML to advance population health research through massive genomic datasets.
- Heterogeneity and interoperability of data across systems.
- Privacy and security risks in cloud and IoT-enabled environments.
- Computational hardness in handling high-dimensional, real-time data.
- Lack of black-box ML models’ explainability hinders clinical trust and uptake.
- Scalability issues in scaling ML models across large, distributed healthcare systems.
Limitations of the Review
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Xu, G.; Fan, X.; Xu, S.; Cao, Y.; Chen, X.; Shang, T.; Yu, S. Anonymity-Enhanced Sequential Multi-Signer Ring Signature for Secure Medical Data Sharing in IoMT. IEEE Trans. Inf. Forensics Secur. 2025, 20, 5647–5662. [Google Scholar] [CrossRef]
- Kandeel, M. Revolutionizing Healthcare: Harnessing the Power of Artificial Intelligence for Enhanced Diagnostics, Treatment and Drug Discovery. Int. J. Pharmacol. 2024, 20, 1–10. [Google Scholar] [CrossRef]
- Xiao, X.; Li, Y.; Wu, Q.; Liu, X.; Cao, X.; Li, M.; Dai, X. Development and validation of a novel predictive model for dementia risk in middle-aged and elderly depression individuals: A large and longitudinal machine learning cohort study. Alzheimer’s Res. Ther. 2025, 17, 103. [Google Scholar] [CrossRef]
- Research and Markets. Global Big Data in Healthcare Market Trends and Forecasts Report 2024: A $540 Billion Industry by 2035, from $67 Billion in 2023; GlobeNewswire: El Segundo, CA, USA, 2024. [Google Scholar]
- Greene, L. How Healthcare Data Technology is Leveraged by Leaders. Arcadia Solutions. 6 September 2023. Available online: https://arcadia.io/resources/healthcare-data-technology (accessed on 10 May 2025).
- He, W.; Zhu, J.; Feng, Y.; Liang, F.; You, K.; Chai, H.; Wang, W. Neuromorphic-enabled video-activated cell sorting. Nat. Commun. 2024, 15, 10792. [Google Scholar] [CrossRef]
- Zhang, G.; Song, C.; Yin, M.; Liu, L.; Zhang, Y.; Li, Y.; Li, C. TRAPT: A multi-stage fused deep learning framework for predicting transcriptional regulators based on large-scale epigenomic data. Nat. Commun. 2025, 16, 3611. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Chai, Y.; Khan, F.; Jan, S.R.U.; Verma, S.; Menon, V.G.; Kavita, f.; Li, X. A comprehensive survey on machine learning-based big data analytics for IoT-enabled smart healthcare system. Mob. Netw. Appl. 2021, 26, 234–252. [Google Scholar] [CrossRef] [PubMed]
- Taha, K. Big Data Analytics in IoT, social media, NLP, and information security: Trends, challenges, and applications. J. Big Data 2025, 12, 150. [Google Scholar] [CrossRef]
- Cai, Q.; Wang, H.; Li, Z.; Liu, X. A survey on multimodal data-driven smart healthcare systems: Approaches and applications. IEEE Access 2019, 7, 133583–133599. [Google Scholar] [CrossRef]
- Badawy, M.; Ramadan, N.; Hefny, H.A. Healthcare predictive analytics using machine learning and deep learning techniques: A survey. J. Electr. Syst. Inf. Technol. 2023, 10, 40. [Google Scholar] [CrossRef]
- Nguyen, D.C.; Pham, Q.-V.; Pathirana, P.N.; Ding, M.; Seneviratne, A.; Lin, Z.; Dobre, O.; Hwang, W.-J. Federated learning for smart healthcare: A survey. ACM Comput. Surv. (CSUR) 2022, 55, 1–37. [Google Scholar] [CrossRef]
- Salman, M.; Munawar, H.S.; Latif, K.; Akram, M.W.; Khan, S.I.; Ullah, F. Big data management in drug–drug interaction: A modern deep learning approach for smart healthcare. Big Data Cogn. Comput. 2022, 6, 30. [Google Scholar] [CrossRef]
- Rahman, A.; Debnath, T.; Kundu, D.; Khan, M.S.I.; Aishi, A.A.; Sazzad, S.; Sayduzzaman, M.; Band, S.S. Machine learning and deep learning-based approach in smart healthcare: Recent advances, applications, challenges and opportunities. AIMS Public Health 2024, 11, 58. [Google Scholar] [CrossRef] [PubMed]
- Babar, M.; Qureshi, B.; Koubaa, A. Review on Federated Learning for digital transformation in healthcare through big data analytics. Future Gener. Comput. Syst. 2024, 160, 14–28. [Google Scholar] [CrossRef]
- Istepanian, R.S.; Al-Anzi, T. m-Health 2.0: New perspectives on mobile health, machine learning and big data analytics. Methods 2018, 151, 34–40. [Google Scholar] [CrossRef] [PubMed]
- Selna, A.; Othman, Z.; Tham, J.; Yoosuf, A.K. Challenges to using electronic health records to enhance patient safety, in a Small Island Developing State (SIDS) context. Rec. Manag. J. 2022, 32, 249–259. [Google Scholar] [CrossRef]
- Hu, F.; Yang, H.; Qiu, L.; Wei, S.; Hu, H.; Zhou, H. Spatial structure and organization of the medical device industry urban network in China: Evidence from Specialized, Refined, Distinctive, and Innovative firms. Front. Public Health 2025, 13, 1518327. [Google Scholar] [CrossRef]
- Gardašević, G.; Katzis, K.; Bajić, D.; Berbakov, L. Emerging wireless sensor networks and Internet of Things technologies—Foundations of smart healthcare. Sensors 2020, 20, 3619. [Google Scholar] [CrossRef]
- Baker, S.B.; Xiang, W.; Atkinson, I. Internet of things for smart healthcare: Technologies, challenges, and opportunities. IEEE Access 2017, 5, 26521–26544. [Google Scholar] [CrossRef]
- Balasundaram, A.; Routray, S.; Prabu, A.; Krishnan, P.; Malla, P.P.; Maiti, M. Internet of things (IoT)-based smart healthcare system for efficient diagnostics of health parameters of patients in emergency care. IEEE Internet Things J. 2023, 10, 18563–18570. [Google Scholar] [CrossRef]
- Ijaz, M.; Li, G.; Wang, H.; El-Sherbeeny, A.M.; Moro Awelisah, Y.; Lin, L.; Koubaa, A.; Noor, A. Intelligent fog-enabled smart healthcare system for wearable physiological parameter detection. Electronics 2020, 9, 2015. [Google Scholar] [CrossRef]
- Sikdar, S.; Guha, S. Advancements of healthcare technologies: Paradigm towards smart healthcare systems. Recent Trends Image Signal Process. Comput. Vis. 2020, 1124, 113–132. [Google Scholar]
- Khan, M.; Hossni, Y. A comparative analysis of LSTM models aided with attention and squeeze and excitation blocks for activity recognition. Sci. Rep. 2025, 15, 3858. [Google Scholar] [CrossRef] [PubMed]
- Qi, K. Advancing hospital healthcare: Achieving IoT-based secure health monitoring through multilayer machine learning. J. Big Data 2025, 12, 1. [Google Scholar] [CrossRef]
- Maruthupandi, J.; Sivakumar, S.; Dhevi, B.L.; Prasanna, S.; Priya, R.K.; Selvarajan, S. An intelligent attention based deep convoluted learning (IADCL) model for smart healthcare security. Sci. Rep. 2025, 15, 1363. [Google Scholar] [CrossRef]
- Khalid, U.; Chen, L.; Khan, A.A.; Chen, B.; Mehmood, F.; Yasir, M. A smart facial acne disease monitoring for automate severity assessment using AI-enabled cloud-based internet of things. Discov. Comput. 2025, 28, 12. [Google Scholar] [CrossRef]
- Xie, Q.; Ding, Z. Provably secure and lightweight blockchain based cross hospital authentication scheme for IoMT-based healthcare. Sci. Rep. 2025, 15, 6461. [Google Scholar] [CrossRef]
- Zhou, Z.; Jin, Y.; Fu, J.; Si, S.; Liu, M.; Hu, Y.; Gan, J.; Deng, Y.; Li, R.; Yang, J. Smart wireless flexible sensing system for unconstrained monitoring of ballistocardiogram and respiration. npj Flex. Electron. 2025, 9, 15. [Google Scholar] [CrossRef]
- Pham, T.P.T.; Huang, M.C. Exploring the relationship between nursing professional values and job satisfaction in Vietnam. Nurs. Pract. Today 2025, 12, 55–64. [Google Scholar] [CrossRef]
- Magara, T.; Zhou, Y. EMAKAS: An efficient three-factor mutual authentication and key-agreement scheme for IoT environment. Cyber. Secur. Appl. 2025, 3, 100066. [Google Scholar] [CrossRef]
- Hossain, M.K.; Thakur, V. A performance management framework for smart health-care supply chain based on industry 4.0 technologies. J. Glob. Oper. Strateg. Sourc. 2024, 18, 285–306. [Google Scholar] [CrossRef]
- Mishra, G. A Comprehensive Review of Smart Healthcare Systems: Architecture, Applications, Challenges, and Future Directions. Int. J. Innov. Res. Technol. Sci. 2024, 12, 210–218. [Google Scholar]
- Zhao, X.; Ge, B. An indicator framework for assessing the readiness of hospital in the smart healthcare transformation. IOP Conf. Ser. Earth Environ. Sci. 2022, 1101, 072010. [Google Scholar] [CrossRef]
- Al-Sanjary, O.I.; Vasuthevan, S.; Omer, H.K.; Mohammed, M.N.; Abdullah, M.I. An Intelligent Recycling Bin Using Wireless Sensor Network Technology. In Proceedings of the 2019 IEEE International Conference on Automatic Control and Intelligent Systems, I2CACIS, Selangor, Malaysia, 29 June 2019; pp. 30–33. [Google Scholar] [CrossRef]
- Cui, Q.; Ding, Z.; Chen, F. Hybrid Directed Hypergraph Learning and Forecasting of Skeleton-Based Human Poses. Cyborg Bionic Syst. 2024, 5, 0093. [Google Scholar] [CrossRef] [PubMed]
- Taware, R.D.; Deshmukh, A.; Singh, C.; Rathod, N. Magnitude of data science & big data in fitness care. AIP Conf. Proc. 2025, 3162, 020020. [Google Scholar]
- Kumar, A.; Gupta, R.; Kumar, S.; Dutta, K.; Rani, M. Securing IoMT-based healthcare system: Issues, challenges, and solutions. In Artificial Intelligence and Cybersecurity in Healthcare Cyber Physical Systems; Agrawal, R., Rathore, P.S., Devarajan, G.G., Divivedi, R.R., Eds.; Scrivener Publishing LLC: Beverly, MA, USA, 2025; pp. 17–56. [Google Scholar]
- Du, M.; Li, Z.; Bian, L.; Randriamahazaka, H.; Chen, W. Two-dimensional materials van der Waals assembly enabling scalable smart textiles. Mater. Sci. Eng. R Rep. 2025, 163, 100915. [Google Scholar] [CrossRef]
- Ibrahim, Y.; Abdel-Malek, M.A.; Azab, M.; Rizk, M.R. Privacy-preserved mutually-trusted 5G communications in presence of pervasive attacks. Internet Things 2025, 30, 101491. [Google Scholar] [CrossRef]
- Wang, W.; Bo, X.; Li, W.; Eldaly, A.B.M.; Wang, L.; Li, W.J.; Chan, L.L.H.; Daoud, W.A. Triboelectric Bending Sensors for AI-Enabled Sign Language Recognition. Adv. Sci. 2025, 12, 2408384. [Google Scholar] [CrossRef]
- Lakshmi, S.G.; Lalitha, C.N.; Lavanya, S.; Vijaya, L.S.; Sri Lakshmi, P.S. IOT-enabled cloud solutions for reliable health monitoring. In Emerging Trends in Computer Science and Its Application; CRC Press: Boca Raton, FL, USA, 2025; pp. 278–282. [Google Scholar]
- Selem, M.; Jemili, F.; Korbaa, O. Deep learning for intrusion detection in IoT networks. Peer-Peer Netw. Appl. 2025, 18, 22. [Google Scholar] [CrossRef]
- Rezaee, K.; Yang, X.; Khosravi, M.R.; Zhang, R.; Lin, W.; Jeon, G. Fusion-based learning for stress recognition in smart home: An IoMT framework. Build. Environ. 2022, 216, 108988. [Google Scholar] [CrossRef]
- Qu, Q.; Sun, H.; Chen, Y. Smart healthcare at home in the era of IoMT. In Internet of Things—New Insights; IntechOpen: London, UK, 2023. [Google Scholar]
- Komalasari, R. Ambient Assisted Living (AAL) Systems to Help Older People. In Exploring Future Opportunities of Brain-Inspired Artificial Intelligence; IGI Global: Hershey, PA, USA, 2023; pp. 84–99. [Google Scholar]
- Bedón-Molina, J.; Lopez, M.J.; Derpich, I.S. A home-based smart health model. Adv. Mech. Eng. 2020, 12, 1687814020935282. [Google Scholar] [CrossRef]
- Cheng, C.K.; Bakar, H.A.; Gollasch, M.; Huang, Y. Perivascular Adipose Tissue: The Sixth Man of the Cardiovascular System. Cardiovasc. Drugs Ther. 2018, 32, 481–502. [Google Scholar] [CrossRef]
- Cáceres, C.; Rosário, J.M.; Amaya, D. Proposal of a smart hospital based on Internet of Things (IoT) concept. In Proceedings of the Processing and Analysis of Biomedical Information: First International SIPAIM Workshop, SaMBa 2018, Held in Conjunction with MICCAI 2018, Granada, Spain, 20 September 2018; Revised Selected Papers 1 2019. pp. 93–104. [Google Scholar]
- Kang, S.; Baek, H.; Jung, E.; Hwang, H.; Yoo, S. Survey on the demand for adoption of Internet of Things (IoT)-based services in hospitals: Investigation of nurses’ perception in a tertiary university hospital. Appl. Nurs. Res. 2019, 47, 18–23. [Google Scholar] [CrossRef] [PubMed]
- Zhang, N.; Wang, Y.; Zhang, H.; Fang, H.; Li, X.; Li, Z.; Gong, Z. Application of interpretable machine learning algorithms to predict macroangiopathy risk in Chinese patients with type 2 diabetes mellitus. Sci. Rep. 2025, 15, 16393. [Google Scholar] [CrossRef] [PubMed]
- Li, N.; Ou, J.; He, H.; He, J.; Zhang, L.; Peng, Z.; Jiang, N. Exploration of a machine learning approach for diagnosing sarcopenia among Chinese community-dwelling older adults using sEMG-based data. J. Neuroeng. Rehabil. 2024, 21, 69. [Google Scholar] [CrossRef] [PubMed]
- Abdullah, M.I.; Hao, S.K.; Abdullah, I.; Faizah, S. Parkinson’s Disease Symptom Detection using Hybrid Feature Extraction and Classification Model. In Proceedings of the 2023 IEEE 14th Control and System Graduate Research Colloquium, ICSGRC 2023—Conference Proceeding, Shah Alam, Malaysia, 5 August 2023; pp. 93–98. [Google Scholar]
- Ding, Z.; Zhang, L.; Zhang, Y.; Yang, J.; Luo, Y.; Ge, M.; Chen, C. A Supervised Explainable Machine Learning Model for Perioperative Neurocognitive Disorder in Liver-Transplantation Patients and External Validation on the Medical Information Mart for Intensive Care IV Database: Retrospective Study. J. Med. Internet Res. 2025, 27, e55046. [Google Scholar] [CrossRef]
- Liang, L.; Liang, X.; Yu, X.; Xiang, W. Bioinformatic Analyses and Integrated Machine Learning to Predict Prognosis and Therapeutic Response Based on E3 Ligase-Related Genes in Colon Cancer. J. Cancer 2024, 15, 5376–5395. [Google Scholar] [CrossRef]
- Kumar, R.; Garg, S.; Kaur, R.; Johar, M.G.M.; Singh, S.; Menon, S.V.; Kumar, P.; Hadi, A.M.; Hasson, S.A.; Lozanović, J. A comprehensive review of machine learning for heart disease prediction: Challenges, trends, ethical considerations, and future directions. Front. Artif. Intell. 2025, 8, 1583459. [Google Scholar] [CrossRef]
- Coskuner-Weber, O.; Alpsoy, S.; Yolcu, O.; Teber, E.; de Marco, A.; Shumka, S. Metagenomics studies in aquaculture systems: Big data analysis, bioinformatics, machine learning and quantum computing. Comput. Biol. Chem. 2025, 118, 108444. [Google Scholar] [CrossRef]
- Sharma, P.; Sharma, P.; Sharma, K.; Varma, V.; Patel, V.; Sarvaiya, J.; Tavethia, J.; Mehta, S.; Bhadania, A.; Patel, I.; et al. Revolutionizing Utility of Big Data Analytics in Personalized Cardiovascular Healthcare. Bioengineering 2025, 12, 463. [Google Scholar] [CrossRef]
- Liu, Z.; Si, L.; Shi, S.; Li, J.; Zhu, J.; Lee, W.H.; Wang, G. Classification of Three Anesthesia Stages Based on Near-Infrared Spectroscopy Signals. IEEE J. Biomed. Health Informat. 2024, 28, 5270–5279. [Google Scholar] [CrossRef]
- Mahawar, K.; Rattan, P.; Jalamneh, A.; Ab Yajid, M.S.; Abdeljaber, O.; Kumar, R.; Lasisi, A.; Ammarullah, M.I. Employing artificial bee and ant colony optimization in machine learning techniques as a cognitive neuroscience tool. Sci. Rep. 2025, 15, 10172. [Google Scholar] [CrossRef]
- Wang, F. Adaptive semi-supervised recursive tree partitioning: The ART towards large scale patient indexing in personalized healthcare. J. Biomed. Inform. 2015, 55, 41–54. [Google Scholar] [CrossRef]
- Tsay, D.; Patterson, C. From Machine Learning to Artificial Intelligence Applications in Cardiac Care: Real-World Examples in Improving Imaging and Patient Access. Circulation 2018, 138, 2569–2575. [Google Scholar] [CrossRef]
- Aris-Brosou, S.; Kim, J.; Li, L.; Liu, H. Predicting the reasons of customer complaints: A first step toward anticipating quality issues of in vitro diagnostics assays with machine learning. JMIR Med. Inform. 2018, 6, e34. [Google Scholar] [CrossRef] [PubMed]
- Moreira, M.W.L.; Rodrigues, J.J.P.C.; Kumar, N.; Saleem, K.; Illin, I.V. Postpartum depression prediction through pregnancy data analysis for emotion-aware smart systems. Inf. Fusion 2019, 47, 23–31. [Google Scholar] [CrossRef]
- Rim, T.H.; Soh, Z.D.; Tham, Y.C.; Yang, H.H.S.; Lee, G.; Kim, Y.; Nusinovici, S.; Ting, D.S.W.; Wong, T.Y.; Cheng, C.Y. Deep Learning for Automated Sorting of Retinal Photographs. Ophthalmol. Retin. 2020, 4, 793–800. [Google Scholar] [CrossRef] [PubMed]
- Bolhasani, H.; Mohseni, M.; Rahmani, A.M. Deep learning applications for IoT in health care: A systematic review. Inform. Med. Unlocked 2021, 23, 100550. [Google Scholar] [CrossRef]
- Saleh, M.; Abbas, M.; Prud’Homm, J.; Somme, D.; Le Bouquin Jeannes, R. A Reliable Fall Detection System Based on Analyzing the Physical Activities of Older Adults Living in Long-Term Care Facilities. IEEE Trans. Neural Syst. Rehabil. Eng. 2021, 29, 2587–2594. [Google Scholar] [CrossRef]
- Montomoli, J.; Hilty, M.P.; Ince, C. Artificial intelligence in intensive care: Moving towards clinical decision support systems. Minerva Anestesiol. 2022, 88, 1066–1072. [Google Scholar] [CrossRef]
- Nicolucci, A.; Romeo, L.; Bernardini, M.; Vespasiani, M.; Rossi, M.C.; Petrelli, M.; Ceriello, A.; Di Bartolo, P.; Frontoni, E.; Vespasiani, G. Prediction of complications of type 2 Diabetes: A Machine learning approach. Diabetes Res. Clin. Pract. 2022, 190, 110013. [Google Scholar] [CrossRef]
- Fatema, N.; Malik, H.; Ahmad, W. Data driven intelligent model for quality management in healthcare. J. Intell. Fuzzy Syst. 2022, 42, 1155–1169. [Google Scholar] [CrossRef]
- Singh, G.; Violi, V.; Fisichella, M. Federated Learning to Safeguard Patients Data: A Medical Image Retrieval Case. Big Data Cogn. Comput. 2023, 7, 18. [Google Scholar] [CrossRef]
- Abidi, M.H.; Umer, U.; Mian, S.H.; Al-Ahmari, A. Big Data-Based Smart Health Monitoring System: Using Deep Ensemble Learning. IEEE Access 2023, 11, 114880–114903. [Google Scholar] [CrossRef]
- Manchadi, O.; Ben-Bouazza, F.E.; Jioudi, B. Predictive Maintenance in Healthcare System: A Survey. IEEE Access 2023, 11, 61313–61330. [Google Scholar] [CrossRef]
- Alqahtani, S.; Luo, S.; Alanazi, M.; Shaukat, K.; Alsubaie, M.G.; Amer, M. Machine Learning for Predicting Intradialytic Hypotension: A Survey Review. Int. J. Adv. Comput. Sci. Appl. 2024, 15, 282–293. [Google Scholar] [CrossRef]
- Shao, Y.; Zhang, S.; Raman, V.K.; Patel, S.S.; Cheng, Y.; Parulkar, A.; Lam, P.H.; Moore, H.; Sheriff, H.M.; Fonarow, G.C.; et al. Artificial intelligence approaches for phenotyping heart failure in U.S. Veterans Health Administration electronic health record. ESC Heart Fail. 2024, 11, 3155–3166. [Google Scholar] [CrossRef]
- Lin, X.; Duan, G.; Huang, J.; Zhou, Q.; Huang, H.; Xiao, J.; Xu, Z.; Shen, H.; Zhuo, H. Construction of A Smart Hospital Innovation Platform Using the Internet + Technology. Altern. Ther. Health Med. 2024, 30, 495–505. [Google Scholar]
- Bartoszewicz, M.; Prokop, P.; Kosieradzki, M.; Fiedor, P. Are Current Educational and Therapeutic Programs, Directed at Rare Disease Transplant Candidates and Recipients, Sufficient to Support Them on the Path From Diagnosis to Life After Allogenic Transplantation?—Recommendations for Member State Policymakers. Transplant. Proc. 2024, 56, 907–909. [Google Scholar] [CrossRef]
- Joshi, A. Big data and AI for gender equality in health: Bias is a big challenge. Front. Big Data 2024, 7, 1436019. [Google Scholar] [CrossRef]
- Balogh, D.B.; Hudelist, G.; Bļizņuks, D.; Raghothama, J.; Becker, C.M.; Horace, R.; Krentel, H.; Horne, A.W.; Bourdel, N.; Marki, G.; et al. FEMaLe: The use of machine learning for early diagnosis of endometriosis based on patient self-reported data—Study protocol of a multicenter trial. PLoS ONE 2024, 19, e0300186. [Google Scholar] [CrossRef]
- Finazzi Agrò, E.; Rosato, E.; Kheir, G.B.; Rademakers, K.; Averbeck, M.A.; Tarcan, T.; Hashim, H.; Gammie, A.; Sinha, S.; Song, Q.X.; et al. How Can We Show That Artificial Intelligence May Improve Our Assessment and Management of Lower Urinary Tract Dysfunctions?—ICI-RS 2024. Neurourol. Urodyn. 2025, 44, 616–621. [Google Scholar] [CrossRef]
- Yajie, L.; Johar, M.G.M.; Hajamydeen, A.I. Poultry disease early detection methods using deep learning technology. Indones. J. Electr. Eng. Comput. Sci. 2023, 32, 1712–1723. [Google Scholar] [CrossRef]
- Dissanayake, K.; Johar, M.G.M. Comparative study on heart disease prediction using feature selection techniques on classification algorithms. Appl. Comput. Intell. Soft Comput. 2021, 2021, 1–17. [Google Scholar] [CrossRef]
- UK Biobank. About Us—UK Biobank; UK Biobank: Stockport, UK, 2025. [Google Scholar]
- Collins, R. UK Biobank is safely sharing health data to drive medical research. The Guardian, 18 April 2025. [Google Scholar]
- Ciborowski, J. NVIDIA and GE HealthCare Collaborate to Advance the Development of Autonomous Diagnostic Imaging With Physical AI. NVIDIA Newsroom, 18 March 2025. [Google Scholar]
- Islam, M.D.S.; Liu, D.; Wang, K.; Zhou, P.; Yu, L.; Wu, D. A Case Study of HealthCare Platform using Big Data Analytics and Machine Learning. In Proceedings of the 2019 3rd High Performance Computing and Cluster Technologies Conference, Guangzhou, China, 22–24 June 2019; pp. 139–146. [Google Scholar]
- Wan, A.E.; Baber Khan, M.S.; Xian Teo, B.S.; Khan, J.; Abdullah, I.; Kaleemullah, M.; Asmani, F.; Suofeiya, M.; Al Dhalli, S.; Kasim, Z.; et al. Screening of antioxidant and antibacterial activity of methanolic extract of ipomoea aquatica leaf and stem against bacteria causes skin infection. Int. J. Med. Toxicol. Leg. Med. 2020, 23, 169–178. [Google Scholar] [CrossRef]
- Qian, T.; Zhu, S.; Hoshida, Y. Use of big data in drug development for precision medicine: An update. Expert. Rev. Precis. Med. Drug Dev. 2019, 4, 189–200. [Google Scholar] [CrossRef] [PubMed]
- Jain, A.K.; Aneja, S.; Fuller, C.D.; Dicker, A.P.; Chung, C.; Kim, E.; Kirby, J.S.; Quon, H.; Lam, C.J.K.; Louv, W.C.; et al. Provider Engagement in Radiation Oncology Data Science: Workshop Report. JCO Clin. Cancer Inf. 2020, 4, 700–710. [Google Scholar] [CrossRef] [PubMed]
- Oncora Medical. Oncology AI Solutions. 2025. Available online: https://www.oncora.ai/ (accessed on 7 May 2025).
- IQVIA Inc. IQVIA NLP Data Factory: Enterprise NLP Made Easy [Video]. 2021. Available online: https://www.iqvia.com/library/videos/iqvia-nlp-data-factory (accessed on 25 July 2025).
- IQVIA Inc. Big Data Analytics for Population Health [Case Study]. 7 March 2023. Available online: https://www.iqvia.com/library/case-studies/nlp-big-data-analytics-for-population-health (accessed on 9 May 2025).
- IQVIA Inc. IQVIA Natural Language Processing (NLP) Risk Adjustment Solution [Fact Sheet]. 3 January 2023. Available online: https://www.iqvia.com/library/fact-sheets/nlp-risk-adjustment-solution (accessed on 15 May 2025).
- López-Martínez, F.; Núñez-Valdez, E.R.; García-Díaz, V.; Bursac, Z. A Case Study for a Big Data and Machine Learning Platform to Improve Medical Decision Support in Population Health Management. Algorithms 2020, 13, 102. [Google Scholar] [CrossRef]
- Salari, M.; Rahmani, B. Machine Learning for Everyone: Simplifying Healthcare Analytics with BigQuery ML. arXiv 2025, arXiv:2502.07026. [Google Scholar] [CrossRef]
- Hennebelle, A.; Materwala, H.; Ismail, L. HealthEdge: A Machine Learning-Based Smart Healthcare Framework for Prediction of Type 2 Diabetes in an Integrated IoT, Edge, and Cloud Computing System. Procedia Comput. Sci. 2023, 220, 331–338. [Google Scholar] [CrossRef]
- Radiological Society of North America (RSNA). AI Predicts Heart Disease Risk Using Single X-Ray [Press Release]. 29 November 2022. Available online: https://press.rsna.org/timssnet/media/pressreleases/14_pr_target.cfm?id=2388 (accessed on 14 May 2025).
- Wang, Y.; Shen, Y.; Li, J.; Wang, T.; Peng, J.; Shang, X. Enhanced RNA secondary structure prediction through integrative deep learning and structural context analysis. Nucleic Acids Res. 2025, 53, gkaf533. [Google Scholar] [CrossRef]
- Li, H.; Wang, Z.; Guan, Z.; Miao, J.; Li, W.; Yu, P.; Molina Jimenez, C. UCFNNet: Ulcerative colitis evaluation based on fine-grained lesion learner and noise suppression gating. Comput. Methods Programs Biomed. 2024, 247, 108080. [Google Scholar] [CrossRef] [PubMed]
- An, Q.; Chen, W.; Shao, W. A Deep Convolutional Neural Network for Pneumonia Detection in X-ray Images with Attention Ensemble. Diagnostics 2024, 14, 390. [Google Scholar] [CrossRef]
- Mabrouk, A.; Díaz Redondo, R.P.; Dahou, A.; Abd Elaziz, M.; Kayed, M. Pneumonia Detection on Chest X-ray Images Using Ensemble of Deep Convolutional Neural Networks. Appl. Sci. 2022, 12, 6448. [Google Scholar] [CrossRef]
- Loukou, E. Fitness Trackers Could Spot Earliest Signs of Alzheimer’s BEFORE Symptoms Start. The Sun, 19 March 2024. Available online: https://www.thesun.co.uk/health/26783341/fitness-trackers-signs-of-alzheimers-before-symptoms-start (accessed on 11 May 2025).
- Iqbal, U.; Tanweer, A.; Rahmanti, A.R.; Greenfield, D.; Lee, L.T.J.; Li, Y.C.J. Impact of large language model (ChatGPT) in healthcare: An umbrella review and evidence synthesis. J. Biomed. Sci. 2025, 32, 45. [Google Scholar] [CrossRef] [PubMed]
- Akbasli, I.T.; Birbilen, A.Z.; Teksam, O. Leveraging large language models to mimic domain expert labeling in unstructured text-based electronic healthcare records in non-english languages. BMC Med. Inform. Decis. Mak. 2025, 25, 154. [Google Scholar] [CrossRef] [PubMed]
- Khan, B.; Talha Khalid, R.; Ul Wara, K.; Hasan Masrur, M.; Khan, S.; Khan, W.U.; Amara, U.; Abdullah, S. Reshaping the healthcare world by AI-integrated wearable sensors following COVID-19. Chem. Eng. J. 2025, 505, 159478. [Google Scholar] [CrossRef]
- Yousefi, M.; Akhbari, M.; Mohamadi, Z.; Karami, S.; Dasoomi, H.; Atabi, A.; Sarkeshikian, S.A.; Abdoullahi Dehaki, M.; Bayati, H.; Mashayekhi, N.; et al. Machine learning based algorithms for virtual early detection and screening of neurodegenerative and neurocognitive disorders: A systematic-review. Front. Neurol. 2024, 15, 1413071. [Google Scholar] [CrossRef]
- Singh, S.G.; Das, D.; Barman, U.; Saikia, M.J. Early Alzheimer’s Disease Detection: A Review of Machine Learning Techniques for Forecasting Transition from Mild Cognitive Impairment. Diagnostics 2024, 14, 1759. [Google Scholar] [CrossRef]
- Wang, K.; Tan, B.; Wang, X.; Qiu, S.; Zhang, Q.; Wang, S.; Yen, Y.T.; Jing, N.; Liu, C.; Chen, X.; et al. Machine learning-assisted point-of-care diagnostics for cardiovascular healthcare. Bioeng. Transl. Med. 2025, 10, e70002. [Google Scholar] [CrossRef]
- Bhattacherjee, A.; Badhan, A.K. Convergence of Data Analytics, Big Data, and Machine Learning: Applications, Challenges, and Future Direction. In Data Analytics and Machine Learning: Navigating the Big Data Landscape; Springer Nature: Singapore, 2024; Volume 145, pp. 317–334. [Google Scholar]
- McComb, M.; Bies, R.; Ramanathan, M. Machine learning in pharmacometrics: Opportunities and challenges. Br. J. Clin. Pharmacol. 2022, 88, 1482–1499. [Google Scholar] [CrossRef]
- Kaur, R.; Kumar, R.; Aggarwal, H. Systematic Review of Artificial Intelligence, Machine Learning, and Deep Learning in Machining Operations: Advancements, Challenges, and Future Directions. Arch. Comput. Methods Eng. 2025, 1–54. [Google Scholar] [CrossRef]
- Tsang, G.; Xie, X.; Zhou, S.M. Harnessing the Power of Machine Learning in Dementia Informatics Research: Issues, Opportunities, and Challenges. IEEE Rev. Biomed. Eng. 2020, 13, 113–129. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Liu, C.; Chen, X.; Zhang, Y.; Li, Y.; Hu, X. Effects of Web-Based Acceptance and Commitment Therapy on Health-Related Outcomes Among Patients With Lung Cancer: A Feasibility Randomized Controlled Trial. Psycho-Oncol. 2024, 33, e70045. [Google Scholar] [CrossRef] [PubMed]
- Swanson, K.; Wu, E.; Zhang, A.; Alizadeh, A.A.; Zou, J. From patterns to patients: Advances in clinical machine learning for cancer diagnosis, prognosis, and treatment. Cell 2023, 186, 1772–1791. [Google Scholar] [CrossRef] [PubMed]
- Alafif, T.; Tehame, A.M.; Bajaba, S.; Barnawi, A.; Zia, S. Machine and deep learning towards COVID-19 diagnosis and treatment: Survey, challenges, and future directions. Int. J. Environ. Res. Public. Health 2021, 18, 1117. [Google Scholar] [CrossRef] [PubMed]
- Giger, M.L. Machine learning in medical imaging. J. Am. Coll. Radiol. 2018, 15, 512–520. [Google Scholar] [CrossRef]
- Kumar, A.; Bi, L.; Kim, J.; Feng, D.D. Machine learning in medical imaging. In Biomedical Information Technology; Elsevier: Amsterdam, The Netherlands, 2020; pp. 167–196. [Google Scholar]
- Vamathevan, J.; Clark, D.; Czodrowski, P.; Dunham, I.; Ferran, E.; Lee, G.; Li, B.; Madabhushi, A.; Shah, P.; Spitzer, M. Applications of machine learning in drug discovery and development. Nat. Rev. Drug Discov. 2019, 18, 463–477. [Google Scholar] [CrossRef]
- Mak, K.-K.; Wong, Y.-H.; Pichika, M.R. Artificial intelligence in drug discovery and development. In Drug Discovery and Evaluation: Safety and Pharmacokinetic Assays; Hock, F.J., Pugsley, M.K., Eds.; Springer: Cham, Switzerland, 2024; pp. 1461–1498. [Google Scholar] [CrossRef]
- Al Meslamani, A.Z.; Sobrino, I.; de la Fuente, J. Machine learning in infectious diseases: Potential applications and limitations. Ann. Med. 2024, 56, 2362869. [Google Scholar] [CrossRef]
- Badal, V.D.; Depp, C.A. Natural language processing of medical records: New understanding of suicide ideation by dementia subtypes: Commentary on “Suicidal ideation in dementia: Associations with neuropsychiatric symptoms and subtype diagnosis” by Naismith et al. Int. Psychogeriatr. 2022, 34, 319–321. [Google Scholar] [CrossRef]
- Kourou, K.; Exarchos, K.P.; Papaloukas, C.; Sakaloglou, P.; Exarchos, T.; Fotiadis, D.I. Applied machine learning in cancer research: A systematic review for patient diagnosis, classification and prognosis. Comput. Struct. Biotechnol. J. 2021, 19, 5546–5555. [Google Scholar] [CrossRef]
- Rahmani, A.M.; Yousefpoor, E.; Yousefpoor, M.S.; Mehmood, Z.; Haider, A.; Hosseinzadeh, M.; Ali Naqvi, R. Machine learning (ML) in medicine: Review, applications, and challenges. Mathematics 2021, 9, 2970. [Google Scholar] [CrossRef]
- Afrifa-Yamoah, E.; Adua, E.; Peprah-Yamoah, E.; Anto, E.O.; Opoku-Yamoah, V.; Acheampong, E.; Macartney, M.J.; Hashmi, R. Pathways to chronic disease detection and prediction: Mapping the potential of machine learning to the pathophysiological processes while navigating ethical challenges. Chronic Dis. Transl. Med. 2025, 11, 1–21. [Google Scholar] [CrossRef] [PubMed]
- Red, G.V.; Palaoag, T.D. Ethical and Privacy Issues in the Use of Machine Learning for Personalized Care for Elderly Patients. Int. J. Eng. Trends Technol. 2024, 72, 32–42. [Google Scholar] [CrossRef]
- Kostick-Quenet, K.; Estep, J.; Blumenthal-Barby, J.S. Ethical Concerns for Remote Computer Perception in Cardiology: New Stages for Digital Health Technologies, Artificial Intelligence, and Machine Learning. Circ. Cardiovasc. Qual. Outcomes 2024, 17, E010717. [Google Scholar] [CrossRef]
- Hajlaoui, R.; Dhahri, S.; Mahfoudhi, S.; Moulahi, T.; Alotibi, G. Protecting machine learning systems using blockchain: Solutions, challenges and future prospects. Multimed. Tools Appl. 2025, 20, 22755–22782. [Google Scholar] [CrossRef]
- Geerthik, S.; Senthil, G.A.; Illakiya, G.; Naveen Raj, S.; Arun Kumar, B. Future Navigation Demand Trends: Accurate Ride Request Forecasting Optimization Using Machine Learning. In Proceedings of the 2024 3rd International Conference on Smart Technologies and Systems for Next Generation Computing, ICSTSN 2024, Villupuram, India, 18–19 July 2024. [Google Scholar]









| Focus Area | Proposed Approach | Key Findings | Challenges Addressed | Future Prospects | Study Evaluation | Ref. |
|---|---|---|---|---|---|---|
| Human Activity Recognition (HAR) Using Sensor Data | LSTM-based HAR model Attention and squeeze-and- excitation blocks | 99% accuracy in activity recognition; improved feature extraction lower computational complexity | Variability in sensor data; imbalanced Datasets; high computational cost | Enhancing real-world applications of HAR by improving model adaptability and efficiency | Well-defined model; limited to specific dataset; 99% on public HAR dataset | [24] |
| IoT-based Clinical Decision Support System | Cloud-based C-IoT model with ANN and lightweight encryption for secure health monitoring | 91% diagnostic accuracy; health monitoring; enhanced data security | Data security; accuracy | Expanding the model for Society 5.0 by integrating AI-driven secure diagnostics | Small-scale deployment; lacks generalizability; moderate reproducibility | [25] |
| Intrusion Detection in Smart Healthcare IoT Systems | IADCL framework using feature selection (IRKO), AConBN classifier, and SA-HHO optimization | High accuracy in cyberattack detection using public datasets like CIC-IDS 2017 and 2018 | Lack of robust security in resource-constrained IoTM devices | Improving security mechanisms for real-time IoT-based healthcare systems | Benchmark datasets used (CIC-IDS); good methodology; reproducible | [26] |
| AI-Enabled Smart Acne Diagnosis | Convolutional neural network (CNN)-based cloud-connected IoT device for facial acne severity assessment | AI-driven real-time acne tracking with geographic adaptability, bridging e-healthcare access gaps | Delayed/inaccurate acne diagnosis and lack of remote dermatological consultation | Expanding AI-based dermatology solutions for various skin conditions | Small sample; limited clinical validation; strong conceptual design | [27] |
| Privacy-Preserving Authentication in IoMT Healthcare | Blockchain-based double anonymity strategy with cross-hospital authentication | Enhanced privacy, decentralization, and a 23–87% reduction in computational costs | Privacy breaches, untraceability, single point of failure in authentication | Implementing blockchain for broader healthcare interoperability | High potential; lacks empirical multi-hospital deployment proof | [28] |
| Unconstrained Health Monitoring via BCG | Smart wireless flexible sensing system for heart and respiration monitoring | High-sensitivity flexible sensor capturing subtle physiological signals | Discomfort and movement limitations in traditional long-term monitoring | Developing advanced flexible sensors for more wearable health monitoring applications | Strong sensing performance; tested in controlled setup | [29] |
| Nursing Professional Values and Job Satisfaction | Survey-based analysis using SEM-PLS modeling | Activism and justice are the key influencers of job satisfaction among Vietnamese nurses | Limited professional development and high patient-to-nurse ratios | Studying nursing satisfaction factors across diverse healthcare environments | Statistical rigor; limited to Vietnam; low generalizability | [30] |
| Secure IoT Communication in Smart Healthcare | Three-factor lightweight mutual authentication scheme with elliptic curve cryptography | Improved security with minimal computational cost, meeting 15 security criteria | Security vulnerabilities in resource-constrained IoT healthcare environments | Enhancing lightweight cryptographic protocols for broader IoT applications | Good cryptographic model; theoretical validation; real-world deployment pending | [31] |
| Focus Area | Proposed Approach | Key Findings | Challenges Addressed | Future Prospects | Study Evaluation | Ref. |
|---|---|---|---|---|---|---|
| Big Data and Gene Therapy in Smart Healthcare | Wearables and tracking devices; early health risk prediction BDA for gene therapy | Early risk identification; before genetic data is available; smart data processing for cost-effective healthcare | Integration of multi-source data; affordability of advanced healthcare analytics | Enhancing predictive healthcare models; expanding data-driven gene therapy applications | Small pilot studies; scalability untested | [37] |
| Security and Privacy in Smart Healthcare Systems | Comprehensive review of SHS security challenges and proposed solutions | Identifies key risks Cyber threats, privacy issues, and attack vulnerabilities in IoMT | Scalability; complexity; securing interconnected smart healthcare devices | Developing robust security frameworks for safeguarding IoMT-based smart healthcare | Synthesis without empirical validation | [38] |
| Smart Textiles for Healthcare and IoT Integration | Van der Waals (vdW) force-based 2D functional material integration with textiles | Preserves textile flexibility Adding intelligence; applications (healthcare, human–machine interaction) | Scalability; performance stability Safety concerns in commercial applications | Expansion into fully connected IoT-integrated wearable healthcare systems | Lab prototypes; real-world use pending | [39] |
| 5G Security for IoT and Wearables | Security enhancements in 5G-AKA authentication protocol | Improved user authentication and reduced exposure to security vulnerabilities | Lack of mutual authentication; privacy risks in 5G communication | Developing more secure and resilient authentication mechanisms for next-gen networks | Theoretical analysis; real-world deployment needed | [40] |
| Self-Powered Wearable Sensors | Triboelectric sensors with AI-based LSTM for sign language recognition | Achieved 96.15% recognition accuracy for sign language patterns | Eliminating external power needs while maintaining accuracy | Expanding self-powered sensors for diverse wearable applications | Limited dataset; controlled conditions | [41] |
| Secure IoT-based Health Monitoring | Cloud and IoT-based secure health monitoring system | Enhanced security and privacy for wearable healthcare technologies | Data privacy concerns and secure remote patient tracking | Improving security standards for cloud-integrated health monitoring | Limited pilot; reproducibility unclear | [42] |
| Ensemble Learning for IoT Intrusion Detection | Bagging-based IDS integrating DNN and CNN for IoT security | Improved threat detection using the Edge-IIoTset dataset | Balancing IDS accuracy with computational efficiency | Enhancing real-time IoT security using AI-driven ensemble models | Good on benchmark dataset; edge deployment pending | [43] |
| Aspect | Wearable Devices | Home-Based Devices | Hospital-Based Devices |
|---|---|---|---|
| Data Collection | Continuous real-time monitoring (e.g., heart rate, steps, SpO2) | Periodic monitoring (e.g., BP monitors, glucose meters) | High-frequency; high-resolution medical data (e.g., MRI, CT scans, ECG) |
| Data Volume | High but fragmented | Moderate to high | Very high (large datasets per patient) |
| Data Variety | Limited (mainly physiological data) | Moderate (includes environmental and physiological data) | Extensive (medical imaging, lab tests, patient history) |
| Data Velocity | Real-time streaming | Near real-time to scheduled readings | Batch processing and real-time for critical care |
| Privacy and Security | Risk of data breaches via cloud or mobile apps | Moderate security concerns (home network vulnerabilities) | High-security standards (hospital IT infrastructure) |
| ML Applications | Activity recognition; anomaly detection; predictive analytics | Disease monitoring; early warning systems | Diagnosis; precision medicine; treatment planning |
| ML Model Complexity | Lightweight models (on-device processing) | Moderate complexity (edge/cloud computing) | High complexity (DL AI-driven diagnostics) |
| Big Data Challenges | Data fragmentation, interoperability issues | Data inconsistency; integration challenges | High computational demands; need for scalable storage |
| Computational Resources | Low (wearables have limited processing power) | Moderate (some devices leverage cloud/edge computing) | High (dedicated servers, GPUs, Cloud computing) |
| Integration with Healthcare Systems | Limited (mostly user-driven insights) | Moderate (telemedicine and EHR integration) | Full integration with EHRs and clinical workflows |
| Study Focus/ Design | Application Domain/ Dataset Size | ML Technique/ Model | Key Contribution/ Reproducibility | Diagnostic Relevance | Ref. |
|---|---|---|---|---|---|
| Patient similarity evaluation framework | General healthcare/large-scale patient data | Adaptive semi-supervised recursive tree partitioning (ART) | Efficient patient similarity indexing and retrieval | Supports prognosis, risk assessment, and comparative effectiveness | [61] |
| AI in operational delivery improvement | Cardiovascular care/healthcare systems | General AI platforms and ML algorithms | Integration of AI in cardiac care operations | Supports diagnosis and risk stratification | [62] |
| Complaint prediction in diagnostic systems | In-vitro diagnostics/QC data over 90 days | Decision trees, adaptive boosting | Prediction of customer complaints using QC data | Indirect diagnostic support through QC performance monitoring | [63] |
| Emotion-aware postpartum depression detection | Maternal health/biomedical and sociodemographic data | Ensemble classifiers | Predicts postpartum depression risk | Enables early detection and intervention | [64] |
| Automated retinal image labeling | Ophthalmology/5000 SEED + public datasets | DL + rule-based classifier | RetiSort for high-accuracy retinal photo sorting | Aids diagnostic preprocessing | [65] |
| DL in IoT healthcare | Healthcare IoT/44 SLR papers | DL frameworks | Review of DL in healthcare IoT | General healthcare diagnostics | [66] |
| Fall detection from real-life data | Elderly care/400 days of real-life data | ML models | High-sensitivity fall detection system | Automatic fall detection and alert | [67] |
| ML in intensive care systems | ICU/general data | ML algorithms | Review of ML clinical decision support | Clinical decision support in ICUs | [68] |
| Prediction of diabetes complications | Diabetes/147,664 patients | XGBoost | Predicts short and long-term complications | Improves prognosis and care quality | [69] |
| Non-invasive liver fibrosis diagnosis | Hepatitis C/SLBs data | EMD + ANN-J48 | Hybrid intelligent classifier | Non-invasive diagnostic tool | [70] |
| Federated learning in healthcare | Healthcare/multi-center EHRs | Federated learning | Systematic study of FL in healthcare | Privacy-preserving diagnosis modeling | [71] |
| Elderly activity tracking | Elderly care/sensor data | HDCO + deep ensemble learning | High-accuracy activity recognition | Behavior monitoring for healthcare | [72] |
| Predictive maintenance of medical devices | Healthcare equipment/SLR data | ML + big data | Review of predictive maintenance techniques | Ensures device reliability | [73] |
| IDH prediction in dialysis | Dialysis/patient records | DL | Survey on ML for IDH | Preemptive diagnosis and prevention | [74] |
| HF phenotyping via AI | Heart failure/VA EHRs (20,000 pts) | NLP + ML (SVM) | Efficient HF identification using EHR | Improved diagnosis in HF registries | [75] |
| Smart hospital optimization | Hospital care/internal data | NLP + ML + BI | Optimized care, diagnostics, and cost | Enhances diagnostic processes | [76] |
| AI in rare disease transplant support | Rare diseases/Polish national databases | Big data + AI tools | Policy analysis and recommendations | Supports early diagnosis and treatment | [77] |
| ML in women’s health | Women’s health/review-based | ML + big data | Perspective on opportunities and biases | Personalized predictive healthcare | [78] |
| ML for endometriosis detection | Endometriosis/Lucy app (10,000 participants) | Machine learning | Real-world data analysis for earlier detection | Early diagnosis and personalized recommendations | [79] |
| AI in functional urology | Functional urology/UDS datasets | AI systems | Proposal and discussion on AI use | Improves diagnosis and personalized therapy | [80] |
| Healthcare Application | Role of Machine Learning | Big Data Challenges |
|---|---|---|
| Disease Diagnosis | Detects diseases like cancer, diabetes, and neurological disorders using medical imaging and patient data. | Data heterogeneity, interoperability, and privacy concerns. |
| Predictive Analytics | Forecasts disease outbreaks, patient deterioration, and risk factors. | High-dimensional data processing and real-time analytics. |
| Medical Imaging | Enhances anomaly detection in X-rays, MRIs, and CT scans using DL. | Large file sizes, data annotation, and storage limitations. |
| Drug Discovery and Development | Predicts molecular interactions, accelerates drug discovery, and optimizes clinical trials. | Data silos, computational complexity, and regulatory constraints. |
| Personalized Medicine | Tailors treatments based on genetics, lifestyle, and medical history. | Data integration from diverse sources, ethical concerns. |
| Remote Patient Monitoring | Analyzes wearable and home-based device data for early intervention. | Real-time processing, connectivity issues, and security risks. |
| EHR Management | Automates data extraction, summarization, and decision support. | Data inconsistency, duplication, and access control. |
| Clinical Decision Support | Assists in treatment recommendations using predictive models. | Data accuracy, bias in training data, and model interpretability. |
| Healthcare Chatbots and Virtual Assistants | Provides symptom checking, appointment scheduling, and medical advice. | NLP limitations, contextual understanding, and data privacy. |
| Surgical Assistance | Aids robotic surgeries with real-time guidance and precision enhancement. | Sensor data processing and integration with surgical workflows. |
| Mental Health Analysis | Detects depression, anxiety, and mood disorders using speech and text analysis. | Subjectivity in diagnosis, patient privacy, and data bias. |
| Fraud Detection and Security | Identifies fraudulent claims and cyber threats in healthcare data. | Anomaly detection in massive datasets, adversarial attacks. |
| Case Study | Application Area | Technologies Used | Key Outcomes |
|---|---|---|---|
| UK Biobank | Medical Research | BDA ML | Enhanced disease understanding through analysis of extensive health data from 500,000 participants. |
| NVIDIA and GE HealthCare | Diagnostic Imaging | AI ML | Improved diagnostic accuracy and efficiency in X-ray and ultrasound imaging. |
| Healthcare Platform | Disease Detection | BDA ML | Achieved over 95% accuracy in disease detection with a 90% cost reduction compared to traditional methods. |
| Oncology Drug Development | Drug Development | BDA | Streamlined drug discovery processes and personalized cancer treatments. |
| Oncora Medical | Oncology Workflows | BDAML | Enhanced treatment planning and decision-making in oncology through integrated data analysis. |
| IQVIA’s NLP Data Factory | Population Health | NLP BDA | Improved population risk stratification by extracting insights from unstructured health data. |
| Digital Health Platform in Colombia | Population Health Management | BDA ML | Enhanced decision-making and proactive healthcare interventions in resource-constrained settings. |
| BigQuery ML for Diabetes Prediction, Google Cloud | Diabetes Prediction | BigQuery ML SQL-based ML | Simplified development of predictive models for diabetes risk assessment. |
| HealthEdge | Type 2 Diabetes Prediction | ML IoT Edge and Cloud Computing | Enabled real-time diabetes risk prediction using integrated IoT-edge-cloud systems. |
| AI Predicting 10-Year Heart Disease Risk | Cardiovascular Risk Assessment | DL AI | Predicted 10-year risk of heart disease using single chest X-rays, aiding early intervention strategies. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rani, S.; Kumar, R.; Panda, B.S.; Kumar, R.; Muften, N.F.; Abass, M.A.; Lozanović, J. Machine Learning-Powered Smart Healthcare Systems in the Era of Big Data: Applications, Diagnostic Insights, Challenges, and Ethical Implications. Diagnostics 2025, 15, 1914. https://doi.org/10.3390/diagnostics15151914
Rani S, Kumar R, Panda BS, Kumar R, Muften NF, Abass MA, Lozanović J. Machine Learning-Powered Smart Healthcare Systems in the Era of Big Data: Applications, Diagnostic Insights, Challenges, and Ethical Implications. Diagnostics. 2025; 15(15):1914. https://doi.org/10.3390/diagnostics15151914
Chicago/Turabian StyleRani, Sita, Raman Kumar, B. S. Panda, Rajender Kumar, Nafaa Farhan Muften, Mayada Ahmed Abass, and Jasmina Lozanović. 2025. "Machine Learning-Powered Smart Healthcare Systems in the Era of Big Data: Applications, Diagnostic Insights, Challenges, and Ethical Implications" Diagnostics 15, no. 15: 1914. https://doi.org/10.3390/diagnostics15151914
APA StyleRani, S., Kumar, R., Panda, B. S., Kumar, R., Muften, N. F., Abass, M. A., & Lozanović, J. (2025). Machine Learning-Powered Smart Healthcare Systems in the Era of Big Data: Applications, Diagnostic Insights, Challenges, and Ethical Implications. Diagnostics, 15(15), 1914. https://doi.org/10.3390/diagnostics15151914







