Hyperpolarized Xenon-129 MRI: Narrative Review of Clinical Studies, Testing, and Implementation of Advanced Pulmonary In Vivo Imaging and Its Diagnostic Applications
Abstract
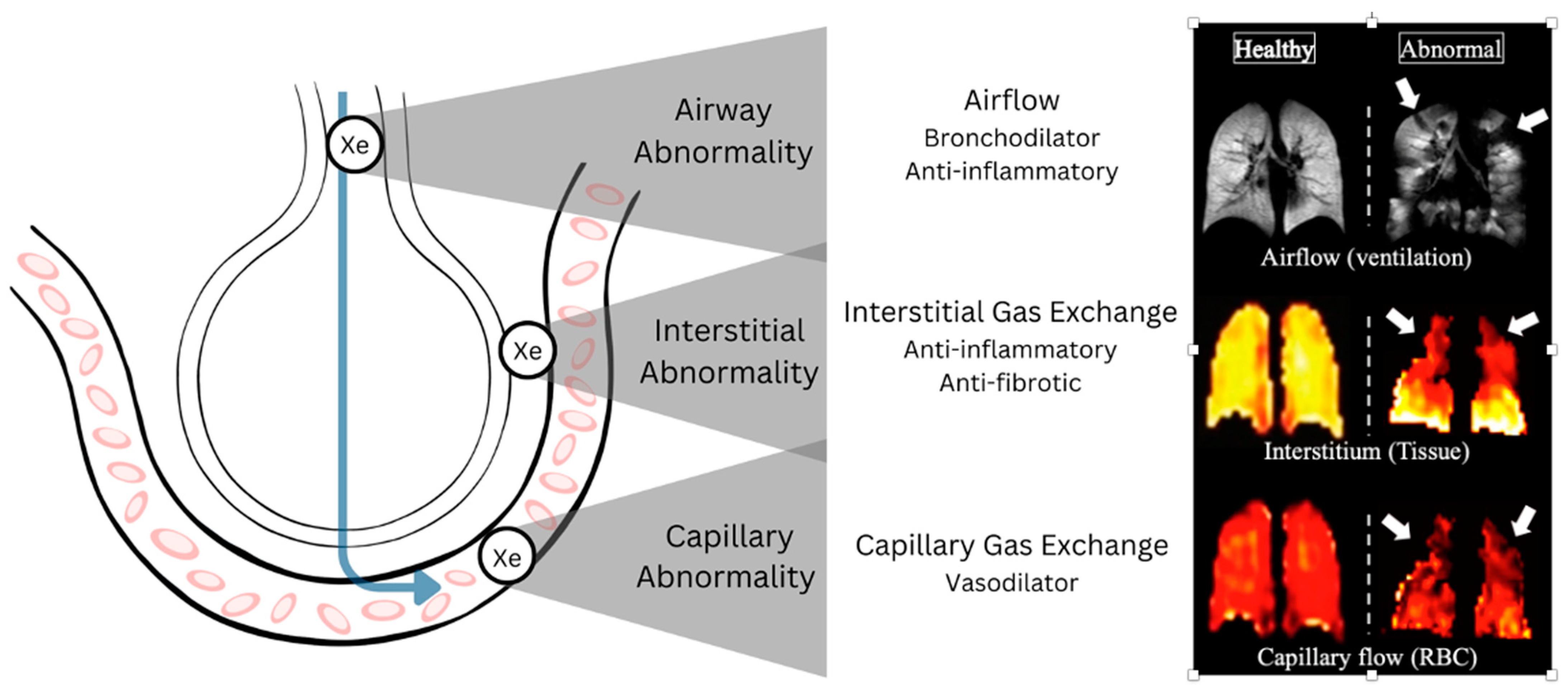
1. Overview of 129XeMRI
2. COPD
3. Asthma
4. Cystic Fibrosis (CF)
5. Idiopathic Pulmonary Fibrosis (IPF)
6. COVID-19
7. Miscellaneous Diseases
8. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Mugler, J.P.; Altes, T.A.; Ruset, I.C.; Dregely, I.M.; Mata, J.F.; Miller, G.W.; Ketel, S.; Ketel, J.; Hersman, F.W.; Ruppert, K. Simultaneous Magnetic Resonance Imaging of Ventilation Distribution and Gas Uptake in the Human Lung Using Hyperpolarized Xenon-129. Proc. Natl. Acad. Sci. USA 2010, 107, 21707–21712. [Google Scholar] [CrossRef] [PubMed]
- Tustison, N.J.; Avants, B.B.; Flors, L.; Altes, T.A.; de Lange, E.E.; Mugler, J.P.; Gee, J.C. Ventilation-Based Segmentation of the Lungs Using Hyperpolarized (3)He MRI. J. Magn. Reson. Imaging JMRI 2011, 34, 831–841. [Google Scholar] [CrossRef]
- Tustison, N.J.; Altes, T.A.; Qing, K.; He, M.; Miller, G.W.; Avants, B.B.; Shim, Y.M.; Gee, J.C.; Mugler, J.P.; Mata, J.F. Image- versus Histogram-Based Considerations in Semantic Segmentation of Pulmonary Hyperpolarized Gas Images. Magn. Reson. Med. 2021, 86, 2822–2836. [Google Scholar] [CrossRef] [PubMed]
- Myc, L.; Qing, K.; He, M.; Tustison, N.; Lin, Z.; Manichaikul, A.W.; Patrie, J.; Cassani, J.; Nunoo-Asare, R.N.; Huang, Y.; et al. Characterisation of Gas Exchange in COPD with Dissolved-Phase Hyperpolarised Xenon-129 MRI. Thorax 2021, 76, 178–181. [Google Scholar] [CrossRef] [PubMed]
- Kaushik, S.S.; Cleveland, Z.I.; Cofer, G.P.; Metz, G.; Beaver, D.; Nouls, J.; Kraft, M.; Auffermann, W.; Wolber, J.; McAdams, H.P.; et al. Diffusion-Weighted Hyperpolarized 129Xe MRI in Healthy Volunteers and Subjects with Chronic Obstructive Pulmonary Disease. Magn. Reson. Med. 2011, 65, 1154–1165. [Google Scholar] [CrossRef] [PubMed]
- Ruppert, K.; Qing, K.; Patrie, J.T.; Altes, T.A.; Mugler, J.P. Using Hyperpolarized Xenon-129 MRI to Quantify Early-Stage Lung Disease in Smokers. Acad. Radiol. 2019, 26, 355–366. [Google Scholar] [CrossRef] [PubMed]
- Doganay, O.; Kim, M.; Gleeson, F.V. Gas Exchange and Ventilation Imaging of Healthy and COPD Subjects Using Hyperpolarized Xenon-129 MRI and a 3D Alveolar Gas-Exchange Model. Eur. Radiol. 2023, 33, 3322–3331. [Google Scholar] [CrossRef] [PubMed]
- Rao, Q.; Li, H.; Zhou, Q.; Zhang, M.; Zhao, X.; Shi, L.; Xie, J.; Fan, L.; Han, Y.; Guo, F.; et al. Assessment of Pulmonary Physiological Changes Caused by Aging, Cigarette Smoking, and COPD with Hyperpolarized 129Xe Magnetic Resonance. Eur. Radiol. 2024, 34, 7450–7459. [Google Scholar] [CrossRef]
- Guan, S.; Tustison, N.; Qing, K.; Shim, Y.M.; Mugler, J.; Altes, T.; Albon, D.; Froh, D.; Mehrad, B.; Patrie, J.; et al. 3D Single-Breath Chemical Shift Imaging Hyperpolarized Xe-129 MRI of Healthy, CF, IPF, and COPD Subjects. Tomography 2022, 8, 2574–2587. [Google Scholar] [CrossRef]
- Mummy, D.G.; Coleman, E.M.; Wang, Z.; Bier, E.A.; Lu, J.; Driehuys, B.; Huang, Y.-C. Regional Gas Exchange Measured by 129 Xe Magnetic Resonance Imaging Before and After Combination Bronchodilators Treatment in Chronic Obstructive Pulmonary Disease. J. Magn. Reson. Imaging JMRI 2021, 54, 964–974. [Google Scholar] [CrossRef] [PubMed]
- Qing, K.; Altes, T.A.; Mugler, J.P., III; Tustison, N.J.; Mata, Ruppert, K.; Komlosi, P.; Feng, X.; Nie, K.; Zhao, L.; Wang, Z.; et al. Pulmonary MRI with Hyperpolarized Xenon-129 Demonstrates Novel Alterations in Gas Transfer across the Air-Blood Barrier in Asthma. Med. Phys. 2024, 51, 2413–2423. [Google Scholar] [CrossRef] [PubMed]
- Qing, K.; Altes, T.A.; Mugler, J.P.; Mata, J.F.; Tustison, N.J.; Ruppert, K.; Bueno, J.; Flors, L.; Shim, Y.M.; Zhao, L.; et al. Hyperpolarized Xenon-129: A New Tool to Assess Pulmonary Physiology in Patients with Pulmonary Fibrosis. Biomedicines 2023, 11, 1533. [Google Scholar] [CrossRef]
- Ebner, L.; Virgincar, R.S.; He, M.; Choudhury, K.R.; Robertson, S.H.; Christe, A.; Mileto, A.; Mammarapallil, J.G.; McAdams, H.P.; Driehuys, B.; et al. Multireader Determination of Clinically Significant Obstruction Using Hyperpolarized 129Xe-Ventilation MRI. AJR Am. J. Roentgenol. 2019, 212, 758–765. [Google Scholar] [CrossRef]
- Ebner, L.; He, M.; Virgincar, R.S.; Heacock, T.; Kaushik, S.S.; Freemann, M.S.; McAdams, H.P.; Kraft, M.; Driehuys, B. Hyperpolarized 129Xenon Magnetic Resonance Imaging to Quantify Regional Ventilation Differences in Mild to Moderate Asthma: A Prospective Comparison Between Semiautomated Ventilation Defect Percentage Calculation and Pulmonary Function Tests. Investig. Radiol. 2017, 52, 120–127. [Google Scholar] [CrossRef] [PubMed]
- Mussell, G.T.; Marshall, H.; Smith, L.J.; Biancardi, A.M.; Hughes, P.J.C.; Capener, D.J.; Bray, J.; Swift, A.J.; Rajaram, S.; Condliffe, A.M.; et al. Xenon Ventilation MRI in Difficult Asthma: Initial Experience in a Clinical Setting. ERJ Open Res. 2021, 7, 00785–02020. [Google Scholar] [CrossRef] [PubMed]
- Svenningsen, S.; Kirby, M.; Starr, D.; Leary, D.; Wheatley, A.; Maksym, G.N.; McCormack, D.G.; Parraga, G. Hyperpolarized (3) He and (129) Xe MRI: Differences in Asthma before Bronchodilation. J. Magn. Reson. Imaging JMRI 2013, 38, 1521–1530. [Google Scholar] [CrossRef]
- Kooner, H.K.; McIntosh, M.J.; Desaigoudar, V.; Rayment, J.H.; Eddy, R.L.; Driehuys, B.; Parraga, G. Pulmonary Functional MRI: Detecting the Structure-Function Pathologies That Drive Asthma Symptoms and Quality of Life. Respirology 2022, 27, 114–133. [Google Scholar] [CrossRef] [PubMed]
- Peiffer, J.D.; Altes, T.; Ruset, I.C.; Hersman, F.W.; Mugler, J.P.; Meyer, C.H.; Mata, J.; Qing, K.; Thomen, R. Hyperpolarized 129Xe MRI, 99mTc Scintigraphy, and SPECT in Lung Ventilation Imaging: A Quantitative Comparison. Acad. Radiol. 2024, 31, 1666–1675. [Google Scholar] [CrossRef]
- Safavi, S.; Munidasa, S.; Zanette, B.; Dai, R.; Stirrat, E.; Li, D.; Moraes, T.J.; Subbarao, P.; Santyr, G. Evaluating Post-Bronchodilator Response in Well-Controlled Paediatric Severe Asthma Using Hyperpolarised 129Xe-MRI: A Pilot Study. Respir. Med. 2021, 180, 106368. [Google Scholar] [CrossRef]
- Lin, N.Y.; Roach, D.J.; Willmering, M.M.; Walkup, L.L.; Hossain, M.M.; Desirazu, P.; Cleveland, Z.I.; Guilbert, T.W.; Woods, J.C. 129Xe MRI as a Measure of Clinical Disease Severity for Pediatric Asthma. J. Allergy Clin. Immunol. 2021, 147, 2146–2153.e1. [Google Scholar] [CrossRef] [PubMed]
- Hall, C.S.; Quirk, J.D.; Goss, C.W.; Lew, D.; Kozlowski, J.; Thomen, R.P.; Woods, J.C.; Tustison, N.J.; Mugler, J.P.; Gallagher, L.; et al. Single-Session Bronchial Thermoplasty Guided by 129Xe Magnetic Resonance Imaging. A Pilot Randomized Controlled Clinical Trial. Am. J. Respir. Crit. Care Med. 2020, 202, 524–534. [Google Scholar] [CrossRef] [PubMed]
- Alam, F.S.; Zanette, B.; Munidasa, S.; Braganza, S.; Li, D.; Woods, J.C.; Ratjen, F.; Santyr, G. Intra- and Inter-Visit Repeatability of 129 Xenon Multiple-Breath Washout MRI in Children with Stable Cystic Fibrosis Lung Disease. J. Magn. Reson. Imaging 2023, 58, 936–948. [Google Scholar] [CrossRef]
- Marshall, H.; Voskrebenzev, A.; Smith, L.J.; Biancardi, A.M.; Kern, A.L.; Collier, G.J.; Wielopolski, P.A.; Ciet, P.; Tiddens, H.A.W.M.; Vogel-Claussen, J.; et al. 129 Xe and Free-Breathing 1 H Ventilation MRI in Patients With Cystic Fibrosis: A Dual-Center Study. J. Magn. Reson. Imaging JMRI 2023, 57, 1908–1921. [Google Scholar] [CrossRef]
- Kirby, M.; Villemaire, L.; Ahmed, H.; Paterson, N.A.; McCormack, D.G.; Lewis, J.F.; Parraga, G. Diffusion-Weighted Hyperpolarized Helium-3 Magnetic Resonance Imaging In Adult Cystic Fibrosis. In A94. Therapeutic and Diagnostic Advances in Cystic Fibrosis; American Thoracic Society International Conference Abstracts; American Thoracic Society: New York, NY, USA, 2013; p. A2072. [Google Scholar]
- Couch, M.J.; Thomen, R.; Kanhere, N.; Hu, R.; Ratjen, F.; Woods, J.; Santyr, G. A Two-Center Analysis of Hyperpolarized 129Xe Lung MRI in Stable Pediatric Cystic Fibrosis: Potential as a Biomarker for Multi-Site Trials. J. Cyst. Fibros. Off. J. Eur. Cyst. Fibros. Soc. 2019, 18, 728–733. [Google Scholar] [CrossRef] [PubMed]
- Bannier, E.; Cieslar, K.; Mosbah, K.; Aubert, F.; Duboeuf, F.; Salhi, Z.; Gaillard, S.; Berthezène, Y.; Crémillieux, Y.; Reix, P. Hyperpolarized 3He MR for Sensitive Imaging of Ventilation Function and Treatment Efficiency in Young Cystic Fibrosis Patients with Normal Lung Function. Radiology 2010, 255, 225–232. [Google Scholar] [CrossRef]
- Wang, J.M.; Robertson, S.H.; Wang, Z.; He, M.; Virgincar, R.S.; Schrank, G.M.; Smigla, R.M.; O’Riordan, T.G.; Sundy, J.; Ebner, L.; et al. Using Hyperpolarized 129Xe MRI to Quantify Regional Gas Transfer in Idiopathic Pulmonary Fibrosis. Thorax 2018, 73, 21–28. [Google Scholar] [CrossRef]
- Hahn, A.D.; Carey, K.J.; Barton, G.P.; Torres, L.A.; Kammerman, J.; Cadman, R.V.; Lee, K.E.; Schiebler, M.L.; Sandbo, N.; Fain, S.B. Functional Xenon-129 Magnetic Resonance Imaging Response to Antifibrotic Treatment in Idiopathic Pulmonary Fibrosis. ERJ Open Res. 2023, 9, 00080–02023. [Google Scholar] [CrossRef] [PubMed]
- Eaden, J.A.; Weatherley, N.D.; Chan, H.-F.; Collier, G.; Norquay, G.; Swift, A.J.; Rajaram, S.; Smith, L.J.; Bartholmai, B.J.; Bianchi, S.M.; et al. Hyperpolarised Xenon-129 Diffusion-Weighted Magnetic Resonance Imaging for Assessing Lung Microstructure in Idiopathic Pulmonary Fibrosis. ERJ Open Res. 2023, 9, 00048–02023. [Google Scholar] [CrossRef] [PubMed]
- Chan, H.-F.; Collier, G.J.; Parra-Robles, J.; Wild, J.M. Finite Element Simulations of Hyperpolarized Gas DWI in Micro-CT Meshes of Acinar Airways: Validating the Cylinder and Stretched Exponential Models of Lung Microstructural Length Scales. Magn. Reson. Med. 2021, 86, 514–525. [Google Scholar] [CrossRef] [PubMed]
- Stiefer, A.; Zhang, S.; Mummy, D.; Salazar, C.; Tighe, R.M.; Driehuys, B.; Swaminathan, A.C. Using 129Xenon MRI to Evaluate the Trajectories of Idiopathic Pulmonary Fibrosis. In A104. Advances in the Diagnosis and Treatment of ILD; American Thoracic Society International Conference Abstracts; American Thoracic Society: New York, NY, USA, 2024; p. A2859. [Google Scholar]
- Grist, J.T.; Chen, M.; Collier, G.J.; Raman, B.; Abueid, G.; McIntyre, A.; Matthews, V.; Fraser, E.; Ho, L.-P.; Wild, J.M.; et al. Hyperpolarized 129Xe MRI Abnormalities in Dyspneic Patients 3 Months after COVID-19 Pneumonia: Preliminary Results. Radiology 2021, 301, E353–E360. [Google Scholar] [CrossRef] [PubMed]
- Saunders, L.C.; Collier, G.J.; Chan, H.F.; Hughes, P.J.; Smith, L.J.; Watson, J.G.R.; Meiring, J.E.; Gabriel, Z.; Newman, T.; Plowright, M.; et al. Longitudinal Lung Function Assessment of Patients Hospitalized with COVID-19 Using 1H and 129Xe Lung MRI. Chest 2023, 164, 700–716. [Google Scholar] [CrossRef]
- Kooner, H.K.; McIntosh, M.J.; Matheson, A.M.; Venegas, C.; Radadia, N.; Ho, T.; Haider, E.A.; Konyer, N.B.; Santyr, G.E.; Albert, M.S.; et al. 129Xe MRI Ventilation Defects in Ever-Hospitalised and Never-Hospitalised People with Post-Acute COVID-19 Syndrome. BMJ Open Respir. Res. 2022, 9, e001235. [Google Scholar] [CrossRef] [PubMed]
- Matheson, A.M.; McIntosh, M.J.; Kooner, H.K.; Lee, J.; Desaigoudar, V.; Bier, E.; Driehuys, B.; Svenningsen, S.; Santyr, G.E.; Kirby, M.; et al. Persistent 129Xe MRI Pulmonary and CT Vascular Abnormalities in Symptomatic Individuals with Post-Acute COVID-19 Syndrome. Radiology 2022, 305, 466–476. [Google Scholar] [CrossRef] [PubMed]
- Eddy, R.L.; Mummy, D.; Zhang, S.; Dai, H.; Bechtel, A.; Schmidt, A.; Frizzell, B.; Gerayeli, F.V.; Leipsic, J.A.; Leung, J.M.; et al. Cluster Analysis to Identify Long COVID Phenotypes Using 129Xe Magnetic Resonance Imaging: A Multi-Centre Evaluation. Eur. Respir. J. 2024, 63, 2302301. [Google Scholar] [CrossRef] [PubMed]
- Kooner, H.K.; McIntosh, M.J.; Matheson, A.M.; Abdelrazek, M.; Albert, M.S.; Dhaliwal, I.; Kirby, M.; Ouriadov, A.; Santyr, G.E.; Venegas, C.; et al. Postacute COVID-19 Syndrome: 129Xe MRI Ventilation Defects and Respiratory Outcomes 1 Year Later. Radiology 2023, 307, e222557. [Google Scholar] [CrossRef] [PubMed]
- Walkup, L.L.; Roach, D.J.; Hall, C.S.; Gupta, N.; Thomen, R.P.; Cleveland, Z.I.; McCormack, F.X.; Woods, J.C. Cyst Ventilation Heterogeneity and Alveolar Airspace Dilation as Early Disease Markers in Lymphangioleiomyomatosis. Ann. Am. Thorac. Soc. 2019, 16, 1008–1016. [Google Scholar] [CrossRef] [PubMed]
- Stewart, N.J.; Higano, N.S.; Mukthapuram, S.; Willmering, M.M.; Loew, W.; West, M.; Arnsperger, A.; Pratt, R.; Rao, M.R.; Schulte, R.F.; et al. Initial feasibility and challenges of hyperpolarized 129 Xe MRI in neonates with bronchopulmonary dysplasia. Magn. Reson. Med. 2023, 90, 2420–2431. [Google Scholar] [CrossRef] [PubMed]
- Rankine, L.J.; Lu, J.; Wang, Z.; Kelsey, C.R.; Marks, L.B.; Das, S.K.; Driehuys, B. Quantifying Regional Radiation-Induced Lung Injury in Patients Using Hyperpolarized 129Xe Gas Exchange Magnetic Resonance Imaging. Int. J. Radiat. Oncol. Biol. Phys. 2024, 120, 216–228. [Google Scholar] [CrossRef]
- Svenningsen, S.; Kjarsgaard, M.; Haider, E.; Carmen Venegas, N.; Konyer, N.; Friedlander, Y.; Nasir, N.; Boylan, C.; Kirby, M.; Nair, P. Effects of Dupilumab on Mucus Plugging and Ventilation Defects in Patients with Moderate-to-Severe Asthma: A Randomized, Double-Blind, Placebo-Controlled Trial. Am. J. Respir. Crit. Care Med. 2023, 208, 995–997. [Google Scholar] [CrossRef] [PubMed]
- He, M.; Qing, K.; Tustison, N.; Beaulac, Z.; King, T.; Huff, T.; Paige, M.; Earasi, K.; Nunoo-Asare, R.; Struchen, S.; et al. Characterizing Gas Exchange Physiology in Healthy Young Electronic-Cigarette Users with Hyperpolarized 129Xe MRI: A Pilot Study. Int. J. Chronic Obstr. Pulm. Dis. 2021, 16, 3183–3187. [Google Scholar] [CrossRef]
| Authors | Disease Summary |
|---|---|
| COPD | |
| Myc et al. [4] | Significant correlations were found between 129XeMRI and FEV1, %DLCO, and emphysema in COPD |
| Kaushik et al. [5] | 129XeMRI ADC correlates with pulmonary function, and detects emphysema and age/posture changes |
| Qing et al. [11] | 129XeMRI CSSR spectroscopy and DP imaging reliably assess lung function in COPD, revealing thicker septal walls and low RBC-to-TP ratios, indicating poor gas exchange |
| Qing et al. [12] | 129XeMRI, with a quick single scan, effectively identifies pulmonary issues in patients with COPD, matching well with CT and gadolinium-enhanced MRI |
| Ruppert et al. [6] | 129XeMRI septal wall thickness correlates with DLCO, distinguishing healthy individuals from smokers and individuals with COPD |
| Doganay et al. [7] | 129XeMRI gas distribution COV and functional volumes were significantly lower in subjects with COPD vs. healthy subjects. |
| Rao et al. [8] | Significant differences in 129XeMRI VDP, alveolar sleeve depth, total septal wall thickness, ADC, and RBC/TP were found among healthy young, age-matched controls, asymptomatic smokers, and COPD groups |
| Guan et al. [9] | 129XeMRI 3D-SBCSI detects ventilation defects, correlates FEV1 with RBC/Gas, and distinguishes between pulmonary diseases |
| Mummy et al. [10] | 129XeMRI baseline bar%ref (barrier uptake relative to a healthy reference population) and DLCO correlated with post-treatment changes in ventilation defect; RBC%ref (red blood cell transfer relative to a healthy reference population) decreased in 58.8% of subjects post-treatment |
| Asthma | |
| Ebner et al. [13] | 129XeMRI VDS is significantly higher in airway obstruction, correlates with disease severity, and does not have a location-specific pattern |
| Ebner et al. [14] | 129XeMRI imaging detects airway obstructions in asthma, correlates with PFTs, and shows age-related VDP increase |
| Mussel et al. [15] | VDP and VHI correlated with lung function (FEV1, FEV1/FVC, FEF 25–75%) but not with ACQ7 or eosinophil count; imaging prompted diagnostic re-evaluation in some cases |
| Qing et al. [11] | There were significant age-related differences in 129XeMRI gas transfer: younger asthmatics had lower tissue uptake and higher blood transfer compared to controls; no differences were found in an older group or post-bronchodilator |
| Svenningsen et al. [16] | Pre-salbutamol, 129XeMRI VDP was higher than 3HeMRI, with greater post-salbutamol improvement with HP-129XeMRI measurement. Both gases showed VDP and ventilation COV reductions post-treatment, with 129XeMRI identifying an airway defect not seen with 3HeMRI |
| Kooner et al. [17] | 129XeMRI helps detect ventilation issues, inflammation, and airflow problems in asthma by visualizing gas exchange and airflow directly in the lungs |
| Peiffer et al. [18] | Scintigraphy–Xe MRI correlation was higher than SPECT-XeMRI. VDP correlated with FEV1, FEV1/FVC, and FEF 25–75, separating those with asthma and COPD from controls |
| Safavi et al. [19] | In 129XeMRI, asthma had more defects pre-BD, which reduced post-BD, matching healthy participants |
| Lin et al. [20] | Children with asthma had higher 129XeMRI VDP and defects per slice, correlating with increased healthcare use, oral corticosteroids, and reduced lung function (FEV1, FEV1/FVC) |
| Hall et al. [21] | One guided bronchoscopy (BT) using 129XeMRI resulted in a greater reduction in nonventilated lung and fewer asthma exacerbations compared to three unguided BTs, with similar quality of life improvements |
| Cystic Fibrosis | |
| Alam et al. [22] | Multiple-breath washout 129XeMRI showed high intra-visit and inter-visit repeatability in both healthy subjects and those with CF. CoV fractional ventilation correlated with LCI, highlighting ventilation heterogeneity’s role in early CF |
| Guan et al. [9] | The 3D-SBCSI detects ventilation defects, correlates FEV1 with RBC/gas, and distinguishes between pulmonary diseases |
| Marshall et al. [23] | 129XeMRI and 3HeMRI VDP correlated strongly with each other, FEV1, and LCI, showing similar large-scale agreement. However, 129XeMRI VDP was more sensitive to subtle ventilation changes in early lung disease than 1H VDP |
| Kirby et al. [24] | 3HeMRI ADC detected significant short-term lung changes in CF, correlating with FEV1 and showing more sensitivity than standard tests |
| Couch et al. [25] | 129XeMRI VDP measurements showed high agreement between analysts (ICC = 0.99), differentiating healthy and CF groups and correlating with FEV1 and LCI, supporting multi-center trial feasibility |
| Bannier et al. [26] | 3HeMRI ventilation defects were present in all patients despite normal spirometry; CPT caused varied defect distribution changes without significantly altering VDI or VF |
| Couch et al. [25] | 129XeMRI VDP measurements showed high agreement between analysts (ICC = 0.99), differentiating healthy and CF groups and correlating with FEV1 and LCI, supporting multi-center trial feasibility |
| IPF | |
| Wang et al. [27] | 129XeMRI showed a 188% increase in barrier uptake in IPF, correlating strongly with DLCO and the RBC/barrier ratio (r = 0.94) but not with CT fibrosis scores |
| Hahn et al. [28] | 129XeMRI detected improvements in regional gas exchange in patients with IPF treated with antifibrotics after 1 year, while no improvements were seen with conventional therapies |
| Eaden et al. [29] | 129XeMRI ADC increased significantly over 12 months in patients with IPF, indicating microstructural disease progression, despite no changes in PFTs. Strong correlations were found between 129XeMRI and DLCO/KCO |
| Qing et al. [12] | 129XeMRI revealed significant ventilation and gas exchange abnormalities in UIP, including impaired diffusion and an elevated tissue-to-gas ratio, even in patients with normal PFTs |
| Hahn et al. [28] | 129XeMRI MRI detected improvements in regional gas exchange in patients with IPF treated with antifibrotics after 1 year, while no improvements were seen with conventional therapies |
| Chan et al. [30] | SEM accurately estimates acinar dimensions and shows robustness across varying conditions and acinar length scales, validated using He-3 and Xe-129 simulations for healthy and IPF lungs |
| Stiefer et al. [31] | 129XeMRI may predict progression in idiopathic pulmonary fibrosis (IPF) |
| COVID-19 | |
| Grist et al. [32] | 129XeMRI revealed alveolar diffusion issues in post-COVID-19 patients, despite normal CT scans |
| Sanders et al. [33] | 129XeMRI gas transfer remained impaired up to 1 year post-hospitalization in patients with COVID-19, despite normal lung ventilation and no structural abnormalities |
| Kooner et al. [34] | 129XeMRI revealed significantly higher VDP in post-COVID, especially in hospitalized participants, correlating with reduced 6MWD and post-exertional SpO2 |
| Matheson et al. [35] | 129XeMRI effectively detects lung and vascular abnormalities in PACS, aiding COVID-19 diagnosis and management |
| Eddy et al. [36] | Four distinct long COVID phenotypes were identified using 129XeMRI, showing varying patterns of gas exchange and PFTs, highlighting the tool’s ability to differentiate long COVID pathophysiology for personalized care |
| Kooner et al. [37] | Post-COVID-19 patients showed improved lung function, gas exchange, and quality of life by 15 months. Early 129XeMRI VDP predicted exercise gains, and respiratory treatment improved quality of life |
| LAM | |
| Walkup et al. [38] | 129XeMRI detected ventilation deficits in LAM, correlating with FEV1/FVC and DLCO, offering sensitive assessment for screening and management |
| BPD | |
| Stewart et al. [39] | 129XeMRI detected mild ventilation abnormalities and elevated ADC in patients with BPD, demonstrating feasibility for assessing neonatal lung disease |
| Miscellaneous Disease | |
| Rankine et al. [40] | 129XeMRI identified dose-dependent changes in ventilation, membrane uptake, and RBC transfer post-RT, aiding in assessing radiation-induced lung injury |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
MacLeod, J.L.; Khan, H.M.; Franklin, A.; Myc, L.; Shim, Y.M. Hyperpolarized Xenon-129 MRI: Narrative Review of Clinical Studies, Testing, and Implementation of Advanced Pulmonary In Vivo Imaging and Its Diagnostic Applications. Diagnostics 2025, 15, 474. https://doi.org/10.3390/diagnostics15040474
MacLeod JL, Khan HM, Franklin A, Myc L, Shim YM. Hyperpolarized Xenon-129 MRI: Narrative Review of Clinical Studies, Testing, and Implementation of Advanced Pulmonary In Vivo Imaging and Its Diagnostic Applications. Diagnostics. 2025; 15(4):474. https://doi.org/10.3390/diagnostics15040474
Chicago/Turabian StyleMacLeod, Jamie L., Humam M. Khan, Ava Franklin, Lukasz Myc, and Yun Michael Shim. 2025. "Hyperpolarized Xenon-129 MRI: Narrative Review of Clinical Studies, Testing, and Implementation of Advanced Pulmonary In Vivo Imaging and Its Diagnostic Applications" Diagnostics 15, no. 4: 474. https://doi.org/10.3390/diagnostics15040474
APA StyleMacLeod, J. L., Khan, H. M., Franklin, A., Myc, L., & Shim, Y. M. (2025). Hyperpolarized Xenon-129 MRI: Narrative Review of Clinical Studies, Testing, and Implementation of Advanced Pulmonary In Vivo Imaging and Its Diagnostic Applications. Diagnostics, 15(4), 474. https://doi.org/10.3390/diagnostics15040474






