Microvascular Anastomosis in Practice: A Pilot Study on Microsurgical Training Efficiency
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Grosu-Bularda, A.; Hodea, F.-V.; Cretu, A.; Lita, F.-F.; Bordeanu-Diaconescu, E.-M.; Vancea, C.-V.; Lascar, I.; Popescu, S.A. Reconstructive Paradigms: A Problem-Solving Approach in Complex Tissue Defects. J. Clin. Med. 2024, 13, 1728. [Google Scholar] [CrossRef]
- Engel, H.; Lin, C.-H.; Wei, F.-C. Role of microsurgery in lower extremity reconstruction. Plast. Reconstr. Surg. 2011, 127 (Suppl. S1), 228S–238S. [Google Scholar] [CrossRef]
- Gasteratos, K.; Morsi-Yeroyannis, A.; Vlachopoulos, N.C.; Spyropoulou, G.-A.; Del Corral, G.; Chaiyasate, K. Microsurgical techniques in the treatment of breast cancer-related lymphedema: A systematic review of efficacy and patient outcomes. Breast Cancer 2021, 28, 1002–1015. [Google Scholar] [CrossRef]
- Marin, A.; Herlea, V.; Bancu, A.; Giuglea, C.; Țăpoi, D.A.; Ciongariu, A.M.; Marin, G.G.; Marinescu, S.A.; Dobrete, N.A.; Dumitru, A.V.; et al. Correlation Between the Clinical and Histopathological Results in Experimental Sciatic Nerve Defect Surgery. Medicina 2025, 61, 317. [Google Scholar] [CrossRef]
- Hardy, K.L.; Davis, K.E.; Constantine, R.S.; Chen, M.; Hein, R.; Jewell, J.L.; Dirisala, K.; Lysikowski, J.; Reed, G.; Kenkel, J.M. The impact of operative time on complications after plastic surgery: A multivariate regression analysis of 1753 cases. Aesthet. Surg. J. 2014, 34, 614–622. [Google Scholar] [CrossRef]
- Camino-Willhuber, G.; Cabrera, J.P.; Carazzo, C.; Guiroy, A.; Gagliardi, M.; Terrasa, S.; Joaquim, A.F. Reporting Complications in Spinal Surgery-a Systematic Literature Review. World Neurosurg. 2021, 150, e765–e770. [Google Scholar] [CrossRef]
- Temple, C.L.F.; Ross, D.C. A new, validated instrument to evaluate competency in microsurgery: The University of Western Ontario Microsurgical Skills Acquisition/Assessment instrument [outcomes article]. Plast. Reconstr. Surg. 2011, 127, 215–222. [Google Scholar] [CrossRef]
- Evgeniou, E.; Walker, H.; Gujral, S. The Role of Simulation in Microsurgical Training. J. Surg. Educ. 2018, 75, 171–181. [Google Scholar] [CrossRef]
- Zeng, W.; Shulzhenko, N.O.; Feldman, C.C.; Dingle, A.M.; Poore, S.O. “Blue-Blood”-infused chicken thigh training model for microsurgery and supermicrosurgery. Plast. Reconstr. Surg.–Glob. Open 2018, 6, e1695. [Google Scholar] [CrossRef]
- Roohi, S.A. Tips and Tricks in Microvascular Anastomoses. In The Current Perspectives on Coronary Artery Bypass Grafting; IntechOpen: London, UK, 2020. [Google Scholar]
- Belykh, E.; Onaka, N.R.; Abramov, I.T.; Yağmurlu, K.; Byvaltsev, V.A.; Spetzler, R.F.; Nakaj, P.; Preul, M.C. Systematic review of factors influencing surgical performance: Practical recommendations for microsurgical procedures in neurosurgery. World Neurosurg. 2018, 112, e182–e207. [Google Scholar] [CrossRef]
- Lakhiani, C.; Fisher, S.M.; Janhofer, D.E.; Song, D.H. Ergonomics in microsurgery. J. Surg. Oncol. 2018, 118, 840–844. [Google Scholar] [CrossRef] [PubMed]
- Acland, R.D.M.; Trachtenberg, L.M. The histopathology of small arteries following experimental microvascular anastomosis. Plast. Reconstr. Surg. 1977, 60, 868–875. [Google Scholar] [CrossRef]
- Alamoudi, U.; Ghanem, T. Solution to vessels mismatch in microsurgery: Vertical arteriotomy technique. Laryngoscope Investig. Otolaryngol. 2021, 6, 1321–1324. [Google Scholar] [CrossRef] [PubMed]
- Valentini, V.; Della Monaca, M. Microvascular Techniques. In Free Flaps in Head and Neck Reconstruction: A Step-By-Step Color Atlas; Springer Nature: Cham, Switzerland, 2020; pp. 19–29. [Google Scholar]
- Burdett, C.; Theakston, M.; Dunning, J.; Goodwin, A.; Kendall, S.W.H. Left-handed surgical instruments—A guide for cardiac surgeons. J. Cardiothorac. Surg. 2016, 11, 135. [Google Scholar] [CrossRef] [PubMed]
- Vila, I.; Couto-González, I.; Brea-García, B. Basic Principles in Microvascular Anastomosis and Free Tissue Transfer. In Vascular Biology-Selection of Mechanisms and Clinical Applications; IntechOpen: London, UK, 2020. [Google Scholar]
- MacDonald, J.D. Learning to perform microvascular anastomosis. Skull Base 2005, 15, 229–240. [Google Scholar] [CrossRef]
- Savetsky, I.L.; Cammarata, M.J.; Kantar, R.S.; Diaz-Siso, J.R.; Avashia, Y.J.; Rohrich, R.J.; Saadeh, P.B. The Left-handed Plastic Surgery Trainee: Perspectives and Recommendations. Plast. Reconstr. Surg. Glob. Open 2020, 8, e2686. [Google Scholar] [CrossRef]
- Szabo, B.; Fazekas, L.; Ghanem, S.; Godo, Z.A.; Madar, J.; Apro, A.; Nemeth, N. Biomechanical comparison of microvascular anastomoses prepared by various suturing techniques. Injury 2020, 51, 2866–2873. [Google Scholar] [CrossRef]
- Sert, G.; Sakarya, A.H. Safe, fast, and minimally-assisted microsurgical anastomosis with combined open-loop suturing and airborne tying: A clinical and experimental study. Turk. J. Trauma Emerg. Surg. 2023, 29, 449–457. [Google Scholar] [CrossRef]
- Sert, G.; Aksoyler, D.; Kara, M.; Bolletta, A.; Losco, L.; Cam, S.B.; Korkusuz, P.; Chen, H.-C. Comparison of total anastomosis time between four different combinations of suturing and knot tying techniques in microsurgical anastomosis. J. Plast. Surg. Hand Surg. 2023, 57, 240–246. [Google Scholar] [CrossRef]
- Lee, S.; Hweidi, S.A.; Skivolocki, W.P. An open-loop technique to facilitate microtubal anastomoses in the rat. J. Reconstr. Microsurg. 1984, 1, 45–48. [Google Scholar] [CrossRef]
- Sapountzis, S.; Kiranantawat, K.; Lim, S.Y.; Constantinides, J.; Ciudad, P.; Nicoli, F.; Wei, M.Y.; Sönmez, T.T.; Chen, H.C. A novel “continuous-interrupted” method for microvascular anastomosis. Microsurgery 2014, 34, 82–84. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, B.; Zoppo, M.; Yao, A.; Henderson, P.W. Simple Interrupted Microvascular Anastomosis: Review of Four Sutures Placement Sequences. J. Reconstr. Microsurg. Open 2020, 5, e101–e106. [Google Scholar] [CrossRef]
- Mehta, S.H.; Belykh, E.; Farhadi, D.S.; Preul, M.C.; Kikuta, K.-I. Needle Parking Interrupted Suturing Technique for Microvascular Anastomosis: A Technical Note. Oper. Neurosurg. 2021, 21, E414–E420. [Google Scholar] [CrossRef] [PubMed]
- Kamath, J.B.M.; Kamath, S.J.M.; Bhardwaj, P.M. A triad of technical tips to make microvascular repair simple and quick. Plast. Reconstr. Surg. 2007, 120, 819–821. [Google Scholar] [CrossRef] [PubMed]
- Akentieva, T.N.; Ovcharenko, E.A.; Kudryavtseva, Y.A. Influence of suture material on the development of postoperative complications in vascular surgery and their prevention. Khirurgiia 2019, 10, 75–81. [Google Scholar] [CrossRef]
- Malik, M.M.; Hachach-Haram, N.; Tahir, M.; Al-Musabi, M.; Masud, D.; Mohanna, P.-N. Acquisition of basic microsurgery skills using home-based simulation training: A randomised control study. J. Plast. Reconstr. Aesthet. Surg. 2017, 70, 478–486. [Google Scholar] [CrossRef]
- Masud, D.; Haram, N.; Moustaki, M.; Chow, W.; Saour, S.; Mohanna, P.N. Microsurgery simulation training system and set up: An essential system to complement every training programme. J. Plast. Reconstr. Aesthet. Surg. 2017, 70, 893–900. [Google Scholar] [CrossRef]
- Dave, A.; Singhal, M.; Tiwari, R.; Chauhan, S.; De, M. Effectiveness of a microsurgery training program using a chicken wing model. J. Plast. Surg. Hand Surg. 2022, 56, 191–197. [Google Scholar] [CrossRef]
- Mattar, T.G.d.M.; dos Santos, G.B.; Telles, J.P.M.; de Rezende, M.R.; Wei, T.H.; Mattar, R. Structured evaluation of a comprehensive microsurgical training program. Clinics 2021, 76, e3194. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Milling, R.; Carolan, D.; Pafitanis, G.; Quinlan, C.; Potter, S. Microtools: A systematic review of validated assessment tools in microsurgery. J. Plast. Reconstr. Aesthet. Surg. 2022, 75, 4013–4022. [Google Scholar] [CrossRef]


| Question | 1 Point | 3 Points | 5 Points |
|---|---|---|---|
| Number of microsurgeries performed | Less than 50 | 50–150 | More than 150 |
| Types of microsurgeries performed | Simple/none | Intermediate | Complex |
| Frequency of performing microsurgeries | Less than once a month | Monthly | Weekly |
| Experience with specific microsurgical tools and techniques | Basic/none | Moderate | Advanced |
| Years of experience in microsurgery | Less than 5 years | 5–10 years | More than 10 years |
| Microsurgery training and education | Self-taught | Microsurgery courses | Microsurgery fellowship |
| Experience in microsurgical research | None | Participated in research studies | Led research studies |
| Outcome of surgeries (rate your success rate from 1 to 5) | Under 70% or not applicable | >70% success rate in the past year | >90% success rate in the past year |
| Case difficulties | Low difficulty (end-to-end anastomoses or basic nerve repairs) | Moderate complexity cases (pedicle dissections or single free flaps) | High-risk or challenging cases (composite flaps, perforator flaps, or multiple anastomoses) |
| Continuing education in microsurgery | Rarely or never attends | Occasionally attends workshops/seminars | Regularly attends |
| Task | 1 Point | 3 Points | 5 Points |
|---|---|---|---|
| Duration to Complete Task | >25 min | 15–25 min | <15 min |
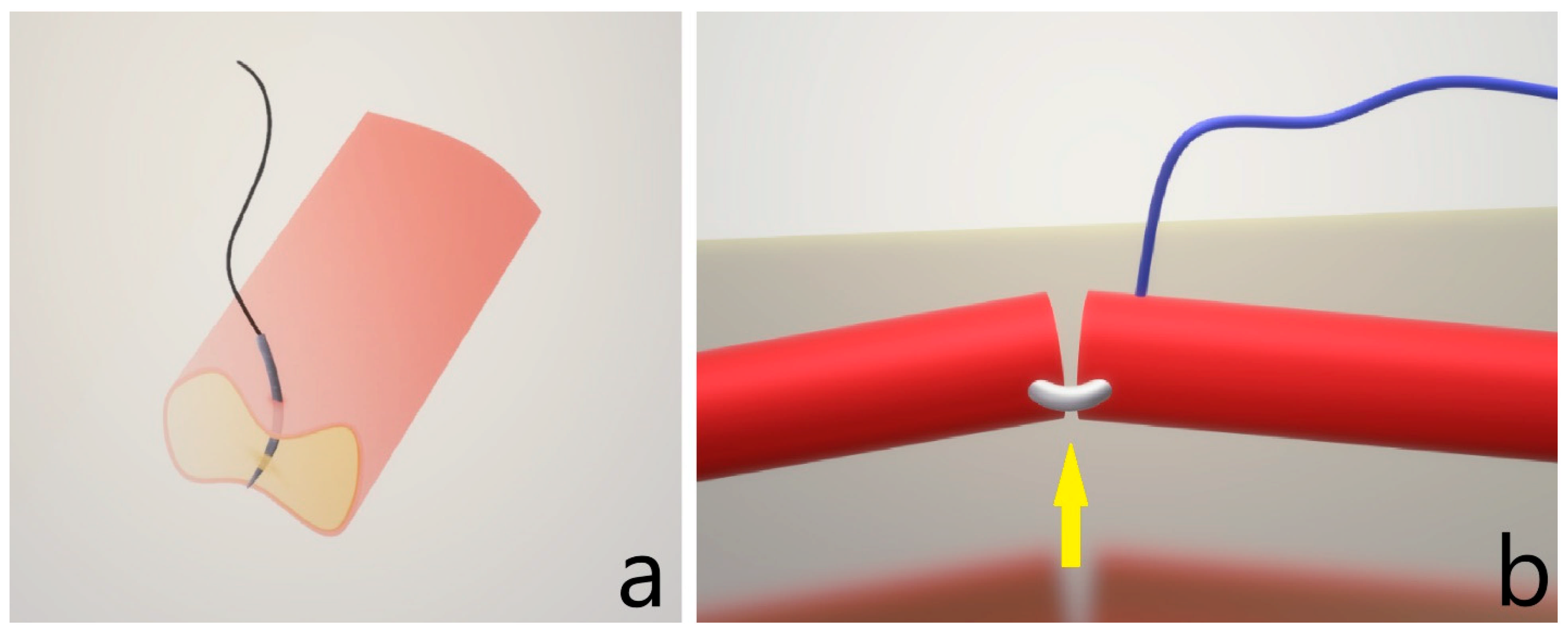
| Preparation: Clamp Placement | Oblique angled, jaws not grasping the entire vessel, tensioned anastomosis | Slightly angled, tensionless anastomosis | Perpendicular with even distribution of jaws placement, tensionless anastomosis |
| Preparation: Dilatation and adventitia cleaning | Forgets | Rough dilation, adventitia not cleaned | Gentle dilation with minimal force and even adventitia excision |
| Suturing: Needle Placement | Back wall stitch or partial only wall placement | Oblique placement through all wall layers | Perpendicular placement through all wall layers |
| Suturing: Needle Passage | Rough passage with damage | Rough passage without damage | Gentle, atraumatic and fluid movement |
| Suturing: Knot Tying | Rough tying with diminished tension within the knots | Rough tying with vessel wall dragging, but correct tension | Fluid motion of tying, correct knot tension |
| Suturing: Lumen Check | Forgets to check more than three times | Forgets to check 1 to 3 times | Always checks |
| Suturing: Movement at Anastomosis | Overlap of hands with obstruction of field | No field obstruction, but struggling for fluent motions | Ease of motion with no field obstruction |
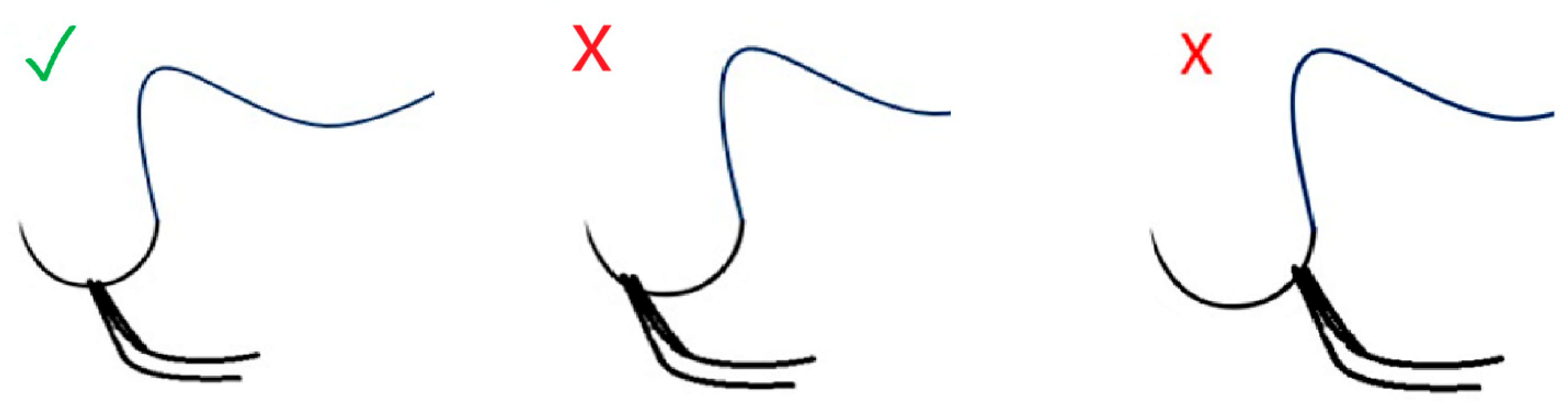
| Final Product: Outer Appearance | Inversed or kinked anastomosis | Areas of vessel wall overlapping | Slightly everted, aligned straight |
| Final Product: Patency | Completely obstructed, back wall stitch | Mild stenosis or leakage | Even-to-vessel caliber anastomosis, no stenosis, no leakage |
| Final Product: Suture Ends | Unevenly, in the lumen | Unevenly outside of the lumen | Even, outside of the lumen |
| Final Product: Suture Spacing | Asymmetric both spacing towards the vessel ends and between sutures | Spaced, but at irregular intervals | Symmetric spacing |
| Ergonomic Efficiency and Posture | Posture is hunched, finds difficulty in every step of the preparation and anastomosis | Breaks correct posture sometimes to accommodate preparation and anastomosis | Correct posture throughout preparation and anastomosis |
| Needle handling | Loses track of both needle and thread at least multiple times | Lost track of needle once | Permanent control of the needle location |
| Instrument handling | Constant improper usage of microsurgical instrument, e.g., dilator for grabbing, scissors for dilating | Sometimes uses incorrect instrument | Correct manipulation of instruments |
| Evaluation Timepoint | Test Group (Mean ± SEM) [95% CI] | Control Group (Mean ± SEM) [95% CI] | Test Group (Mean ± SD) | Control Group (Mean ± SD) | p-Value (t-Test) |
|---|---|---|---|---|---|
| Initial evaluation | 26.5 ± 1.50 [22.78–30.22] | 26 ± 2.65 [18.21–33.79] | 26.5 ± 3 | 26 ± 5.3 | 0.8748 |
| Evaluation after 3 weeks | 40 ± 2.38 [32.28–47.72] | 35 ± 0.82 [33.07–36.93] | 40 ± 4.8 | 35 ± 1.6 | 0.0941 |
| Evaluation after 3 months | 59 ± 1.83 [52.40–65.60] | 38 ± 2.08 [30.91–45.09] | 59 ± 3.7 | 38 ± 4.2 | 0.00027 |
| Skill Category | Specific Techniques Taught | Key Objectives |
|---|---|---|
| Ergonomics and setup | Proper posture maintenance (relaxed shoulders, straight spine), resting elbows, and optimizing microscope-eye alignment to reduce fatigue. | Reduce surgeon fatigue and enhance precision during procedures. |
| Vessel preparation and handling | Adventitia trimming, symmetric and tension-free clamp placement, gentle lumen dilation. | Improve preparation efficiency and minimize vessel damage. |
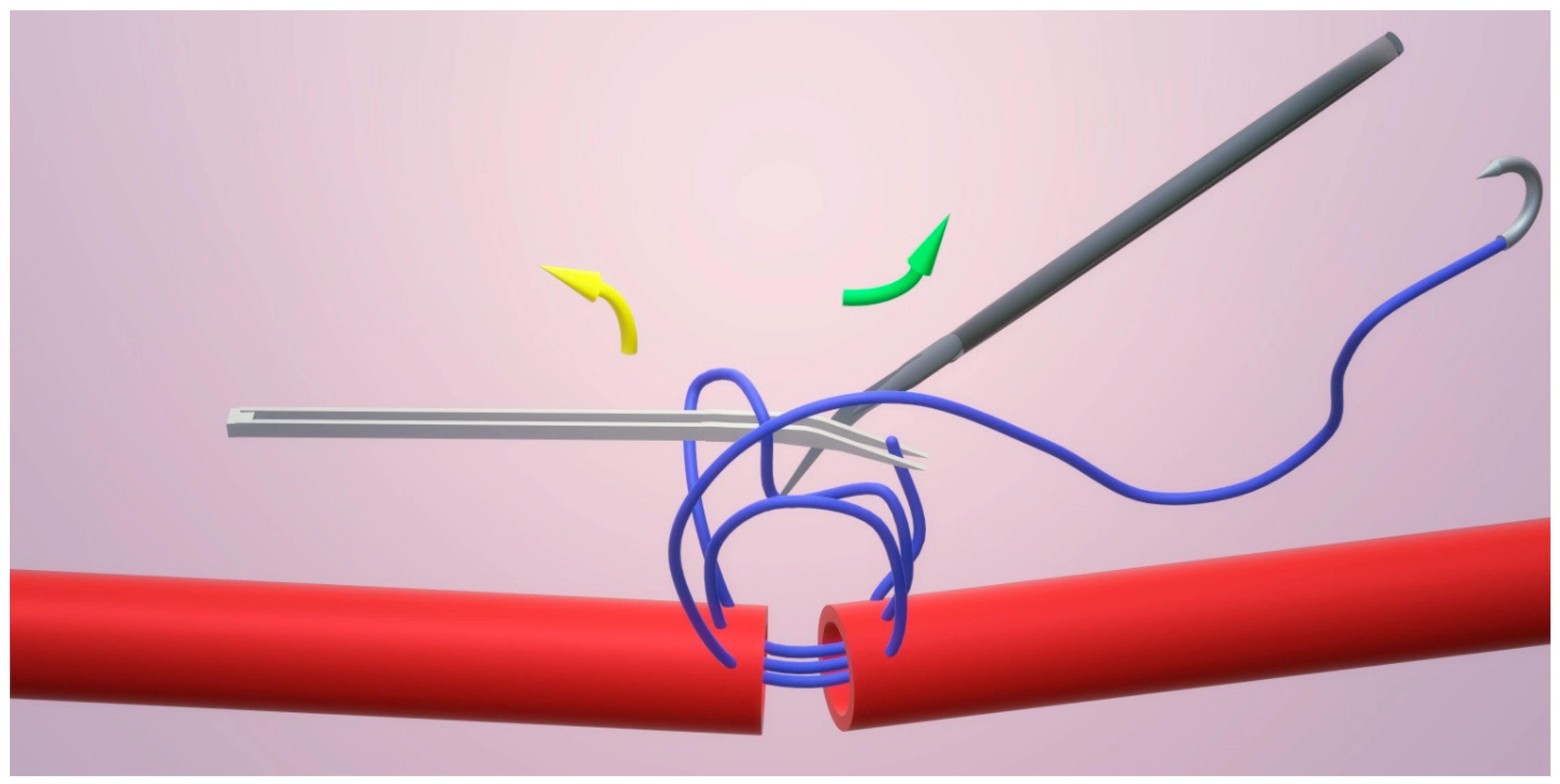
| Suturing | Open-loop suturing method to ensure lumen patency, ambidextrous knot tying for efficiency and avoid hand overlapping, and maintaining consistent suture spacing. | Optimize suturing speed and reduce complications like lumen obstruction. |
| Needle handling and insertion | Correct needle gripping, atraumatic passage through vessel walls, and applying counterpressure to prevent back-wall bites. | Enhance control during needle manipulation and avoid errors. |
| Instrument handling and workflow | Standardized instrument positioning for easier access, minimizing interruptions in microscope focus, and promoting smoother transitions. | Streamline workflow for consistent and efficient instrument use. |
| Final product assessment | Assessing vessel patency, avoiding stenosis, ensuring even suture spacing, and visually confirming lumen integrity (e.g., flipping vessel to detect ‘steel sign’). | Ensure high-quality anastomosis with minimal errors and obstructions. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hodea, F.-V.; Grosu-Bularda, A.; Cretu, A.; Dumitru, C.-S.; Ratoiu, V.-A.; Bordeanu-Diaconescu, E.-M.; Costache, R.-A.; Teodoreanu, R.-N.; Lascar, I.; Hariga, C.-S. Microvascular Anastomosis in Practice: A Pilot Study on Microsurgical Training Efficiency. Clin. Pract. 2025, 15, 82. https://doi.org/10.3390/clinpract15050082
Hodea F-V, Grosu-Bularda A, Cretu A, Dumitru C-S, Ratoiu V-A, Bordeanu-Diaconescu E-M, Costache R-A, Teodoreanu R-N, Lascar I, Hariga C-S. Microvascular Anastomosis in Practice: A Pilot Study on Microsurgical Training Efficiency. Clinics and Practice. 2025; 15(5):82. https://doi.org/10.3390/clinpract15050082
Chicago/Turabian StyleHodea, Florin-Vlad, Andreea Grosu-Bularda, Andrei Cretu, Catalina-Stefania Dumitru, Vladut-Alin Ratoiu, Eliza-Maria Bordeanu-Diaconescu, Raducu-Andrei Costache, Razvan-Nicolae Teodoreanu, Ioan Lascar, and Cristian-Sorin Hariga. 2025. "Microvascular Anastomosis in Practice: A Pilot Study on Microsurgical Training Efficiency" Clinics and Practice 15, no. 5: 82. https://doi.org/10.3390/clinpract15050082
APA StyleHodea, F.-V., Grosu-Bularda, A., Cretu, A., Dumitru, C.-S., Ratoiu, V.-A., Bordeanu-Diaconescu, E.-M., Costache, R.-A., Teodoreanu, R.-N., Lascar, I., & Hariga, C.-S. (2025). Microvascular Anastomosis in Practice: A Pilot Study on Microsurgical Training Efficiency. Clinics and Practice, 15(5), 82. https://doi.org/10.3390/clinpract15050082






