Whole Lung Irradiation after High-Dose Busulfan/Melphalan in Ewing Sarcoma with Lung Metastases: An Italian Sarcoma Group and Associazione Italiana Ematologia Oncologia Pediatrica Joint Study
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Setting and Staging
2.2. Consolidation Treatment
2.3. Toxicity Evaluation
2.4. Response and Outcome Evaluation
2.5. Data Collection and Statistical Analysis
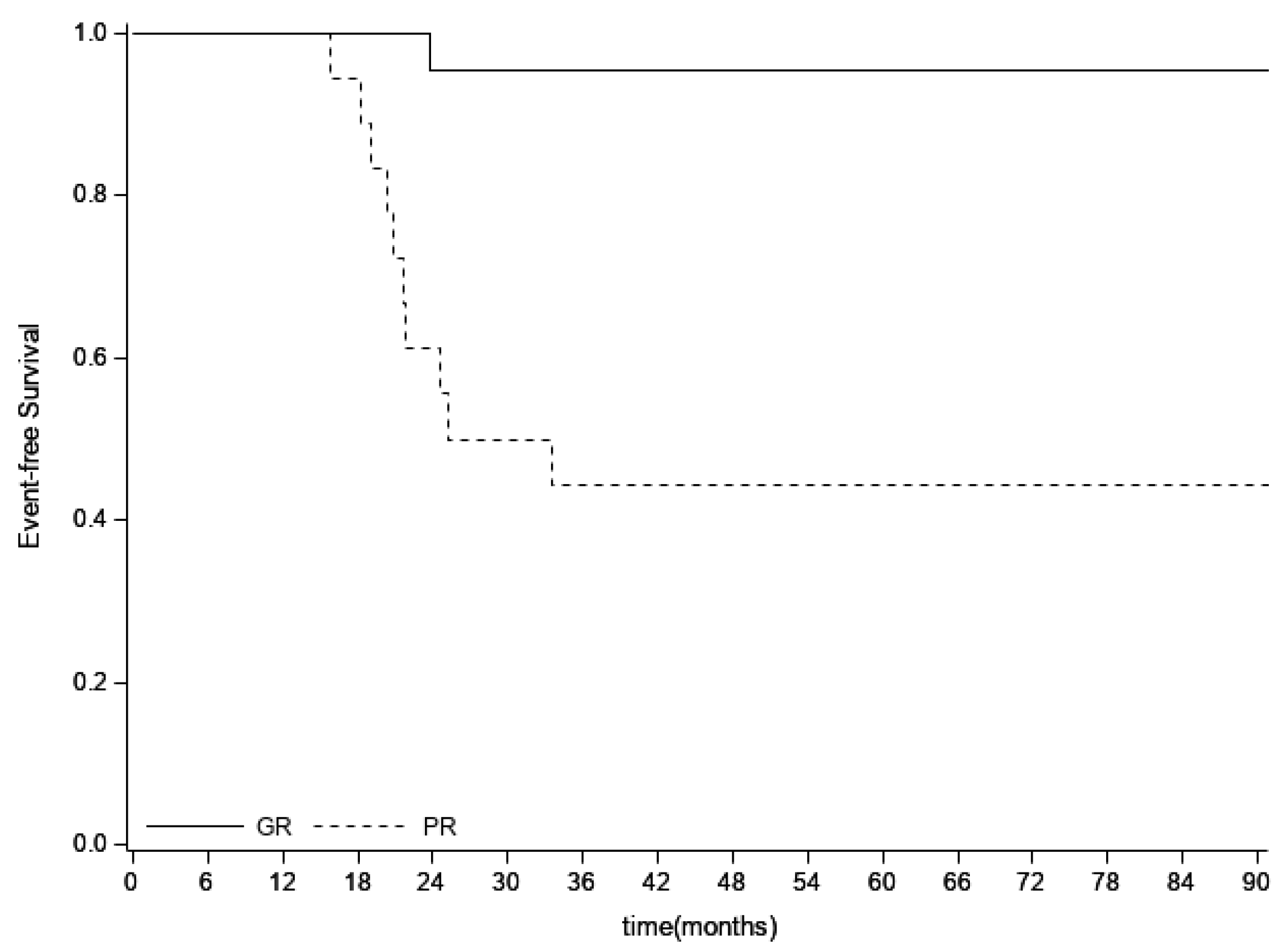
3. Results
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Manfrini, M.; Fabbri, N. Atlas of Musculoskeletal Tumors and Tumorlike Lesions; Picci, P., Gambarotti, M., Vanel, D., Eds.; Springer International Publishing: Cham, Switzerland, 2014; pp. 203–209. [Google Scholar] [CrossRef]
- Wolden, S.L.; Alektiar, K.M. Sarcomas across the Age Spectrum. Semin. Radiat. Oncol. 2010, 20, 45–51. [Google Scholar] [CrossRef]
- Bölling, T.; Schuck, A.; Paulussen, M.; Dirksen, U.; Ranft, A.; Könemann, S.; Dunst, J.; Willich, N.; Jürgens, H. Whole Lung Irradiation in Patients with Exclusively Pulmonary Metastases of Ewing Tumors. Strahlenther Onkol. 2008, 184, 193–197. [Google Scholar] [CrossRef]
- Grier, H.E.; Krailo, M.D.; Tarbell, N.J.; Link, M.P.; Fryer, C.J.H.; Pritchard, D.J.; Gebhardt, M.C.; Dickman, P.S.; Perlman, E.J.; Meyers, P.A.; et al. Addition of Ifosfamide and Etoposide to Standard Chemotherapy for Ewing’s Sarcoma and Primitive Neuroectodermal Tumor of Bone. N. Engl. J. Med. 2003, 348, 694–701. [Google Scholar] [CrossRef] [PubMed]
- Paulussen, M.; Craft, A.W.; Lewis, I.; Hackshaw, A.; Douglas, C.; Dunst, J.; Shuck, A.; Winkelmann, W.; Köhler, G.; Poremba, C.; et al. Results of the EICESS-92 Study: Two Randomized Trials of Ewing’s Sarcoma Treatment—Cyclophosphamide Compared With Ifosfamide in Standard-Risk Patients and Assessment of Benefit of Etoposide Added to Standard Treatment in High-Risk Patients. J. Clin. Oncol. 2008, 26, 4385–4393. [Google Scholar] [CrossRef] [PubMed]
- Granowetter, L.; Womer, R.; Devidas, M.; Krailo, M.; Wang, C.; Bernstein, M.; Marina, N.; Leavey, P.; Gebhardt, M.; Healey, J.; et al. Dose-Intensified Compared With Standard Chemotherapy for Nonmetastatic Ewing Sarcoma Family of Tumors: A Children’s Oncology Group Study. J. Clin. Oncol. 2009, 27, 2536–2541. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, S.; Sundby Hall, K.; Luksch, R.; Tienghi, A.; Wiebe, T.; Fagioli, F.; Alvegard, T.A.; Brach Del Prever, A.; Tamburini, A.; Alberghini, M.; et al. Nonmetastatic Ewing family tumors: High-dose chemotherapy with stem cell rescue in poor responder patients. Results of the Italian Sarcoma Group/Scandinavian Sarcoma Group III protocol. Ann. Oncol. 2011, 22, 1221–1227. [Google Scholar] [CrossRef] [PubMed]
- Womer, R.B.; West, D.C.; Krailo, M.D.; Dickman, P.S.; Pawel, B.R.; Grier, H.E.; Marcus, K.; Sailer, S.; Healey, J.H.; Dormans, J.P.; et al. Randomized Controlled Trial of Interval-Compressed Chemotherapy for the Treatment of Localized Ewing Sarcoma: A Report from the Children’s Oncology Group. J. Clin. Oncol. 2012, 30, 4148–4154. [Google Scholar] [CrossRef]
- Le Deley, M.-C.; Paulussen, M.; Lewis, I.; Brennan, B.; Ranft, A.; Whelan, J.; Le Teuff, G.; Michin, J.; Ladenstein, R.; Marec-Bérard, P.; et al. Cyclophosphamide compared with ifosfamide in consolidation treatment of standard-risk Ewing sarcoma: Results of the randomized noninferiority Euro-EWING99-R1 trial. J. Clin. Oncol. 2014, 32, 2440–2448. [Google Scholar] [CrossRef]
- Whelan, J.; Le Deley, M.-C.; Dirksen, U.; Le Teuff, G.; Brennan, B.; Gaspar, N.; Hawkins, D.S.; Amler, S.; Bauer, S.; Bielack, S.; et al. High-Dose Chemotherapy and Blood Autologous Stem-Cell Rescue Compared With Standard Chemotherapy in Localized High-Risk Ewing Sarcoma: Results of Euro-E.W.I.N.G.99 and Ewing-2008. J. Clin. Oncol. 2018, 36, 3110–3119. [Google Scholar] [CrossRef]
- Ladenstein, R.; Pötschger, U.; Le Deley, M.C.; Whelan, J.; Paulussen, M.; Oberlin, O.; van den Berg, H.; Dirksen, U.; Hjorth, L.; Michon, J.; et al. Primary Disseminated Multifocal Ewing Sarcoma: Results of the Euro-EWING 99 Trial. J. Clin. Oncol. 2010, 28, 3284–3291. [Google Scholar] [CrossRef] [PubMed]
- Oberlin, O.; Rey, A.; Desfachelles, A.S.; Philip, T.; Plantaz, D.; Schmitt, C.; Plouvier, E.; Lejars, O.; Rubie, H.; Terrier, P.; et al. Impact of High-Dose Busulfan Plus Melphalan As Consolidation in Metastatic Ewing Tumors: A Study by the Société Française des Cancers de l’Enfant. J. Clin. Oncol. 2006, 24, 3997–4002. [Google Scholar] [CrossRef]
- Luksch, R.; Tienghi, A.; Hall, K.S.; Fagioli, F.; Picci, P.; Barbieri, E.; Gandola, L.; Eriksson, M.; Ruggieri, P.; Daolio, P.; et al. Primary metastatic Ewing’s family tumors: Results of the Italian Sarcoma Group and Scandinavian Sarcoma Group ISG/SSG IV Study including myeloablative chemotherapy and total-lung irradiation. Ann. Oncol. 2012, 23, 2970–2976. [Google Scholar] [CrossRef]
- Dirksen, U.; Brennan, B.; Le Deley, M.-C.; Cozic, N.; van den Berg, H.; Bhadri, V.; Brichard, B.; Claude, L.; Craft, A.; Amler, S.; et al. High-Dose Chemotherapy Compared With Standard Chemotherapy and Lung Radiation in Ewing Sarcoma With Pulmonary Metastases: Results of the European Ewing Tumour Working Initiative of National Groups, 99 Trial and EWING 2008. J. Clin. Oncol. 2019, 37, 3192–3202. [Google Scholar] [CrossRef]
- Bacci, G.; Ferrari, S.; Longhi, A.; Donati, D.; De Paolis, M.; Forni, C.; Versari, M.; Setola, E.; Briccoli, A.; Barbieri, E. Therapy and survival after recurrence of Ewing’s tumors: The Rizzoli experience in 195 patients treated with adjuvant and neoadjuvant chemotherapy from 1979 to 1997. Ann. Oncol. 2003, 14, 1654–1659. [Google Scholar] [CrossRef]
- McTiernan, A.; Driver, D.; Michelagnoli, M.P.; Kilby, A.M.; Whelan, J.S. High dose chemotherapy with bone marrow or peripheral stem cell rescue is an effective treatment option for patients with relapsed or progressive Ewing’s sarcoma family of tumours. Ann. Oncol. 2006, 17, 1301–1305. [Google Scholar] [CrossRef]
- Ferrari, S.; Luksch, R.; Hall, K.S.; Fagioli, F.; Prete, A.; Tamburini, A.; Tienghi, A.; DiGirolamo, S.; Paioli, A.; Abate, M.E.; et al. Post-relapse survival in patients with Ewing sarcoma: High-Dose Therapy in Recurrent Ewing Sarcoma. Pediatr. Blood Cancer 2015, 62, 994–999. [Google Scholar] [CrossRef] [PubMed]
- Dunst, J.; Paulussen, M.; Jürgens, H. Lung irradiation for Ewing’s sarcoma with pulmonary metastases at diagnosis: Results of the CESS-studies. Strahlenther Onkol. 1993, 169, 621–623. [Google Scholar] [PubMed]
- Paulussen, M.; Ahrens, S.; Burdach, S.; Craft, A.; Dockhorn-Dworniczak, B.; Dunst, J.; Fröhlich, B.; Winkelmann, W.; Zoubek, A.; Jürgens, H. Primary metastatic (stage IV) Ewing tumor: Survival analysis of 171 patients from the EICESS studies. Ann. Oncol. 1998, 9, 275–281. [Google Scholar] [CrossRef] [PubMed]
- Biermann, J.S.; Chow, W.; Reed, D.R.; Lucas, D.; Adkins, D.R.; Agulnik, M.; Benjamin, R.S.; Brigman, B.; Budd, G.T.; Curry, W.T.; et al. NCCN Guidelines Insights: Bone Cancer, Version 2.2017. J. Natl. Compr. Canc. Netw. 2017, 15, 155–167. [Google Scholar] [CrossRef]
- Razek, A.; Perez, C.A.; Tefft, M.; Nesbit, M.; Vietti, T.; Burgert, E.O.; Kissane, J.; Pritchard, D.J.; Gehan, E.A. Intergroup Ewing’s Sarcoma Study: Local control related to radiation dose, volume, and site of primary lesion in Ewing’s sarcoma. Cancer 1980, 46, 516–521. [Google Scholar] [CrossRef]
- Whelan, J.S.; Burcombe, R.J.; Janinis, J.; Baldelli, A.M.; Cassoni, A.M. A systematic review of the role of pulmonary irradiation in the management of primary bone tumours. Ann. Oncol. 2002, 13, 23–30. [Google Scholar] [CrossRef]
- Ronchi, L.; Buwenge, M.; Cortesi, A.; Ammendolia, I.; Frakulli, R.; Abate, M.E.; Arcelli, A.; Donati, C.M.; Macchia, G.; Morganti, A.G.; et al. Whole Lung Irradiation in Patients with Osteosarcoma and Ewing Sarcoma. Anticancer Res. 2018, 38, 4977–4985. [Google Scholar] [CrossRef] [PubMed]
- Scobioala, S.; Ranft, A.; Wolters, H.; Jabar, S.; Paulussen, M.; Timmermann, B.; Jürgens, H.; Hassenpflug, W.; Klingebiel, T.; Elsayad, K.; et al. Impact of Whole Lung Irradiation on Survival Outcome in Patients With Lung Relapsed Ewing Sarcoma. Int. J. Radiat. Oncol. Biol. Phys. 2018, 102, 584–592. [Google Scholar] [CrossRef] [PubMed]
- Ladenstein, R.; Lasset, C.; Pinkerton, R.; Zucker, J.M.; Peters, C.; Burdach, S.; Pardo, N.; Dallorso, S.; Coze, C. Impact of megatherapy in children with high-risk Ewing’s tumours in complete remission: A report from the EBMT Solid Tumour Registry. Bone Marrow Transpl. 1995, 15, 697–705. [Google Scholar] [PubMed]
- Spunt, S.L.; McCarville, M.B.; Kun, L.E.; Poquette, C.A.; Cain, A.M.; Brandao, L.; Pappo, A.S. Selective Use of Whole-Lung Irradiation for Patients with Ewing Sarcoma Family Tumors and Pulmonary Metastases at the Time of Diagnosis. J. Pediatr. Hematol. Oncol. 2001, 23, 93–98. [Google Scholar] [CrossRef]
- Puma, N.; Asaftei, D.S.; Paioli, A.; Bisogno, G.; Rabusin, M.; Coccoli, L.; Tamburini, A.; Milano, G.M.; Mascarin, M.; Bertulli, R.; et al. Maintenance therapy with oral cyclophosphamide plus celecoxib in patients with metastatic Ewing sarcoma: Results of the Italian Sarcoma Group/AIEOP EW-2 study. J. Clin. Oncol. 2020, 38 (Suppl. 15), 10517. [Google Scholar] [CrossRef]
- Bauer, L.A.; Edwards, W.A.D.; Dellinger, E.P.; Simonowitz, D.A. Influence of weight on aminoglycoside pharmacokinetics in normal weight and morbidly obese patients. Eur. J. Clin. Pharmacol. 1983, 24, 643–647. [Google Scholar] [CrossRef]
- Basch, E.; Bennett, A.; Pietanza, M.C. Use of patient-reported outcomes to improve the predictive accuracy of clinician-reported adverse events. J. Natl Cancer Inst. 2011, 103, 1808–1810. [Google Scholar] [CrossRef] [PubMed]
- Mei, Z.; Grummer-Strawn, L.M.; Pietrobelli, A.; Goulding, A.; Goran, M.I.; Dietz, W.H. Validity of body mass index compared with other body-composition screening indexes for the assessment of body fatness in children and adolescents. Am. J. Clin. Nutr. 2002, 75, 978–985. [Google Scholar] [CrossRef] [PubMed]
- Kuczmarski, R.J.; Ogden, C.L.; Grummer-Strawn, L.M.; Flegal, K.M.; Guo, S.S.; Wei, R.; Mei, Z.; Curtin, L.R.; Roche, A.F.; Johnson, C.L. CDC growth charts: United States. Adv. Data 2000, 314, 1–27. [Google Scholar] [PubMed]
- Picci, P.; Böhling, T.; Bacci, G.; Ferrari, S.; Sangiorgi, L.; Mercuri, M.; Ruggieri, P.; Manfrini, M.; Ferraro, A.; Casadei, R.; et al. Chemotherapy-induced tumor necrosis as a prognostic factor in localized Ewing’s sarcoma of the extremities. J. Clin. Oncol. 1997, 15, 1553–1559. [Google Scholar] [CrossRef]
- Eisenhauer, E.A.; Therasse, P.; Bogaerts, J.; Schwartz, L.H.; Sargent, D.; Ford, R.; Dancey, J.; Arbuck, S.; Gwyther, S.; Mooney, M.; et al. New response evaluation criteria in solid tumours: Revised RECIST guideline (version 1.1). Eur. J. Cancer 2009, 45, 228–247. [Google Scholar] [CrossRef]
- Scobioala, S.; Eich, H.T. Risk stratification of pulmonary toxicities in the combination of whole lung irradiation and high-dose chemotherapy for Ewing sarcoma patients with lung metastases: A review. Strahlenther Onkol. 2020, 196, 495–504. [Google Scholar] [CrossRef] [PubMed]
- Mazzola, R.; Ruggieri, R.; Figlia, V.; Rigo, M.; Giaj Levra, N.; Ricchetti, F.; Nicosia, L.; Corradini, S.; Alongi, F. Stereotactic body radiotherapy of central lung malignancies using a simultaneous integrated protection approach. Strahlenther Onkol. 2019, 195, 719–724. [Google Scholar] [CrossRef] [PubMed]
- Rasper, M.; Jabar, S.; Ranft, A.; Jürgens, H.; Amler, S.; Dirksen, U. The value of high-dose chemotherapy in patients with first relapsed Ewing sarcoma. Pediatr. Blood Cancer 2014, 61, 1382–1386, Epub 11 April 2014. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | N | % | ||
|---|---|---|---|---|
| Median age (range) | 14 years (8 months–35 years) | |||
| Gender | Male | 39 | 57.3 | |
| Female | 29 | 42.7 | ||
| Trial | ISG/AIEOP EW2 | 36 | 52.9 | |
| ISG/SSG IV | 32 | 47.1 | ||
| Primary tumor site | Extremities | 33 | 48.5 | |
| Pelvis | 21 | 30.9 | ||
| Vertebrae | 4 | 5.9 | ||
| Ribs | 5 | 7.3 | ||
| Other | 5 | 7.3 | ||
| Metastases | Only lung | 56 | 82.3 | |
| Lung + extra pulmonary | 12 | 17.7 | ||
| Lung bilateral | 52 | 76.5 | ||
| Lung monolateral | 16 | 23.2 | ||
| Local treatment | Surgery 1 | 33 | 48.5 | |
| Surgery + radiotherapy 2 | 16 | 23.5 | ||
| Radiotherapy | 19 | 27.9 | ||
| Metastasectomy | Lung | 4 | 5.9 | |
| Bone | 1 | 1.5 | ||
| Busulfan administration | IV | 42 | 61.8 | |
| Oral | 26 | 38.1 | ||
| Radiotherapy technique | 3D | 50 | 73.5 | |
| IMRT/VMAT | 18 | 26.5 |
| Spirometry | Pre-BuMel | Pre-WLI | Post-WLI | Last Follow-Up |
|---|---|---|---|---|
| No. of patients | 61 | 38 | 55 | 44 |
| Restrictive | 4 | 9 | 17 | 15 |
| Grade 1 | 3 | 7 | 13 | 10 |
| Grade 2 | 1 | 2 | 4 | 5 |
| Grade 3 | - | - | - | - |
| Obstructive | 1 | 0 | 3 | 1 |
| Grade 1 | 1 | - | 3 | - |
| Grade 2 | - | - | - | 1 |
| Grade 3 | - | - | - | - |
| No. (%) pathologic | 5 (8.2%) | 9 (23.7%) | 20 (36.4%) | 16 (36.4%) |
| 95% CI | 3.4–18.2% | 12.8–39.6% | 24.8–49.7% | 23.6–51.4% |
| Toxicity CTCAE Grade | Pts | % | 95% C.I. |
|---|---|---|---|
| Pulmonary Fibrosis Grade 1 2 | 7 3 4 | 10.3 | 5–20.1% |
| Alveolitis | 4 | 5.9 | 2.2–14.6% |
| Grade 1 2 3 | 2 1 1 | ||
| Pulmonary Fibrosis + Alveolitis Grade 1 2 | 7 5 2 | 10.3 | 5–20.1% 17.4–38.2% |
| TOTAL Grade 1 2 3 | 18 10 7 1 | 26.5 |
| Toxicity CTCAE Grade | Pts | % | 95% C.I. |
|---|---|---|---|
| Pneumonitis/Pneumonia Grade 1 2 | 6 2 4 | 8.8 | 4–18% |
| Cough Grade 1 2 | 5 1 4 | 7.4 | 3.1–16.3% |
| Esophagitis Grade 1 2 | 4 1 3 | 5.9 | 2.2–14.6% |
| Anorexia Grade 2 | 3 3 | 4.3 | 1.4–12.6% |
| Asthenia Grade 2 | 3 3 | 4.3 | 1.4–12.6% |
| Nausea Grade 2 | 3 3 | 4.3 | 1.4–12.6% |
| Odynophagia Grade 2 3 | 3 2 1 | 4.3 | 1.4–12.6% |
| Dyspnea Grade 1 | 1 1 | 1.5 | 0.2–9.6% |
| Hypothyroidism Grade 2 | 1 1 | 1.5 | 0.2–9.6% |
| Variable | Pts | Events 3y | %EFS 3y (95%CI) | Events 5y | %EFS 5y (95%CI) | p Value | |
|---|---|---|---|---|---|---|---|
| Age | ≤14 y | 31 | 12 | 61 (41.6–75.7) | 12 | 61 (41.6–75.7) | 0.9634 |
| >14 y | 37 | 13 | 64.9 (47.3–77.9) | 14 | 61.6 (43.9–75.2) | ||
| Primary site | Pelvic | 21 | 12 | 42.9 (21.9–62.3) | 13 | 38.1 (18.3–57.8) | 0.0040 |
| Other | 47 | 13 | 72.1 (56.8–82.8) | 13 | 72.1 (56.8–82.8) | ||
| Soft tissue response | CR | 18 | 5 | 71.1 (43.8–86.9) | 5 | 71.1 (43.8–86.9) | 0.2295 |
| PR/SD | 49 | 20 | 59.2 (44.2–71.4) | 21 | 56.7 (41.6–69.3) | ||
| Local therapy | Surgery | 33 | 9 | 72.4 (53.6–84.6) | 9 | 72.4 (53.6–84.6) | 0.0005 |
| Surgery + RT | 16 | 3 | 81.3 (52.5–93.5) | 4 | 74.5 (45.4–89.6) | ||
| RT | 19 | 13 | 31.6 (12.9–52.2) | 13 | 31.6 (12.9–52.2) | ||
| Histological necrosis | Good | 22 | 1 | 95.5 (71.9–99.3) | 1 | 95.5 (71.9–99.3) | 0.0003 |
| Poor | 18 | 10 | 44.4 (21.6–65.1) | 10 | 44.4 (21.6–65.1) | ||
| Metastatic site | Only lung | 56 | 17 | 69.5 (55.6–79.8) | 18 | 67.2 (53–78) | 0.0178 |
| Lung + extra pulmonary | 12 | 8 | 33.3 (10.3–58.8) | 8 | 33.3 (10.3–58.8) | ||
| Lung metastases | ≤10 | 46 | 14 | 69.5 (54–80.7) | 15 | 66.6 (50.7–78.4) | 0.2485 |
| >10 | 22 | 11 | 50 (28.2–68.4) | 11 | 50 (28.2–68.4) | ||
| Bilateral | 52 | 21 | 59.3 (44.7–71.3) | 21 | 59.3 (44.7–71.3) | 0.5647 | |
| Monolateral | 16 | 4 | 75 (46.3–71.3) | 5 | 65.6 (34.9–84.5) | ||
| Chest CT response | CR | 42 | 11 | 73.8 (57.7–84.6) | 12 | 70.7 (54.1–82.3) | 0.0218 |
| PR/SD | 26 | 14 | 45.6 (25.9–63.3) | 14 | 45.6 (25.9–63.3) | ||
| Busulfan | IV | 42 | 19 | 54.5 (38.3–68.1) | 19 | 54.5 (38.3–68.1) | 0.0824 |
| OS | 26 | 6 | 76.9 (55.7–88.9) | 7 | 72.9 (51.4–86.1) | ||
| WLI start from ASCT | >90 days | 17 | 7 | 58.8 (32.5–77.8) | 7 | 58.8 (32.5–77.8) | 0.8484 |
| ≤90 days | 51 | 18 | 64.5 (49.8–76) | 19 | 61.8 (46.8–73.8) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abate, M.E.; Cammelli, S.; Ronchi, L.; Diletto, B.; Gandola, L.; Paioli, A.; Longhi, A.; Palmerini, E.; Puma, N.; Tamburini, A.; et al. Whole Lung Irradiation after High-Dose Busulfan/Melphalan in Ewing Sarcoma with Lung Metastases: An Italian Sarcoma Group and Associazione Italiana Ematologia Oncologia Pediatrica Joint Study. Cancers 2021, 13, 2789. https://doi.org/10.3390/cancers13112789
Abate ME, Cammelli S, Ronchi L, Diletto B, Gandola L, Paioli A, Longhi A, Palmerini E, Puma N, Tamburini A, et al. Whole Lung Irradiation after High-Dose Busulfan/Melphalan in Ewing Sarcoma with Lung Metastases: An Italian Sarcoma Group and Associazione Italiana Ematologia Oncologia Pediatrica Joint Study. Cancers. 2021; 13(11):2789. https://doi.org/10.3390/cancers13112789
Chicago/Turabian StyleAbate, Massimo E., Silvia Cammelli, Letizia Ronchi, Barbara Diletto, Lorenza Gandola, Anna Paioli, Alessandra Longhi, Emanuela Palmerini, Nadia Puma, Angela Tamburini, and et al. 2021. "Whole Lung Irradiation after High-Dose Busulfan/Melphalan in Ewing Sarcoma with Lung Metastases: An Italian Sarcoma Group and Associazione Italiana Ematologia Oncologia Pediatrica Joint Study" Cancers 13, no. 11: 2789. https://doi.org/10.3390/cancers13112789
APA StyleAbate, M. E., Cammelli, S., Ronchi, L., Diletto, B., Gandola, L., Paioli, A., Longhi, A., Palmerini, E., Puma, N., Tamburini, A., Mascarin, M., Coassin, E., Prete, A., Asaftei, S. D., Manzitti, C., Bisogno, G., Pierobon, M., Coccoli, L., Capasso, M., ... Luksch, R. (2021). Whole Lung Irradiation after High-Dose Busulfan/Melphalan in Ewing Sarcoma with Lung Metastases: An Italian Sarcoma Group and Associazione Italiana Ematologia Oncologia Pediatrica Joint Study. Cancers, 13(11), 2789. https://doi.org/10.3390/cancers13112789








