Fibrin Sealants and Axillary Lymphatic Morbidity: A Systematic Review and Meta-Analysis of 23 Clinical Randomized Trials
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Selection
2.2. Outcomes
2.3. Statistical Analysis
3. Results
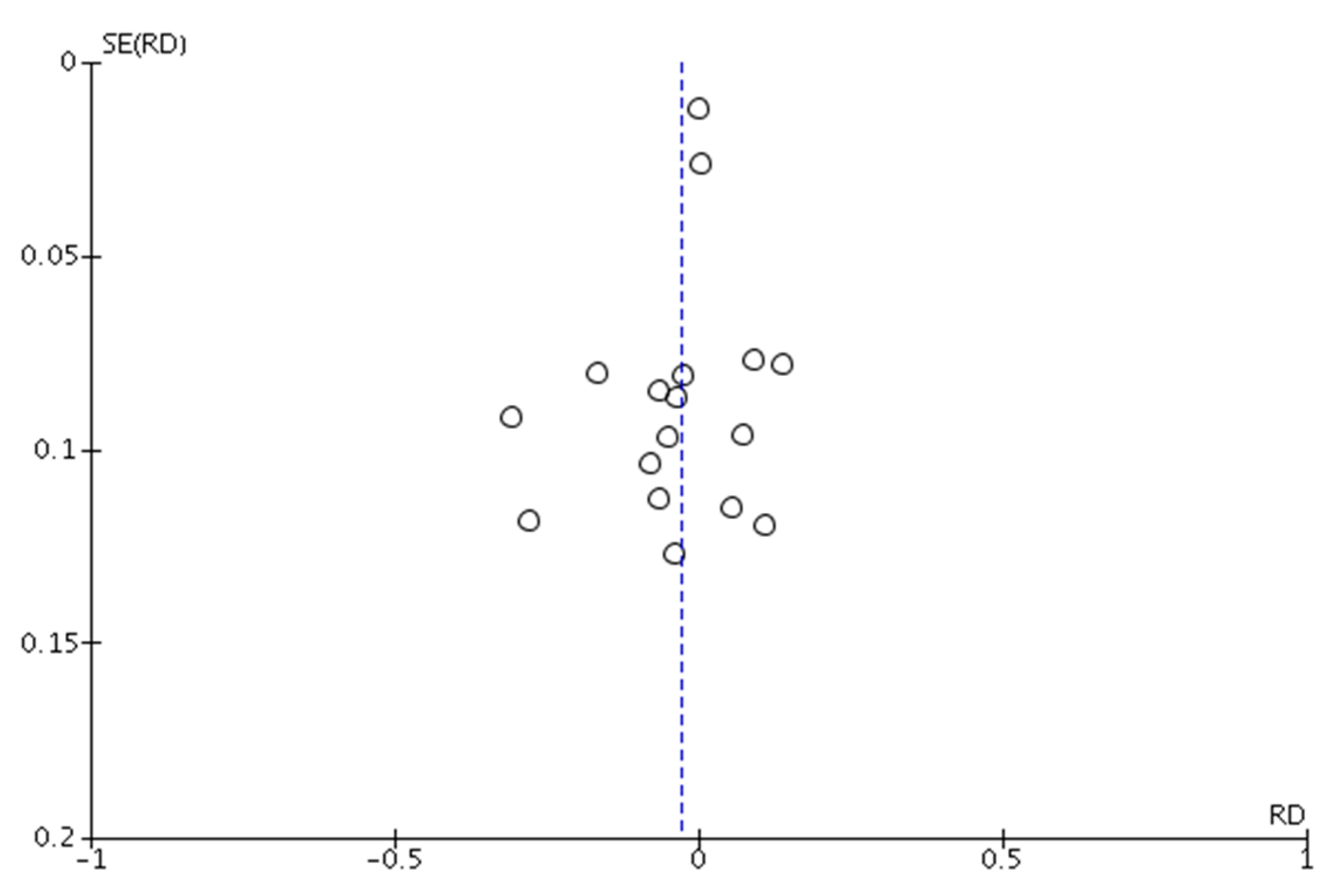
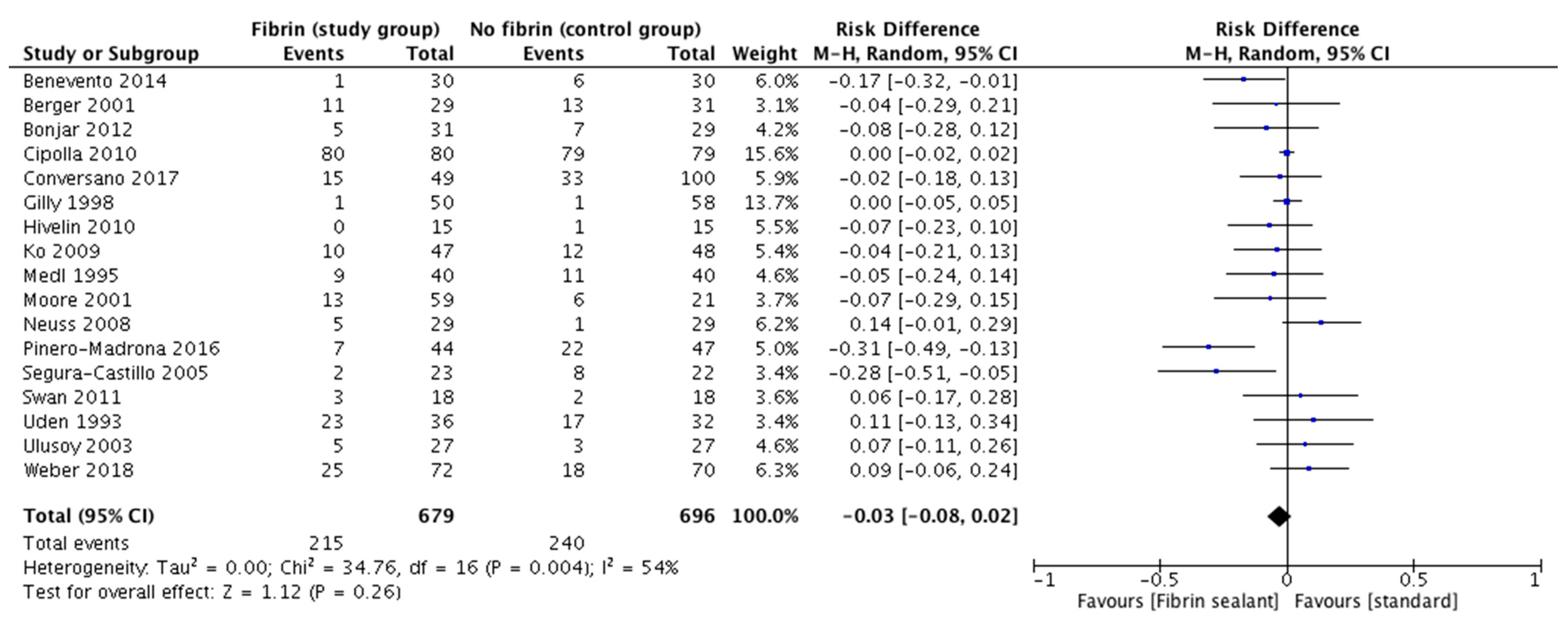
3.1. Axillary Lymphocele
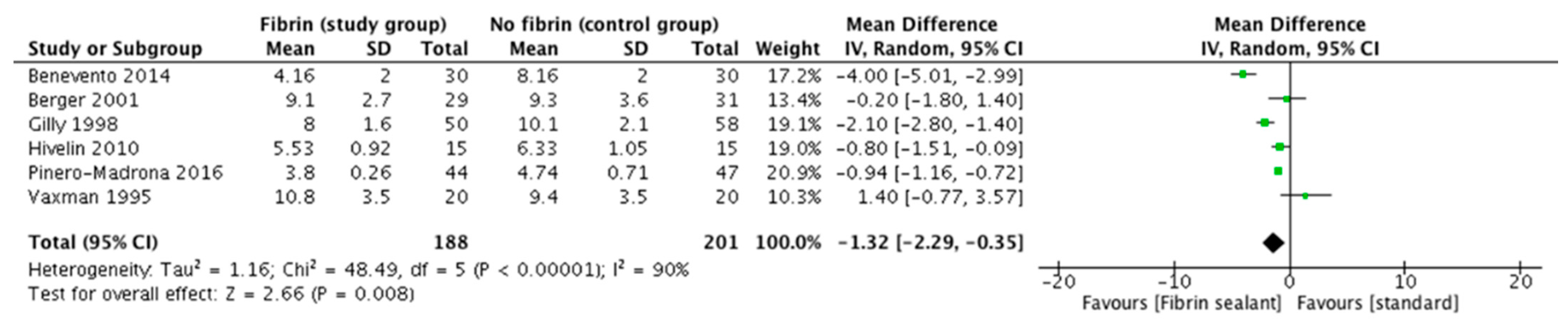
3.2. Axillary Drainage Output
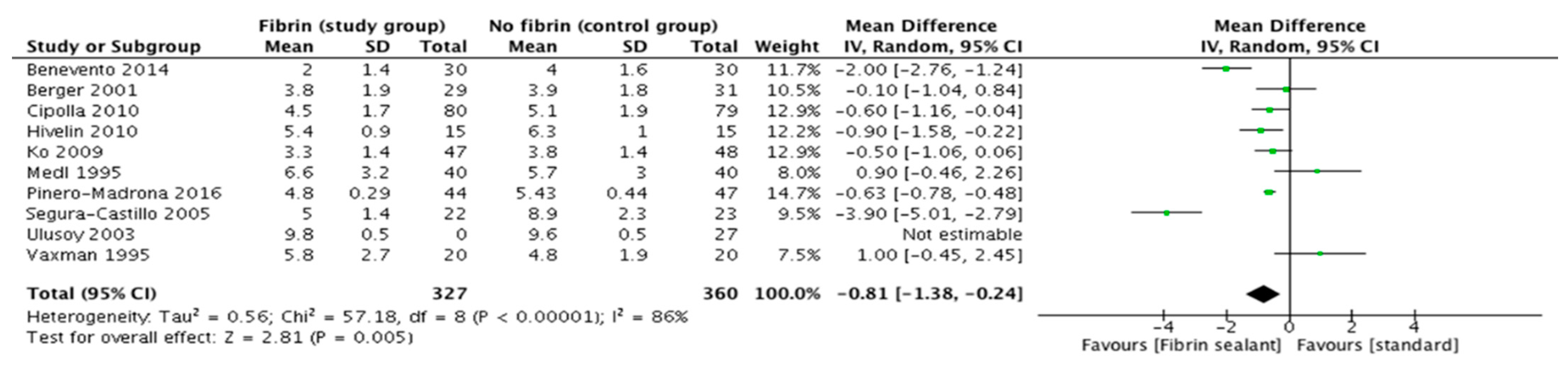
3.3. Days of Hospital Stay
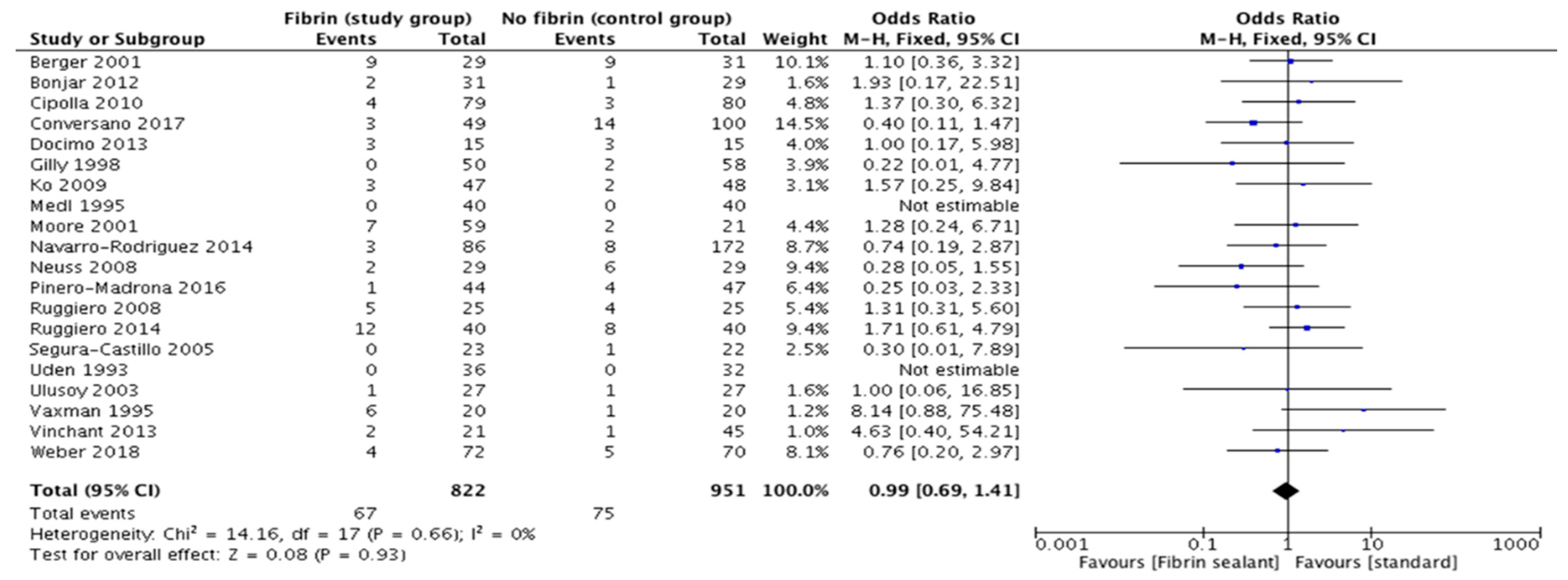
3.4. Surgical Site Complications
3.5. Number of Days before Removal of Axillary Drainage
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Appendix A
| TASK | DESCRIPTION | CLASSIFICATION |
|---|---|---|
| Formulate question | Question: Does the off-label use of fibrin sealant affect lymphatic morbidity after axillary dissection? | Step I: preparation |
| Check for previous systematic review (SR) | Similar SRs, but in different settings were identified and commented in the discussion. | Step I: preparation |
| Protocol drafting | An objective and reproducible methodology was designed and reported in the “methods” paragraph of the manuscript. | Step I: preparation |
| Search strategy definition | Data were identified using the electronic databases PubMed, MEDLINE, and Scopus and strict inclusion criteria were defined. | Step I: preparation |
| Literature search | 238 citations, even if many irrelevant ones included at the first literature screening. | Step II: retrieval |
| De-duplicate | Twenty-one identical citations were excluded. | Step II: retrieval |
| Screen abstract | Based on titles and abstract, the irrelevant trials were definitely removed. | Step III: appraisal |
| Obtain full text | All the remaining studies were downloaded. When download was not allowed, a copy was requested from author or alternative library. | Step II–III: retrieval and appraisal |
| Screen full text | Further screening was performed after carefully reading the full manuscript. | Step III: appraisal |
| Snowball | Additional trials were found checking the citations of the included trials. | Step II–III: retrieval and appraisal |
| Data extraction | Number of events/total and mean +/− standard deviation were collected from each sty arm. | Step IV: synthesis |
| Literature re-check | A literature search was repeated to find new eligible trials since the initial search. | Step II–IV: retrieval, appraisal, synthesis |
| Analysis | Data were statistically combined from all the included trials. | Step IV: synthesis |
| Manuscript draft and editing | The final paper was written following the PRISMA checklist. | Step V: write-up |
Appendix B
References
- Mansel, R.E.; Fallowfield, L.; Kissin, M.; Goyal, A.; Newcombe, R.G.; Dixon, J.M.; Yiangou, C.; Horgan, K.; Bundred, N.; Monypenny, I.; et al. Randomized Multicenter Trial of Sentinel Node Biopsy Versus Standard Axillary Treatment in Operable Breast Cancer: The ALMANAC Trial. J. Natl. Cancer Inst. 2006, 98, 599–609. [Google Scholar] [CrossRef] [Green Version]
- Ditsch, N.; Rubio, I.T.; Gasparri, M.L.; de Boniface, J.; Kuehn, T. Breast and axillary surgery in malignant breast disease: A review focused on literature of 2018 and 2019. Curr. Opin. Obstet. Gynecol. 2020, 32, 91–99. [Google Scholar] [CrossRef]
- Galimberti, V.; Cole, B.F.; Viale, G.; Veronesi, P.; Vicini, E.; Intra, M.; Mazzarol, G.; Massarut, S.; Zgajnar, J.; Forbes, J.; et al. Axillary dissection versus no axillary dissection in patients with breast cancer and sentinel-node micrometastases (IBCSG 23-01): 10-year follow-up of a randomised, controlled phase 3 trial. Lancet Oncol. 2018, 19, 1385–1393. [Google Scholar] [CrossRef]
- Droeser, R.; Frey, D.; Oertli, D.; Kopelman, D.; Peeters, M.B.-V.; Giuliano, A.; Dalberg, K.; Kallam, R.; Nordmann, A. Volume-controlled vs no/short-term drainage after axillary lymph node dissection in breast cancer surgery: A meta-analysis. Breast 2009, 18, 109–114. [Google Scholar] [CrossRef]
- He, X.-D.; Guo, Z.-H.; Tian, J.-H.; Yang, K.-H.; Xie, X.-D. Whether drainage should be used after surgery for breast cancer? A systematic review of randomized controlled trials. Med. Oncol. 2010, 28, 22–30. [Google Scholar] [CrossRef] [PubMed]
- Van Bemmel AJ, M.; Van De Velde CJ, H.; Schmitz, R.F.; Liefers, G.J. Prevention of seroma formation after axillary dissection in breast cancer: A systematic review. Eur. J. Surg. Oncol. 2011, 37, 829–835. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ten Wolde, B.; van den Wildenberg, F.J.; Polat, F.; de Wilt, J.H.; Strobbe, L.J. Can gentamicin-collagen sponges prevent seroma formation following mastectomy? Clin. Breast Cancer 2018, 18, e1023–e1026. [Google Scholar] [CrossRef]
- De Oliveira, M.M.F.; Gurgel, M.S.C.; Amorim, B.J.; Ramos, C.D.; Derchain, S.; Furlan-Santos, N.; Dos Santos, C.C.; Sarian, L.O. Long term effects of manual lymphatic drainage and active exercises on physical morbidities, lymphoscintigraphy parameters and lymphedema formation in patients operated due to breast cancer: A clinical trial. PLoS ONE 2018, 13, e0189176. [Google Scholar] [CrossRef] [PubMed]
- Uideline on The Clinical Investigation of Plasma Derived Fibrin Sealant/Haemostatic Products (CPMP/BPWG/1089/00). Available online: https://www.ema.europa.eu/en/documents/scientific-guideline/guideline-clinical-investigation-plasma-derived-fibrin-sealant/haemostatic-products-cpmp/bpwg/1089/00_en.pdf (accessed on 10 January 2021).
- Gasparri, M.L.; Ruscito, I.; Bolla, D.; Panici, P.B.; Mueller, M.D.; Papadia, A. The Efficacy of Fibrin Sealant Patches in Reducing the Incidence of Lymphatic Morbidity after Radical Lymphadenectomy: A Meta-Analysis. Int. J. Gynecol. Cancer 2017, 27, 1283–1292. [Google Scholar] [CrossRef] [PubMed]
- Roberts, I.V.; Bukhary, D.; Valdivieso, C.Y.L.; Tirelli, N. Fibrin matrices as (injectable) biomaterials: Formation, clinical use, and molecular engineering. Macromol. Biosci. 2020, 20, 1900283. [Google Scholar] [CrossRef]
- Fang, C.-L.; Changchien, C.-H.; Chen, M.-S.; Hsu, C.-H.; Chen, W.-C.; Yang, H.-Y.; Lin, Y.-L. The Effects of Combining Progressive Tension Sutures, Closed Drain, and Fibrin Sealant in Abdominoplasty Wound After Deep Inferior Epigastric Perforator Flap Harvesting. Ann. Plast. Surg. 2020, 84, S89–S93. [Google Scholar] [CrossRef]
- Vinchant, M.; Bonneau, C.; Lesavre, M.; Akerman, G.; Raiffort, C.; Barranger, E.; Bricou, A. Interest of a thrombin and fibrinogen combipatch in preventing breast cancer seroma after lymph node dissection. Gynecol. Obstet. Fertil. 2013, 41, 583–587. [Google Scholar] [CrossRef]
- Benevento, R.; Santoriello, A.; Pellino, G.; Sciaudone, G.; Candilio, G.; De Fatico, G.S.; Selvaggi, F.; Canonico, S. The effects of low-thrombin fibrin sealant on wound serous drainage, seroma formation and length of postoperative stay in patients undergoing axillary node dissection for breast cancer. A randomized controlled trial. Int. J. Surg. 2014, 12, 1210–1215. [Google Scholar] [CrossRef] [Green Version]
- Berger, A.; Tempfer, C.; Hartmann, B.; Kornprat, P.; Rossmann, A.; Neuwirth, G.; Tulusan, A.; Kubista, E. Sealing of Postoperative Axillary Leakage After Axillary Lymphadenectomy Using a Fibrin Glue Coated Collagen Patch: A Prospective Randomised Study. Breast Cancer Res. Treat. 2001, 67, 9–14. [Google Scholar] [CrossRef]
- Cipolla, C.; Fricano, S.; Vieni, S.; Graceffa, G.; Licari, G.; Torcivia, A.; Latteri, M.A. Does the use of fibrin glue prevent seroma formation after axillary lymphadenectomy for breast cancer? A prospective randomized trial in 159 patients. J. Surg. Oncol. 2010, 101, 600–603. [Google Scholar] [CrossRef] [PubMed]
- Conversano, A.; Mazouni, C.; Thomin, A.; Gaudin, A.; Fournier, M.; Rimareix, F.; Bonastre, J. Use of Low-Thrombin Fibrin Sealant Glue After Axillary Lymphadenectomy for Breast Cancer to Reduce Hospital Length and Seroma. Clin. Breast Cancer 2017, 17, 293–297. [Google Scholar] [CrossRef] [PubMed]
- Docimo, G.; Limongelli, P.; Conzo, G.; Gili, S.; Bosco, A.; Rizzuto, A.; Amoroso, V.; Marsico, S.; Leone, N.; Esposito, A.; et al. Axillary lymphadenectomy for breast cancer in elderly patients and fibrin glue. BMC Surg. 2013, 13, S8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gilly, F.N.; Francois, Y.; Sayag-Beaujard, A.C.; Glehen, O.; Brachet, A.; Vignal, J. Prevention of lymphorrhea by means of fibrin glue after axillary lymphadenectomy in breast cancer: Prospective randomized trial. Eur. Surg. Res. 1998, 30, 439–443. [Google Scholar] [CrossRef]
- Hivelin, M.; Heusse, J.L.; Matar, N.; Lepage, C.; Lantieri, L. Fibrin sealant decreases postoperative drainage in immediate breast reconstruction by deep inferior epigastric perforator flap after mastectomy with axillary dissection. Microsurgery 2010, 31, 18–25. [Google Scholar] [CrossRef] [PubMed]
- Ko, E.; Han, W.; Cho, J.; Lee, J.W.; Kang, S.Y.; Jung, S.-Y.; Kim, E.-K.; Hwang, K.-T.; Noh, D.-Y. Fibrin Glue Reduces the Duration of Lymphatic Drainage after Lumpectomy and Level II or III Axillary Lymph Node Dissection for Breast Cancer: A Prospective Randomized Trial. J. Korean Med. Sci. 2009, 24, 92–96. [Google Scholar] [CrossRef] [PubMed]
- Medl, M.; Mayerhofer, K.; Peters-Engl, C.; Mahrhofer, P.; Huber, S.; Buxbaum, P.; Sevelda, P.; Leodolter, S. The application of fibrin glue after axillary lymphadenectomy in the surgical treatment of human breast cancer. Anticancer Res. 1995, 15, 2843–2845. [Google Scholar] [PubMed]
- Miri Bonjar, M.R.; Maghsoudi, H.; Samnia, R.; Saleh, P.; Parsafar, F. Efficacy of fibrin glue on seroma formation after breast surgery. Int. J. Breast Cancer 2012, 2012, 643132. [Google Scholar] [CrossRef] [PubMed]
- Moore, M.; E Burak, W.; Nelson, E.; Kearney, T.; Simmons, R.; Mayers, L.; Spotnitz, W.D. Fibrin sealant reduces the duration and amount of fluid1 drainage after axillary dissection: A randomized prospective clinical trial. J. Am. Coll. Surg. 2001, 192, 591–599. [Google Scholar] [CrossRef]
- Navarro-Rodríguez, E.; Gómez-Luque, I.; Díaz-Jiménez, N.; Rioja-Torres, P.; Bascuñana-Estudillo, G.; Ruiz-Rabelo, J.F.; Ciria-Bru, R.; Álvarez-Benito, M.; Rufián-Peña, S.; Briceño-Delgado, J. Effectiveness of an absorbable fibrin sealant patch to reduce lymphoceles formation after axillary lymphadenectomy for breast cancer: A matched-pair analysis. Am. J. Surg. 2014, 208, 824–830. [Google Scholar] [CrossRef] [PubMed]
- Neuss, H.; Raue, W.; Koplin, G.; Schwenk, W.; Reetz, C.; Mall, J.W. Intraoperative Application of Fibrin Sealant does not Reduce the Duration of Closed Suction Drainage Following Radical Axillary Lymph Node Dissection in Melanoma Patients: A Prospective Randomized Trial in 58 Patients. World J. Surg. 2008, 32, 1450–1455. [Google Scholar] [CrossRef] [PubMed]
- Piñero-Madrona, A.; Castellanos-Escrig, G.; Abrisqueta-Carrión, J.; Canteras-Jordana, M. Prospective randomized controlled study to assess the value of a hemostatic and sealing agent for preventing seroma after axillary lymphadenectomy. J. Surg. Oncol. 2016, 114, 423–427. [Google Scholar] [CrossRef] [PubMed]
- Ruggiero, R.; Procaccini, E.; Piazza, P.; Docimo, G.; Iovino, F.; Antoniol, G.; Irlandese, E.; Gili, S.; Schiavo, F.L. Effectiveness of fibrin glue in conjunction with collagen patches to reduce seroma formation after axillary lymphadenectomy for breast cancer. Am. J. Surg. 2008, 196, 170–174. [Google Scholar] [CrossRef] [PubMed]
- Ruggiero, R.; Procaccini, E.; Gili, S.; Cremone, C.; Parmeggiani, D.; Conzo, G.; Docimo, L.; Sparavigna, L.; Gubitosi, A.; Docimo, G.; et al. New trends on fibrin glue in seroma after axillary lymphadenectomy for breast cancer. G. Chir. 2009, 30, 306–310. [Google Scholar]
- Ruggiero, R.; Docimo, G.; Gubitosi, A.; Conzo, G.; Tolone, S.; Gili, S.; Bosco, A.; Docimo, L. Axillary lymphadenectomy for breast cancer and fibrin glue. Ann. Ital. Chir. 2012, 85, 88–92. [Google Scholar]
- Segura-Castillo, J.L.; Estrada-Rivera, O.; Castro-Cervantes, J.M.; Cortés-Flores, A.O.; Velázquez-Ramírez, G.A.; González-Ojeda, A. Reduction of lymphatic drainage posterior to modified radical mastectomy with the application of fibrin glue. Cirugía Cir. 2005, 73, 345–350. [Google Scholar]
- Swan, M.C.; Oliver, D.W.; Cassell OC, S.; Coleman, D.J.; Williams, N.; Morritt, D.G.; Giele, H.P. Randomized controlled trial of fibrin sealant to reduce postoperative drainage following elective lymph node dissection. Br. J. Surg. 2011, 98, 918–924. [Google Scholar] [CrossRef] [PubMed]
- Udén, P.; Aspegren, K.; Balldin, G.; Garne, J.P.; A Larsson, S. Fibrin adhesive in radical mastectomy. Eur. J. Surg. 1993, 159, 263–265. [Google Scholar]
- Ulusoy, A.N.; Polat, C.; Alvur, M.; Kandemir, B.; Bulut, F. Effect of Fibrin Glue on Lymphatic Drainage and on Drain Removal Time After Modified Radical Mastectomy: A Prospective Randomized Study. Breast J. 2003, 9, 393–396. [Google Scholar] [CrossRef]
- Vaxman, F.; Kolbe, A.; Stricher, F.; Zund, D.; Volkmar, P.; Gros, D.; Grenier, J.; Strieker, F. Does Fibrin Glue Improve Drainage after Axillary Lymph Node Dissection? Prospective and Randomized Study in Humans. Eur. Surg. Res. 1995, 27, 346–352. [Google Scholar] [CrossRef]
- Weber, W.P.; Tausch, C.; Hayoz, S.; Fehr, M.K.; Ribi, K.; Hawle, H.; Knauer, M. Impact of a surgical sealing patch on lymphatic drainage after axillary dissection for breast cancer: The SAKK 23/13 multicenter randomized phase III trial. Ann. Surg. Oncol. 2018, 25, 2632–2640. [Google Scholar] [CrossRef]
- Gonzalez, E.A.; Saltzstein, E.C.; Riedner, C.S.; Nelson, B.K. Seroma Formation Following Breast Cancer Surgery. Breast J. 2003, 9, 385–388. [Google Scholar] [CrossRef] [PubMed]
- Srivastava, V.; Basu, S.; Shukla, V.K. Seroma Formation after Breast Cancer Surgery: What We Have Learned in the Last Two Decades. J. Breast Cancer 2012, 15, 373–380. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hashemi, E.; Kaviani, A.; Najafi, M.; Ebrahimi, M.; Hooshmand, H.; Montazeri, A. Seroma formation after surgery for breast cancer. World J. Surg. Oncol. 2004, 2, 44. [Google Scholar] [CrossRef] [Green Version]
- Woodworth, P.A.; McBoyle, M.F.; Helmer, S.D.; Beamer, R.L. Seroma formation after breast cancer surgery: Incidence and predicting factors/discussions. Am. Surg. 2000, 66, 444. [Google Scholar]
- Stanczyk, M.; Grala, B.; Zwierowicz, T.; Maruszynski, M. Surgical resection for persistent seroma, following modified radical mastectomy. World J. Surg. Oncol. 2007, 5, 104. [Google Scholar] [CrossRef] [Green Version]
- Gauthier, T.; Garuchet-Bigot, A.; Marin, B.; Mollard, J.; Loum, O.; Fermeaux, V.; Jammet, I.; Kanoun, D.; Maubon, A.; Aubard, Y. Lanreotide autogel 90 mg and lymphorrhea prevention after axillary node dissection in breast cancer: A phase III double blind, randomized, placebo-controlled trial. Eur. J. Surg. Oncol. 2012, 38, 902–909. [Google Scholar] [CrossRef]
- O’Hea, B.J.; Ho, M.N.; Petrek, J.A. External compression dressing versus standard dressing after axillary lymphadenectomy. Am. J. Surg. 1999, 177, 450–453. [Google Scholar] [CrossRef]
- Shamley, D.R.; Barker, K.; Simonite, V.; Beardshaw, A. Delayed versus immediate exercises following surgery for breast cancer: A systematic review. Breast Cancer Res. Treat. 2005, 90, 263–271. [Google Scholar] [CrossRef]
- Gambardella, C.; Clarizia, G.; Patrone, R.; Offi, C.; Mauriello, C.; Romano, R.; Filardo, M.; Conzo, A.; Sanguinetti, A.; Polistena, A.; et al. Advanced hemostasis in axillary lymph node dissection for locally advanced breast cancer: New technology devices compared in the prevention of seroma formation. BMC Surg. 2019, 18, 125. [Google Scholar] [CrossRef]
- Simonato, A.; Varca, V.; Esposito, M.; Venzano, F.; Carmignani, G. The Use of a Surgical Patch in the Prevention of Lymphoceles After Extraperitoneal Pelvic Lymphadenectomy for Prostate Cancer: A Randomized Prospective Pilot Study. J. Urol. 2009, 182, 2285–2290. [Google Scholar] [CrossRef]
- Hester Jr, T.R.; Shire, J.R.; Nguyen, D.B.; Gerut, Z.E.; Chen, A.H.; Diamond, J.; Desmond, J.C.; Silvati-Fidell, L.; Abrams, S.Z.; Rohrich, R.J. Randomized, controlled, phase 3 study to evaluate the safety and efficacy of fibrin sealant VH S/D 4 s-apr (Artiss) to improve tissue adherence in subjects undergoing rhytidectomy. Aesthetic Surg. J. 2013, 33, 487–496. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yamamoto, K.T.; DeJoseph, L.M. Efficacy and Safety of Artiss Fibrin Tissue Sealant Use in Rhytidectomy: A Review of 120 Cases. Surg. J. 2017, 3, e69–e74. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- van Bastelaar, J.; Theunissen, L.L.; Snoeijs, M.G.; Beets, G.L.; Vissers, Y.L. Flap fixation using tissue glue or sutures appears to reduce seroma aspiration after mastectomy for breast cancer. Clin. Breast Cancer 2017, 17, 316–321. [Google Scholar] [CrossRef] [PubMed]
- Jain, P.K.; Sowdi, R.; Anderson, A.D.G.; MacFie, J. Randomized clinical trial investigating the use of drains and fibrin sealant following surgery for breast cancer. BJS 2003, 91, 54–60. [Google Scholar] [CrossRef] [PubMed]
- Harrison, C.; Remoundos, D.D.; Harvey, K.L.; Stoker, G.V.; MacLean, G.; Adwani, A.; Roy, P.G. Increasing the incidence of drain-free day-case mastectomies with the use of a fibrin tissue sealant; data from a single surgical center in the United Kingdom. Breast J. 2019, 25, 1090–1096. [Google Scholar] [CrossRef] [PubMed]
- Sajid, M.S.; Hutson, K.H.; Rapisarda, I.F.F.; Bonomi, R. Fibrin glue instillation under skin flaps to prevent seroma-related morbidity following breast and axillary surgery. Cochrane Database Syst. Rev. 2013, 5, CD009557. [Google Scholar] [CrossRef] [PubMed]
- ClinicalTrials.gov. Identifier: NCT00504582. Available online: https://clinicaltrials.gov/ct2/show/NCT00504582 (accessed on 10 January 2021).
- Fagotti, A.; Costantini, B.; Fanfani, F.; Vizzielli, G.; Rossitto, C.; Lecca, A.; Scambia, G. Risk of Postoperative Pelvic Abscess in Major Gynecologic Oncology Surgery: One-Year Single-Institution Experience. Ann. Surg. Oncol. 2010, 17, 2452–2458. [Google Scholar] [CrossRef] [PubMed]
- Perniola, G.; Antonilli, M.; Gasparri, M.L. Let’s Think Twice Before Abandoning Fibrillar Oxidized Regenerated Cellulose. Ann. Surg. Oncol. 2011, 18, 292. [Google Scholar] [CrossRef] [PubMed]


| Author (Ref) | Tumor Type | Pts Study Group/Tot | Fibrin Device | Quantity | NACT N (%) | Criteria for Drainage Removal (mL/24 h) |
|---|---|---|---|---|---|---|
| BENEVENTO 2014 [14] | Breast cancer | 30/60 | Tisseel glue | 4 mL | NR | ≤30 |
| BERGER 2001 [15] | Breast cancer | 30/60 | TachoSil patch | 1,5 patches | Excluded | ≤70 |
| CIPOLLA 2010 [16] | Breast cancer | 80/159 | Glue | 2 mL | Excluded | ≤80 |
| CONVERSANO 2017 [17] | Breast cancer | 49/149 | Tisseel glue | 4 mL | 22 (44.9%) study group 23 (23%) control group | ≤50 |
| DOCIMO 2013 [18] | Breast cancer | 15/30 | Tisseel glue | 2 mL | NR | ≤100 |
| GILLY 1994 [19] | Breast cancer | 50/108 | Tisseel glue | 2 mL | Excluded | After 6 days |
| HIVELIN 2011 [20] | Breast cancer | 15/30 | Tisseel glue | 5 mL | NR | ≤30 |
| KO 2009 [21] | Breast cancer | 50/100 | glue | 2 mL | Excluded | ≤30 |
| MEDL 1995 [22] | Breast cancer | 67/142 | TachoSil patch | 3 patches | 21 (29.2%) study group 21 (30%) control group | ≤30 |
| MIRI BONJAR 2012 [23] | Breast cancer | 31/60 | glue | 2 mL | NR | ≤30 |
| MOORE 2001 [24] | Breast cancer | 59/80 | glue | 4 mL, 8 mL, 16 mL | NR | ≤40 |
| NAVARRO-RODRIGUEZ 2014 [25] | Breast cancer | 86/258 | TachoSil patch | 2 patches | 16 (18.6%) study group 32 (28.6%) C | ≤50 |
| NEUSS 2008 [26] | Melanoma | 29/58 | Tisseel glue | 2 mL | NR | ≤50 |
| PINERO-MADRONA 2016 [27] | Melanoma, Breast cancer, Hodgkin’s disease | 44/91 | TachoSil patch | 3 patches | 24 | ≤50 |
| RUGGIERO 2008 [28] | Breast cancer | 25/50 | Glue + patch | 2 mL | NR | ≤100 |
| RUGGIERO 2009 [29] | Breast cancer | 45/90 | Tisseel glue | 2 mL | NR | ≤100 |
| RUGGIERO 2014 [30] | Breast cancer | 40/80 | Tisseel glue | 2 mL | NR | ≤100 |
| SEGURA-CASTILLO 2005 [31] | Breast cancer | 22/43 | Quixil gel | 10 mL | 11 (20%) study group 10 (20%) control group | ≤50 |
| SWAN 2011 [32] | Melanoma Others | 18/36 | Tisseel glue | 4 mL | NR | ≤30 |
| UDEN 1992 [33] | Breast cancer | 36/68 | Tisseel glue | 2 mL | NR | ≤100 |
| ULUSOY 2003 [34] | Breast cancer | 27/54 | Tisseel glue | 4 mL | Excluded | ≤20 |
| VAXMAN 1995 [35] | Breast cancer | 20/40 | Tisseel glue | 5 mL | NR | ≤10 |
| WEBER 2018 [36] | Breast cancer | 67/142 | TachoSil patch | 3 patches | 21 (29.2%) study group 21 (30%) control group | ≤30 |
| Author (ref) | Breast Surgery | Level of Dissection | N. Nodes Removed (Median) | N. Positive Nodes (Median) | Pts with Positive Nodes |
|---|---|---|---|---|---|
| BENEVENTO 2014 [14] | Quadrantectomy, mastectomy | III | 23.7 study group 24 control group | NR | NR |
| BERGER 2001 [15] | Lumpectomy, mastectomy | II | NR | NR | NR |
| CIPOLLA 2010 [16] | Quadrantectomy, mastectomy | III | 16.6 study group 17.4 control group | NR | 46 study group 3 control group |
| CONVERSANO 2017 [17] | Quadrantectomy or ALND only | II | 14.5 study group 14 control group | 1 study group 1 control group | NR |
| DOCIMO 2013 [18] | Quadrantectomy, mastectomy | NR | NR | NR | NR |
| GILLY 1994 [19] | Modified radical mastectomy, sector mastectomy | III | 10.6 study group 0.8 control group | 1.9 study group 1.9 control group | NR |
| HIVELIN 2011 [20] | Mastectomy | NR | NR | NR | NR |
| KO 2009 [21] | Quadrantectomy | I-III | 12.6 study group 12.5 control group | 0.8 study group 0.8 control group | NR |
| MEDL 1995 [22] | Quadrantectomy, mastectomy | NR | 12.8 study group 3.9 control group | 4.2study group; 4.4 control group | NR |
| MIRI BONJAR 2012 [23] | Quadrantectomy, mastectomy | NR | 14.7study group 4.2 control group | 1.2 study group 2.5 control group | NR |
| MOORE 2001 [24] | Lumpectomy, mastectomy | NR | NR | NR | NR |
| NAVARRO-RODRIGUEZ 2014 [25] | Quadrantectomy, mastectomy | III | 14.95 study group 15.66 control group | NR | 64 Study group 102 control group |
| NEUSS 2008 [26] | Null | III | 16 study group ; 15 control group | 3study group 3 control group | NR |
| PIERO MADRONA [27] | NR | II; III | 16.59 study group 18.36 control group | NR | NR |
| RUGGIERO 2008 [28] | Quadrantectomy, mastectomy | I; II | 18.1 study group 18.7 control group | 12 study group 13 control group | NR |
| RUGGIERO 2009 [29] | Quadrantectomy, mastectomy | I; II | NR | NR | NR |
| RUGGIERO 2014 [30] | Quadrantectomy, mastectomy | I; II | NR | NR | NR |
| SEGURA-CASTILLO 2005 [31] | Mastectomy | III | NR | NR | NR |
| SWAN 2011 [32] | NR | III | 18 study group 12.5 control group | NR | NR |
| UDEN 1992 [33] | Mastectomy | III | NR | NR | NR |
| ULUSOY 2003 [34] | Mastectomy | III | NR | 5.7 study group 2.66 control group | NR |
| VAXMAN 1995 [35] | Quadrantectomy, Patey’s mastectomy | NR | 10.8 study group 9.3 control group | 2.9 study group 2.1 control group | 11 study group 11 control group |
| WEBER 2018 [36] | Quadrantectomy | II; III | 16 study group 18.5 control group | 2 study group 3 control group | NR |
| Type of Bias | Selection Bias | Performance Bias | Detection Bias | Attrition Bias | |
|---|---|---|---|---|---|
| Study (Ref) | |||||
| BENEVENTO 2014 [14] | Low risk | Intermediate risk | Low risk | Intermediate risk | |
| BERGER 2001 [15] | Low risk | Intermediate risk | Intermediate risk | Intermediate risk | |
| CIPOLLA 2010 [16] | Low risk | Intermediate risk | Low risk | Intermediate risk | |
| CONVERSANO 2017 [17] | Intermediate risk | Intermediate risk | Intermediate risk | Intermediate risk | |
| DOCIMO 2013 [18] | NA | Intermediate risk | Low risk | Intermediate risk | |
| GILLY 1994 [19] | Low risk | High risk | Low risk | Intermediate risk | |
| HIVELIN 2011 [20] | NA | NA | NA | NA | |
| KO 2009 [21] | High risk | Low risk | Low risk | Low risk | |
| MEDL 1995 [22] | High risk | High risk | Intermediate risk | Intermediate risk | |
| MIRI BONJAR 2012 [23] | High risk | Low risk | Low risk | Intermediate risk | |
| MOORE 2001 [24] | Low risk | Low risk | Low risk | Low risk | |
| NAVARRO-RODRIGUEZ 2014 [25] | Low risk | Intermediate risk | Low risk | Intermediate risk | |
| NEUSS 2008 [26] | NA | Intermediate risk | Low risk | Intermediate risk | |
| PINERO MADRONA [27] | NA | Low risk | Low risk | Low risk | |
| RUGGIERO 2008 [28] | Intermediate risk | Intermediate risk | Low risk | Intermediate risk | |
| RUGGIERO 2009 [29] | Intermediate risk | Low risk | Low risk | Low risk | |
| RUGGIERO 2014 [30] | Intermediate risk | Low risk | Intermediate risk | Low risk | |
| SEGURA-CASTILLO 2005 [31] | Low risk | Intermediate risk | Low risk | High risk | |
| SWAN 2011 [32] | NA | Low risk | Low risk | Low risk | |
| UDEN 1992 [33] | Low risk | Intermediate risk | Intermediate risk | Intermediate risk | |
| ULUSOY 2003 [34] | Low risk | Low risk | High risk | Low risk | |
| VAXMAN 1995 [35] | NA | Low risk | Low risk | Low risk | |
| WEBER 2018 [36] | Low risk | Low risk | Low risk | Low risk | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gasparri, M.L.; Kuehn, T.; Ruscito, I.; Zuber, V.; Di Micco, R.; Galiano, I.; Navarro Quinones, S.C.; Santurro, L.; Di Vittorio, F.; Meani, F.; et al. Fibrin Sealants and Axillary Lymphatic Morbidity: A Systematic Review and Meta-Analysis of 23 Clinical Randomized Trials. Cancers 2021, 13, 2056. https://doi.org/10.3390/cancers13092056
Gasparri ML, Kuehn T, Ruscito I, Zuber V, Di Micco R, Galiano I, Navarro Quinones SC, Santurro L, Di Vittorio F, Meani F, et al. Fibrin Sealants and Axillary Lymphatic Morbidity: A Systematic Review and Meta-Analysis of 23 Clinical Randomized Trials. Cancers. 2021; 13(9):2056. https://doi.org/10.3390/cancers13092056
Chicago/Turabian StyleGasparri, Maria Luisa, Thorsten Kuehn, Ilary Ruscito, Veronica Zuber, Rosa Di Micco, Ilaria Galiano, Siobana C. Navarro Quinones, Letizia Santurro, Francesca Di Vittorio, Francesco Meani, and et al. 2021. "Fibrin Sealants and Axillary Lymphatic Morbidity: A Systematic Review and Meta-Analysis of 23 Clinical Randomized Trials" Cancers 13, no. 9: 2056. https://doi.org/10.3390/cancers13092056








