Enterococcus hirae Mitral Valve Infectious Endocarditis: A Case Report and Review of the Literature
Abstract
1. Introduction
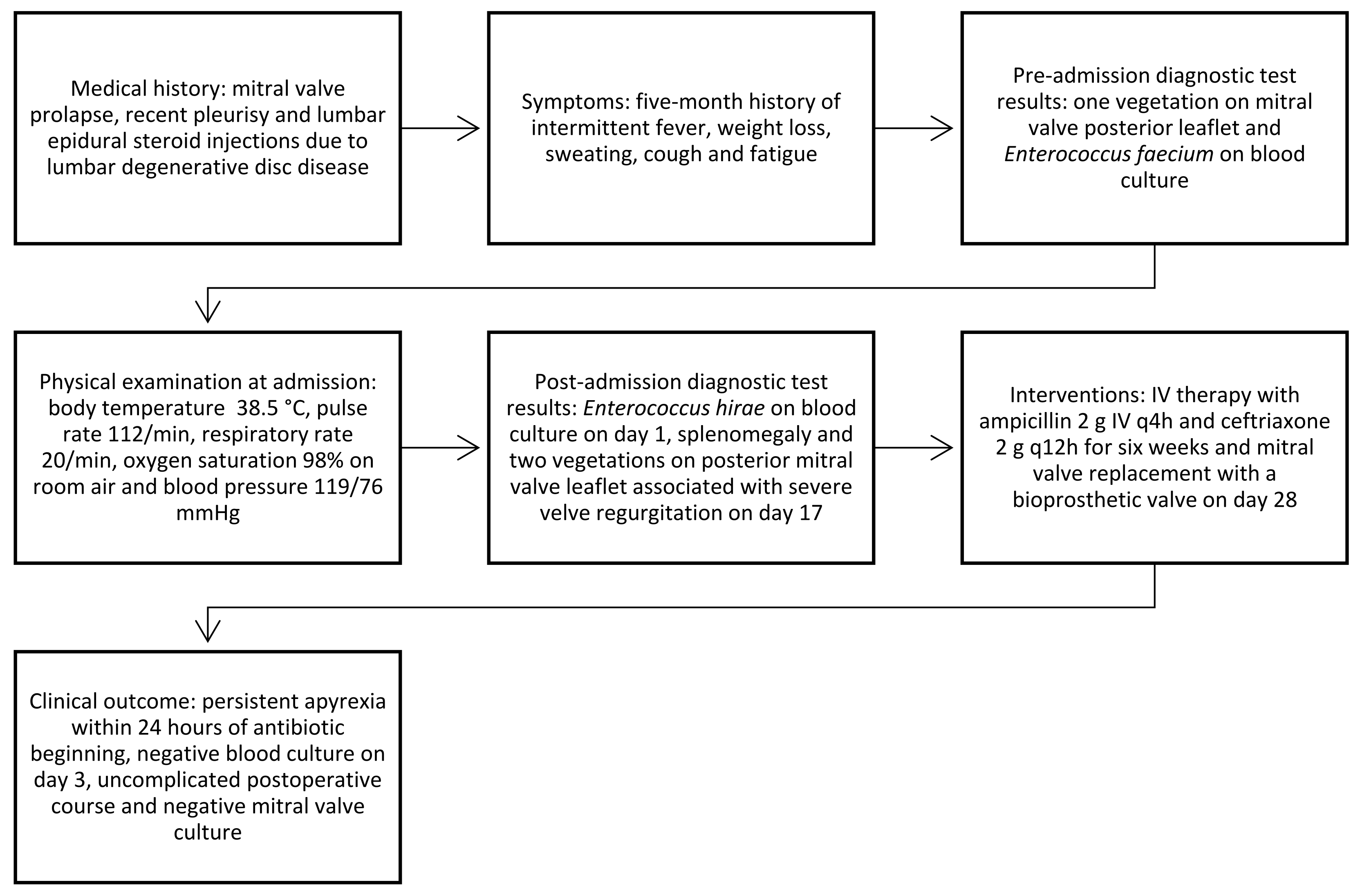
2. Case Report
3. Literature Research
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Piccininiwe, D.; Bernasconi, E.; Di Benedetto, C.; Martinetti Lucchini, G.; Bongiovani, M. Enterococcus hirae infections in the clinical practice. Infect. Dis. 2023, 55, 71–73. [Google Scholar] [CrossRef] [PubMed]
- Gilad, J.; Borer, A.; Riesenberg, K.; Peled, N.; Shnaider, A.; Schlaeffer, F. Enterococcus hirae septicemia in a patient with end-stage renal disease undergoing hemodialysis. Eur. J. Clin. Microbiol. Infect. Dis. 1998, 17, 576–577. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.-H.; Chon, J.-W.; Jeong, H.-W.; Song, K.-Y.; Kim, D.-H.; Bae, D.; Kim, H.; Seo, K.-H. Identification and phylogenetic analysis of Enterococcus isolates using MALDI-TOF MS and VITEK 2. AMB Expr. 2023, 13, 21. [Google Scholar] [CrossRef] [PubMed]
- Fowler, V.G.; Durack, D.T.; Selton-Suty, C.; Athan, E.; Bayer, A.S.; Chamis, A.L.; Dahl, A.; DiBernardo, L.; Durante-Mangoni, E.; Duval, X.; et al. The 2023 Duke-International Society for Cardiovascular Infectious Diseases Criteria for Infective Endocarditis: Updating the Modified Duke Criteria. Clin. Infect. Dis. 2023, ciad271. [Google Scholar] [CrossRef] [PubMed]
- Poyart, C.; Lambert, T.; Morand, P.; Abassade, P.; Quesne, G.; Baudouy, Y.; Trieu-Cuot, P. Native valve endocarditis due to Enterococcus hirae. J. Clin. Microbiol. 2002, 40, 2689–2690. [Google Scholar] [CrossRef] [PubMed]
- Talarmin, J.P.; Pineau, S.; Guillouzouic, A.; Boutoille, D.; Giraudeau, C.; Reynaud, A.; Lepelletier, D.; Corvec, S. Relapse of Enterococcus hirae prosthetic valve endocarditis. J. Clin. Microbiol. 2011, 49, 1182–1184. [Google Scholar] [CrossRef] [PubMed]
- Anghinah, R.; Watanabe, R.G.S.; Simabukuro, M.M.; Guariglia, C.; Pinto, L.F. Native valve endocarditis due to Enterococcus hirae presenting as a neurological deficit. Case Rep. Neurol. Med. 2013, 2013, 636070. [Google Scholar] [PubMed]
- Ebeling, C.G.; Romito, B.T. Aortic valve endocarditis from Enterococcus hirae infection. Bayl. Univ. Med. Cent. Proc. 2019, 32, 249–250. [Google Scholar] [CrossRef] [PubMed]
- Pinkes, M.E.; White, C.; Wong, C.S. Native-Valve Enterococcus hirae endocarditis: A case report and review of the literature. BMC Infect. Dis. 2019, 19, 891. [Google Scholar] [CrossRef] [PubMed]
- Winther, M.; Dalager-Pedersen, M.; Tarpgaard, I.H.; Nielsen, H.L. First Danish case of infective endocarditis caused by Enterococcus hirae. BMJ Case Rep. 2020, 13, e237950. [Google Scholar] [CrossRef] [PubMed]
- Iung, B. Infective endocarditis. Epidemiology, pathophysiology and histopathology. Presse Med. 2019, 48, 513–521. [Google Scholar] [CrossRef] [PubMed]
- Moreno, B.; Bolea, R.; Andrés-Lasheras, S.; Sevilla, E.; Samper, S.; Morales, M.; Vargas, A.; Chirino-Trejo, M.; Badiola, J.J. Antimicrobial Susceptibilities and Phylogenetic Analyses of Enterococcus hirae Isolated from Broilers with Valvular Endocarditis. Avian Dis. 2019, 63, 318–324. [Google Scholar] [CrossRef] [PubMed]
- Vinh, D.C.; Nichol, K.A.; Rand, F.; Embil, J.M. Native-valve bacterial endocarditis caused by Lactococcus garvieae. Diagn. Microbiol. Infect. Dis. 2006, 56, 91–94. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, T.; Ishikawa, K.; Matsuo, T.; Kawai, F.; Uehara, Y.; Mori, N. Enterococcus hirae bacteremia associated with acute pyelonephritis in a patient with alcoholic cirrhosis: A case report and literature review. BMC Infect. Dis. 2021, 21, 999. [Google Scholar] [CrossRef] [PubMed]
- Lévesque, S.; Dufresne, P.J.; Soualhine, H.; Domingo, M.-C.; Bekal, S.; Lefebvre, B.; Tremblay, C. A Side by Side Comparison of Bruker Biotyper and VITEK MS: Utility of MALDI-TOF MS Technology for Microorganism Identification in a Public Health Reference Laboratory. PLoS ONE 2015, 10, e0144878. [Google Scholar] [CrossRef] [PubMed]
- Habib, G.; Lancellotti, P.; Antunes, M.J.; Bongiorni, M.G.; Casalta, J.P.; Del Zotti, F.; Dulgheru, R.; El Khoury, G.; Erba, P.A.; Iung, B.; et al. 2015 ESC guidelines for the management of infective endocarditis: The task force for the management of infective endocarditis of the European Society of cardiology (ESC). Endorsed by: European association for Cardio-Thoracic surgery (EACTS), the European association of nuclear medicine (EANM). Eur. Heart J. 2015, 36, 3075–3128. [Google Scholar] [PubMed]
- Freeman, L.; Milkovits, A.; McDaniel, L.; Everson, N. Evaluation of penicillin-gentamicin and dual beta-lactam therapies in Enterococcus faecalis infective endocarditis. Int. J. Antimicrob. Agents 2022, 59, 106522. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Hidalgo, N.; Almirante, B.; Gavaldà, J.; Gurgui, M.; Peña, C.; De Alarcón, A.; Ruiz, J.; Vilacosta, I.; Montejo, M.; Vallejo, N.; et al. Ampicillin plus ceftriaxone is as effective as ampicillin plus gentamicin for treating enterococcus faecalis infective endocarditis. Clin. Infect. Dis. 2013, 56, 1261–1268. [Google Scholar] [CrossRef] [PubMed]
| E. faecium | Sensitivity | M.I.C. | E. hirae | Sensitivity | M.I.C. |
|---|---|---|---|---|---|
| Ampicillin | S | <=2 | Ampicillin | S | <=1 |
| Linezolid | S | 2 | Linezolid | S | 1 |
| Teicoplanin | S | <=0.5 | Teicoplanin | S | <=0.5 |
| Tigecycline | S | <=0.12 | |||
| Vancomycin | S | <=0.5 | Vancomycin | S | <=0.5 |
| Gentamicin (SYN) | S | <=500 |
| Age | Sex | Medical History | Valve Involvement | Predisposing Risk Factors | Identification | Treatment | Relapse | |
|---|---|---|---|---|---|---|---|---|
| Poyart et al., 2002 [5] | 72 | M | 1-month history of fever, chills, progressive malaise, generalized weakness | Vegetations involving the left and right aortic-valve leaflets | Aortic insufficiency. History of coronary artery disease and percutaneous transluminal coronary angioplasty | sodAint gene sequencing | Ampicillin plus gentamicin followed by rifampin for a total of six weeks. | Yes, treated with vancomycin followed by amoxicillin plus gentamicin for a total of eight weeks; aortic valve replacement with a homograft |
| Talarmin et al., 2011 [6] | 78 | F | 5-month history of fever, generalized weakness, and a 7 kg weight loss | Normal TEE during the first presentation, vegetation on aortic prosthetic valve at relapse | Aortic valve replacement with a bioprosthetic valve | sodAint gene sequencing | Amoxicillin and gentamicin followed by rifampin for a total of six weeks | Yes, treated with amoxicillin and gentamicin followed by rifampin for a total of six weeks |
| Anghinah et al., 2013 [7] | 56 | M | Dysarthria, dysphagia, and left hemiparesis are associated with recent weight loss, fatigue, depressive symptoms, and evening fever | Vegetations involving aortic and mitral valves | Cardiac arrhythmia with surgical ablation and patent foramen ovale | Unknown | Rifampin plus ampicillin followed by amoxicillin for a total of six weeks; aortic valve replacement by a biological valve, plastic of the mitral valve, and correction of the foramen ovale. | No |
| Ebeling et al., 2019 [8] | 70 | M | 3- month history of bilateral leg edema, dyspnea on exertion, fatigue, mild weight loss | Vegetation on aortic valve, purulent aortic root abscesses | Severe aortic regurgitation, moderate anterolateral hypokinesis | MALDI-TOF | Ampicillin followed by penicillin G plus ceftriaxone for a total of six weeks, then indefinite chronic suppressive therapy with oral penicillin; aortic valve replacement | No |
| Pinkes et al., 2019 [9] | 64 | F | Fever, hypotension, 2-week history of lightheadedness | Multiple small vegetations on aortic valve, root abscess beneath the right coronary cusp | Severe aortic stenosis, bicuspid aortic valve | MALDI-TOF | Ampicillin and ceftriaxone for six weeks; aortic valve replacement with a bovine pericardial valve | No |
| Winther et al., 2020 [10] | 62 | F | 2-week history of diarrhea, vomiting, a 10 kg weight loss, headache, dizziness | Vegetation on aortic valve | No | MALDI-TOF | Benzylpenicillin for 4 weeks plus gentamicin for 2 weeks | No |
| Present case 2023 | 62 | M | 5-month intermittent fever not responding to antibiotics, accompanied by weight loss, sweating, cough, abnormal fatigue | Vegetation of size 4 mm × 6 mm over the posterior leaflet of the mitral valve | Mitral valve prolapses | MALDI-TOF Bruker Biotyper | Ampicillin and ceftriaxone for 6 weeks; mitral valve replacement with a bioprosthetic valve | No |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gaudiano, R.; Trizzino, M.; Torre, S.; Virruso, R.; Fiorino, F.; Argano, V.; Cascio, A. Enterococcus hirae Mitral Valve Infectious Endocarditis: A Case Report and Review of the Literature. Antibiotics 2023, 12, 1232. https://doi.org/10.3390/antibiotics12081232
Gaudiano R, Trizzino M, Torre S, Virruso R, Fiorino F, Argano V, Cascio A. Enterococcus hirae Mitral Valve Infectious Endocarditis: A Case Report and Review of the Literature. Antibiotics. 2023; 12(8):1232. https://doi.org/10.3390/antibiotics12081232
Chicago/Turabian StyleGaudiano, Roberta, Marcello Trizzino, Salvatore Torre, Roberta Virruso, Fabio Fiorino, Vincenzo Argano, and Antonio Cascio. 2023. "Enterococcus hirae Mitral Valve Infectious Endocarditis: A Case Report and Review of the Literature" Antibiotics 12, no. 8: 1232. https://doi.org/10.3390/antibiotics12081232
APA StyleGaudiano, R., Trizzino, M., Torre, S., Virruso, R., Fiorino, F., Argano, V., & Cascio, A. (2023). Enterococcus hirae Mitral Valve Infectious Endocarditis: A Case Report and Review of the Literature. Antibiotics, 12(8), 1232. https://doi.org/10.3390/antibiotics12081232






