Epidemiological Situation of High-Prevalence Non-Communicable Diseases in Spain: A Systematic Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Protocol and Registration
2.2. Inclusion and Exclusion Criteria
2.3. Search Strategy
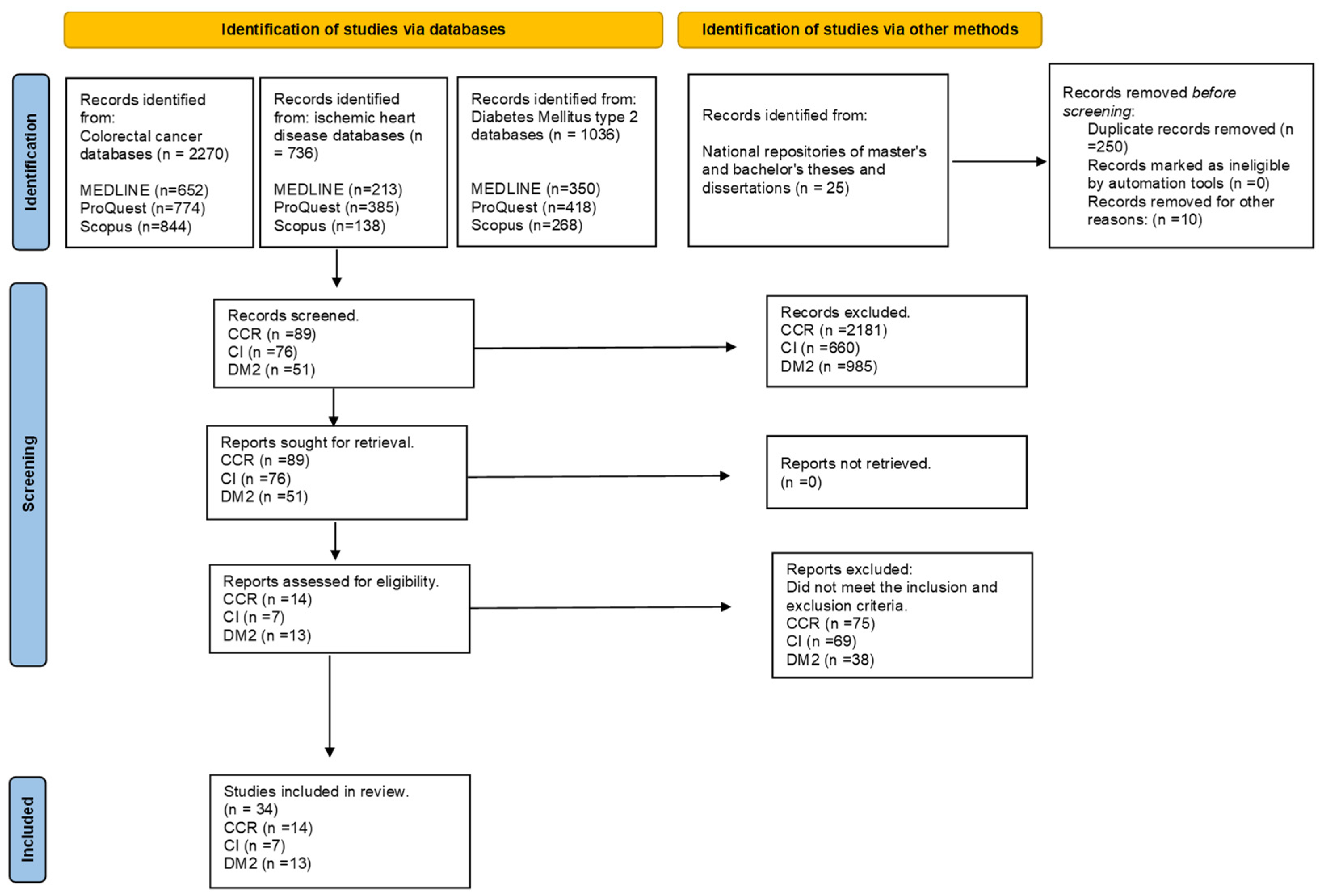
2.4. Study Selection and Data Extraction
2.5. Methodological Quality Assessment and Risk of Bias
2.6. Data Analysis
3. Results
3.1. Colorectal Cancer
3.1.1. Implementation of Screening and Early Detection Tests
3.1.2. Determinants in Screening
3.1.3. Healthy Lifestyle and Genetics in CRC
3.1.4. Mortality
3.2. Ischaemic Heart Disease
3.2.1. Risk Factors Associated with Ischaemic Heart Disease
3.2.2. Types of IHD
3.2.3. Healthy Lifestyle
3.2.4. Mortality and Incidence
3.3. Diabetes Mellitus Type 2
3.3.1. Risk Factors and Incidence of Diabetes Mellitus Type 2 (DM2) in Spain
3.3.2. Preventive Measures Applied for the Control of the Disease
3.3.3. Empowering the Patient with Type 2 DM
3.3.4. Comorbidities in Patients with DM2
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
Formulation of the Question
| Diseases | Databases | ||
|---|---|---|---|
| PubMed | ProQuest | Scopus | |
| Colorectal cancer | (colorectal cancer [title/abstract])) OR (colonic neoplasms [Mesh terms])) AND (incidence)) AND (Spain) | (colon cancer AND epidemiology AND (Spain OR Spanish) | colon AND neoplasms AND epidemiology AND Spain |
| Ischaemic heart disease | (((ischemic heart disease) AND (myocardial ischemia) AND (((incidence) OR (prevalence)) OR (epidemiology) AND (((Spain) OR (Spanish)) | (ischemic heart disease AND risk factors AND incidence AND Spain) | ischemic heart disease AND risk factors AND incidence AND Spain |
| Diabetes mellitus type 2 | ((((diabetes mellitus type 2) AND (incidence [MeSH Terms]))) AND (epidemiology)) AND (Spain) | (diabetes mellitus type 2) AND (incidence) AND (risks factors) AND (Spain) | diabetes mellitus type 2 AND risks factors AND incidence AND Spain |
References
- Organización Mundial de la Salud Enfermedades No Transmisibles. Available online: https://www.who.int/es/news-room/fact-sheets/detail/noncommunicable-diseases (accessed on 20 February 2023).
- Banco Mundial Abordar Las Enfermedades Más Mortales Del Mundo Puede Contribuir a Una Fuerza Laboral Más Saludable y Un Mayor Crecimiento Económico. Available online: https://www.bancomundial.org/es/news/immersive-story/2020/02/06/tackling-worlds-deadliest-diseases-can-boost-healthy-workforce-and-economic-growth (accessed on 20 February 2023).
- Organización Panamericana de la Salud Economía de Las ENT—OPS/OMS|Organización Panamericana de La Salud. Available online: https://www.paho.org/es/temas/economia-ent (accessed on 20 February 2023).
- United Nations. Sustainable Development Goals Report; General Report; United Nations: New York, NY, USA, 2020.
- Banco Mundial Nueva Clasificación de Los Países Según El Nivel de Ingresos Para 2019 y 2020. Available online: https://blogs.worldbank.org/es/opendata/nueva-clasificacion-de-los-paises-segun-el-nivel-de-ingresos-para-2019-y-2020 (accessed on 11 May 2023).
- Vandenberghe, D.; Albrecht, J. The Financial Burden of Non-Communicable Diseases in the European Union: A Systematic Review. Eur. J. Public Health 2020, 30, 833–839. [Google Scholar] [CrossRef] [PubMed]
- Comisión Europea Enfermedades No Transmisibles. Visión General. Available online: https://health.ec.europa.eu/non-communicable-diseases/overview_es (accessed on 3 March 2023).
- Naciones Unidas. Transformar Nuestro Mundo: La Agenda 2030 Para el Desarrollo Sostenible; Informe Técnico; Naciones Unidas: New York, NY, USA, 2015.
- Ángel, M.; Valdés, S.; Serra Ruíz, M.; Viera García, M. Las Enfermedades Crónicas No Transmisibles: Magnitud Actual y Tendencias Futuras. Rev. Finlay 2018, 8, 140–148. [Google Scholar]
- Shanmuganathan, S.; Mustapha, F.I.; Wilson, A. Evaluating the Sustainability of Non-Communicable Diseases Programs in Malaysia. BMC Public Health 2022, 22, 1463. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization WHO/Europe: Health Systems Response to NCDs—Noncommunicable Diseases in 53 Countries: WHO/Europe Launches New Visual Data Tool. Available online: https://www.euro.who.int/en/health-topics/Health-systems/health-systems-response-to-ncds/news/news/2022/01/noncommunicable-diseases-in-53-countries-whoeurope-presents-new-visual-data-tool (accessed on 23 February 2022).
- Zaletel, J.; Maggini, M. Fostering the Quality of Care for People with Chronic Diseases, from Theory to Practice: The Development of Good Practices in Disease Prevention and Care in JA CHRODIS PLUS Using JA CHRODIS Recommendations and Quality Criteria. Int. J. Environ. Res. Public Health 2020, 17, 951. [Google Scholar] [CrossRef]
- Ministerio de Sanidad. ESTRATEGIA DE SALUD PÚBLICA 2022 ESP 2022 Mejorando La Salud y El Bienestar de La Población Agosto de 2022 SANIDAD 2022; Ministerio de Sanidad: Madrid, Spain, 2022.
- Ministerio de Sanidad. Estrategia Para El Abordaje de La Cronicidad En El Sistema Nacional de Salud; Informe de Evaluación; Ministerio de Sanidad: Madrid, Spain, 2021.
- Organización Mundial de la Salud. Monitoreo de Los Avances En Relación Con Las Enfermedades No Transmisibles 2022; Informe de Seguimiento; OMS: Geneva, Switzerland, 2022. [Google Scholar]
- Instituto Nacional de Estadística. Defunciones Según La Causa de Muerte-Año 2021 (Datos Definitivos) y Primer Semestre 2022 (Datos Provisionales) (2/16); Informe Annual; INE: Madrid, Spain, 2022. [Google Scholar]
- Ministerio de Sanidad. Estrategia En Salud Cardiovascular Del Sistema Nacional de Salud (ESCAV); Informe Técnico; Ministerio de Sanidad: Madrid, Spain, 2022.
- Federación Internacional de Diabetes España Informe Diabetes 2000–2045. Available online: https://diabetesatlas.org/data/en/country/187/es.html (accessed on 1 March 2023).
- Ministerio de Sanidad. Prevalencia de La Diabetes Mellitus; Informe Global; Ministerio de Sanidad: Madrid, Spain, 2017.
- Sociedad Española de Diabetes (SED) España Es El Segundo País Con Mayor Prevalencia de Diabetes de Europa|Sociedad Española de Diabetes. Available online: https://www.sediabetes.org/comunicacion/sala-de-prensa/espana-es-el-segundo-pais-con-mayor-prevalencia-de-diabetes-de-europa/ (accessed on 14 March 2023).
- International Agency for Research on Cancer (IARC) Spain Source: Globocan 2020. Available online: https://gco.iarc.fr/today/data/factsheets/populations/724-spain-fact-sheets.pdf (accessed on 16 March 2023).
- Globocan Cancer Today. Available online: https://gco.iarc.fr/today/home (accessed on 11 May 2023).
- Sociedad Española de Oncología Médica. Las Cifras Del Cáncer En España 2023; Informe global; Sociedad Española de Oncología Médica: Madrid, Spain, 2023. [Google Scholar]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Vandenbroucke, J.P.; Von Elm, E.; Altman, D.G.; Gøtzsche, P.C.; Mulrow, C.D.; Pocock, S.J.; Poole, C.; Schlesselman, J.J.; Egger, M. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and Elaboration. Ann. Intern. Med. 2007, 147, W-163. [Google Scholar] [CrossRef] [PubMed]
- Verhagen, A.P.; De Vet, H.C.W.; De Bie, R.A.; Kessels, A.G.H.; Boers, M.; Bouter, L.M.; Knipschild, P.G. The Delphi List: A Criteria List for Quality Assessment of Randomized Clinical Trials for Conducting Systematic Reviews Developed by Delphi Consensus. J. Clin. Epidemiol. 1998, 51, 1235–1241. [Google Scholar] [CrossRef]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated Criteria for Reporting Qualitative Research (COREQ): A 32-Item Checklist for Interviews and Focus Groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef]
- Berra, S.; Elorza-Ricart, J.M.; Estrada, M.-D.; Sánchez, E. Instrumento Para La Lectura Crítica y La Evaluación de Estudios Epidemiológicos Transversales. Gac. Sanit. 2008, 22, 492–497. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.; Welch, V. Manual Cochrane Para Revisiones Sistemáticas de Intervenciones|Entrenamiento Cochrane. Available online: https://training.cochrane.org/handbook#how-to-access (accessed on 4 November 2023).
- Sterne, J.; Hernán, M.; McAleenan, A.; Reeves, B.; Higgins, J. Capítulo 25: Evaluación Del Riesgo de Sesgo En Un Estudio No Aleatorio|Entrenamiento Cochrane. Available online: https://training.cochrane.org/handbook/current/chapter-25 (accessed on 4 November 2023).
- González, L.V.; Sotos, F.E.; de Miguel Ibáñez, R. Colorectal Cancer Screening in Castilla La Mancha, Spain: The Influence of Social, Economic, Demographic and Geographic Factors. J. Community Health 2022, 47, 446–453. [Google Scholar] [CrossRef]
- Alegria-Lertxundi, I.; Aguirre, C.; Bujanda, L.; Fernández, F.J.; Polo, F.; Ordovás, J.M.; Etxezarraga, M.C.; Zabalza, I.; Larzabal, M.; Portillo, I.; et al. Gene–Diet Interactions in Colorectal Cancer: Survey Design, Instruments, Participants and Descriptive Data of a Case–Control Study in the Basque Country. Nutrients 2020, 12, 2362. [Google Scholar] [CrossRef]
- Nouni-García, R.; Lara-López, Á.; Carratalá-Munuera, C.; Gil-Guillén, V.F.; López-Pineda, A.; Orozco-Beltrán, D.; Quesada, J.A. Factors Associated with Colorectal Cancer Screening in Spain: Results of the 2017 National Health Survey. Int. J. Environ. Res. Public Health 2022, 19, 5460. [Google Scholar] [CrossRef] [PubMed]
- Perea, J.; Marti, M.; Espin, E.; Hernandez-Villafranca, S.; Orihuela, P.; Vidal Tocino, R.; Alcazar, J.A.; Vivas, A.; Narvaez, C.; Prieto, I.; et al. Cohort Profile: The Spanish Early-Onset Colorectal Cancer (SECOC) Cohort: A Multicentre Cohort Study on the Molecular Basis of Colorectal Cancer among Young Individuals in Spain. BMJ Open 2021, 11, e055409. [Google Scholar] [CrossRef]
- Darbà, J.; Marsà, A. Results after 10 Years of Colorectal Cancer Screenings in Spain: Hospital Incidence and In-Hospital Mortality (2011–2016). PLoS ONE 2020, 15, e0228795. [Google Scholar] [CrossRef] [PubMed]
- Rubín-García, M.; Martín, V.; Vitelli-Storelli, F.; Moreno, V.; Aragonés, N.; Ardanaz, E.; Alonso-Molero, J.; Jiménez-Moleón, J.J.; Amiano, P.; Fernández-Tardón, G.; et al. Antecedentes Familiares de Primer Grado Como Factor de Riesgo En El Cáncer Colorrectal. Gac. Sanit. 2022, 36, 345–352. [Google Scholar] [CrossRef] [PubMed]
- Cayuela, L.; Rodríguez-Domínguez, S.; Giráldez, Á.; Cayuela, A. Regional Differences in Colorectal Cancer Mortality Trends, Spain (1980–2018). Rev. Esp. Enferm. Dig. 2021, 113, 570–575. [Google Scholar] [CrossRef]
- Solís-Ibinagagoitia, M.; Unanue-Arza, S.; Díaz-Seoane, M.; Martínez-Indart, L.; Lebeña-Maluf, A.; Idigoras, I.; Bilbao, I.; Portillo, I. Factors Related to Non-Participation in the Basque Country Colorectal Cancer Screening Programme. Front. Public Health 2020, 8, 604385. [Google Scholar] [CrossRef]
- Zamorano-Leon, J.J.; López-De-Andres, A.; Álvarez-González, A.; Maestre-Miquel, C.; Astasio-Arbiza, P.; López-Farré, A.; De-Miguel-Diez, J.; Jiménez-García, R.; Albaladejo-Vicente, R. Trends and Predictors for the Uptake of Colon Cancer Screening Using the Fecal Occult Blood Test in Spain from 2011 to 2017. Int. J. Environ. Res. Public Health 2020, 17, 6222. [Google Scholar] [CrossRef] [PubMed]
- Perestelo-Perez, L.; Rivero-Santana, A.; Torres-Castaño, A.; Ramos-Garcia, V.; Alvarez-Perez, Y.; Gonzalez-Hernandez, N.; Buron, A.; Pignone, M.; Serrano-Aguilar, P. Effectiveness of a Decision Aid for Promoting Colorectal Cancer Screening in Spain: A Randomized Trial. BMC Med. Inform. Decis. Mak. 2019, 19, 8. [Google Scholar] [CrossRef]
- Solé Llop, M.E.; Cano del Pozo, M.; García Montero, J.I.; Carrera-Lasfuentes, P.; Lanas, Á. Programa de Cribado Poblacional de Cáncer Colorrectal En Aragón. Primeros Resultados. Gac. Sanit. 2018, 32, 559–562. [Google Scholar] [CrossRef]
- Álvarez-delgado, A.; Pérez García, M.L.; García-gonzález, J.M.; Iglesias de Sena, H.; Chamorro, A.J.; Lorenzo Gómez, M.F.; Marcos, M.; Mirón-canelo, J.A. Improvements in the Effectiveness of Early Detection in Colorectal Cancer with Open-label Randomised Study. J. Clin. Med. 2021, 10, 5072. [Google Scholar] [CrossRef] [PubMed]
- García-Torrecillas, J.M.; Olvera-Porcel, M.C.; Ferrer-Márquez, M.; Rubio-Gil, F.; Sánchez, M.J.; Rodríguez-Barranco, M. Spatial and Temporal Variations in Spain in the Standardised Ratio of In-Hospital Mortality Due to Colorectal Cancer, 2008–2014. BMC Cancer 2019, 19, 310. [Google Scholar] [CrossRef]
- Ibáñez-Sanz, G.; Diéz-Villanueva, A.; Alonso, M.H.; Rodríguez-Moranta, F.; Pérez-Gómez, B.; Bustamante, M.; Martin, V.; Llorca, J.; Amiano, P.; Ardanaz, E.; et al. Risk Model for Colorectal Cancer in Spanish Population Using Environmental and Genetic Factors: Results from the MCC-Spain Study. Sci. Rep. 2017, 7, 43263. [Google Scholar] [CrossRef] [PubMed]
- Estarlich, M.; Tolsa, C.; Trapero, I.; Buigues, C. Circadian Variations and Associated Factors in Patients with Ischaemic Heart Disease. Int. J. Environ. Res. Public Health 2022, 19, 15628. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-Lazaro, C.I.; Sayon-Orea, C.; Toledo, E.; Moreno-Iribas, C.; Guembe, M.J.; Cosials, J.B.; Reyero, J.B.; Martínez, J.D.; Diego, P.G.; Uche, A.M.G.; et al. Association of Ideal Cardiovascular Health with Cardiovascular Events and Risk Advancement Periods in a Mediterranean Population-Based Cohort. BMC Med. 2022, 20, 232. [Google Scholar] [CrossRef] [PubMed]
- Hervella, M.I.; Carratalá-Munuera, C.; Orozco-Beltrán, D.; López-Pineda, A.; Bertomeu-González, V.; Gil-Guillén, V.F.; Pascual, R.; Quesada, J.A. Trends in Premature Mortality Due to Ischemic Heart Disease in Spain from 1998 to 2018. Rev. Esp. Cardiol. (Engl. Ed.) 2021, 74, 838–845. [Google Scholar] [CrossRef] [PubMed]
- Álvarez-Fernández, C.; Romero-Saldaña, M.; Álvarez-López, C.; Vaquero-Abellán, M. Incidencia de Cardiopatía Isquémica y Accidente Cerebrovascular En Trabajadores de Una Administración Local Del Sur de España a Lo Largo de Diez Años de Seguimiento. Rev. Esp. Salud Pública 2020, 94, 202001001. [Google Scholar] [CrossRef]
- Mendoza Alarcón, M.Á.; Tejero Mas, M.; Morales Gabardino, J.A.; Buitrago Ramírez, F. Prevalencia y Grado de Control de Los Factores de Riesgo Cardiovascular En Pacientes Con Cardiopatía Isquémica Adscritos a Un Centro de Salud Urbano. Rev. Esp. Salud Pública 2021, 95, e202102040. [Google Scholar]
- Cordero, A.; Galve, E.; Bertomeu-Martínez, V.; Bueno, H.; Fácila, L.; Alegría, E.; Cequier, Á.; Ruiz, E.; González-Juanatey, J.R. Tendencias En Factores de Riesgo y Tratamientos de Pacientes Con Cardiopatía Isquémica Estable Atendidos En Consultas de Cardiología Entre 2006 y 2014. Rev. Española Cardiol. 2016, 69, 401–407. [Google Scholar] [CrossRef]
- Melero-Alegria, J.I.; Cascon, M.; Romero, A.; Vara, P.P.; Barreiro-Perez, M.; Vicente-Palacios, V.; Perez-Escanilla, F.; Hernandez-Hernandez, J.; Garde, B.; Cascon, S.; et al. SALMANTICOR Study. Rationale and Design of a Population-Based Study to Identify Structural Heart Disease Abnormalities: A Spatial and Machine Learning Analysis. BMJ Open 2019, 9, e024605. [Google Scholar] [CrossRef]
- Martínez-Hervás, S.; Morales-Suarez-Varela, M.M.; Andrés-Blasco, I.; Lara-Hernández, F.; Peraita-Costa, I.; Real, J.T.; García-García, A.B.; Chaves, F.J. Developing a Simple and Practical Decision Model to Predict the Risk of Incident Type 2 Diabetes among the General Population: The Di@bet.Es Study. Eur. J. Intern. Med. 2022, 102, 80–87. [Google Scholar] [CrossRef]
- Hawkins Carranza, F.; Corbatón-Anchuelo, A.; Bermejo Pareja, F.; Martín-Arriscado Arroba, C.; Vega-Quiroga, S.; Benito-León, J.; Serrano-Ríos, M. Incidence of Type 2 Diabetes in the Elderly in Central Spain: Association with Socioeconomic Status, Educational Level, and Other Risk Factors. Prim. Care Diabetes 2022, 16, 279–286. [Google Scholar] [CrossRef]
- Cuevas Fernández, F.J.; Pérez de Armas, A.; Cerdeña Rodríguez, E.; Hernández Andreu, M.; Iglesias Girón, M.J.; García Marrero, M.R.; Cabrera de León, A.; García Bello, M.Á. Mal Control de La Diabetes Tipo 2 En Un Centro de Salud de Atención Primaria: Factores Modificables y Población Diana. Aten. Primaria 2021, 53, 102066. [Google Scholar] [CrossRef]
- Alustiza, E.; Perales, A.; Mateo-Abad, M.; Ozcoidi, I.; Aizpuru, G.; Albaina, O.; Vergara, I. Tackling Risk Factors for Type 2 Diabetes in Adolescents: PRE-STARt Study in Euskadi. An. Pediatría Engl. Ed. 2021, 95, 186–196. [Google Scholar] [CrossRef]
- Ruiz-Estigarribia, L.; Martínez-González, M.A.; Díaz-Gutiérrez, J.; Sayón-Orea, C.; Basterra-Gortari, F.J.; Bes-Rastrollo, M. Lifestyle Behavior and the Risk of Type 2 Diabetes in the Seguimiento Universidad de Navarra (SUN) Cohort. Nutr. Metab. Cardiovasc. Dis. 2020, 30, 1355–1364. [Google Scholar] [CrossRef] [PubMed]
- Mata-Cases, M.; Franch-Nadal, J.; Real, J.; Cedenilla, M.; Mauricio, D. Prevalence and Coprevalence of Chronic Comorbid Conditions in Patients with Type 2 Diabetes in Catalonia: A Population-Based Cross-Sectional Study. BMJ Open 2019, 9, e031281. [Google Scholar] [CrossRef] [PubMed]
- Martin-Ridaura, C.; Ochoa-Esteban, D.; Berlinches-Zapero, C.; Ruiz-Fernández, D.; Sanz-Martín, V.; Gavira-Izquierdo, R.; March, S.; López-Toribio, M.; Ceinos-Arcones, M.; Rivas-Hernández, D.; et al. Evaluation under Real-Life Conditions of a Lifestyle Intervention for Diabetes Prevention Developed by the Municipal Health Services of Madrid, Spain. Sci. Rep. 2022, 12, 19700. [Google Scholar] [CrossRef] [PubMed]
- Duarte-Díaz, A.; González-Pacheco, H.; Rivero-Santana, A.; Ramallo-Fariña, Y.; Perestelo-Pérez, L.; Peñate, W.; Carrion, C.; Serrano-Aguilar, P. Factors Associated with Patient Empowerment in Spanish Adults with Type 2 Diabetes: A Cross-Sectional Analysis. Health Expect. 2022, 25, 2762–2774. [Google Scholar] [CrossRef]
- Cos, F.X.; Gómez-Huelgas, R.; Gomez-Peralta, F. Are There Different Viewpoints about the Management of Type 2 Diabetes Mellitus and Comorbidities? A Multidisciplinary Spanish Qualitative Research. Diabetes Ther. 2022, 13, 189–203. [Google Scholar] [CrossRef]
- Martos-Cabrera, M.B.; Gómez-Urquiza, J.L.; Cañadas-González, G.; Romero-Bejar, J.L.; Suleiman-Martos, N.; Cañadas-De la Fuente, G.A.; Albendín-García, L. Nursing-Intense Health Education Intervention for Persons with Type 2 Diabetes: A Quasi-Experimental Study. Healthcare 2021, 9, 832. [Google Scholar] [CrossRef]
- Vilafranca Cartagena, M.; Arreciado Marañón, A.; Artigues-Barbera, E.; Tort-Nasarre, G. Successful Practices in Performing and Maintaining Physical Activity in Adults with Type 2 Diabetes Mellitus: A Qualitative Study. Int. J. Environ. Res. Public Health 2022, 19, 14041. [Google Scholar] [CrossRef] [PubMed]
- Represas-Carrera, F.; Couso-Viana, S.; Méndez-López, F.; Masluk, B.; Magallón-Botaya, R.; Recio-Rodríguez, J.I.; Pombo, H.; Leiva-Rus, A.; Gil-Girbau, M.; Motrico, E.; et al. Effectiveness of a Multicomponent Intervention in Primary Care That Addresses Patients with Diabetes Mellitus with Two or More Unhealthy Habits, Such as Diet, Physical Activity or Smoking: Multicenter Randomized Cluster Trial (Eira Study). Int. J. Environ. Res. Public Health 2021, 18, 5788. [Google Scholar] [CrossRef] [PubMed]
- López-Cobo, I.; Rodriguez-Latre, L.; Cunillera, O.; Ruiz, I.; Copetti, S.; Albareda, M.; Vila, L. Trends in Glycemic Control, Cardiovascular Risk Factors and Chronic Complications of Type 2 Diabetes, 2012–2016, in a Healthcare Area of Barcelona. Diabetes Res. Clin. Pract. 2022, 190, 110014. [Google Scholar] [CrossRef] [PubMed]
- García Torrecillas, J.M.; Ferrer Márquez, M.; Duarte, R.; Rubio-Gil, F. Investigación Epidemiológica En Cáncer Colorrectal: Perspectiva, Prospectiva y Retos Bajo La Óptica de Explotación Del Big-Data. Semer.—Med. Fam. 2016, 42, 509–513. [Google Scholar] [CrossRef] [PubMed]
- Gonzales, R.; Ratnapradipa, K.; De Alba, A.; Chen, K.; Smith, L.; Kim, J.; Wang, H.; Farazi, P.A. Awareness and Knowledge of Colorectal Cancer Screening among Latinos in Omaha, Nebraska. J. Immigr. Minor. Health 2023, 25, 161–167. [Google Scholar] [CrossRef]
- Portero de la Cruz, S.; Cebrino, J. Uptake Patterns and Predictors of Colorectal Cancer Screening among Adults Resident in Spain: A Population-Based Study from 2017 to 2020. Front. Public Health 2023, 11, 1151225. [Google Scholar] [CrossRef]
- Lee, K.M.N.; Hunleth, J.; Rolf, L.; Maki, J.; Lewis-Thames, M.; Oestmann, K.; James, A.S. Distance and Transportation Barriers to Colorectal Cancer Screening in a Rural Community. J. Prim. Care Community Health 2023, 14, 21501319221147126. [Google Scholar] [CrossRef]
- Wele, P.; Wu, X.; Shi, H. Sex-Dependent Differences in Colorectal Cancer: With a Focus on Obesity. Cells 2022, 11, 3688. [Google Scholar] [CrossRef]
- Popovici, D.; Stanisav, C.; Saftescu, S.; Negru, S.; Dragomir, R.; Ciurescu, D.; Diaconescu, R. Exploring the Influence of Age, Gender and Body Mass Index on Colorectal Cancer Location. Medicina 2023, 59, 1399. [Google Scholar] [CrossRef]
- Cheng, V.; Oveisi, N.; McTaggart-Cowan, H.; Loree, J.M.; Murphy, R.A.; De Vera, M.A. Colorectal Cancer and Onset of Anxiety and Depression: A Systematic Review and Meta-Analysis. Curr. Oncol. 2022, 29, 8751–8766. [Google Scholar] [CrossRef]
- Chávez-Villa, M.; Ruffolo, L.I.; Al-Judaibi, B.M.; Fujiki, M.; Hashimoto, K.; Kallas, J.; Kwon, C.H.D.; Nair, A.; Orloff, M.S.; Pineda-Solis, K.; et al. The High Incidence of Occult Carcinoma in Total Hepatectomy Specimens of Patients Treated for Unresectable Colorectal Liver Metastases with Liver Transplant. Ann. Surg. 2023, 278, e1026. [Google Scholar] [CrossRef] [PubMed]
- Avan, A.; Aamodt, A.H.; Selbæk, G.; Bovim, G.; Bassetti, C.L.A.; Boon, P.; Grisold, W.; Hachinski, V. Decreasing Incidence of Stroke, Ischaemic Heart Disease and Dementia in Norway, 1990–2019, a Global Burden of Disease Study: An Opportunity. Eur. J. Neurol. 2023, 30, 2267–2277. [Google Scholar] [CrossRef]
- Dai, H.; Much, A.A.; Maor, E.; Asher, E.; Younis, A.; Xu, Y.; Lu, Y.; Liu, X.; Shu, J.; Bragazzi, N.L. Global, Regional, and National Burden of Ischaemic Heart Disease and Its Attributable Risk Factors, 1990–2017: Results from the Global Burden of Disease Study 2017. Eur. Heart J. Qual. Care Clin. Outcomes 2022, 8, 50. [Google Scholar] [CrossRef]
- Liu, S.; Luo, J.; Zhang, T.; Zhang, D.; Zhang, H. The Combined Role of Obesity and Depressive Symptoms in the Association with Ischaemic Heart Disease and Its Subtypes. Sci. Rep. 2022, 12, 14419. [Google Scholar] [CrossRef] [PubMed]
- Lecoeur, E.; Domengé, O.; Fayol, A.; Jannot, A.S.; Hulot, J.S. Epidemiology of Heart Failure in Young Adults: A French Nationwide Cohort Study. Eur. Heart J. 2023, 44, 383. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, W.; Muhammad, T.; Maurya, C.; Akhtar, S.N. Prevalence and Factors Associated with Undiagnosed and Uncontrolled Heart Disease: A Study Based on Self-Reported Chronic Heart Disease and Symptom-Based Angina Pectoris among Middle-Aged and Older Indian Adults. PLoS ONE 2023, 18, e0287455. [Google Scholar] [CrossRef]
- Su, J.; Geng, H.; Chen, L.; Fan, X.; Zhou, J.; Wu, M.; Lu, Y.; Hua, Y.; Jin, J.; Guo, Y.; et al. Association of Healthy Lifestyle with Incident Cardiovascular Diseases among Hypertensive and Normotensive Chinese Adults. Front. Cardiovasc. Med. 2023, 10, 1046943. [Google Scholar] [CrossRef]
- Acosta, S.; Johansson, A.; Drake, I. Diet and Lifestyle Factors and Risk of Atherosclerotic Cardiovascular Disease—A Prospective Cohort Study. Nutrients 2021, 13, 3822. [Google Scholar] [CrossRef]
- Fernández-Bergés, D.; Buitrago Ramírez, F.; Palomo Cobos, L.; Lozano Mera, L.; González-Fernández, M.R.; Rubini, A.; Ramírez Moreno, J.M.; Robles Pérez-Monteoliva, N.R.; Félix-Redondo, F.J. Incidencia de Cardiopatía Isquémica En El Estudio HERMEX y Su Asociación Con Los Factores de Riesgo Cardiovascular Clásicos. Med. Fam. Semer. 2022, 48, 88–95. [Google Scholar] [CrossRef]
- Lazarus, J.V.; Ortiz, A.; Tyrovolas, S.; Fernández, E.; Guy, D.; White, T.M.; Ma, R.; Hay, S.I.; Naghavi, M.; Soriano, J.B.; et al. A GBD 2019 Study of Health and Sustainable Development Goal Gains and Forecasts to 2030 in Spain. Sci. Rep. 2022, 12, 21154. [Google Scholar] [CrossRef]
- Nanda, M.; Sharma, R.; Mubarik, S.; Aashima, A.; Zhang, K. Type-2 Diabetes Mellitus (T2DM): Spatial-Temporal Patterns of Incidence, Mortality and Attributable Risk Factors from 1990 to 2019 among 21 World Regions. Endocrine 2022, 77, 444–454. [Google Scholar] [CrossRef]
- Iheanacho, C.O.; Osoba, D.O.; Eze, U.I.H. Evaluation of Predominant Risk Factors for Type 2 Diabetes Mellitus among Out-Patients in Two Nigerian Secondary Health Facilities. Afr. Health Sci. 2021, 21, 693. [Google Scholar] [CrossRef] [PubMed]
- Liu, G.; Li, Y.; Pan, A.; Hu, Y.; Chen, S.; Qian, F.; Rimm, E.B.; Manson, J.E.; Stampfer, M.J.; Giatsidis, G.; et al. Adherence to a Healthy Lifestyle in Association with Microvascular Complications among Adults with Type 2 Diabetes. JAMA Netw. Open 2023, 6, e2252239. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; He, X.; Zhou, J.; Wang, Y.; Yu, L.; Li, X.; Liu, T.; Luo, J. Impact of Healthy Lifestyle on the Risk of Type 2 Diabetes Mellitus in Southwest China: A Prospective Cohort Study. J. Diabetes Investig. 2022, 13, 2091. [Google Scholar] [CrossRef] [PubMed]
- Khowaja, M.A.; Rozi, S.; Sawani, S.; Ahmed, A. Factors Associated with Diabetes Empowerment among Patients with Type 2 Diabetes, at OPD Setting, Karachi, Pakistan. Sci. Rep. 2023, 13, 7165. [Google Scholar] [CrossRef]
- Dimore, A.L.; Edosa, Z.K.; Mitiku, A.A. Glycemic Control and Diabetes Complications among Adult Type 2 Diabetic Patients at Public Hospitals in Hadiya Zone, Southern Ethiopia. PLoS ONE 2023, 18, e0282962. [Google Scholar] [CrossRef]
- Luo, X.; Sun, J.; Pan, H.; Zhou, D.; Huang, P.; Tang, J.; Shi, R.; Ye, H.; Zhao, Y.; Zhang, A. Establishment and Health Management Application of a Prediction Model for High-Risk Complication Combination of Type 2 Diabetes Mellitus Based on Data Mining. PLoS ONE 2023, 18, e0289749. [Google Scholar] [CrossRef]
- Berhe, K.K.; Mselle, L.T.; Gebru, H.B. The Magnitude of Chronic Diabetes Complications and Its Associated Factors among Diabetic Patients Attending the General Hospitals in Tigray Region, Northern Ethiopia. PLoS ONE 2023, 18, 0290240. [Google Scholar] [CrossRef]
| Author and Year | Disease | Region of Spain | Study Design | Risk of Bias | Participants and Population | Variables | Results |
|---|---|---|---|---|---|---|---|
| González et al., 2022 [31] | CCR | Province of Cuenca | Retrospective, descriptive, analytical and observational study | Low | n = 1422 male and female patients between 50 and 69 years old | Sociodemographic, economic and clinical data | Present determining factors of screening: place of residence, annual income and unemployment rate. |
| Alegria-Lertxundi et al., 2020 [32] | CCR | Osakidetza/Basque Service | Observational study epidemiological study | Low | n = 308 cases diagnosed with CRC and n = 308 controls. Participants (between 50 and 69 years old) | The evaluation of dietary intake, lifestyle, demographic and socioeconomic determinants, and genetic factors. | The presence of diagnosed CRC occurred more in men than in women (4.8% versus 2.1%). The interaction of genetic factors with a healthy lifestyle plays an important role in reducing the risk of CRC. |
| Nouni-García et al., 2022 [33] | CCR | All of Spain | Transversal study | Low | n = 10,595 men and n = 12,494 women. Men and women between 50 and 69 years old. | Faecal occult blood (FOBT). On the other hand, the explanatory variables covered sociodemographic variables, health determinants, medical care variables and self-perceived health. | The communities with the most participation that had had an FOBT were the Basque Country (72.3%), Navarra (60.5%) and Castilla y León (49.1%). On the contrary, low participation was represented by Extremadura (8.7%, n = 16), Ceuta and Melilla (10.4%, n = 3) and Andalusia (14.1%, n = 186). |
| Perea et al., 2021 [34] | CCR | All of Spain | Multicentre prospective cohort | Unclear | n = 220 patients with early onset colorectal cancer Investigation (EOCRC) | Demographic, clinic-pathological characteristics of EOCRC and molecular characterisation. | 60.3% of the cases were men and the average age was 44 years. Regarding location, the tumour with the most cases was the rectum (42.6%), then the left colon (32.4%) and the right colon (25%). |
| Darbà and Marsà, 2020 [35] | CCR | All of Spain | Retrospective multicentre observational study | Low | n = 99,653 income records | The variables studied include the information recorded from the patient’s profile and details of the admission. | The male sex obtained the highest percentage both in the records obtained from primary care (56.17% men and 43.83% women) and those from hospitalised care (60.70%). The lowest hospital mortality rates by regions occurred in Cantabria, Catalonia and La Rioja, and the highest in Ceuta and Melilla, and the Canary Islands. |
| Rubín-García et al., 2022 [36] | CCR | Leon, Barcelona, Madrid, Asturias, Cantabria, Guipuzcoa and Navarra, Granada, Huelva, Murcia and Valencia | Observational, multicentre, multicase-control study | Low | Cases, n = 1360 and controls, n = 2857. The participants ranged in age from 20 to 85 years. | The variables to be studied: information on diet, sociodemographic data, anthropometric data, environmental exposures and lifestyles, and physical activity. | The cases were higher than the controls. In this case, the presence of first-degree FA (family history) increased 4 times (aOR: 4.22; 95% CI: 2.29–7.78) and with a family member diagnosed before the age of 50 there were three times more likely (aOR: 3.24; 95% CI: 1.52–6.91). |
| Cayuela et al., 2021 [37] | CCR | All of Spain | Observational record | High | CRC death records (1980–2018). | Age-standardised mortality rates for CRC. For these rates, individual records broken down by sex, age and year of death were used. | Mortality from CRC increased in both men and women. Men experienced an increase from 2256 new cases in 1980 to 9222 in 2018, while women increased the number of cases from 2285 to 6066 in absolute values for the same period. |
| Solís-Ibinagagoitia et al., 2020 [38] | CCR | Basque Country | Study was cross-sectional descriptive | Low | n = 515,388 people. Target population between 50 and 69 years old | Age, sex, smoker, diabetes, high blood pressure, obesity, use of health services, vaccination, comorbidity, deprivation, type of participants. Non-participation was a fundamental aspect of the study. | It was observed that men were more prone to risk factors such as smoking, obesity, hypertension and diabetes than women. On the other hand, 45.4% of men use APS services, less than women (52.5%). |
| Zamorano-Leon et al., 2020 [39] | CCR | All of Spain | Transversal study | Low | n = 12,657. Participants aged 50 to 69 years old | Adoption of FOBT-based CRC screening, sociodemographic characteristics, health status, and lifestyle behavior. | The Spanish population from 2011 to 2017 had a positive acceptance of FOBT programs. |
| Perestelo-Perez et al., 2019 [40] | CCR | Tenerife | Randomised controlled trial study | Low | n = 107 patients, of which n = 83 belonged to centre A and n = 24 to centre B. | Decision aid (DA), decisional conflict, knowledge about CRC and screening options | The effect of the intervention on the decisional conflict showed that centre A had better acceptance of the intervention than centre B. For its part, centre A obtained a beneficial effect on the decision-making process, favouring the intervention group. |
| Solé Llop et al., 2018 [41] | CCR | Aragon | Prospective observational | Unclear | n = 12,518 people, population aged 60–69 years | The screening process indicators were evaluated: indicators of detected injuries; indicators of detected tumours; and positive predictive value. | Of the overall rate, 10.75% of patients were positive for the FOBT test, and was higher in men than in women (13.77% vs. 7.92%). Regarding the colonoscopy, 95.07% of the participants agreed to have it done. |
| Álvarez-delgado et al., 2021 [42] | CCR | Salamanca | Experimental or intervention study | Low | n = 33,167 patients aged 60 to 69 years | Sex, comorbidities, use of anticoagulants, allergies, patient’s initiative to participate, patient preparation, food intake before the intervention, abstinence time, tolerance to the preparation, intestinal cleansing with the scale of Boston, faecal intubation, divided dosing, clinical-preventive relevance, efficacy of colonoscopy as treatment and location of adenomas. | Regarding the characteristics of the population, there were no significant differences in age, sex, comorbidities, the use of antiplatelet drugs, use of anticoagulants or allergies between the intervention and control groups. Both the IG and the CG were similar and homogeneous, and therefore comparable. |
| García-Torrecillas et al., 2019 [43] | CCR | All of Spain | Cohort study | Low | n = 258,927 hospitalisation episodes | The main variable analysed was mortality during hospitalisation. Other variables studied were sociodemographic, clinical features such as discharge diagnoses and discharge procedures. Other variables analysed were level of severity, type of admission and management variables. | 258,927 hospitalisation episodes were evaluated. As for the average hospital stay, it was 13.16 days, with the majority being men (60.6%). The average annual CRC mortality rate nationwide was 20.0 per 100,000 inhabitants. An increase in rates was recorded in the regions of Galicia, Asturias, Cantabria, the Basque Country, La Rioja, Castilla León, Extremadura, Valencia and Catalonia |
| Ibáñez-Sanz et al., 2017 [44] | CCR | Madrid, Barcelona, Navarra, Girona, Gipuzkoa, Leon, Asturias, Murcia, Huelva, Cantabria, Valencia and Granada | Cases and controls study | Low | n = 1336 CRC cases and n = 2744 controls with genotype data. People between 20 and 85 years old | Variables to study: family history of CRC, smoking, BMI, average physical exercise, consumption of red meat and patient medications. For location anatomical distribution: proximal, distal colon and rectum. | Family history of CRC was the single most important risk factor for CRC and modifiable risk factors were stronger in predicting risk than genetic susceptibility. |
| Estarlich et al., 2022 [45] | IC | Alzira | Retrospective cross-sectional study | Low | n = 244 patients. Patients admitted to the ICU with a diagnosis of IC | Circadian rhythm variables, sociodemographic and risk factors, IHD severity variables, location of infarction and length of hospital stay. | The individual risk factors that were associated with the severity of ischaemic heart disease were age, previous IHD, and dyslipidemia. |
| Fernandez-Lazaro et al., 2022 [46] | IC | Navarra | Population cohort study | Low | n = 3826 people between 35 and 84 years old. | Sociodemographic and lifestyle data, medical history, medication use and biological parameters. | After the ideal metrics evaluated, a lower risk of major cardiovascular events such as AMI, stroke or deaths from cardiovascular causes were significantly associated. |
| Hervella et al., 2021 [47] | IC | All of Spain | Observational study | Low | n = 232,617 premature deaths due to IC. Ages between 0 to 74 years | The variables to be studied were age, sex, year, province of residence and year of death. | In data, premature mortality recorded in 1998 was 14,876 people, while in 2018 this figure was reduced to 8780 people, with the female sex having the lowest percentage. |
| Álvarez-Fernández et al., 2020 [48] | IC | Cordoba | Longitudinal cohort study | Low | n = 698 workers. Age between 35 and 60 years | Among the study variables were REGICOR’s own rating, whether or not to suffer from ischaemic heart disease, person and lifestyle, analytical and anthropometric variables. | Age, blood pressure and smoking were the risk factors most associated with cardiovascular events (IHD and stroke). The incidence for IHD was 276.3 per 100,000 person-years and for cardiovascular disease (IHD AND stroke) was 360.1 per 100,000 workers-year. |
| Mendoza Alarcón et al., 2021 [49] | IC | Bajadoz | Observational study | Low | n = 200 patients assigned to the La Paz health centre in Badajoz with hospital diagnosis | Prevalence of cardiovascular risk factors being hypercholesterolemia, tobacco consumption, high blood pressure, diabetes, obesity and chronic kidney disease. Also, their degree of control and drug adhesions. | This study revealed that the risk factors associated with the disease corresponded to 77.9% for high blood pressure, 69.3% for dyslipidemia, 48.2% for obesity and 32.3% for diabetes. |
| Cordero et al., 2016 [50] | IC | All of Spain | Data from two prospective, observational, multicentre registries | Unclear | In 2006, n = 1583 patients and in 2014, n = 1110 patients. | Among the variables to be studied was the record of all treatments and doses received before the visit and the optimal medical treatment (BMT). On the other hand, the control of HBP, heart rate, dyslipidemia, DM, obesity and glomerular filtration rate. | The study showed that diabetes (DM) and hypertension (HTN) decreased. Notable improvement in medical treatment, especially in control of risk factors. |
| Melero-Alegria et al., 2019 [51] | IC | Salamanca | Cross-sectional descriptive population-based study | Unclear | n = 2400 people over 18 years old | Medical history, different surveys including social status, Mediterranean diet, functional capacity, ECG, echocardiogram, VASERA, biochemical and genetic analysis. | Analysis of the SALMANTICOR study (study of the prevalence of structural heart disease and its risk factors). This study provides echocardiographic parameters. |
| Martínez-Hervás et al., 2022 [52] | DM2 | All of Spain | Prospective, multicentre, population-based cohort study | Low | n = 2408 participants. People aged ≥18 years from the Di@bet.es study | Age, educational level, physical activity, smoking, dyslipidemia, medication and family history. | After a follow-up of 7.5 years, they detected as risk factors a higher initial age, BMI, waist circumference, blood pressure, FPG (fasting plasma glucose), HOMA (Homeostatic Model Assessment), HbA1c, LDL and FTG (fasting triglycerides), and lower HDL. The patients had a crude incidence of 8.5 per 1000 person-years. |
| Hawkins Carranza et al., 2022 [53] | DM2 | Central Spain (Las Margaritas, Lista and Arevalo) | Cohort study | Low | n = 2000 people for each area. People over 65 years of age | Age, sex, educational level, occupation, physical activity (PA), weight and height, BMI and blood tests. | In their analysis, they show that the predictive risk factors in their study were BMI, hypertension, occupation and the incidence of T2D. In the three central areas of Spain studied (Las Margaritas, Lista, Arevalo), their results showed an average incidence of type 2 DM of 9.8 per 1000 person-years. |
| Cuevas Fernández et al., 2021 [54] | DM2 | Tenerife | Retrospective cross-sectional descriptive study | Low | n = 587 patients with DM2 | Good or bad control of T2DM according to the GDPS 2018 network. In addition, sociodemographic variables, habits, clinical variables, dyslipidemia, high blood pressure, metabolic syndrome, years of evolution of T2DM, ischaemic heart disease, complications of T2DM, general comorbidities and therapeutic guidelines. | There was a risk of obesity, low level of education, dyslipidemia, hypertension and metabolic syndrome. Of the total number of participants, 24% had poor diabetes control and 25% had complications of the disease. |
| Alustiza et al., 2021 [55] | DM2 | Basque Country (Osakidetza) | Randomised controlled clinical trial | Low | n = 92 participants, n = 47 in the intervention group (IG) and n = 45 in the control group (CG); adolescents aged 12 to 14 years | Anthropometric measurements, vital signs, stage of pubertal development, diet, physical activity, sociodemographic characteristics, family, prenatal, personal history and laboratory parameters. | The increase in BMI was stopped through the intervention. Significant differences were observed between those participants who spent an hour of their time exercising and those who did not. There was an increase in the consumption of fruits and vegetables, and improvements in eating habits in the GI. |
| Ruiz-Estigarribia et al., 2020 [56] | DM2 | Navarra | Prospective cohort study | Low | n = 11,005 participants, Spanish university graduates. Follow-up University of Navarra (SUN) | Sociodemographic aspects, lifestyle, anthropometric variables and medical history. Other variables to be studied were clinical variables such as prevalence of family history of diabetes, personal history of hypertension, hypertriglyceridemia and hypercholesterolemia status. | In their analysis of the healthy lifestyle (HLS) components, results showed that never smoking, moderate to high physical activity, and a moderate to high Mediterranean diet were factors that helped with diabetes risk. |
| Mata-Cases et al., 2019 [57] | DM2 | Catalonia | Transversal study | Low | n = 373,185 patients, ≥18 years old with a diagnosis of DM2 | Comorbidities, age, gender, smoking status, onset of DM2, date of DM2 diagnosis, blood pressure, cholesterol, weight, height, urine albumin creatinine to creatinine ratio (UACR) and glycated haemoglobin (HbA1c) and pharmacological treatments. | Patients over 75 years of age had greater comorbidity than younger patients. The most frequently presented comorbidities were hypertension (72%), hyperlipidemia (60%), obesity (45%), chronic kidney disease (33%), chronic kidney failure (28%) and cardiovascular disease (23%). |
| Martin-Ridaura et al., 2022 [58] | DM2 | Madrid | Quasi-experimental study, pre-post evaluation of the intervention | Low | n = 1629 start of the intervention, n = 1021 end of the intervention; people between 35 and 69 years old | Weight, BMI, waist circumference and glycaemic levels. On the other hand, the sociodemographic variables, educational level, employment situation, origin and marital status. | Six months after the intervention, the participants showed a decrease in their initial weight, and a reduction in waist circumference and BMI. At 12 months, both weight and waist circumference decreased. |
| Duarte-Díaz et al., 2022 [59] | DM2 | Canary Islands | Transversal study | Low | n = 2334 patients between 18 and 65 years old | The main variable was empowerment. Other variables to be studied were sociodemographic data, clinical data, knowledge of diabetes and quality of life related to diabetes. | Study that mentions patient empowerment. The factors that were significantly associated with empowerment in the participants were sociodemographic and clinical factors, age, sex, educational level, living alone, employment status, country of birth, time since diagnosis, HbA1c and the number of comorbidities. |
| Cos et al., 2022 [60] | DM2 | Spain | Qualitative study | Low | n = 300 doctors primary care doctors and hospital care specialists | A Delphi-type survey was carried out with 25 statements and 13 questions on opinion, attitude and behavior (OAB). | Doctors expressed the importance of early screening for patients with type 2 DM, interventions for good healthy lifestyle practice, glycosylated testing and glycaemic control as key strategies to reduce the prevalence of the disease. |
| Martos-Cabrera et al., 2021 [61] | DM2 | Andalusia | Quasi-experimental study | Low | n = 249 patients (171 in the control group and 78 in the intervention group) over 30 years of age | Sociodemographic data (age and sex) and health data (body mass index, presence of hypertension, retinopathy, neuropathy and risk of diabetic foot). | Once the intervention was applied, HbA1c levels were reduced in both groups. The favourable group in this study was the intervention group, since they managed to reduce the levels of glycosylated haemoglobin. |
| Vilafranca Cartagena et al., 2022 [62] | DM2 | Catalonia | Qualitative study | Low | n = 10 adult patients between 55 and 79 years old who had been diagnosed with DM2 | The inclusion criteria were adults with DM2 in the age range of 55 to 79 years who had been diagnosed at least two years earlier, presenting complications associated with DM2, good metabolic control and good adherence to healthy treatments. | The study demonstrates the importance of the knowledge and empowerment that patients must have when treating the disease. |
| Represas-Carrera et al., 2021 [63] | DM2 | 7 Spanish autonomous communities (CEA) | Randomised clinical trial | Low | n = 694 with DM. CG n = 356 GI n = 338 Patients between 45 and 75 years old unhealthy lifestyle habits | The main variable was HbA1c and the secondary variables: Mediterranean diet, diet quality, physical activity, sedentary lifestyle, smoking and quality of life. | The results showed a significant improvement in adherence to the Mediterranean diet, with the intervention group being the ones who followed the diet best. Non-significance was demonstrated for glycaemic control, physical activity, sedentary lifestyle, smoking and quality of life during the study period. |
| López-Cobo et al., 2022 [64] | DM2 | Barcelona | observational study | Low | n = 20,457 patients, registered between 2012 and 2016 Population with DM2 from 30 to 80 years old. | Age, sex, HbA1c, BMI, systolic and diastolic Blood Pressure (BP), smoking, albumin/creatinine ratio, estimated glomerular filtration rate (eGFR) and blood lipids. | Glycemic control was maintained among the studied population. The chronic complications of type 2 DM with significance in the study were: diabetic retinopathy, diabetic neuropathy, heart failure and peripheral vascular disease. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aparicio-Rodríguez, Y.D.; Alonso-Morillejo, E.; García-Torrecillas, J.M. Epidemiological Situation of High-Prevalence Non-Communicable Diseases in Spain: A Systematic Review. J. Clin. Med. 2023, 12, 7109. https://doi.org/10.3390/jcm12227109
Aparicio-Rodríguez YD, Alonso-Morillejo E, García-Torrecillas JM. Epidemiological Situation of High-Prevalence Non-Communicable Diseases in Spain: A Systematic Review. Journal of Clinical Medicine. 2023; 12(22):7109. https://doi.org/10.3390/jcm12227109
Chicago/Turabian StyleAparicio-Rodríguez, Yessineth D., Enrique Alonso-Morillejo, and Juan Manuel García-Torrecillas. 2023. "Epidemiological Situation of High-Prevalence Non-Communicable Diseases in Spain: A Systematic Review" Journal of Clinical Medicine 12, no. 22: 7109. https://doi.org/10.3390/jcm12227109
APA StyleAparicio-Rodríguez, Y. D., Alonso-Morillejo, E., & García-Torrecillas, J. M. (2023). Epidemiological Situation of High-Prevalence Non-Communicable Diseases in Spain: A Systematic Review. Journal of Clinical Medicine, 12(22), 7109. https://doi.org/10.3390/jcm12227109







