Physicians’ Perceptions of and Barriers to Cardiopulmonary Rehabilitation for Heart Failure Patients in Saudi Arabia: A Cross-Sectional Study
Abstract
:1. Introduction
2. Methods
2.1. Study Design
2.2. Questionnaire Tool
2.3. Study Population and Sampling Strategy
2.4. Sample Size
2.5. Ethical Approval
2.6. Statistical Analysis
3. Results
3.1. Cardiopulmonary Rehabilitation Referral Rate by Physicians’ Specialty
3.2. Opinions on Referring Patients with HF, Mode of Delivery, and Components of Cardiopulmonary Rehabilitation
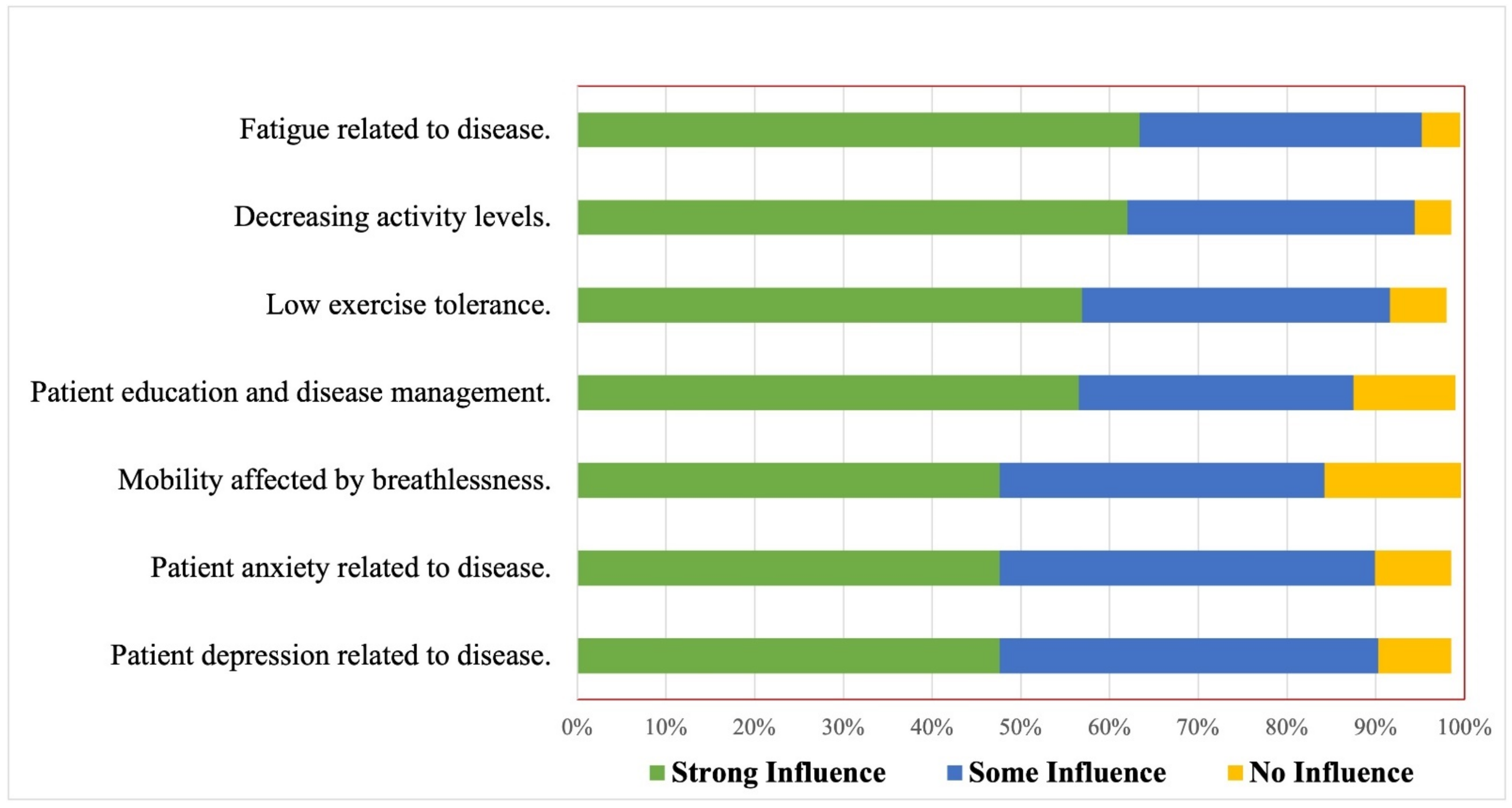
3.3. Patient-Related Factors That Influence Referral Decision to Cardiopulmonary Rehabilitation
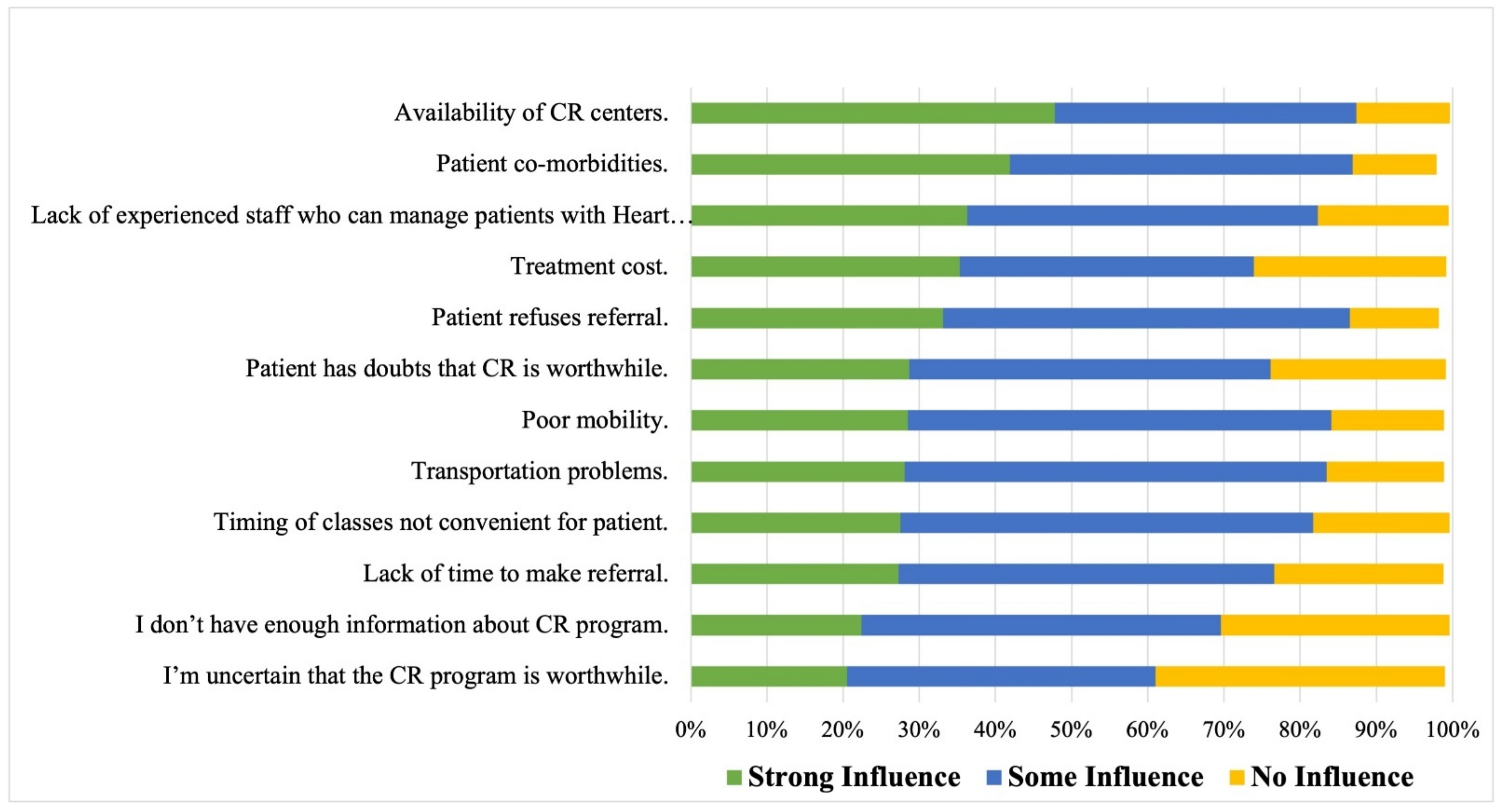
3.4. Cardiopulmonary Rehabilitation Referral Barriers
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Heidenreich, P.A.; Bozkurt, B.; Aguilar, D.; Allen, L.A.; Byun, J.J.; Colvin, M.M.; Deswal, A.; Drazner, M.H.; Dunlay, S.M.; Evers, L.R.; et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: Executive Summary: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2022, 145, e876–e894. [Google Scholar] [CrossRef] [PubMed]
- Cooper, L.B.; Hernandez, A.F. Assessing the Quality and Comparative Effectiveness of Team-Based Care for Heart Failure: Who, What, Where, When, and How. Heart Fail. Clin. 2015, 11, 499–506. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Iyngkaran, P.; De Courten, M. Heart Failure Paradigms in the Developed World—A ‘Taproot’ Plan (Part 2). Curr. Cardiol. Rev. 2022, 18, e130522204750. [Google Scholar] [CrossRef] [PubMed]
- Kolben, Y.; Kessler, A.; Puris, G.; Nachman, D.; Alvarez, P.; Briasoulis, A.; Asleh, R. Management of heart failure with reduced ejection fraction: Challenges in patients with atrial fibrillation, renal disease and in the elderly. Rev. Cardiovasc. Med. 2022, 23, 16. [Google Scholar] [CrossRef] [PubMed]
- Bozkurt, B.; Fonarow, G.C.; Goldberg, L.R.; Guglin, M.; Josephson, R.A.; Forman, D.E.; Lin, G.; Lindenfeld, J.; O’Connor, C.; Panjrath, G.; et al. Cardiac Rehabilitation for Patients With Heart Failure: JACC Expert Panel. J. Am. Coll. Cardiol. 2021, 77, 1454–1469. [Google Scholar] [CrossRef] [PubMed]
- Beckers, P.J.; Denollet, J.; Possemiers, N.M.; Wuyts, F.L.; Vrints, C.J.; Conraads, V.M. Combined endurance-resistance training vs. endurance training in patients with chronic heart failure: A prospective randomized study. Eur. Heart J. 2008, 29, 1858–1866. [Google Scholar] [CrossRef] [Green Version]
- Fukuta, H.; Goto, T.; Wakami, K.; Kamiya, T.; Ohte, N. Effects of exercise training on cardiac function, exercise capacity, and quality of life in heart failure with preserved ejection fraction: A meta-analysis of randomized controlled trials. Heart Fail. Rev. 2019, 24, 535–547. [Google Scholar] [CrossRef]
- Coats, A.J.; Adamopoulos, S.; Radaelli, A.; McCance, A.; Meyer, T.E.; Bernardi, L.; Solda, P.L.; Davey, P.; Ormerod, O.; Forfar, C.; et al. Controlled trial of physical training in chronic heart failure. Exercise performance, hemodynamics, ventilation, and autonomic function. Circulation 1992, 85, 2119–2131. [Google Scholar] [CrossRef] [Green Version]
- Belardinelli, R.; Georgiou, D.; Cianci, G.; Purcaro, A. Randomized, controlled trial of long-term moderate exercise training in chronic heart failure: Effects on functional capacity, quality of life, and clinical outcome. Circulation 1999, 99, 1173–1182. [Google Scholar] [CrossRef] [Green Version]
- Davies, E.J.; Moxham, T.; Rees, K.; Singh, S.; Coats, A.J.; Ebrahim, S.; Lough, F.; Taylor, R.S. Exercise training for systolic heart failure: Cochrane systematic review and meta-analysis. Eur. J. Heart Fail. 2010, 12, 706–715. [Google Scholar] [CrossRef]
- Haykowsky, M.J.; Timmons, M.P.; Kruger, C.; McNeely, M.; Taylor, D.A.; Clark, A.M. Meta-analysis of aerobic interval training on exercise capacity and systolic function in patients with heart failure and reduced ejection fractions. Am. J. Cardiol. 2013, 111, 1466–1469. [Google Scholar] [CrossRef]
- Santos, F.V.; Chiappa, G.R.; Ramalho, S.H.R.; de Lima, A.; de Souza, F.S.J.; Cahalin, L.P.; Durigan, J.L.Q.; de Castro, I.; Cipriano, G., Jr. Resistance exercise enhances oxygen uptake without worsening cardiac function in patients with systolic heart failure: A systematic review and meta-analysis. Heart Fail. Rev. 2018, 23, 73–89. [Google Scholar] [CrossRef]
- Taylor, R.S.; Walker, S.; Ciani, O.; Warren, F.; Smart, N.A.; Piepoli, M.; Davos, C.H. Exercise-based cardiac rehabilitation for chronic heart failure: The EXTRAMATCH II individual participant data meta-analysis. Health Technol. Assess. 2019, 23, 1–98. [Google Scholar] [CrossRef]
- Pina, I.L.; Apstein, C.S.; Balady, G.J.; Belardinelli, R.; Chaitman, B.R.; Duscha, B.D.; Fletcher, B.J.; Fleg, J.L.; Myers, J.N.; Sullivan, M.J.; et al. Exercise and heart failure: A statement from the American Heart Association Committee on exercise, rehabilitation, and prevention. Circulation 2003, 107, 1210–1225. [Google Scholar] [CrossRef]
- Kitzman, D.W.; Brubaker, P.H.; Herrington, D.M.; Morgan, T.M.; Stewart, K.P.; Hundley, W.G.; Abdelhamed, A.; Haykowsky, M.J. Effect of endurance exercise training on endothelial function and arterial stiffness in older patients with heart failure and preserved ejection fraction: A randomized, controlled, single-blind trial. J. Am. Coll. Cardiol. 2013, 62, 584–592. [Google Scholar] [CrossRef]
- Rashed, M.; Theruvan, N.; Gad, A.; Shaheen, H.; Mosbah, S. Cardiac Rehabilitation: Future of Heart Health in Saudi Arabia, a Perceptual View. World J. Cardiovasc. Dis. 2020, 10, 666–677. [Google Scholar] [CrossRef]
- Aldhahir, A.M.; Alghamdi, S.M.; Alqahtani, J.S.; Alqahtani, K.A.; Al Rajah, A.M.; Alkhathlan, B.S.; Singh, S.J.; Mandal, S.; Hurst, J.R. Pulmonary rehabilitation for COPD: A narrative review and call for further implementation in Saudi Arabia. Ann. Thorac. Med. 2021, 16, 299–305. [Google Scholar] [CrossRef]
- Aldhahir, A.M.; Alqahtani, J.S.; Alghamdi, S.M.; Alqarni, A.A.; Khormi, S.K.; Alwafi, H.; Samannodi, M.; Siraj, R.A.; Alhotye, M.; Naser, A.Y.; et al. Physicians’ Attitudes, Beliefs and Barriers to a Pulmonary Rehabilitation for COPD Patients in Saudi Arabia: A Cross-Sectional Study. Healthcare 2022, 10, 904. [Google Scholar] [CrossRef]
- Spruit, M.A.; Singh, S.J.; Garvey, C.; ZuWallack, R.; Nici, L.; Rochester, C.; Hill, K.; Holland, A.E.; Lareau, S.C.; Man, W.D.; et al. An official American Thoracic Society/European Respiratory Society statement: Key concepts and advances in pulmonary rehabilitation. Am. J. Respir. Crit. Care Med. 2013, 188, e13–e64. [Google Scholar] [CrossRef] [Green Version]
- Hill, K.; Vogiatzis, I.; Burtin, C. The importance of components of pulmonary rehabilitation, other than exercise training, in COPD. Eur. Respir. Rev. 2013, 22, 405. [Google Scholar] [CrossRef]
- Holland, A.E.; Cox, N.S.; Houchen-Wolloff, L.; Rochester, C.L.; Garvey, C.; ZuWallack, R.; Nici, L.; Limberg, T.; Lareau, S.C.; Yawn, B.P.; et al. Defining Modern Pulmonary Rehabilitation. An Official American Thoracic Society Workshop Report. Ann. Am. Thorac. Soc. 2021, 18, e12–e29. [Google Scholar] [CrossRef]
- Aldhahir, A.M.; Alhotye, M.; Alqahtani, J.S.; AlDraiwiesh, I.A.; Alghamdi, S.M.; Alsulayyim, A.S.; Alqarni, A.A.; Khormi, S.K.; Alzahrani, E.M.; Al Rajeh, A.M.; et al. Physiotherapists’ Attitudes, and Barriers of Delivering Cardiopulmonary Rehabilitation for Patients with Heart Failure in Saudi Arabia: A Cross-Sectional Study. J. Multidiscip. Health 2022, 15, 2353–2361. [Google Scholar] [CrossRef]
- Aldhahir, A.M.; Alqahtani, J.S.; AlDraiwiesh, I.A.; Alghamdi, S.M.; Alsulayyim, A.S.; Alqarni, A.A.; Alhotye, M.; Alwafi, H.; Siraj, R.; Alrajeh, A.; et al. Healthcare providers’ attitudes, beliefs and barriers to pulmonary rehabilitation for patients with chronic obstructive pulmonary disease in Saudi Arabia: A cross-sectional study. BMJ Open 2022, 12, e063900. [Google Scholar] [CrossRef]
- Aldhahir, A.M. Nurses’ Perception of, and Barriers to, Delivering Cardiopulmonary Rehabilitation for Heart Failure Patients: A National Survey in Saudi Arabia. Int. J. Environ. Res. Public Health 2022, 19, 13586. [Google Scholar] [CrossRef]
- Yancy, C.W.; Jessup, M.; Bozkurt, B.; Butler, J.; Casey, D.E.; Drazner, M.H.; Fonarow, G.C.; Geraci, S.A.; Horwich, T.; Januzzi, J.L. 2013 ACCF/AHA guideline for the management of heart failure: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J. Am. Coll. Cardiol. 2013, 62, e147–e239. [Google Scholar] [CrossRef] [Green Version]
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Čelutkienė, J.; Chioncel, O. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: Developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) With the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. Heart J. 2021, 42, 3599–3726. [Google Scholar]
- Long, L.; Mordi, I.R.; Bridges, C.; Sagar, V.A.; Davies, E.J.; Coats, A.J.; Dalal, H.; Rees, K.; Singh, S.J.; Taylor, R.S. Exercise-based cardiac rehabilitation for adults with heart failure. Cochrane Database Syst. Rev. 2019, 2019, CD003331. [Google Scholar] [CrossRef] [Green Version]
- Taylor, R.S.; Long, L.; Mordi, I.R.; Madsen, M.T.; Davies, E.J.; Dalal, H.; Rees, K.; Singh, S.J.; Gluud, C.; Zwisler, A.-D. Exercise-based rehabilitation for heart failure: Cochrane systematic review, meta-analysis, and trial sequential analysis. JACC Heart Fail. 2019, 7, 691–705. [Google Scholar] [CrossRef]
- Abu Hasheesh, M.O. Health care professionals’ awareness and knowledge of cardiac rehabilitation programs among cardiovascular disease patients in Al-Madinah, Saudi Arabia. Life Sci. J. 2014, 11, 911–917. [Google Scholar]
- Barber, K.; Stommel, M.; Kroll, J.; Holmes-Rovner, M.; McIntosh, B. Cardiac rehabilitation for community-based patients with myocardial infarction: Factors predicting discharge recommendation and participation. J. Clin. Epidemiol. 2001, 54, 1025–1030. [Google Scholar] [CrossRef]
- Grace, S.L.; Grewal, K.; Stewart, D.E. Factors affecting cardiac rehabilitation referral by physician specialty. J. Cardiopulm. Rehabil. Prev. 2008, 28, 248–252. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alsubaiei, M.E.; Cafarella, P.A.; Frith, P.A.; McEvoy, R.D.; Effing, T.W. Barriers for setting up a pulmonary rehabilitation program in the Eastern Province of Saudi Arabia. Ann. Thorac. Med. 2016, 11, 121. [Google Scholar] [CrossRef] [PubMed]
- Triposkiadis, F.K.; Skoularigis, J. Prevalence and importance of comorbidities in patients with heart failure. Curr. Heart Fail. Rep. 2012, 9, 354–362. [Google Scholar] [CrossRef] [PubMed]
- Forman, D.E.; Sanderson, B.K.; Josephson, R.A.; Raikhelkar, J.; Bittner, V.; American College of Cardiology’s Prevention of Cardiovascular Disease Section. Heart failure as a newly approved diagnosis for cardiac rehabilitation: Challenges and opportunities. J. Am. Coll. Cardiol. 2015, 65, 2652–2659. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, L.G.; Schopfer, D.W.; Zhang, N.; Shen, H.; Whooley, M.A. Participation in cardiac rehabilitation among patients with heart failure. J. Card. Fail. 2017, 23, 427–431. [Google Scholar] [CrossRef] [Green Version]
- Im, H.W.; Baek, S.; Jee, S.; Ahn, J.-M.; Park, M.W.; Kim, W.-S. Barriers to outpatient hospital-based cardiac rehabilitation in Korean patients with acute coronary syndrome. Ann. Rehabil. Med. 2018, 42, 154–165. [Google Scholar] [CrossRef] [Green Version]
- Golwala, H.; Pandey, A.; Ju, C.; Butler, J.; Yancy, C.; Bhatt, D.L.; Hernandez, A.F.; Fonarow, G.C. Temporal trends and factors associated with cardiac rehabilitation referral among patients hospitalized with heart failure: Findings from Get With The Guidelines–Heart Failure Registry. J. Am. Coll. Cardiol. 2015, 66, 917–926. [Google Scholar] [CrossRef] [Green Version]
- Blair, J.; Corrigall, H.; Angus, N.J.; Thompson, D.R.; Leslie, S. Home versus hospital-based cardiac rehabilitation: A systematic review. Rural. Remote Health 2011, 11, 190–206. [Google Scholar] [CrossRef]
- Jones, M.I.; Greenfield, S.; Jolly, K. Patients’ experience of home and hospital based cardiac rehabilitation: A focus group study. Eur. J. Cardiovasc. Nurs. 2009, 8, 9–17. [Google Scholar] [CrossRef]
- Anderson, L.; Sharp, G.A.; Norton, R.J.; Dalal, H.; Dean, S.G.; Jolly, K.; Cowie, A.; Zawada, A.; Taylor, R.S. Home-based versus centre-based cardiac rehabilitation. Cochrane Database Syst. Rev. 2017. [Google Scholar] [CrossRef]
- Kraal, J.J.; Marle, M.E.V.D.A.-V.; Abu-Hanna, A.; Stut, W.; Peek, N.; Kemps, H.M. Clinical and cost-effectiveness of home-based cardiac rehabilitation compared to conventional, centre-based cardiac rehabilitation: Results of the FIT@ Home study. Eur. J. Prev. Cardiol. 2017, 24, 1260–1273. [Google Scholar] [CrossRef]
- Cowie, A.; Buckley, J.; Doherty, P.; Furze, G.; Hayward, J.; Hinton, S.; Jones, J.; Speck, L.; Dalal, H.; Mills, J. British Association for Cardiovascular Prevention and Rehabilitation (BACPR). Standards and core components for cardiovascular disease prevention and rehabilitation. Heart 2019, 105, 510–515. [Google Scholar] [CrossRef]
- Yancy, C.W.; Jessup, M.; Bozkurt, B.; Butler, J.; Casey, D.E., Jr.; Colvin, M.M.; Drazner, M.H.; Filippatos, G.S.; Fonarow, G.C.; Givertz, M.M. 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. J. Am. Coll. Cardiol. 2017, 70, 776–803. [Google Scholar]
- Strömberg, A. The crucial role of patient education in heart failure. Eur. J. Heart Fail. 2005, 7, 363–369. [Google Scholar] [CrossRef]
- Michalsen, A.; König, G.; Thimme, W. Preventable causative factors leading to hospital admission with decompensated heart failure. Heart 1998, 80, 437–441. [Google Scholar] [CrossRef]
- Rogers, A.; Addington-Hall, J.M.; McCoy, A.S.; Edmonds, P.M.; Abery, A.J.; Coats, A.J.; Simon, J.; Gibbs, R. A qualitative study of chronic heart failure patients’ understanding of their symptoms and drug therapy. Eur. J. Heart Fail. 2002, 4, 283–287. [Google Scholar] [CrossRef]
| Demographic Variables | General Physicians | Cardiac Doctors |
|---|---|---|
| n (%) | 399 (78%) | 114 (22%) |
| Gender | ||
| Male | 249 (62%) | 83 (73%) |
| Female | 150 (38%) | 31 (27%) |
| Geographic Location | ||
| Eastern region | 87 (22%) | 26 (23%) |
| Central region | 108 (27%) | 30 (26%) |
| Western region | 105 (26%) | 29 (25%) |
| Southern region | 64 (16%) | 18 (16%) |
| Northern region | 35 (9%) | 11 (10%) |
| Year of experience with HF patients | ||
| <1 year | 21 (5%) | 1 (1%) |
| 1–2 years | 41 (10%) | 4 (4%) |
| 3–4 years | 56 (14%) | 4 (4%) |
| 5–6 years | 64 (16%) | 23 (20%) |
| 7–8 years | 46 (12%) | 22 (19%) |
| 9–10 years | 43 (11%) | 14 (12%) |
| >10 years | 128 (32%) | 46 (40%) |
| Responsibilities of care for HF patients | ||
| Diagnosis | 314 (79%) | 108 (95%) |
| Urgent assessments | 243 (61%) | 83 (73%) |
| Non-urgent care | 196 (49%) | 69 (61%) |
| Ongoing management | 212 (53%) | 86 (75%) |
| Admission prevention | 165 (41%) | 57 (50%) |
| Medication checks | 240 (60%) | 32 (28%) |
| Prescribing | 211 (53%) | 70 (61%) |
| Oxygen therapy | 144 (37%) | 30 (26%) |
| In-patient treatment | 215 (54%) | 97 (85%) |
| Outpatient clinics | 110 (28%) | 67 (59%) |
| Primary care | 148 (37%) | 26 (23%) |
| Others | 5 (1%) | 12 (11%) |
| Item | Frequency (%) |
|---|---|
| Patients’ Referral | |
| General physician | |
| Yes | 236 (59%) |
| No | 99 (25%) |
| Not sure | 64 (16%) |
| Cardiac doctor | |
| Yes | 66 (58%) |
| No | 33 (29%) |
| Not sure | 15 (13%) |
| Item | General Physicians | Cardiac Doctors |
|---|---|---|
| Perception of referring HF patients to CR | ||
| I believe CR will improve patients’ physical fitness | ||
| Strongly agree | 194 (49%) | 52 (45%) |
| Agree | 134 (34%) | 57 (50%) |
| Neutral | 49 (12%) | 1 (1%) |
| Disagree | 3 (0.7%) | 1 (1%) |
| Strongly disagree | 19 (5%) | 3 (3%) |
| I believe CR will reduce patients’ breathlessness | ||
| Strongly agree | 152 (38%) | 33 (29%) |
| Agree | 143 (36%) | 68 (59%) |
| Neutral | 70 (18%) | 8 (7%) |
| Disagree | 14 (4%) | 4 (4%) |
| Strongly disagree | 20 (5%) | 1 (1%) |
| I believe CR will improve patients’ palpitation & fatigue | ||
| Strongly agree | 147 (37%) | 20 (17%) |
| Agree | 127 (32%) | 65 (57%) |
| Neutral | 98 (25%) | 27 (24%) |
| Disagree | 12 (3%) | 1 (1%) |
| Strongly disagree | 15 (4%) | 1 (1%) |
| I believe CR will improve patients’ ability to perform daily actives | ||
| Strongly agree | 184 (46%) | 54 (48%) |
| Agree | 124 (31%) | 55 (48%) |
| Neutral | 65 (16%) | 2 (2%) |
| Disagree | 6 (2%) | 1 (1) |
| Strongly disagree | 20 (5%) | 2 (2%) |
| I believe CR will reduce hospital readmission | ||
| Strongly agree | 75 (19%) | 9 (8%) |
| Agree | 118 (30%) | 46 (41%) |
| Neutral | 96 (24%) | 37 (32%) |
| Disagree | 40 (10%) | 6 (5%) |
| Strongly disagree | 70 (18%) | 16 (14%) |
| The best way to deliver CR program for HF patients | ||
| At home | 223 (56%) | 84 (74%) |
| In hospital-supervised program | 315 (79%) | 82 (72%) |
| Online program with healthcare provider support | 189 (47%) | 28 (25%) |
| Tailored program with healthcare provider support through phone | 152 (38%) | 53 (46%) |
| Components of CR program aside from exercise component | ||
| Information about HF disease | 321(80%) | 93 (82%) |
| Weight management | 269 (67%) | 93 (82%) |
| Stress management | 265 (66%) | 96 (84%) |
| Information about medications | 280 (70%) | 95 (83%) |
| Symptoms management | 261 (65%) | 108 (95%) |
| Smoking cessation | 270 (68%) | 91 (80%) |
| Others | 7 (2%) | 23 (20%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aldhahir, A.M.; Alhotye, M.; Alqahtani, J.S.; Alghamdi, S.M.; Alsulayyim, A.S.; Alqarni, A.A.; Alzahrani, E.M.; Siraj, R.A.; Alwafi, H. Physicians’ Perceptions of and Barriers to Cardiopulmonary Rehabilitation for Heart Failure Patients in Saudi Arabia: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 15208. https://doi.org/10.3390/ijerph192215208
Aldhahir AM, Alhotye M, Alqahtani JS, Alghamdi SM, Alsulayyim AS, Alqarni AA, Alzahrani EM, Siraj RA, Alwafi H. Physicians’ Perceptions of and Barriers to Cardiopulmonary Rehabilitation for Heart Failure Patients in Saudi Arabia: A Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2022; 19(22):15208. https://doi.org/10.3390/ijerph192215208
Chicago/Turabian StyleAldhahir, Abdulelah M., Munyra Alhotye, Jaber S. Alqahtani, Saeed M. Alghamdi, Abdullah S. Alsulayyim, Abdullah A. Alqarni, Eidan M. Alzahrani, Rayan A. Siraj, and Hassan Alwafi. 2022. "Physicians’ Perceptions of and Barriers to Cardiopulmonary Rehabilitation for Heart Failure Patients in Saudi Arabia: A Cross-Sectional Study" International Journal of Environmental Research and Public Health 19, no. 22: 15208. https://doi.org/10.3390/ijerph192215208
APA StyleAldhahir, A. M., Alhotye, M., Alqahtani, J. S., Alghamdi, S. M., Alsulayyim, A. S., Alqarni, A. A., Alzahrani, E. M., Siraj, R. A., & Alwafi, H. (2022). Physicians’ Perceptions of and Barriers to Cardiopulmonary Rehabilitation for Heart Failure Patients in Saudi Arabia: A Cross-Sectional Study. International Journal of Environmental Research and Public Health, 19(22), 15208. https://doi.org/10.3390/ijerph192215208










