Treatment of Diabetes Nephropathy in Mice by Germinating Seeds of Euryale ferox through Improving Oxidative Stress
Abstract
1. Introduction
2. Materials and Methods
2.1. Preparation of Gordon Euryale Kernel Extract (EKE) and Germinated Gordon Euryale Kernel Extract (GEKE)
2.2. Phytochemical Assays
2.2.1. Quantification of Total Polyphenols
2.2.2. Quantification of Flavonoids
2.2.3. Soluble Protein Content
2.3. LC-MS/MS Analysis
2.4. Murine Model of Diabetes
2.5. Experimental Setup
2.6. Determination of Biochemical Parameters
2.7. Histological Examinations
2.8. Gene Expression Analysis by RT-PCR
2.9. Protein Expression
2.10. Statistical Analysis
3. Results
3.1. Total Polyphenol and Flavonoid Content
3.2. LC-MS/MS Analysis of EKE and GEKE
3.3. Body Weight and Visceral Indexes
3.4. Fasting Blood Glucose (FBG) and Oral Glucose Tolerance Test (OGTT)
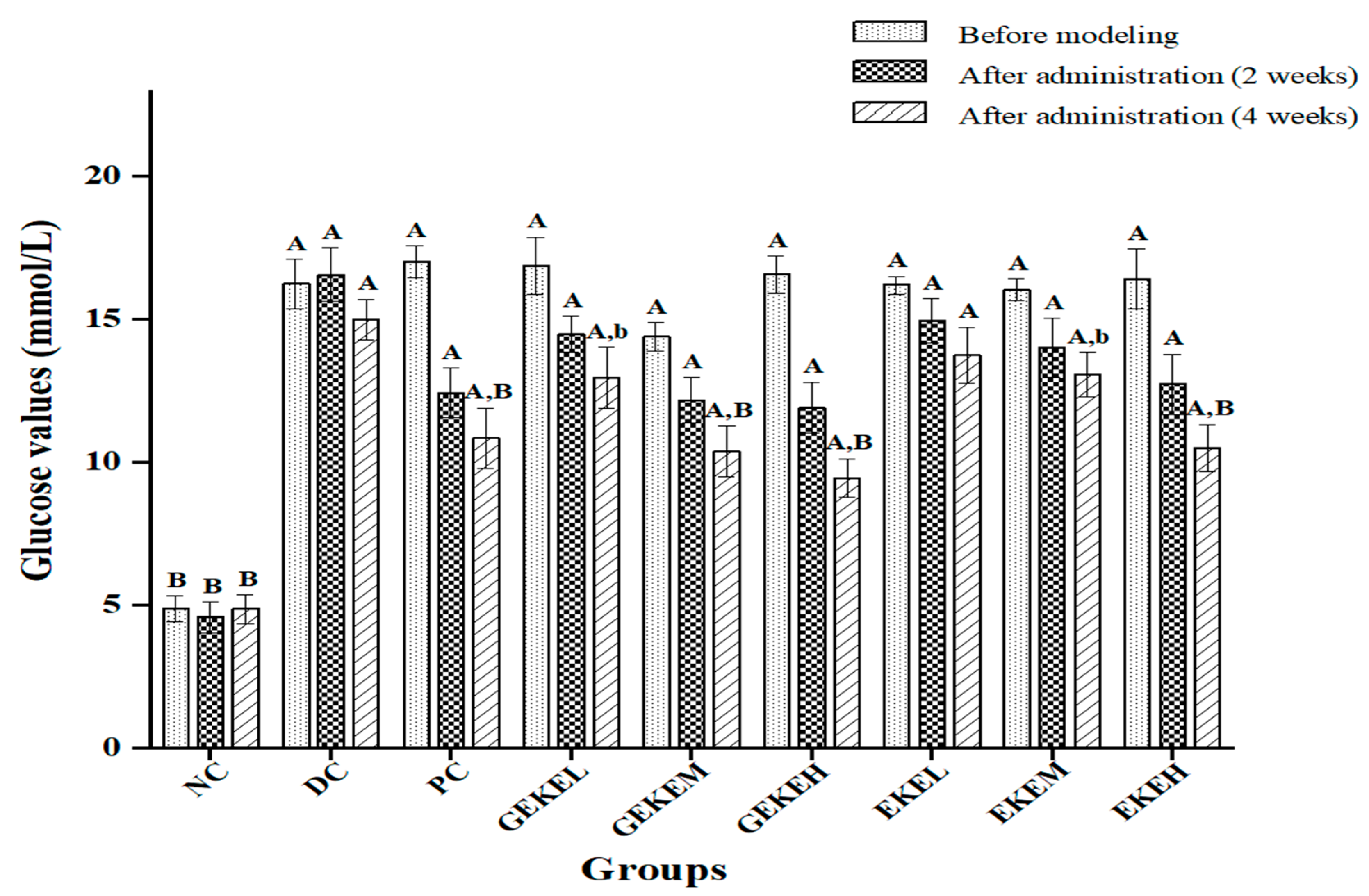
3.5. Serum Biochemical Parameters
3.6. Renal Indicators
3.7. Oxidative Stress Indicators
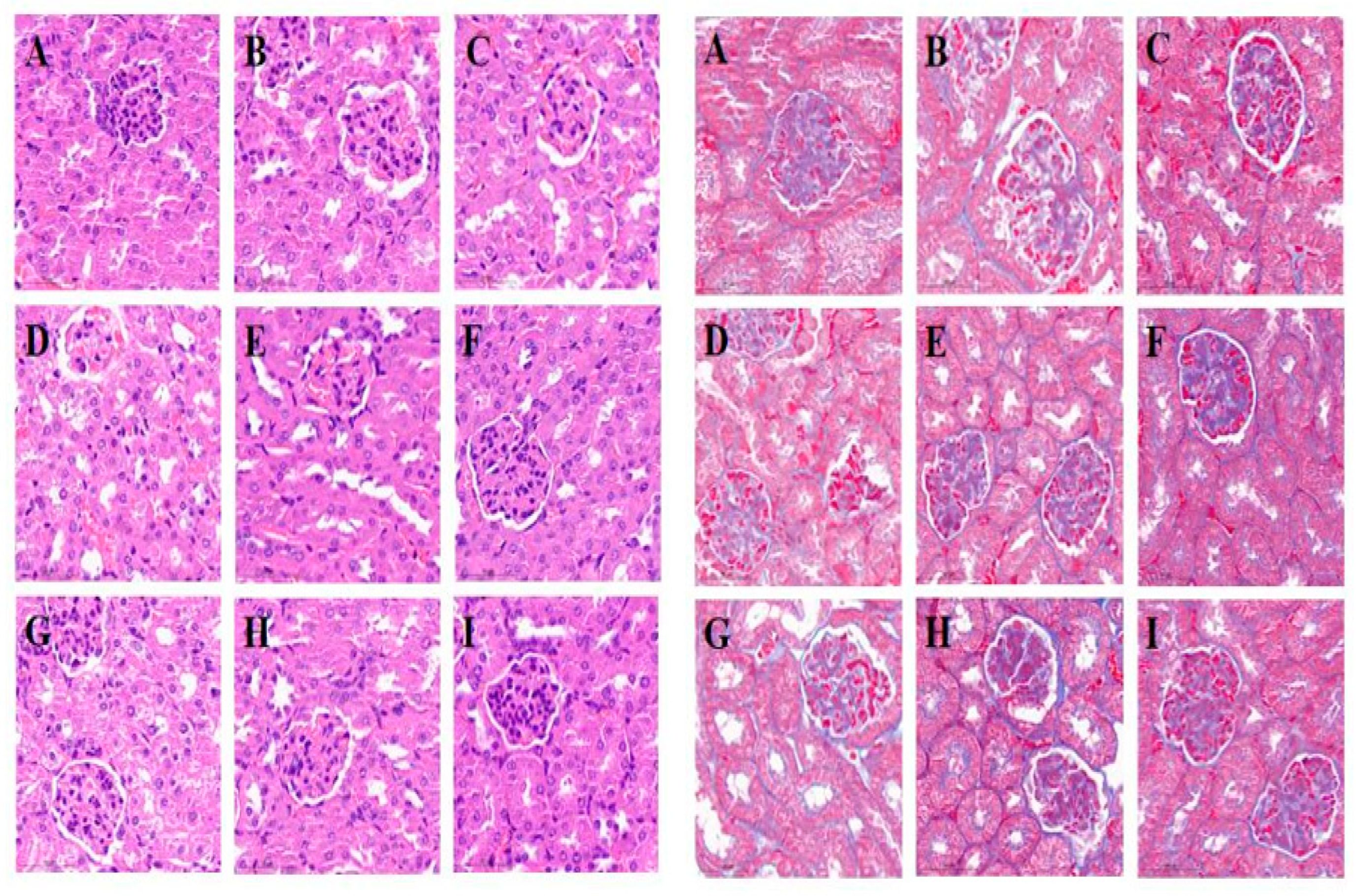
3.8. Pathological Changes in the Kidney
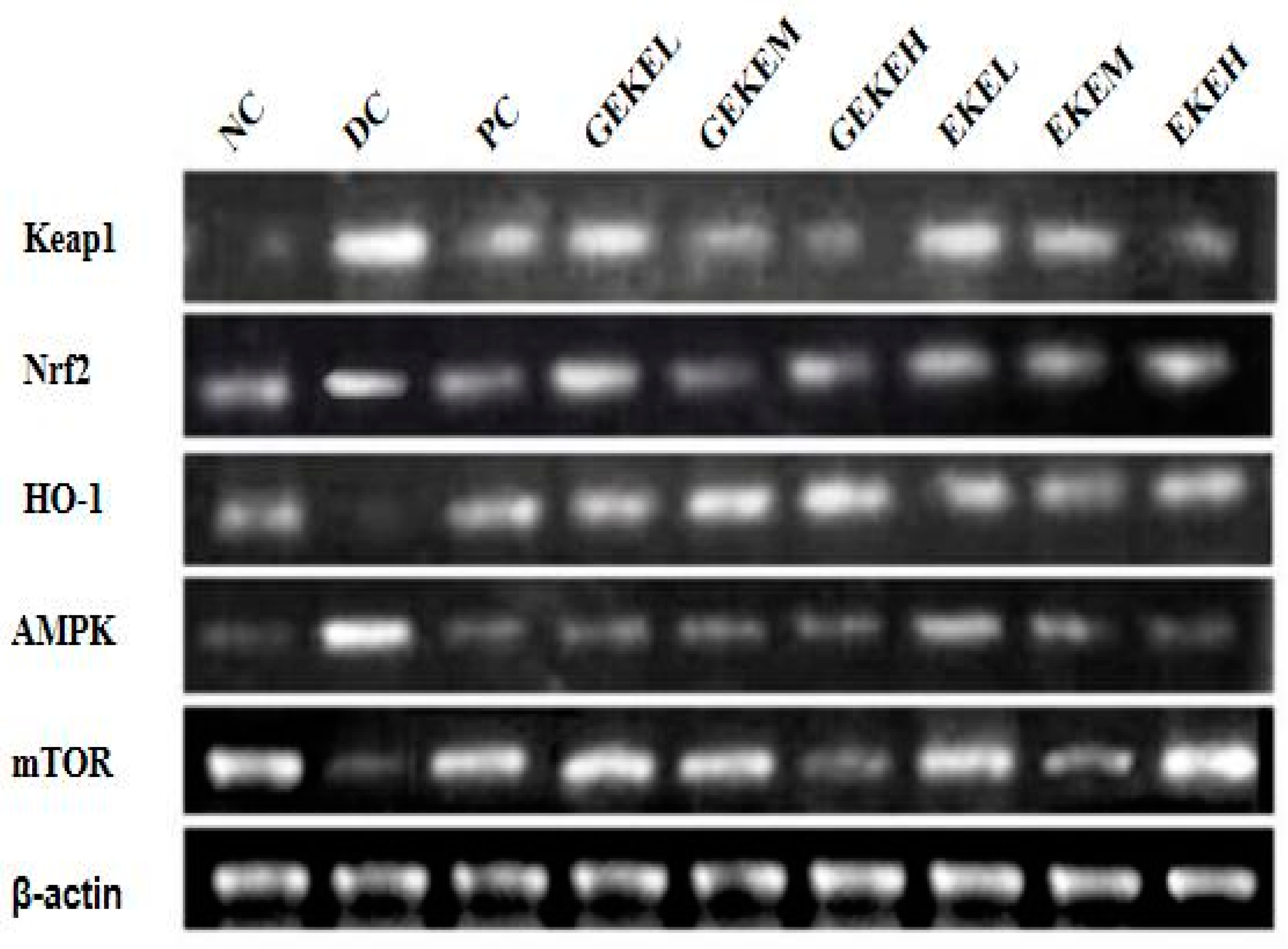
3.9. Renal Gene mRNA Levels and Protein Expression
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| Full English Name | Abbreviation | Full English Name | Abbreviation |
| ungerminated seed extract | EKE | nuclear factor erythroid 2-related factor-2 | Nrf2 |
| germinated seed extract | GEKE | Kelch-like ECH-associated protein 1 | Keap1 |
| microalbunminuria | ALB | AMP-activated kinase | AMPK |
| blood urea nitrogen | BUN | Mechanistic Target Of Rapamycin | mTOR |
| serum creatinine | Scr | γ-aminobutyric acid | GABA |
| malondialdehyde | MDA | streptozotocin | STZ |
| glutathione | GSH | total phenolic content | TPC |
| catalase | CAT | gallic acid equivalents | EAG |
| superoxide dismutase | SOD | Liquid chromatography | LC |
| total antioxidant capacity | T-AOC | Mass spectrometry | MS |
| Diabetes mellitus | DM | body weight | BW |
| type 2 diabetes mellitus | T2D | fasting blood glucose | FBG |
| reactive oxygen species | ROS | serum creatinine | Scr |
| advanced glycosylation end products | AGEs | total cholesterol | TC |
| oxidase-plus 1 | HO-1 | LDL-cholesterol | LDL-C |
| NAD(P)H:quinone oxidoreductase-1 | NQO1 | HDL-cholesterol | HDL-C |
| total superoxide dismutase | T-SOD | triglycerides | TG |
| glycopeptin peroxidase | GSH-Px |
References
- Saracoglu, G.; Bas, H.; Pandır, D. Furan-induced cardiotoxicity in diabetic rats and protective role of lycopene. J. Food Biochem. 2019, 43, e12738. [Google Scholar] [CrossRef] [PubMed]
- Jazani, A.M.; Karimi, A.; Azgomi, R.N.D. The potential role of saffron (Crocus sativus L.) and its components in oxidative stress in diabetes mellitus: A systematic review. Clin. Nutr. ESPEN 2022, 48, 148–157. [Google Scholar] [CrossRef] [PubMed]
- Sun, H.; Saeedi, P.; Karuranga, S.; Pinkepank, M.; Ogurtsova, K.; Duncan, B.B.; Stein, C.; Basit, A.; Chan, J.C.; Mbanya, J.C.; et al. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res. Clin. Pract. 2022, 183, 109119. [Google Scholar] [CrossRef] [PubMed]
- Khanra, R.; Bhattacharjee, N.; Dua, T.K.; Nandy, A.; Saha, A.; Kalita, J.; Manna, P.; Dewanjee, S. Taraxerol, a pentacyclic triterpenoid, from Abroma augusta leaf attenuates diabetic nephropathy in type 2 diabetic rats. Biomed. Pharmacother. 2017, 94, 726–741. [Google Scholar] [CrossRef]
- Dewanjee, S.; Bhattacharjee, N. MicroRNA: A new generation therapeutic target in diabetic nephropathy. Biochem. Pharm. 2018, 155, 32–47. [Google Scholar] [CrossRef]
- Dua, T.K.; Joardar, S.; Chakraborty, P.; Bhowmick, S.; Saha, A.; De Feo, V.; Dewanjee, S. Myricitrin, a glycosyloxyflavone in myrica esculenta bark ameliorates diabetic nephropathy via improving glycemic status, reducing oxidative stress, and suppressing inflammation. Molecules 2021, 26, 258. [Google Scholar] [CrossRef]
- Adelusi, T.; Du, L.; Hao, M.; Zhou, X.; Xuan, Q.; Apu, C.; Sun, Y.; Lu, Q.; Yin, X. Keap1/Nrf2/ARE signaling unfolds therapeutic targets for redox imbalanced-mediated diseases and diabetic nephropathy. Biomed. Pharmacother. 2020, 123, 109732. [Google Scholar] [CrossRef]
- Keane, K.N.; Fernandes Cruzat, V.; Carlessi, R.; De Bittencour, P.I.H.; Newsholme, P. Molecular events linking oxidative stress and inflammation to insulin resistance and b-cell dysfunction. Oxid. Med. Cell Longev. 2015, 2015, 181643. [Google Scholar] [CrossRef]
- Oguntibeju, O.O. Type 2 diabetes mellitus, oxidative stress and inflammation: Examining the links. Int. J. Physiol. Pathophysiol. Pharmacol. 2019, 11, 45–63. [Google Scholar]
- Domingueti, C.; Dusse, L.; Carvalho, M.; De Sousa, L.; Gomes, K.; Fernandes, A.P. Diabetes mellitus: The linkage between oxidative stress, inflammation, hypercoagulability and vascular complications. J. Diabetes Complicat. 2016, 30, 738–745. [Google Scholar] [CrossRef]
- Włodarczyk, M.; Nowicka, G. Obesity, DNA damage, and development of obesityrelated diseases. Int. J. Mol. Sci. 2019, 20, 1146. [Google Scholar] [CrossRef] [PubMed]
- Ye, X.; Jiang, R.; Zhang, Q.; Wang, R.; Yang, C.; Ma, J.; Du, H. Increased 8-hydroxy- 2′-deoxyguanosine in leukocyte DNA from patients with type 2 diabetes and microangiopathy. J. Int. Med. Res. 2016, 44, 472–482. [Google Scholar] [CrossRef] [PubMed]
- Liguori, I.; Russo, G.; Curcio, F.; Bulli, G.; Aran, L.; Della-Morte, D.; Gargiulo, G.; Testa, G.; Cacciatore, F.; Bonaduce, D.; et al. Oxidative stress, aging, and diseases. Clin. Interv. Aging 2018, 13, 757–772. [Google Scholar] [CrossRef] [PubMed]
- Satoh, T.; Okamoto, S.; Cui, J.; Watanabe, Y.; Furuta, K.; Suzuki, M.; Tohyama, K.; Lipton, S.A. Activation of the Keap1/Nrf2 pathway for neuroprotection by electrophilic [correction of electrophillic] phase II inducers. Proc. Natl. Acad. Sci. USA 2006, 103, 768–773. [Google Scholar] [CrossRef]
- Baird, L.; Yamamoto, M. The molecular mechanisms regulating the KEAP1-NRF2 pathway. Mol. Cell Biol. 2020, 40, e00099-20. [Google Scholar] [CrossRef]
- Baird, L.; Lleres, D.; Swift, S.; Dinkova-Kostova, A. Regulatory flexibility in the Nrf2-mediated stress response is conferred by conformational cycling of the Keap1-Nrf2 protein complex. Proc. Natl. Acad. Sci. USA 2013, 110, 15259–15264. [Google Scholar] [CrossRef]
- Petsouki, E.; Cabrera, S.N.S.; Heiss, E.H. AMPK and NRF2: Interactive Players in the Same Team for Cellular Homeostasis? Free Radic. Biol. Med. 2022, 190, 75–93. [Google Scholar] [CrossRef]
- Ayinde, K.S.; Olaoba, O.T.; Ibrahim, B.; Lei, D.; Lu, Q.; Yin, X.; Adelusi, T.I. AMPK allostery: A therapeutic target for the management/treatment of diabetic nephropathy. Life Sci. 2020, 261, 118455. [Google Scholar] [CrossRef]
- Luo, X.; Deng, L.; Lamsal, L.; Xu, W.; Xiang, C.; Cheng, L. AMP-activated protein kinase alleviates extracellular matrix accumulation in high glucose-induced renal fibroblasts through mTOR signaling pathway. Cell. Physiol. Biochem. 2015, 35, 191–200. [Google Scholar] [CrossRef]
- Aguilera, Y.; Díaz, M.F.; Jiménez, T.; Benítez, V.; Herrera, T.; Cuadrado, C.; Martín-Pedrosa, M.; Martín-Cabrejas, M.A. Changes in nonnutritional factors and antioxidant activity during germination of nonconventional legumes. J. Agric. Food Chem. 2013, 61, 8120–8125. [Google Scholar] [CrossRef]
- Beitane, I.; Krumina-Zemture, G.; Sabovics, M. Effect of germination and extrusion on the phenolic content and antioxidant activity of raw buckwheat (Fagopyrum esculentum Moench). Agron. Res. 2018, 16, 1331–1340. [Google Scholar] [CrossRef]
- Chu, C.; Du, Y.M.; Yu, X.T.; Shi, J.; Yuan, X.L.; Liu, X.M.; Liu, Y.H.; Zhang, H.B.; Zhang, Z.F.; Yan, N. Dynamics of antioxidant activities, metabolites, phenolic acids, flavonoids, and phenolic biosynthetic genes in germinating Chinese wild rice (Zizania latifolia). Food Chem. 2020, 318, 126483. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Wei, S.L.; Liao, M.C. Optimization of ultrasonic extraction of phenolic compounds from Euryale ferox seed shells using response surface methodology. Ind. Crops Prod. 2013, 49, 837–843. [Google Scholar] [CrossRef]
- Ahmed, D.; Khan, M.I.; Sharma, M.; Khan, M.F. Novel pentacyclic triterpene isolated from seeds of Euryale ferox Salisb. ameliorates diabetes in streptozotocin induced diabetic rats. Interdiscip. Toxicol. 2018, 11, 275–288. [Google Scholar] [CrossRef] [PubMed]
- McDonald, S.; Prenzler, P.D.; Autolovich, M.; Robards, K. Phenolic content and antioxidant activity of olive extracts. Food Chem. 2001, 73, 73–84. [Google Scholar] [CrossRef]
- Zhang, L.; Jiang, Y.; Pang, X.; Hua, P.; Gao, X.; Li, Q.; Li, Z. Simultaneous Optimization of Ultrasound-Assisted Extraction for Flavonoids and Antioxidant Activity of Angelica keiskei Using Response Surface Methodology (RSM). Molecules 2019, 24, 3461. [Google Scholar] [CrossRef]
- Aminian, M.; Nabatchian, F.; Vaisi-Raygani, A.; Torabi, M. Mechanism of Coomassie Brilliant Blue G-250 binding to cetyltrimethylammonium bromide: An interference with the Bradford assay. Anal. Biochem. 2013, 434, 287–291. [Google Scholar] [CrossRef]
- Wang, Y.D.; Yuan, H.B.; Chen, X.; Zeng, T.T. Effect of water caltrop (Trapa bispinosaRoxb.) pericarp extract on improving insulin resistance in STZ-induced diabetic mice. Pharmacol. Res. Mod. Chin. Med. 2021, 1, 100015. [Google Scholar] [CrossRef]
- Ahmed, D.; Kumar, V.; Verma, A.; Shukla, G.S.; Sharma, M. Antidiabetic, antioxidant, antihyperlipidemic effect of extract of Euryale ferox salisb. with enhanced histopathology of pancreas, liver and kidney in streptozotocin induced diabetic rats. Springerplus 2015, 4, 315. [Google Scholar] [CrossRef]
- Xia, T.; Liu, C.-S.; Hu, Y.-N.; Luo, Z.-Y.; Chen, F.-L.; Yuan, L.-X.; Tan, X.-M. Coix seed polysaccharides alleviate type 2 diabetes mellitus via gut microbiota-derived short-chain fatty acids activation of IGF1/PI3K/AKT signaling. Food Res. Int. 2021, 150, 110717. [Google Scholar] [CrossRef]
- Gong, P.; Xiao, X.; Wang, S.; Shi, F.; Liu, N.; Chen, X.; Yang, W.; Wang, L.; Chen, F. Hypoglycemic effect of astragaloside IV via modulating gut microbiota and regulating AMPK/SIRT1 and PI3K/AKT pathway. J. Ethnopharmacol. 2021, 281, 114558. [Google Scholar] [CrossRef] [PubMed]
- Su, L.; Xin, C.; Yang, J.; Dong, L.; Mei, H.; Dai, X.; Wang, Q. A polysaccharide from Inonotus obliquus ameliorates intestinal barrier dysfunction in mice with type 2 diabetes mellitus. Int. J. Biol. Macromol. 2022, 214, 312–323. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Liang, R.; Zhang, W.; Tian, K.; Li, J.; Chen, X.; Yu, T.; Chen, Q.; Tao, Y. Faecalibacterium prausnitzii-derived microbial anti-inflammatory molecule regulates intestinal integrity in diabetes mellitus mice via modulating tight junction protein expression. J. Diabetes 2020, 12, 224–236. [Google Scholar] [CrossRef] [PubMed]
- Kane, J.P.; Pullinger, C.R.; Goldfine, I.D.; Malloy, M.J. Dyslipidemia and diabetes mellitus: Role of lipoprotein species and interrelated pathways of lipid metabolism in diabetes mellitus. Curr. Opin. Pharmacol. 2021, 61, 21–27. [Google Scholar] [CrossRef] [PubMed]
- Perez-Gonzalez, A.; Galano, A. OH radical scavenging activity of edaravone: Mechanism and kinetics. J. Phys. Chem. B 2011, 115, 1306–1314. [Google Scholar] [CrossRef] [PubMed]
- de Oliveira, L.S.; Thomé, G.R.; Lopes, T.F.; Reichert, K.P.; de Oliveira, J.S.; Pereira, A.D.S.; Baldissareli, J.; Krewer, C.D.C.; Morsch, V.M.; Schetinger, M.R.C.; et al. Effects of gallic acid on delta—Aminolevulinic dehydratase activity and in the biochemical, histological and oxidative stress parameters in the liver and kidney of diabetic rats. Biomed. Pharmacother. 2016, 84, 1291–1299. [Google Scholar] [CrossRef]
- Tian, R.; Pan, Q.; Zhan, J.; Li, J.; Wan, S.; Zhang, Q.; Huang, W. Comparison of phenolic acids and flavan-3-ols during wine fermentation of grapes with different harvest times. Molecules 2009, 14, 827–838. [Google Scholar] [CrossRef]
- Jian, Z.; Lei, K.; Lili, L.; Dandan, W.; Yan, X.; Sheng, S.; Jun, W.; Fuan, W.; Weiguo, Z. Caffeic acid as a preservative that extends shelf-life and maintains fruit quality of mulberries during cold storage. Afr. J. Agric. Res. 2018, 13, 2414–2422. [Google Scholar] [CrossRef]
- Gilani, S.J.; Bin-Jumah, M.N.; Al-Abbasi, F.A.; Nadeem, M.S.; Afzal, M.; Sayyed, N.; Kazmi, I. Fustin ameliorates hyperglycemia in streptozotocin induced type-2 diabetes via modulating glutathione/Superoxide dismutase/Catalase expressions, suppress lipid peroxidation and regulates histopathological changes. Saudi J. Biol. Sci. 2021, 28, 6963–6971. [Google Scholar] [CrossRef]
- Costa, C.; Tsatsakis, A.; Mamoulakis, C.; Teodoro, M.; Briguglio, G.; Caruso, E.; Tsoukalas, D.; Margina, D.; Dardiotis, E.; Kouretas, D.; et al. Current evidence on the effect of dietary polyphenols intake on chronic diseases. Food Chem. Toxicol. 2017, 110, 286–299. [Google Scholar] [CrossRef]
- Liu, S.; Wang, W.; Lu, H.; Shu, Q.; Zhang, Y.; Chen, Q. New perspectives on physiological, biochemical and bioactive components during germination of edible seeds: A review. Trends Food Sci. Technol. 2022, 123, 187–197. [Google Scholar] [CrossRef]
- Velikova, T.V.; Kabakchieva, P.P.; Assyov, Y.S.; Georgiev, T.A.; Infante, M. Targeting inflammatory cytokines to improve type 2 diabetes control. Biomed. Res. Int. 2021, 2021, 7297419. [Google Scholar] [CrossRef] [PubMed]
- Singh, D.K.; Winocour, P.; Farrington, K. Oxidative stress in early diabetic nephropathy: Fueling the fire. Nat. Rev. Endocrinol. 2011, 7, 176–184. [Google Scholar] [CrossRef] [PubMed]
- Bhattacharya, S.; Manna, P.; Gachhui, R.; Sil, P.C. d-Saccharic acid 1,4-lactone protects diabetic rat kidney by ameliorating hyperglycemia-mediated oxidative stress and renal inflammatory cytokines via NF-kB and PKC signaling. Toxicol. Appl. Pharmacol. 2013, 267, 16–29. [Google Scholar] [CrossRef] [PubMed]
- Jin, Y.; Liu, S.; Ma, Q.; Xiao, D.; Chen, L. Berberine enhances the AMPK activation and autophagy and mitigates high glucose-induced apoptosis of mouse podocytes. Eur. J. Pharmacol. 2017, 794, 106–114. [Google Scholar] [CrossRef]
- Kim, M.; Lim, Y. Protective effect of short-term genistein supplementation on the early stage in diabetes-induced renal damage. Mediat. Inflamm. 2013, 2013, 510212. [Google Scholar] [CrossRef]



| Group (10 Mice per Group) | STZ | Treatment 1 | Diet |
|---|---|---|---|
| NC: Normal control group | no | None | Normal chow |
| DC: Diabetic control group | yes | None | Normal chow |
| PC: Positive control group | yes | Metformin, 200 mg/kg bw | Normal chow |
| EKE: Low-dose EKE group | yes | EKE, 100 mg/kg bw | Normal chow |
| EKEM: Medium-dose EKE group | yes | EKE, 200 mg/kg bw | Normal chow |
| EKEH High-dose EKE group | yes | EKE, 400 mg/kg bw | Normal chow |
| GEKE: Low-dose GEKE group | yes | GEKE, 100 mg/kg bw | Normal chow |
| GEKEM: Medium-dose GEKE group | yes | GEKE, 200 mg/kg bw | Normal chow |
| GEKEH: High-dose GEKE group | yes | GEKE, 400 mg/kg bw | Normal chow |
| Gene | Primer Sequences | Amplicon Length (bp) |
|---|---|---|
| Nrf2 | Primer F: GCTGATACTACCGCTGTTC Primer R: GTGGAGAGGATGCTGCTGA | 123 |
| HO-1 | Primer F: ACACAGCACTATGTAAAGCGTCTCC Primer R: GTTGAGCAGGAAGGCGGTCTTAG | 300 |
| Keap1 | Primer F: AGTGCTCAACCGCTTGCTGTATG Primer R: ACGAAAGTCCAGGTCTCTGTCTCC | 243 |
| mTOR | Primer F: ACATCACGCCCTTCACCAGTTTC Primer R:GCAGTCCGTTCCTTCTCCTTCTTG | 361 |
| AMPK | Primer F: ACCCAATTATGCCGCACCAGAAG Primer R: GGACCTCCTCCTCCGAACACTC | 395 |
| β-actin | Primer F: CACGATGGAGGGGCCGGACTCATC Primer R: TAAAGACCTCTATGCCAACACAGT | 300 |
| No. | Compound | RT (min) | Molecular Formula | [M+H] + (m/z) | [M-H]-(m/z) | MS/MS Fragments (m/z) | Ratio: (EKE.raw)/(GEKE.raw) |
|---|---|---|---|---|---|---|---|
| 1 | 2-Hydroxyphenylalanine | 0.719 | C9 H11 N O3 | 165.05441 | 91.05470, 119.0492, 123.04409, 136.07555, 165.05446 | 0 | |
| 2 | L-Tyrosine methyl ester | 1.189 | C10 H13 N O3 | 179.0699 | 91.05466, 119.04919, 136.07549, 137.05949, 179.06999 | 0 | |
| 3 | 2-Methoxyresorcinol | 3.853 | C7 H8 O3 | 141.05449 | 81.03411, 109.02865, 127.03895, 141.05444 | 0 | |
| 4 | 1,2,3,4-Tetrakis-O-(3,4,5-trihydroxybenzoyl)-β-D-glucopyranose | 8.721 | C34 H28 O22 | 787.10022 | 125.02311, 169.01332, 787.10040 | 0 | |
| 5 | Gallic acid | 4.676 | C7 H6 O5 | 169.01326 | 125.02311, 169.01326 | 0 | |
| 6 | Cycloolivil | 7.622 | C20 H24 O7 | 375.14478 | 125.02312, 360.12140, 375.14471 | 0 | |
| 7 | 2,4,6-Trihydroxy-2-(4-hydroxybenzyl)-1-benzofuran-3(2H)-one | 7.183 | C15 H12 O6 | 287.05634 | 125.02311, 259.06107, 287.05597 | 0 | |
| 8 | Gentisic acid | 3.637 | C7 H6 O4 | 153.0182 | 109.02814, 153.01825 | 0 | |
| 9 | Caffeic acid | 20.522 | C9 H8 O4 | 181.04909 | 149.02309, 163.03864 | 0 | |
| 10 | Matairesinol | 5.895 | C20 H22 O6 | 341.13757 | 137.05943, 175.07501, 309.11139 | 0 | |
| 11 | 3’,4’-Dihydroxyphenylacetone | 7.738 | C9 H10 O3 | 167.0701 | 167.06999 | 0 | |
| 12 | Hydromorphinol | 0.473 | C17 H21 N O4 | 30416006 | 114.0555, 185.09174, 286.13913 | 0 | |
| 13 | (8E)-11,13-Dihydroxy-4-methyl-4,5,6,7-tetrahydro-2H-3-benzoxacyclododecine-2,10(1H)-dione | 12.713 | C16 H18 O5 | 291.12244 | 273.18460, 291.19470 | 0 | |
| 14 | Estriol | 15.814 | C18 H24 O3 | 311.16342 | 293.21042, 311.22089, 313.23651 | 0 | |
| 15 | Norbutorphanol | 0.98 | C16 H21 N O2 | 260.1601 | 83.06090, 84.04491, 86.09689, 242.14937, 264.14380 | 0 | |
| 16 | (-)-Fustin | 4.596 | C15 H12 O6 | 289.07028 | 111.04423, 123.04400, 139.03870 | 0 | |
| 17 | Resorcinol monoacetate | 3.655 | C8 H8 O3 | 153.05443 | 110.03642, 138.03091, 153.05434 | 0 | |
| 18 | Prostaglandin E2-1-glyceryl ester | 15.041 | C23 H38 O7 | 409.25522 | 409.255 | 0 | |
| 19 | Eucalyptol | 17.562 | C10 H18 O | 137.13248 | 81.07042, 95.08590 | Infinity | |
| 20 | 1,6-Bis-O-(3,4,5-trihydroxybenzoyl)hexopyranose | 5.464 | C20 H20 O14 | 502.11838 | 153.01787 | Infinity | |
| 21 | Phloroglucinol | 2.236 | C6 H6 O3 | 127.03893 | 130.15894, 127.03889 | Infinity | |
| 22 | Malvidin | 13.006 | C17 H14 O7 | 331.08066 | 315.04907, 331.08032 | Infinity | |
| 23 | 7-Acetyl-3,6-dihydroxy-8-methyl-tetralone | 5.475 | C13 H14 O4 | 235.09616 | 129.07014, 157.06456, 217.08580, 236.09613, 239.13870 | Infinity | |
| 24 | 3’,4’-Dihydroxyphenylacetone | 7.299 | C9 H10 O3 | 167.07011 | 170.11737, 167.06993 | Infinity | |
| 25 | Cycloolivil | 9.042 | C20 H24 O7 | 377.15891 | 375.14334, 377.12265, 375.14590, 379.26978 | Infinity | |
| 26 | 2,4,6-Trihydroxyacetophenone | 2.563 | C8 H8 O4 | 167.03401 | 68.99425, 167.03398 | Infinity | |
| 27 | Octyl gallate | 6.092 | C15 H22 O5 | 281.1395 | 281.13943 | Infinity | |
| 28 | 4-Methylumbelliferone | 5.053 | C10 H8 O3 | 177.05455 | 89.03896, 117.03363, 145.02818, 177.05418 | Infinity | |
| 29 | N-Acetyltyramine | 4.677 | C10 H13 N O2 | 180.10168 | 121.0648 | 0.032 | |
| 30 | 4-Amino-3-hydroxybenzoic acid | 2.614 | C7 H7 N O3 | 154.04973 | 111.03170, 126.05496, 154.04962 | 0.164 | |
| 31 | N-Acetyl-L-tyrosine | 3.719 | C11 H13 N O4 | 224.09151 | 58.02824, 180.06584, 222.07704, 227.17508, 245.18568 | 0.169 | |
| 32 | Trolox | 13.196 | C14 H18 O4 | 251.12491 | 223.13126, 249.11020, 264.15900, 267.12146 | 0.164 | |
| 33 | 1,6-Bis-O-[(2E)-3-(4-hydroxyphenyl)-2-propenoyl]-β-D-glucopyranose | 9.115 | C24 H24 O10 | 471.12958 | 125.02316, 169.01331, 471.12964, 475.03360 | 0.191 | |
| 34 | 4-Acetyl-3-hydroxy-5-methylphenyl β-D-glucopyranoside | 4.487 | C15 H20 O8 | 327.10852 | 59.01235, 147.04401, 165.05473 | 0.153 | |
| 35 | DL-4-Hydroxyphenyllactic acid | 3.152 | C9 H10 O4 | 181.04977 | 135.04395, 163.03909, 181.04985 | 0.095 | |
| 36 | Epicatechin | 0.908 | C15 H14 O6 | 291.08359 | 291.08368, 294.15421 | 0.054 | |
| 37 | 2,6-Dimethoxyphenol | 6.925 | C8 H10 O3 | 155.0701 | 155.06999 | 0.059 | |
| 38 | 5-Hydroxyindole-3-acetic acid | 5.398 | C10 H9 N O3 | 192.06537 | 146.05977, 174.05470, 195.08757 | 0.076 | |
| 39 | Ethamivan | 2.169 | C12 H17 N O3 | 224.12778 | 160.11180, 178.12234, 224.12762 | 0.029 | |
| 40 | 5-Sulfosalicylic acid | 4.509 | C7 H6 O6 S | 216.98065 | 93.03311, 137.02316, 216.98061 | 0.028 |
| Visceral Index | Kidney (%) | Liver (%) | Spleen (%) |
|---|---|---|---|
| NC | 1.35 ± 0.16 B | 4.49 ± 0.21 B | 0.32 ± 0.08 B |
| DC | 1.74 ± 0.24 A | 5.49 ± 0.16 A | 0.49 ± 0.06 A |
| PC | 1.52 ± 0.27 b | 4.74 ± 0.38 B | 0.38 ± 0.19 b |
| GEKEL | 1.49 ± 0.21 b | 4.69 ± 0.28 B | 0.36 ± 0.12 b |
| GEKEM | 1.42 ± 0.22 B | 4.62 ± 0.25 B | 0.31 ± 0.1 B |
| GEKEH | 1.41 ± 0.14 B | 4.51 ± 0.31 B | 0.36 ± 0.11 B |
| EKEL | 1.53 ± 0.18 | 4.76 ± 0.28 a,B | 0.45 ± 0.08 |
| EKEM | 1.51 ± 0.22 b | 4.64 ± 0.27 B | 0.41 ± 0.11 a |
| EKEH | 1.44 ± 0.24 B | 4.59 ± 0.46 B | 0.36 ± 0.17 b |
| Group | Glucose Value/(mmol/L) | AUC/(min·mmol/L) | ||||
|---|---|---|---|---|---|---|
| 0 min | 30 min | 60 min | 90 min | 120 min | ||
| NC | 5.2 ± 1.13 B | 13.7 ± 2.1 B | 10.4 ± 1.06 B | 5.7 ± 1.01 B | 3.6 ± 1.51 B | 1005 ± 148.69 B |
| DC | 19.8 ± 1.09 A | 26.00 ± 1.51 A | 23.2 ± 1.23 A | 21.2 ± 1.32 A | 20.3 ± 1.52 A | 2695.5 ± 201.88 A |
| PC | 6.8 ± 1.01 B | 17.8 ± 1.89 | 22.8 ± 1.62 a | 18.4 ± 1.53 A | 16.7 ± 1.28 A | 1981.5 ± 352.17 a,b |
| GEKEL | 12.9 ± 1.31 | 18.4 ± 1.81 | 23.3 ± 1.65 A | 21.3 ± 1.39 A | 19.1 ± 1.25 A | 2266.5 ± 532.18 A |
| GEKEM | 8.7 ± 1.18 b | 19.9 ± 1.46 a | 17.1 ± 1.38 a,b | 13.7 ± 1.42 | 10.4 ± 1.21 b | 1798.5 ± 561.86 a,b |
| GEKEH | 7.1 ± 1.16 B | 16.3 ± 1.35 b | 14.6 ± 1.28 b | 10.5 ± 1.56 B | 8.7 ± 1.40 B | 1443 ± 577.65 a,B |
| EKEL | 13.4 ± 1.21 a | 23.9 ± 1.68 A | 23.5 ± 1.46 A | 19.6 ± 1.52 A | 18.2 ± 1.26 A | 2431.5 ± 562.37 A |
| EKEM | 9.1 ± 1.13 b | 18.4 ± 1.59 | 16.3 ± 1.78 | 15.1 ± 1.23 A,b | 14.3 ± 1.12 A,b | 1858.5 ± 538.68 A |
| EKEH | 8.6 ± 1.2 b | 18.3 ± 1.39 b | 15.9 ± 1.57 b | 13.1 ± 1.38 a,b | 10.9 ± 1.51 b | 1705.5 ± 587.91 a,B |
| Group | T-CHO (mmol/L) | TG (mmol/L) | LDL-C (mmol/L) | HDL-C (mmol/L) |
|---|---|---|---|---|
| NC | 5.83 ± 0.22 B | 1.59 ± 0.09 b | 0.42 ± 0.21 B | 3.35 ± 0.21 b |
| DC | 6.89 ± 0.2 A | 1.81 ± 0.1 a | 0.77 ± 0.24 A | 2.83 ± 0.45 a |
| PC | 5.77 ± 0.17 | 1.68 ± 0.11 | 0.56 ± 0.27 b | 3.29 ± 0.24 b |
| GEKEL | 6.73 ± 0.26 A | 1.63 ± 0.12 b | 0.61 ± 0.16 a | 2.96 ± 0.20 |
| GEKEM | 6.01 ± 0.21 a,B | 1.52 ± 0.14 B | 0.57 ± 0.23 b | 3.14 ± 0.19 b |
| GEKEH | 5.79 ± 0.17 B | 1.39 ± 0.12 A,B | 0.3 ± 0.14 B | 3.23 ± 0.16 B |
| EKEL | 6.79 ± 0.18 A | 1.67 ± 0.10 | 0.64 ± 0.15 a | 2.87 ± 0.14 A |
| EKEM | 6.35 ± 0.17 | 1.57 ± 0.12 B | 0.54 ± 0.17 b | 2.98 ± 0.18 |
| EKEH | 6.02 ± 0.25 a,B | 1.48 ± 0.13 a,B | 0.39 ± 0.14 B | 3.17 ± 0.13 b |
| Group | ALB (μg/mL) | BUN (μg/mL) | Scr (μmol/L) |
|---|---|---|---|
| NC | 21.03 ± 0.92 B | 11.58 ± 1.02 B | 36.17 ± 1.32 B |
| DC | 29.77 ± 1.12 A | 19.47 ± 1.27 A | 40.85 ± 1.04 A |
| PC | 24.41 ± 1.30 b | 16.03 ± 1.42A,b | 34.17 ± 1.09 B |
| GEKEL | 24.79 ± 1.36 a,b | 15.11 ± 1.58 | 34.67 ± 1.14 b |
| GEKEM | 23.81 ± 1.21 B | 13.85 ± 1.33 B | 33.91 ± 1.01 B |
| GEKEH | 22.51 ± 1.31 B | 14.27 ± 1.09 a,B | 33.08 ± 1.03 a,B |
| EKEL | 25.41 ± 1.49 | 15.93 ± 1.43 | 38.98 ± 1.11 |
| EKEM | 25.15 ± 1.37 a | 15.35 ± 1.06 | 35.97 ± 0.94 b |
| EKEH | 24.52 ± 1.75 b | 14.09 ± 1.10 B | 34.81 ± 1.10 b |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, Y.; Yuan, H.; Wang, Y. Treatment of Diabetes Nephropathy in Mice by Germinating Seeds of Euryale ferox through Improving Oxidative Stress. Foods 2023, 12, 767. https://doi.org/10.3390/foods12040767
Wang Y, Yuan H, Wang Y. Treatment of Diabetes Nephropathy in Mice by Germinating Seeds of Euryale ferox through Improving Oxidative Stress. Foods. 2023; 12(4):767. https://doi.org/10.3390/foods12040767
Chicago/Turabian StyleWang, Yani, Huaibo Yuan, and Yidi Wang. 2023. "Treatment of Diabetes Nephropathy in Mice by Germinating Seeds of Euryale ferox through Improving Oxidative Stress" Foods 12, no. 4: 767. https://doi.org/10.3390/foods12040767
APA StyleWang, Y., Yuan, H., & Wang, Y. (2023). Treatment of Diabetes Nephropathy in Mice by Germinating Seeds of Euryale ferox through Improving Oxidative Stress. Foods, 12(4), 767. https://doi.org/10.3390/foods12040767




