Axial Length and Prevalence of Myopia among Schoolchildren in the Equatorial Region of Brazil
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Measures
2.3. Questionnaire
2.4. Statistical Analysis
3. Results
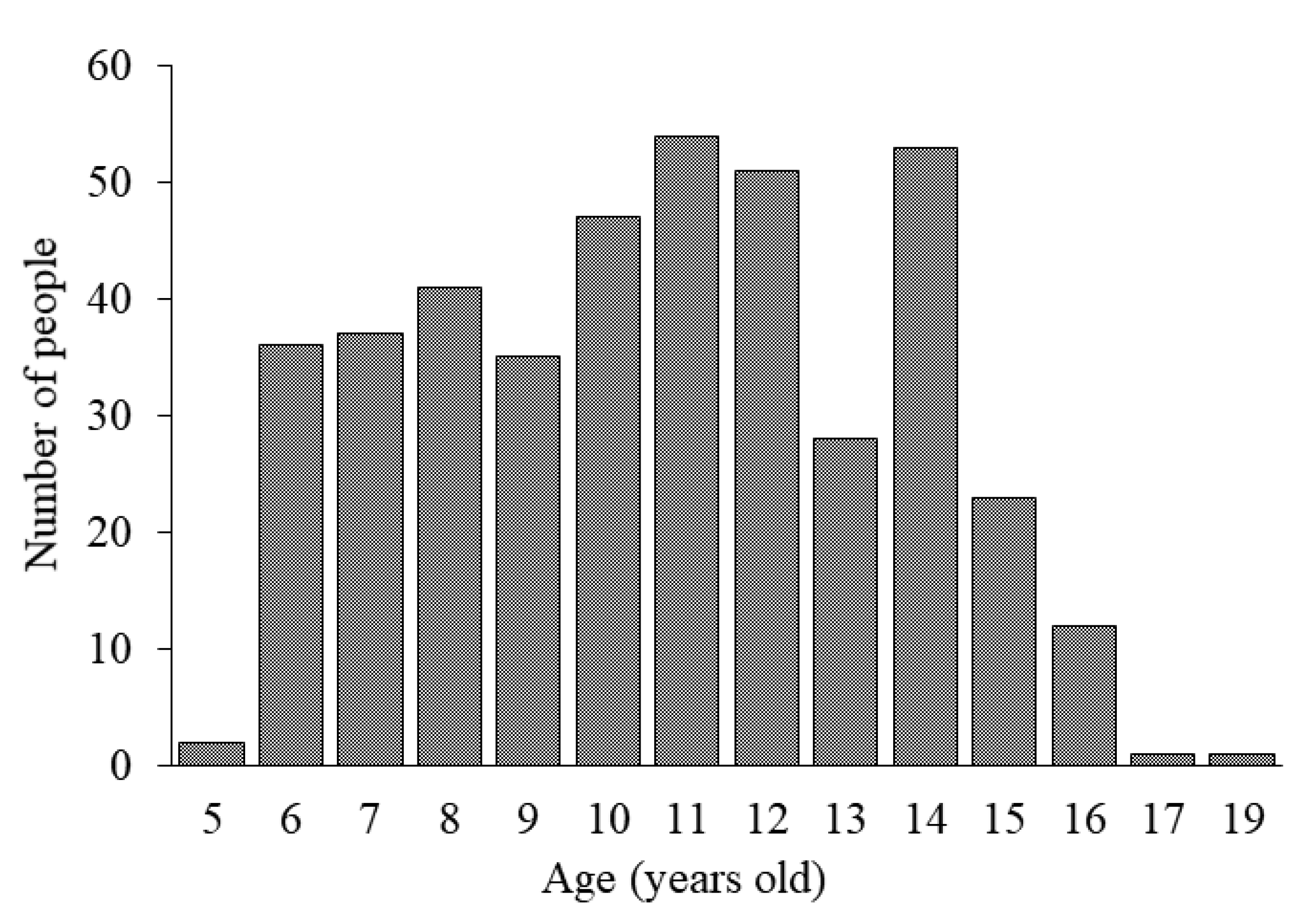
3.1. Study Population
3.2. Illuminance and Violet Light Irradiance
3.3. Factors Affecting SE and AL According to Simple Correlation and Multiple Regression Analyses
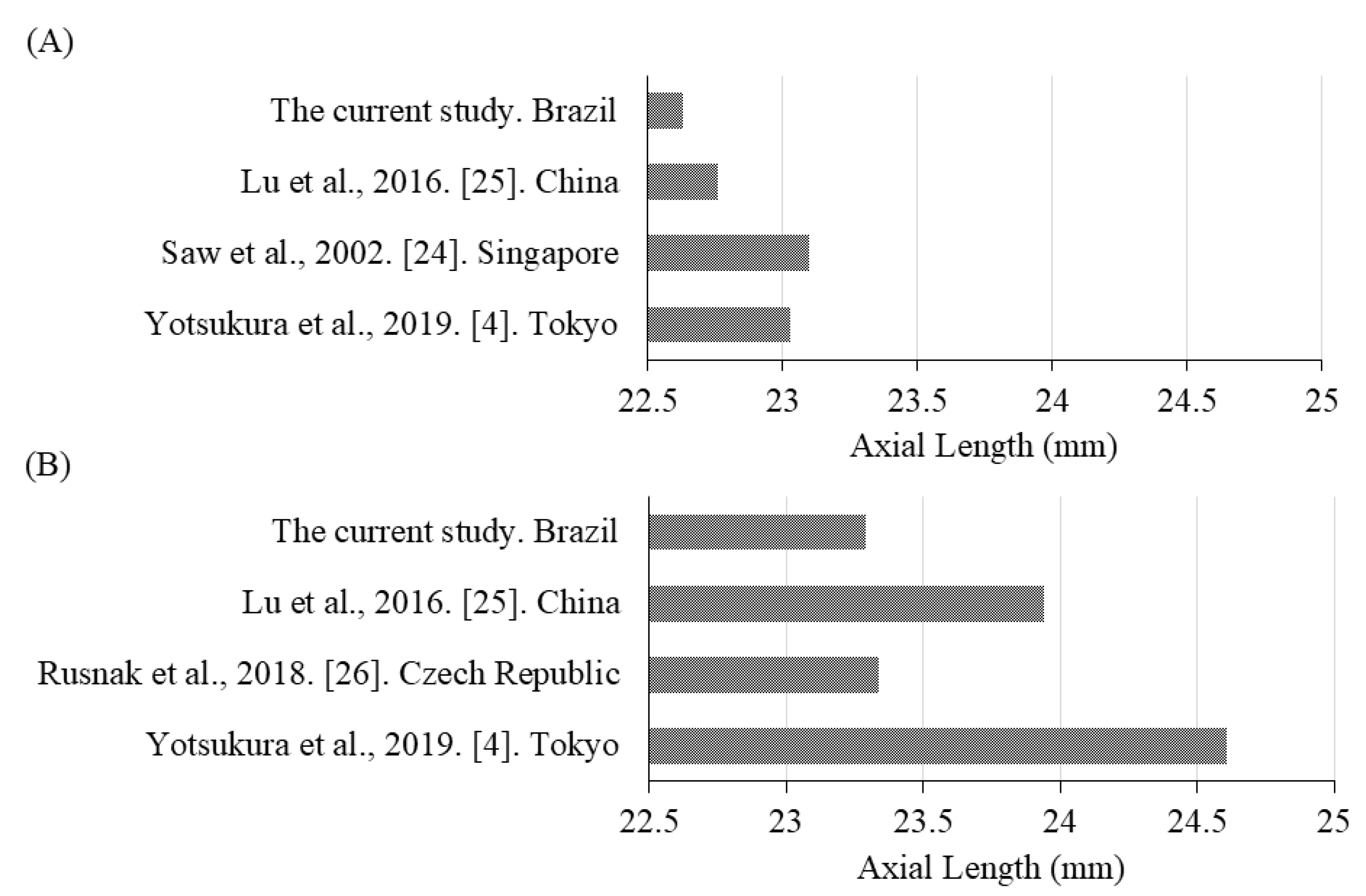
4. Discussion
5. Conclusions
6. Patents
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Morgan, I.G.; Ohno-Matsui, K.; Saw, S.-M. Myopia. Lancet 2012, 379, 1739–1748. [Google Scholar] [CrossRef]
- Foster, P.J.; Jiang, Y. Epidemiology of myopia. Eye 2014, 28, 202–208. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dolgin, E. The myopia boom. Nature 2015, 519, 276–278. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yotsukura, E.; Torii, H.; Inokuchi, M.; Tokumura, M.; Uchino, M.; Nakamura, K.; Hyodo, M.; Mori, K.; Jiang, X.; Ikeda, S.-I.; et al. Current Prevalence of Myopia and Association of Myopia With Environmental Factors Among Schoolchildren in Japan. JAMA Ophthalmol. 2019, 137, 1233–1239. [Google Scholar] [CrossRef] [PubMed]
- Sherwin, J.C.; Reacher, M.H.; Keogh, R.H.; Khawaja, A.P.; Mackey, D.A.; Foster, P.J. The association between time spent outdoors and myopia in children and adolescents: A systematic review and meta-analysis. Ophthalmology 2012, 119, 2141–2151. [Google Scholar] [CrossRef] [PubMed]
- Jones, L.A.; Sinnott, L.T.; Mutti, D.O.; Mitchell, G.L.; Moeschberger, M.L.; Zadnik, K. Parental history of myopia, sports and outdoor activities, and future myopia. Investig. Ophthalmol. Vis. Sci. 2007, 48, 3524–3532. [Google Scholar] [CrossRef] [Green Version]
- Rose, K.A.; Morgan, I.G.; Ip, J.; Kifley, A.; Huynh, S.; Smith, W.; Mitchell, P. Outdoor activity reduces the prevalence of myopia in children. Ophthalmology 2008, 115, 1279–1285. [Google Scholar] [CrossRef]
- Xiong, S.; Sankaridurg, P.; Naduvilath, T.; Zang, J.; Zou, H.; Zhu, J.; Lv, M.; He, X.; Xu, X. Time spent in outdoor activities in relation to myopia prevention and control: A meta-analysis and systematic review. Acta Ophthalmol. 2017, 95, 551–566. [Google Scholar] [CrossRef] [Green Version]
- Ho, C.-L.; Wu, W.-F.; Liou, Y.M. Dose-Response Relationship of Outdoor Exposure and Myopia Indicators: A Systematic Review and Meta-Analysis of Various Research Methods. Int. J. Environ. Res. Public Health 2019, 16, 2595. [Google Scholar] [CrossRef] [Green Version]
- Ashby, R.S.; Ohlendorf, A.; Schaeffel, F. The effect of ambient illuminance on the development of deprivation myopia in chicks. Investig. Ophthalmol. Vis. Sci. 2009, 50, 5348–5354. [Google Scholar] [CrossRef] [Green Version]
- Karouta, C.; Ashby, R.S. Correlation Between Light Levels and the Development of Deprivation Myopia. Investig. Ophthalmol. Vis. Sci. 2015, 56, 299–309. [Google Scholar] [CrossRef]
- Torii, H.; Kurihara, T.; Seko, Y.; Negishi, K.; Ohnuma, K.; Inaba, T.; Kawashima, M.; Jiang, X.; Kondo, S.; Miyauchi, M.; et al. Violet Light Exposure Can Be a Preventive Strategy Against Myopia Progression. EBioMedicine 2017, 15, 210–219. [Google Scholar] [CrossRef] [Green Version]
- Torii, H.; Ohnuma, K.; Kurihara, T.; Tsubota, K.; Negishi, K. Violet Light Transmission is Related to Myopia Progression in Adult High Myopia. Sci. Rep. 2017, 7, 14523. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Troilo, D.; Smith, E.L., 3rd; Nickla, D.L.; Ashby, R.; Tkatchenko, A.V.; Ostrin, L.A.; Gawne, T.J.; Pardue, M.T.; Summers, J.A.; Kee, C.S.; et al. IMI—Report on Experimental Models of Emmetropization and Myopia. Investig. Ophthalmol. Vis. Sci. 2019, 60, M31–M88. [Google Scholar] [CrossRef] [Green Version]
- Saw, S.-M.; Zhang, M.-Z.; Hong, R.-Z.; Fu, Z.-F.; Pang, M.-H.; Tan, D.T.H. Near-work activity, night-lights, and myopia in the Singapore-China study. Arch. Ophthalmol. 2002, 120, 620–627. [Google Scholar] [CrossRef] [PubMed]
- Lin, Z.; Vasudevan, B.; Jhanji, V.; Mao, G.Y.; Gao, T.Y.; Wang, F.H.; Rong, S.S.; Ciuffreda, K.; Liang, Y.B. Near work, outdoor activity, and their association with refractive error. Optom. Vis. Sci. 2014, 91, 376–382. [Google Scholar] [CrossRef]
- Mutti, D.O.; Mitchell, G.L.; Moeschberger, M.L.; Jones, L.A.; Zadnik, K. Parental myopia, near work, school achievement, and children’s refractive error. Investig. Ophthalmol. Vis. Sci. 2002, 43, 3633–3640. [Google Scholar]
- Ip, J.M.; Saw, S.-M.; Rose, K.A.; Morgan, I.G.; Kifley, A.; Liew, G.; Mitchell, P. Role of near work in myopia: Findings in a sample of Australian school children. Investig. Ophthalmol. Vis. Sci. 2008, 49, 2903–2910. [Google Scholar] [CrossRef]
- Pan, C.-W.; Ramamurthy, D.; Saw, S.-M. Worldwide prevalence and risk factors for myopia. Ophthalmic. Physiol. Opt. 2012, 32, 3–16. [Google Scholar] [CrossRef]
- Yang, M.-L.; Huang, C.-Y.; Hou, C.-H.; Lin, K.-K.; Lee, J.-S. Relationship of lifestyle and body stature growth with the development of myopia and axial length elongation in Taiwanese elementary school children. Indian J. Ophthalmol. 2014, 62, 865–869. [Google Scholar] [CrossRef] [PubMed]
- Schaal, L.F.; Schellini, S.A.; Pesci, L.T.; Galindo, A.; Padovani, C.R.; Corrente, J.E. The Prevalence of Strabismus and Associated Risk Factors in a Southeastern Region of Brazil. Semin. Ophthalmol. 2018, 33, 357–360. [Google Scholar] [CrossRef] [PubMed]
- Lira, R.P.C.; Santo, I.F.D.E.; Astur, G.L.D.V.; Maziero, D.; Passos, T.H.M.; Arieta, C.E.L. Refractive error in school children in Campinas, Brazil. Arq. Bras. Oftalmol. 2014, 77, 203–204. [Google Scholar] [CrossRef] [Green Version]
- Ferraz, F.H.; Corrente, J.E.; Opromolla, P.A.; Padovani, C.R.; Schellini, S.A. Refractive errors in a Brazilian population: Age and sex distribution. Ophthalmic. Physiol. Opt. 2015, 35, 19–27. [Google Scholar] [CrossRef]
- Saw, S.-M.; Chua, W.-H.; Hong, C.-Y.; Wu, H.-M.; Chia, K.-S.; A Stone, R.; Tan, D. Height and its relationship to refraction and biometry parameters in Singapore Chinese children. Investig. Ophthalmol. Vis. Sci. 2002, 43, 1408–1413. [Google Scholar]
- Lu, T.L.; Wu, J.F.; Ye, X.; Hu, Y.Y.; Wu, H.; Sun, W.; Guo, D.D.; Wang, X.R.; Bi, H.; Jonas, J.B. Axial Length and Associated Factors in Children: The Shandong Children Eye Study. Ophthalmologica 2016, 235, 78–86. [Google Scholar] [CrossRef] [PubMed]
- Rusnak, S.; Salcman, V.; Hecova, L.; Kasl, Z. Myopia Progression Risk: Seasonal and Lifestyle Variations in Axial Length Growth in Czech Children. J. Ophthalmol. 2018, 2018, 5076454. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lira, R.P.C.; Arieta, C.E.L.; Passos, T.H.M.; Maziero, D.; Astur, G.L.D.V.; Santo Ítalo, F.D.E.; Bertolani, A.C.; Pozzi, L.F.; De Castro, R.S.; Ferraz, Á.B. Distribution of Ocular Component Measures and Refraction in Brazilian School Children. Ophthalmic. Epidemiol. 2017, 24, 29–35. [Google Scholar] [CrossRef] [PubMed]
- French, A.N.; Morgan, I.G.; Mitchell, P.; Rose, K.A. Risk factors for incident myopia in Australian schoolchildren: The Sydney adolescent vascular and eye study. Ophthalmology 2013, 120, 2100–2108. [Google Scholar] [CrossRef]
- Li, S.-M.; Li, S.-Y.; Kang, M.-T.; Zhou, Y.; Liu, L.-R.; Li, H.; Wang, Y.-P.; Zhan, S.-Y.; Gopinath, B.; Mitchell, P.; et al. Anyang Childhood Eye Study, Near Work Related Parameters and Myopia in Chinese Children: The Anyang Childhood Eye Study. PLoS ONE 2015, 10, e0134514. [Google Scholar] [CrossRef]
- You, Q.S.; Wu, L.J.; Duan, J.L.; Luo, Y.X.; Liu, L.J.; Li, X.; Gao, Q.; Wang, W.; Xu, L.; Jonas, J.B.; et al. Factors Associated with Myopia in School Children in China: The Beijing Childhood Eye Study. PLoS ONE 2012, 7, e52668. [Google Scholar] [CrossRef]
- Gong, Y.; Zhang, X.; Tian, D.; Wang, D.; Xiao, G. Parental myopia, near work, hours of sleep and myopia in Chinese children. Health 2014, 6, 64–70. [Google Scholar] [CrossRef]
- Huang, H.-M.; Chang, D.S.-T.; Wu, P.-C. The Association between Near Work Activities and Myopia in Children-A Systematic Review and Meta-Analysis. PLoS ONE 2015, 10, e0140419. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bucksch, J.; Sigmundova, D.; Hamrik, Z.; Troped, P.J.; Melkevik, O.; Ahluwalia, N.; Borraccino, A.; Tynjälä, J.; Kalman, M.; Inchley, J.C. International Trends in Adolescent Screen-Time Behaviors From 2002 to 2010. J. Adolesc. Health 2016, 58, 417–425. [Google Scholar] [CrossRef] [PubMed]
- Bassett, D.R.; John, D.; Conger, S.A.; Fitzhugh, E.C.; Coe, D.P. Trends in Physical Activity and Sedentary Behaviors of United States Youth. J. Phys. Act. Health 2015, 12, 1102–1111. [Google Scholar] [CrossRef] [PubMed]
- Read, S.A.; Collins, M.J.; Vincent, S.J. Light exposure and physical activity in myopic and emmetropic children. Optom. Vis. Sci. 2014, 91, 330–341. [Google Scholar] [CrossRef] [Green Version]
- Guo, Y.; Liu, L.J.; Xu, L.; Lv, Y.Y.; Tang, P.; Feng, Y.; Meng, M.; Jonas, J.B. Outdoor activity and myopia among primary students in rural and urban regions of Beijing. Ophthalmology 2013, 120, 277–283. [Google Scholar] [CrossRef]
- French, A.N.; Ashby, R.S.; Morgan, I.G.; Rose, K.A. Time outdoors and the prevention of myopia. Exp. Eye Res. 2013, 114, 58–68. [Google Scholar] [CrossRef] [Green Version]
- Guggenheim, J.A.; Northstone, K.; McMahon, G.; Ness, A.R.; Deere, K.; Mattocks, C.; Pourcain, B.S.; Williams, C. Time outdoors and physical activity as predictors of incident myopia in childhood: A prospective cohort study. Investig. Ophthalmol. Vis. Sci. 2012, 53, 2856–2865. [Google Scholar] [CrossRef]
- Dirani, M.; Tong, L.; Gazzard, G.; Zhang, X.; Chia, A.; Young, T.L.; Rose, K.A.; Mitchell, P.; Saw, S.-M. Outdoor activity and myopia in Singapore teenage children. Br. J. Ophthalmol. 2009, 93, 997–1000. [Google Scholar] [CrossRef]
- Jones-Jordan, L.A.; Sinnott, L.T.; Graham, N.D.; Cotter, S.A.; Kleinstein, R.N.; Manny, R.E.; Mutti, D.O.; Twelker, J.D.; Zadnik, K. The contributions of near work and outdoor activity to the correlation between siblings in the Collaborative Longitudinal Evaluation of Ethnicity and Refractive Error (CLEERE) Study. Investig. Ophthalmol. Vis. Sci. 2014, 55, 6333–6339. [Google Scholar] [CrossRef] [Green Version]
- Wu, P.-C.; Tsai, C.-L.; Wu, H.-L.; Yang, Y.-H.; Kuo, H.-K. Outdoor activity during class recess reduces myopia onset and progression in school children. Ophthalmology 2013, 120, 1080–1085. [Google Scholar] [CrossRef]
- Jin, J.-X.; Hua, W.; Jiang, X.; Wu, X.; Yang, J.-W.; Gao, G.; Fang, Y.; Pei, C.-L.; Wang, S.; Zhang, J.-Z.; et al. Effect of outdoor activity on myopia onset and progression in school-aged children in northeast China: The Sujiatun Eye Care Study. BMC Ophthalmol. 2015, 15, 73. [Google Scholar] [CrossRef] [Green Version]
- He, M.; Xiang, F.; Zeng, Y.; Mai, J.; Chen, Q.; Zhang, J.; Smith, W.; Rose, K.; Morgan, I.G. Effect of Time Spent Outdoors at School on the Development of Myopia Among Children in China: A Randomized Clinical Trial. JAMA 2015, 314, 1142–1148. [Google Scholar] [CrossRef] [Green Version]
- Tkatchenko, T.V.; Shen, Y.; Braun, R.D.; Bawa, G.; Kumar, P.; Avrutsky, I.; Tkatchenko, A.V. Photopic visual input is necessary for emmetropization in mice. Exp. Eye Res. 2013, 115, 87–95. [Google Scholar] [CrossRef] [Green Version]
- Norton, T.T.; Siegwart, J.T., Jr. Light levels, refractive development, and myopia—A speculative review. Exp. Eye Res. 2013, 114, 48–57. [Google Scholar] [CrossRef] [Green Version]
- World Weather Online. Available online: https://www.worldweatheronline.com/ (accessed on 23 September 2020).
- Saw, S.-M.; Tong, L.; Chua, W.-H.; Chia, K.-S.; Koh, D.; Tan, D.T.H.; Katz, J. Incidence and progression of myopia in Singaporean school children. Investig. Ophthalmol. Vis. Sci. 2005, 46, 51–57. [Google Scholar] [CrossRef]
- Saw, S.-M.; Tan, S.-B.; Fung, D.; Chia, K.-S.; Koh, D.; Tan, D.T.H.; Stone, R.A. Stone, IQ and the association with myopia in children. Investig. Ophthalmol. Vis. Sci. 2004, 45, 2943–2948. [Google Scholar] [CrossRef] [Green Version]
- Quek, T.P.L.; Chua, C.G.; Chong, C.S.; Chong, J.H.; Hey, H.W.; Lee, J.; Lim, Y.F.; Saw, S.-M. Prevalence of refractive errors in teenage high school students in Singapore. Ophthalmic. Physiol. Opt. 2004, 24, 47–55. [Google Scholar] [CrossRef]
- Read, S.A.; Vincent, S.J.; Tan, C.-S.; Ngo, C.; Collins, M.J.; Saw, S.-M. Patterns of Daily Outdoor Light Exposure in Australian and Singaporean Children. Transl. Vis. Sci. Technol. 2018, 7, 8. [Google Scholar] [CrossRef] [Green Version]
- Ayaki, M.; Torii, H.; Tsubota, K.; Negishi, K. Decreased sleep quality in high myopia children. Sci. Rep. 2016, 6, 33902. [Google Scholar] [CrossRef]
- Hashemi, H.; Asharlous, A.; Khabazkhoob, M.; Iribarren, R.; Khosravi, A.; Yekta, A.; Emamian, M.H.; Fotouhi, A. The Effect of Cyclopentolate on Ocular Biometric Components. Optom. Vis. Sci. 2020, 97, 440–447. [Google Scholar] [CrossRef] [PubMed]

| Number of Cases | Mean ± Standard Deviation (Range) | |
|---|---|---|
| Age (years) | 10.6 ± 2.9 (5.0–19.0) | |
| Number of students | 421 | |
| Males | 212 | |
| Females | 209 | |
| Height (cm) | 417 | 144.5 ± 15.6 (110.0–179.0) |
| Weight (kg) | 416 | 40.4 ± 13.9 (16.7–91.2) |
| BMI (kg/m2) | 416 | 18.8 ± 3.6 (12.1–31.9) |
| SE (D) | 421 | −0.44 ± 1.38 (−12.63–7.25) |
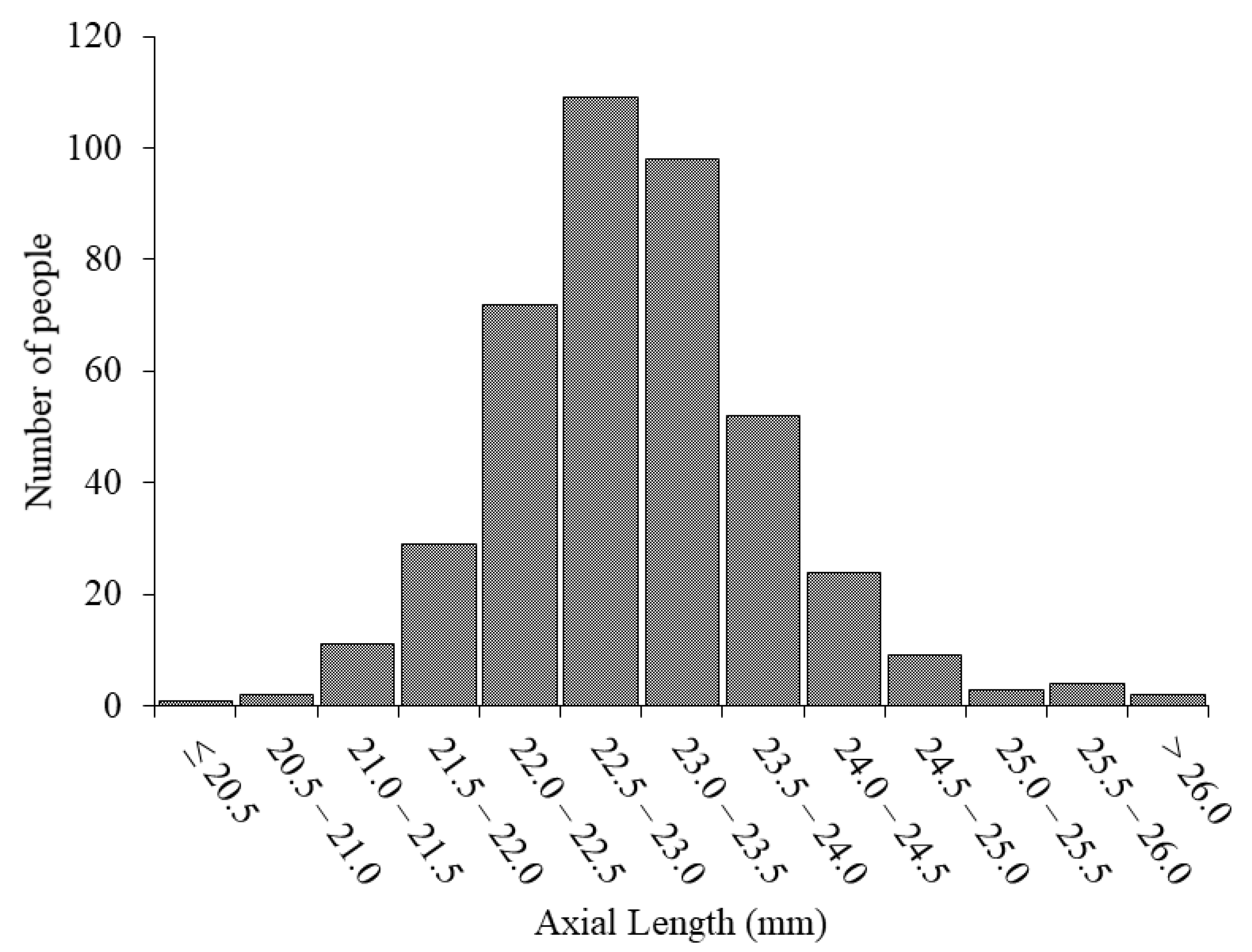
| AL (mm) | 416 | 22.98 ± 0.87 (20.16–26.90) |
| Time spent outdoors (min/day) | 123 | 155.9 ± 104.3 (9.3–540.0) |
| Time spent in near work (min/day) | 121 | 516.4 ± 248.3 (60.0–1096.5) |
| Time spent sleeping (min/day) | 113 | 507.8 ± 100.7 (300.0–875.0) |
| Family economic status | ||
| Less than BRL 1000 | 42 | |
| BRL 1000 to 3000 | 19 | |
| BRL 3000 to 5000 | 5 | |
| More than BRL 5000 | 5 | |
| Unknown | 171 | |
| Number of parents with myopia | ||
| 0 | 158 | |
| 1 | 38 | |
| 2 | 6 | |
| Unknown | 219 |
| Univariate Analysis | Multivariate Analysis | ||||
|---|---|---|---|---|---|
| Variable | Correlation Coefficient | p Value | Coefficient | Standard Error | p Value |
| Age (years) | −0.170 | <0.001 * | −0.082 | 0.023 | <0.001 * |
| Sex (males = 0, females = 1) | −0.041 | 0.201 | N/A | N/A | ≥0.05 |
| BMI | −0.075 | 0.062 | N/A | N/A | ≥0.05 |
| Univariate Analysis | Multivariate Analysis | ||||
|---|---|---|---|---|---|
| Variable | Correlation Coefficient | p Value | Coefficient | Standard Error | p Value |
| Age (years) | 0.326 | <0.001 * | 0.079 | 0.015 | <0.001 * |
| Sex (males = 0, females = 1) | −0.267 | <0.001 * | −0.438 | 0.078 | <0.001 * |
| BMI | 0.248 | <0.001 * | 0.031 | 0.012 | 0.01 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yotsukura, E.; Torii, H.; Ozawa, H.; Hida, R.Y.; Shiraishi, T.; Corso Teixeira, I.; Rautha, Y.V.B.L.; Moraes do Nascimento, C.F.; Mori, K.; Uchino, M.; et al. Axial Length and Prevalence of Myopia among Schoolchildren in the Equatorial Region of Brazil. J. Clin. Med. 2021, 10, 115. https://doi.org/10.3390/jcm10010115
Yotsukura E, Torii H, Ozawa H, Hida RY, Shiraishi T, Corso Teixeira I, Rautha YVBL, Moraes do Nascimento CF, Mori K, Uchino M, et al. Axial Length and Prevalence of Myopia among Schoolchildren in the Equatorial Region of Brazil. Journal of Clinical Medicine. 2021; 10(1):115. https://doi.org/10.3390/jcm10010115
Chicago/Turabian StyleYotsukura, Erisa, Hidemasa Torii, Hiroko Ozawa, Richard Yudi Hida, Tetsuro Shiraishi, Ivan Corso Teixeira, Yessa Vervloet Bertollo Lamego Rautha, Caio Felipe Moraes do Nascimento, Kiwako Mori, Miki Uchino, and et al. 2021. "Axial Length and Prevalence of Myopia among Schoolchildren in the Equatorial Region of Brazil" Journal of Clinical Medicine 10, no. 1: 115. https://doi.org/10.3390/jcm10010115








