Analysis of Mortality and Morbidity in COVID-19 Patients with Obesity Using Clinical Epidemiological Data from the Korean Center for Disease Control & Prevention
Abstract
1. Introduction
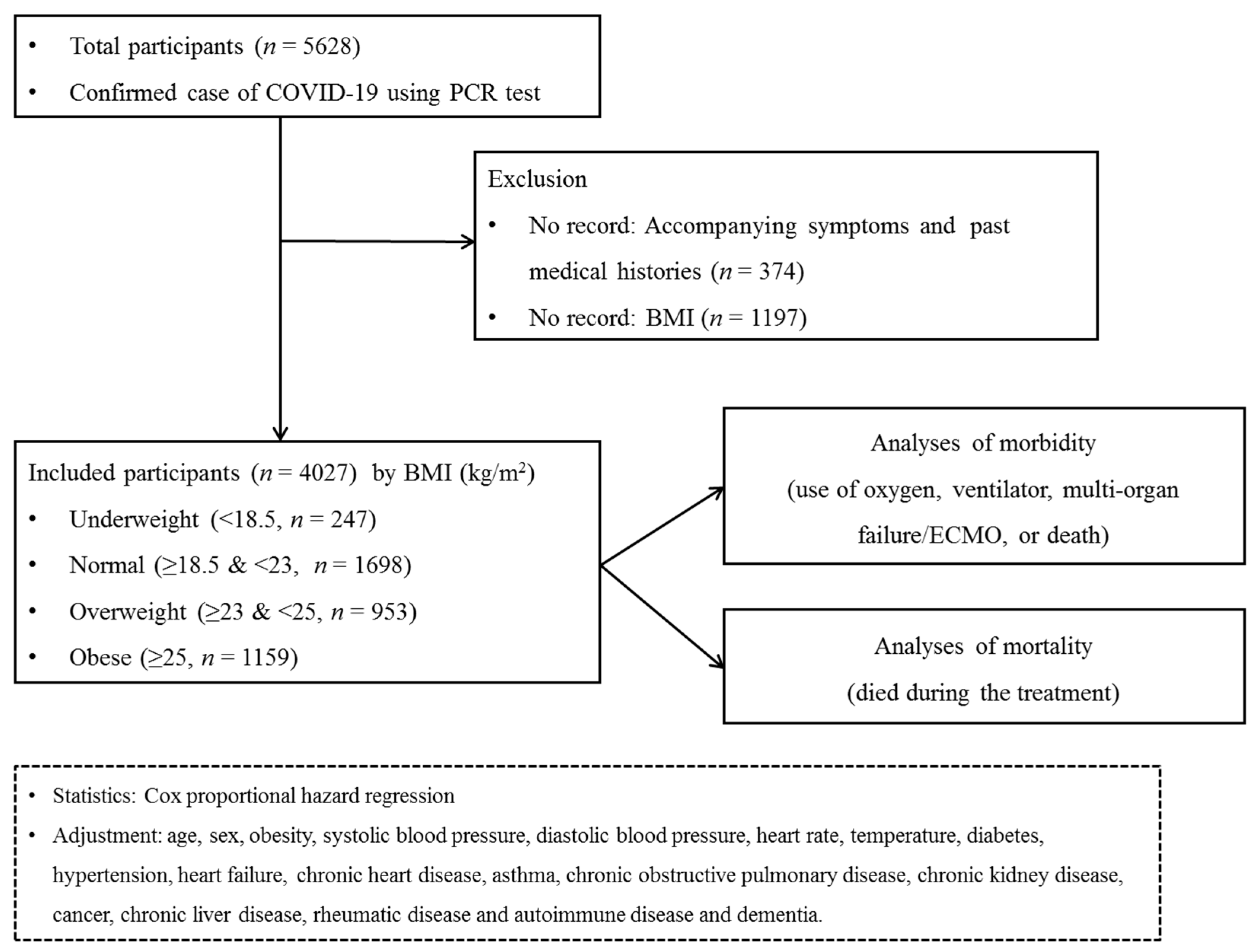
2. Materials and Methods
2.1. Ethics
2.2. Study Population and Participant Selection
2.3. Exposure (Obesity)
2.4. Outcome (Mortality)
2.5. Outcome (Maximum Level of Morbidity)
2.6. Covariates
2.7. Statistical Analyses
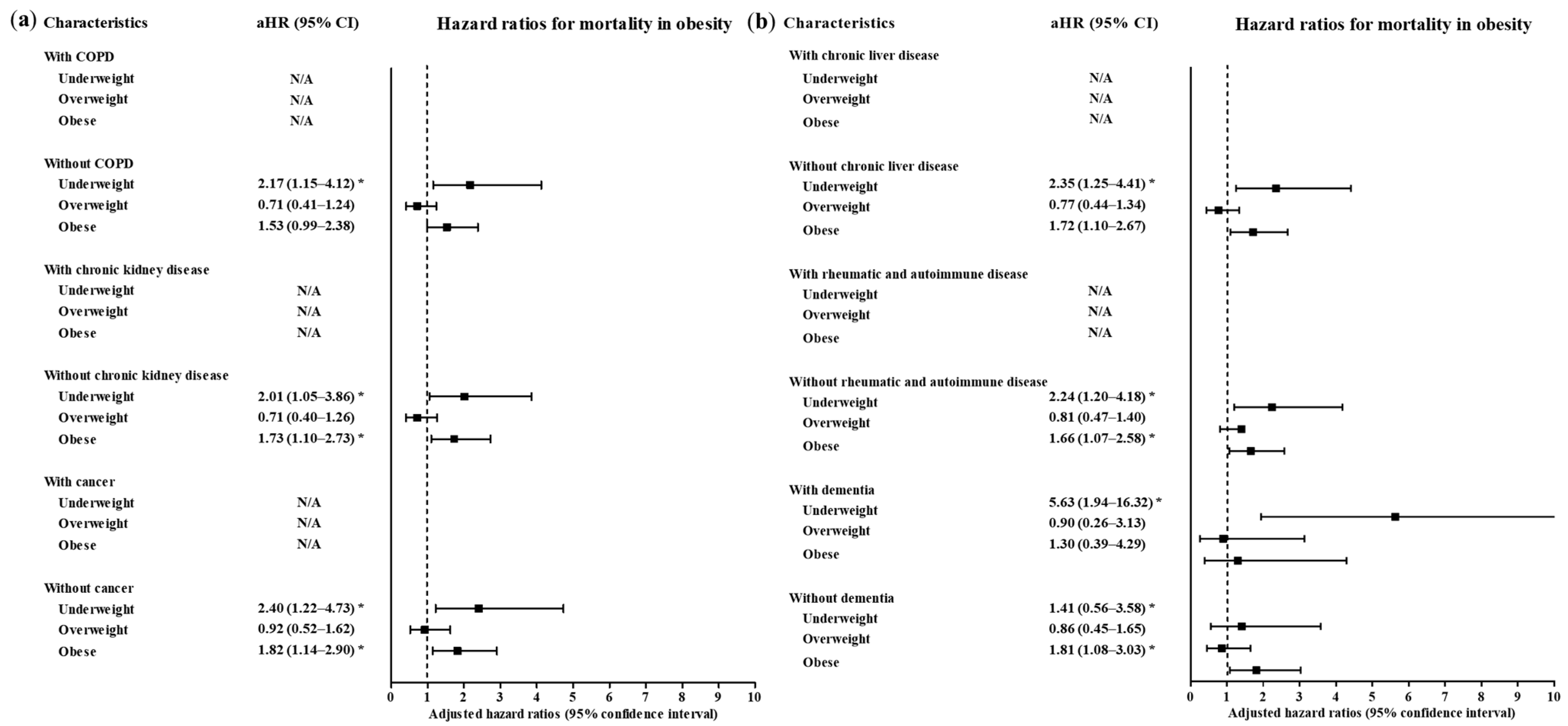
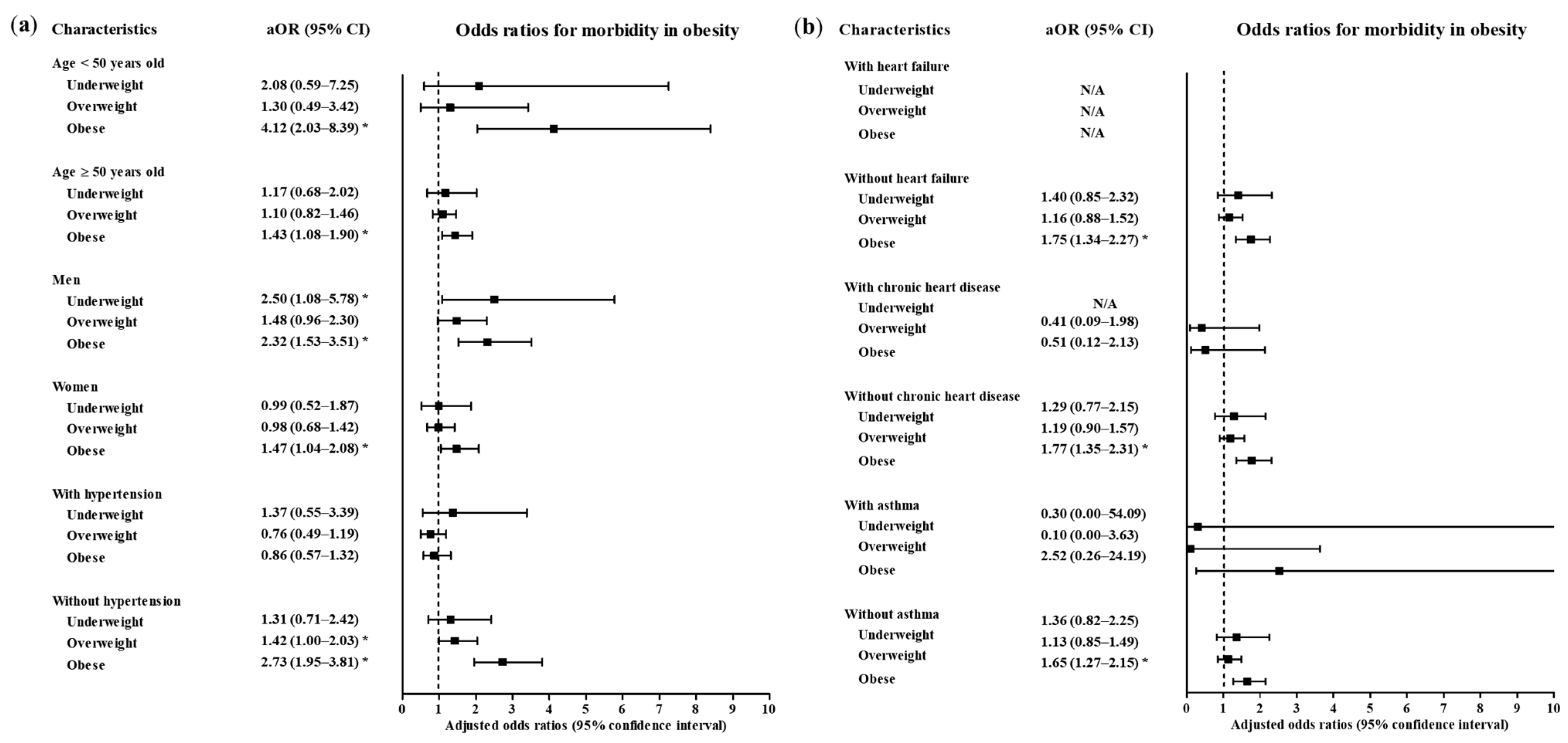
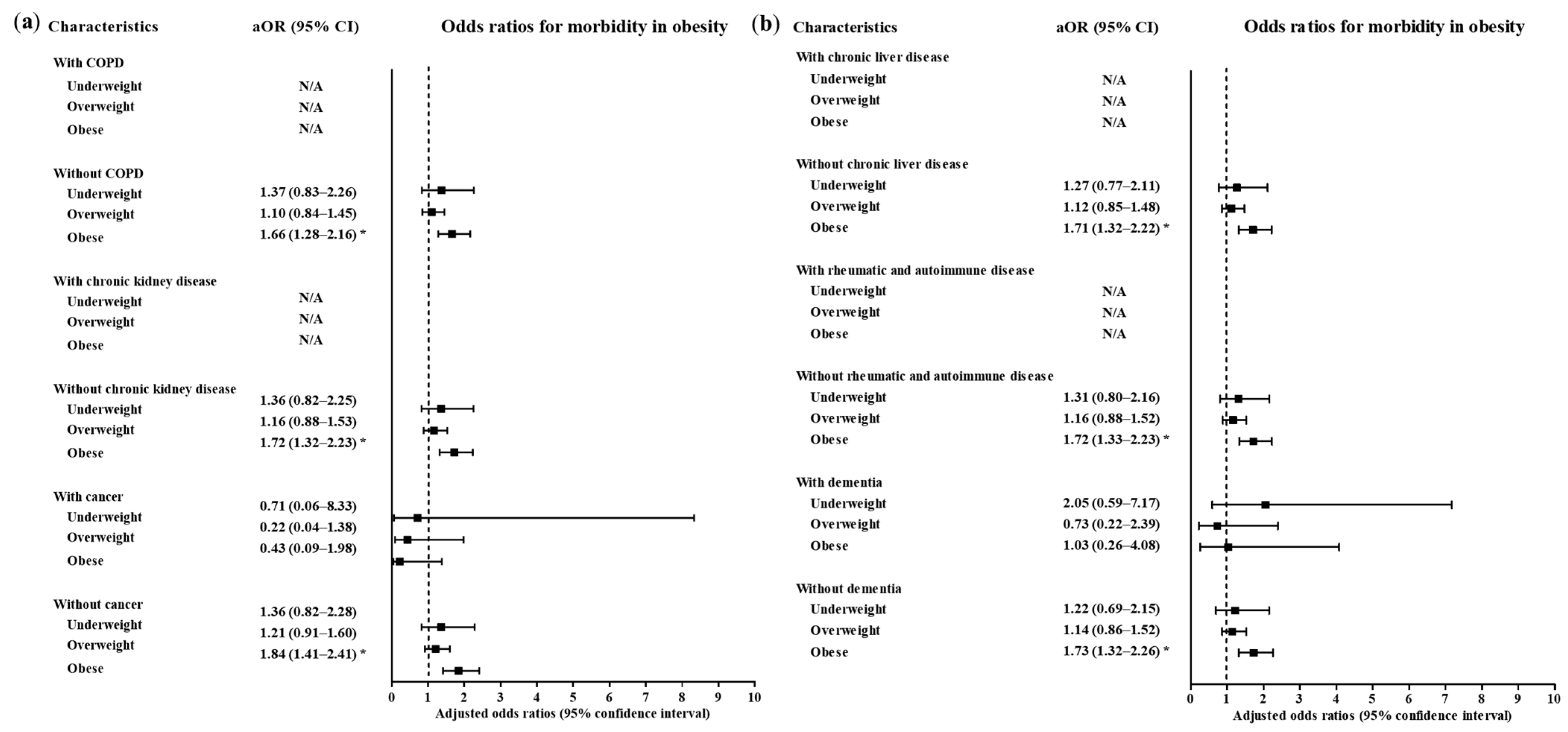
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
References
- WHO. Coronavirus Disease (COVID-19) Weekly Epidemiological Update and Weekly Operational Update 2020. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports/ (accessed on 2 November 2020).
- Kim, D.; Lee, J.-Y.; Yang, J.-S.; Kim, J.W.; Kim, V.N.; Chang, H. The Architecture of SARS-CoV-2 Transcriptome. Cell 2020, 181, 914–921.e10. [Google Scholar] [CrossRef] [PubMed]
- Gordon, D.E.; Jang, G.M.; Bouhaddou, M.; Xu, J.; Obernier, K.; O’Meara, M.; Rezelj, V.; Guo, J.; Swaney, D.; Tummino, T.; et al. A SARS-CoV-2-human protein-protein interaction map reveals drug targets and potential drug-repurposing. BioRxiv 2020. [Google Scholar] [CrossRef]
- Liu, D.; Zhang, W.; Pan, F.; Li, L.; Yang, L.; Zheng, D.; Wang, J.; Liang, B. The pulmonary sequalae in discharged patients with COVID-19: A short-term observational study. Respir. Res. 2020, 21, 125. [Google Scholar] [CrossRef] [PubMed]
- Kotfis, K.; Roberson, S.W.; Wilson, J.E.; Dabrowski, W.; Pun, B.T.; Ely, E.W. COVID-19: ICU delirium management during SARS-CoV-2 pandemic. Crit. Care 2020, 24, 176. [Google Scholar] [CrossRef]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- Chen, T.; Wu, D.; Chen, H.; Yan, W.; Yang, D.; Chen, G.; Ma, K.; Xu, D.; Yu, H.; Wang, H.; et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: Retrospective study. BMJ 2020, 368, m1091. [Google Scholar] [CrossRef]
- Petrilli, C.M.; Jones, S.A.; Yang, J.; Rajagopalan, H.; O’Donnell, L.; Chernyak, Y.; Tobin, K.A.; Cerfolio, R.J.; Francois, F.; Horwitz, L.I. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: Prospective cohort study. BMJ 2020, 369, m1966. [Google Scholar] [CrossRef]
- Seiglie, J.A.; Platt, J.; Cromer, S.J.; Bunda, B.; Foulkes, A.S.; Bassett, I.V.; Hsu, J.; Meigs, J.B.; Leong, A.; Putman, M.S.; et al. Diabetes as a Risk Factor for Poor Early Outcomes in Patients Hospitalized With COVID-19. Diabetes Care 2020, 43, 2938–2944. [Google Scholar] [CrossRef]
- Sattar, N.; McInnes, I.B.; McMurray, J.J. Obesity Is a Risk Factor for Severe COVID-19 Infection. Circulation 2020, 142, 4–6. [Google Scholar] [CrossRef]
- Klang, E.; Kassim, G.; Soffer, S.; Freeman, R.; Levin, M.A.; Reich, D.L. Severe Obesity as an Independent Risk Factor for COVID-19 Mortality in Hospitalized Patients Younger than 50. Obesity 2020, 28, 1595–1599. [Google Scholar] [CrossRef]
- Palaiodimos, L.; Kokkinidis, D.G.; Li, W.; Karamanis, D.; Ognibene, J.; Arora, S.; Southern, W.N.; Mantzoros, C.S. Severe obesity, increasing age and male sex are independently associated with worse in-hospital outcomes, and higher in-hospital mortality, in a cohort of patients with COVID-19 in the Bronx, New York. Metabolism 2020, 108, 154262. [Google Scholar] [CrossRef] [PubMed]
- Popkin, B.; Du, S.; Green, W.D.; Beck, M.A.; Algaith, T.; Herbst, C.H.; Alsukait, R.F.; Alluhidan, M.; Alazemi, N.; Shekar, M. Individuals with obesity and COVID-19: A global perspective on the epidemiology and biological relationships. Obes. Rev. 2020, 21. [Google Scholar] [CrossRef] [PubMed]
- Cai, Q.; Chen, F.; Wang, T.; Luo, F.; Liu, X.; Wu, Q.; He, Q.; Wang, Z.; Liu, Y.; Liu, L.; et al. Obesity and COVID-19 Severity in a Designated Hospital in Shenzhen, China. Diabetes Care 2020, 43, 1392–1398. [Google Scholar] [CrossRef] [PubMed]
- Kalligeros, M.; Shehadeh, F.; Mylona, E.K.; Benitez, G.; Beckwith, C.G.; Chan, P.A.; Mylonakis, E. Association of Obesity with Disease Severity Among Patients with Coronavirus Disease 2019. Obesity 2020, 28, 1200–1204. [Google Scholar] [CrossRef] [PubMed]
- Ni, Y.-N.; Luo, J.; Yu, H.; Wang, Y.-W.; Hu, Y.-H.; Liu, D.; Liang, B.-M.; Liang, Z.-A. Can body mass index predict clinical outcomes for patients with acute lung injury/acute respiratory distress syndrome? A meta-analysis. Crit. Care 2017, 21, 36. [Google Scholar] [CrossRef] [PubMed]
- Jose, R.J.; Manuel, A. Does Coronavirus Disease 2019 Disprove the Obesity Paradox in Acute Respiratory Distress Syndrome? Obesity 2020, 28, 1007. [Google Scholar] [CrossRef] [PubMed]
- Wold Health Organization. WHO expert consultation, Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004, 363, 157–163. [Google Scholar] [CrossRef]
- Rasouli, N.; Kern, P.A. Adipocytokines and the Metabolic Complications of Obesity. J. Clin. Endocrinol. Metab. 2008, 93, S64–S73. [Google Scholar] [CrossRef]
- Zhu, Z.; Hasegawa, K.; Ma, B.; Fujiogi, M.; Camargo, C.A.; Liang, L. Association of obesity and its genetic predisposition with the risk of severe COVID-19: Analysis of population-based cohort data. Metabolism 2020, 112, 154345. [Google Scholar] [CrossRef]
- Stefan, N.; Birkenfeld, A.L.; Schulze, M.B.; Ludwig, D.S. Obesity and impaired metabolic health in patients with COVID-19. Nat. Rev. Endocrinol. 2020, 16, 341–342. [Google Scholar] [CrossRef]
- Green, W.D.; Beck, M.A. Obesity Impairs the Adaptive Immune Response to Influenza Virus. Ann. Am. Thorac. Soc. 2017, 14, S406–S409. [Google Scholar] [CrossRef] [PubMed]
- Rychter, A.M.; Zawada, A.E.; Ratajczak, A.E.; Dobrowolska, A.; Krela-Kaźmierczak, I. Should patients with obesity be more afraid of COVID-19? Obes. Rev. 2020, 21, e13083. [Google Scholar] [CrossRef] [PubMed]
- Zhu, L.; She, Z.-G.; Cheng, X.; Qin, J.-J.; Zhang, X.-J.; Cai, J.; Lei, F.; Wang, H.; Xie, J.; Wang, W.; et al. Association of Blood Glucose Control and Outcomes in Patients with COVID-19 and Pre-existing Type 2 Diabetes. Cell Metab. 2020, 31, 1068–1077.e3. [Google Scholar] [CrossRef] [PubMed]
- Lecube, A.; Pachón, G.; Petriz, J.; Hernández, C.; Simó, R. Phagocytic Activity Is Impaired in Type 2 Diabetes Mellitus and Increases after Metabolic Improvement. PLoS ONE 2011, 6, e23366. [Google Scholar] [CrossRef]
- Sheetz, M.J. Molecular Understanding of Hyperglycemia’s Adverse Effects for Diabetic Complications. JAMA 2002, 288, 2579–2588. [Google Scholar] [CrossRef]
- Moser, J.S.; Galindo-Fraga, A.; Ortiz-Hernández, A.A.; Gu, W.; Hunsberger, S.; Galán-Herrera, J.; Guerrero, M.L.; Ruiz-Palacios, G.M.; Beigel, J.H. The La Red ILI 002 Study Group Underweight, overweight, and obesity as independent risk factors for hospitalization in adults and children from influenza and other respiratory viruses. Influ. Other Respir. Viruses 2019, 13, 3–9. [Google Scholar] [CrossRef]
- Okubo, Y.; Michihata, N.; Uda, K.; Morisaki, N.; Miyairi, I.; Matsui, H.; Fushimi, K.; Yasunaga, H. Dose-response relationship between weight status and clinical outcomes in pediatric influenza-related respiratory infections. Pediatr. Pulmonol. 2017, 53, 218–223. [Google Scholar] [CrossRef]
- Ma, H.-Y.; Wu, J.-L.; Lu, C.-Y.; Chen, J.-M.; Lee, P.-I.; Chang, L.-Y.; Huang, L.-M. Risk factors associated with severe influenza virus infections in hospitalized children during the 2013 to 2014 season. J. Microbiol. Immunol. Infect. 2016, 49, 387–393. [Google Scholar] [CrossRef][Green Version]
- Taylor, A.K.; Cao, W.; Vora, K.P.; De La Cruz, J.; Shieh, W.-J.; Zaki, S.R.; Katz, J.M.; Sambhara, S.; Gangappa, S. Protein Energy Malnutrition Decreases Immunity and Increases Susceptibility to Influenza Infection in Mice. J. Infect. Dis. 2013, 207, 501–510. [Google Scholar] [CrossRef]
- Kivimäki, M.; Shipley, M.J.; Bell, J.A.; Brunner, E.J.; Batty, G.D.; Singh-Manoux, A. Underweight as a risk factor for respiratory death in the Whitehall cohort study: Exploring reverse causality using a 45-year follow-up. Thorax 2015, 71, 84–85. [Google Scholar] [CrossRef]

| Characteristics | The Participants with COVID-19 ‡ | ||||
|---|---|---|---|---|---|
| Underweight | Normal | Overweight | Obese | p-Value | |
| Total participants (n, %) | 247 (100.0) | 1668 (100.0) | 953 (100.0) | 1159 (100.0) | |
| Age (years old) (n, %) | <0.001 * | ||||
| 0–9 | 39 (15.8) | 16 (0.9) | 0 (0.0) | 2 (0.2) | |
| 10–19 | 27 (10.9) | 86 (5.1) | 25 (2.6) | 37 (3.2) | |
| 20–29 | 62 (25.1) | 402 (23.7) | 151 (15.8) | 220 (19.0) | |
| 30–39 | 22 (8.9) | 170 (10.0) | 96 (10.1) | 148 (12.8) | |
| 40–49 | 11 (4.5) | 243 (14.3) | 116 (12.2) | 166 (14.3) | |
| 50–59 | 20 (8.1) | 313 (18.4) | 220 (23.1) | 248 (21.4) | |
| 60–69 | 16 (6.5) | 232 (13.7) | 194 (20.4) | 192 (16.6) | |
| 70–79 | 28 (11.3) | 136 (8.0) | 109 (11.4) | 101 (8.7) | |
| 80+ | 22 (8.9) | 100 (5.9) | 42 (4.4) | 45 (3.9) | |
| Sex (n, %) | <0.001 * | ||||
| Male | 84 (34.0) | 571 (33.6) | 455 (47.7) | 613 (52.9) | |
| Female | 163 (66.0) | 1127 (66.4) | 498 (52.3) | 546 (47.1) | |
| Systolic blood pressure (n, %) | <0.001 * | ||||
| <120 mmHg | 104 (42.1) | 541 (31.9) | 180 (18.9) | 171 (14.8) | |
| 120–129 mmHg | 59 (23.9) | 384 (22.6) | 213 (22.4) | 244 (21.1) | |
| 130–139 mmHg | 35 (14.2) | 322 (19.0) | 197 (20.7) | 257 (22.2) | |
| 140–159 mmHg | 32 (13.0) | 340 (20.0) | 264 (27.7) | 363 (31.3) | |
| ≥160 mmHg | 17 (6.9) | 111 (6.5) | 99 (10.4) | 124 (10.7) | |
| Diastolic blood pressure (n, %) | <0.001 * | ||||
| <80 mmHg | 128 (51.8) | 770 (45.4) | 316 (33.2) | 318 (27.4) | |
| 80–89 mmHg | 71 (28.7) | 576 (33.9) | 336 (35.3) | 423 (36.5) | |
| 90–99 mmHg | 32 (13.0) | 248 (14.6) | 203 (21.3) | 276 (23.8) | |
| ≥100 mmHg | 16 (6.5) | 104 (6.1) | 98 (10.3) | 142 (12.3) | |
| Heart rate (mean, SD) | 89.28 (17.80) | 84.11 (14.74) | 85.30 (14.69) | 86.41 (14.46) | <0.001 † |
| Temperature (mean, SD) | 36.92 (0.54) | 36.90 (0.54) | 36.91 (0.53) | 37.02 (0.58) | 0.486 |
| Past medical history | |||||
| Diabetes mellitus (n, %) | 18 (7.3) | 155 (9.1) | 135 (14.2) | 184 (15.9) | <0.001 * |
| Hypertension (n, %) | 28 (11.3) | 228 (13.4) | 237 (24.9) | 336 (29.0) | <0.001 * |
| Heart failure (n, %) | 6 (2.4) | 12 (0.7) | 8 (0.8) | 14 (1.2) | 0.060 |
| Chronic heart disease (n, %) | 7 (2.8) | 41 (2.4) | 40 (4.2) | 44 (3.8) | 0.052 |
| Asthma (n.%) | 5 (2.0) | 30 (1.8) | 31 (3.3) | 30 (2.6) | 0.100 |
| COPD (n, %) | 6 (2.4) | 14 (0.8) | 5 (0.5) | 5 (0.4) | 0.008* |
| Chronic kidney disease (n, %) | 3 (1.2) | 17 (1.0) | 8 (0.8) | 15 (1.3) | 0.763 |
| Cancer (n, %) | 7 (2.8) | 48 (2.8) | 26 (2.7) | 26 (2.2) | 0.800 |
| Chronic liver disease (n, %) | 3 (1.2) | 19 (1.1) | 15 (1.6) | 21 (1.8) | 0.460 |
| Rheumatic or autoimmune disease (n, %) | 1 (0.4) | 18 (1.1) | 8 (0.8) | 4 (0.4) | 0.162 |
| Dementia (n, %) | 20 (8.1) | 64 (3.7) | 20 (2.1) | 16 (1.4) | <0.001 * |
| Death (n, %) | 16 (6.5) | 46 (2.7) | 20 (2.1) | 44 (3.8) | 0.002 * |
| Maximum morbidity | <0.001 * | ||||
| Low morbidity | 213 (86.2) | 1507 (88.8) | 816 (85.6) | 952 (82.1) | |
| High morbidity | 34 (13.8) | 191 (11.3) | 137 (14.4) | 207 (17.9) | |
| Obesity (BMI, kg/m2) | HRs for Death | |||
|---|---|---|---|---|
| Crude | p-Value | Adjusted † | p-Value | |
| Underweight (<18.5) | 2.56 (1.45–4.52) | 0.001 * | 2.28 (1.23–4.25) | 0.009 * |
| Normal (≥18.5 to <23) | 1 | 1 | ||
| Overweight (≥23 to <25) | 0.79 (0.47–1.34) | 0.387 | 0.80 (0.46–1.39) | 0.432 |
| Obese (≥25) | 1.36 (0.90–2.05) | 0.149 | 1.71 (1.10–2.66) | 0.017 * |
| Obesity (BMI, kg/m2) | ORs for High Morbidity | |||
|---|---|---|---|---|
| Crude | p-Value | Adjusted † | p-Value | |
| Underweight (<18.5) | 1.26 (0.85–1.86) | 0.249 | 1.29 (0.79–2.12) | 0.312 |
| Normal (≥18.5 to <23) | 1 | 1 | ||
| Overweight (≥23 to <25) | 1.33 (1.05–1.68) | 0.019 * | 1.13 (0.86–1.49) | 0.369 |
| Obese (≥25) | 1.72 (1.39–2.12) | <0.001 * | 1.71 (1.32–2.21) | <0.001 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, S.Y.; Yoo, D.-M.; Min, C.; Wee, J.H.; Kim, J.-H.; Choi, H.G. Analysis of Mortality and Morbidity in COVID-19 Patients with Obesity Using Clinical Epidemiological Data from the Korean Center for Disease Control & Prevention. Int. J. Environ. Res. Public Health 2020, 17, 9336. https://doi.org/10.3390/ijerph17249336
Kim SY, Yoo D-M, Min C, Wee JH, Kim J-H, Choi HG. Analysis of Mortality and Morbidity in COVID-19 Patients with Obesity Using Clinical Epidemiological Data from the Korean Center for Disease Control & Prevention. International Journal of Environmental Research and Public Health. 2020; 17(24):9336. https://doi.org/10.3390/ijerph17249336
Chicago/Turabian StyleKim, So Young, Dae-Myoung Yoo, Chanyang Min, Jee Hye Wee, Joo-Hee Kim, and Hyo Geun Choi. 2020. "Analysis of Mortality and Morbidity in COVID-19 Patients with Obesity Using Clinical Epidemiological Data from the Korean Center for Disease Control & Prevention" International Journal of Environmental Research and Public Health 17, no. 24: 9336. https://doi.org/10.3390/ijerph17249336
APA StyleKim, S. Y., Yoo, D.-M., Min, C., Wee, J. H., Kim, J.-H., & Choi, H. G. (2020). Analysis of Mortality and Morbidity in COVID-19 Patients with Obesity Using Clinical Epidemiological Data from the Korean Center for Disease Control & Prevention. International Journal of Environmental Research and Public Health, 17(24), 9336. https://doi.org/10.3390/ijerph17249336






