Generic and Respiratory-Specific Quality of Life in Non-Hospitalized Patients with COVID-19
Abstract
:1. Introduction
2. Materials and Methods
2.1. Generic Quality of Life
2.2. Respiratory-Specific Quality of Life
2.3. Statistical Analysis
3. Results
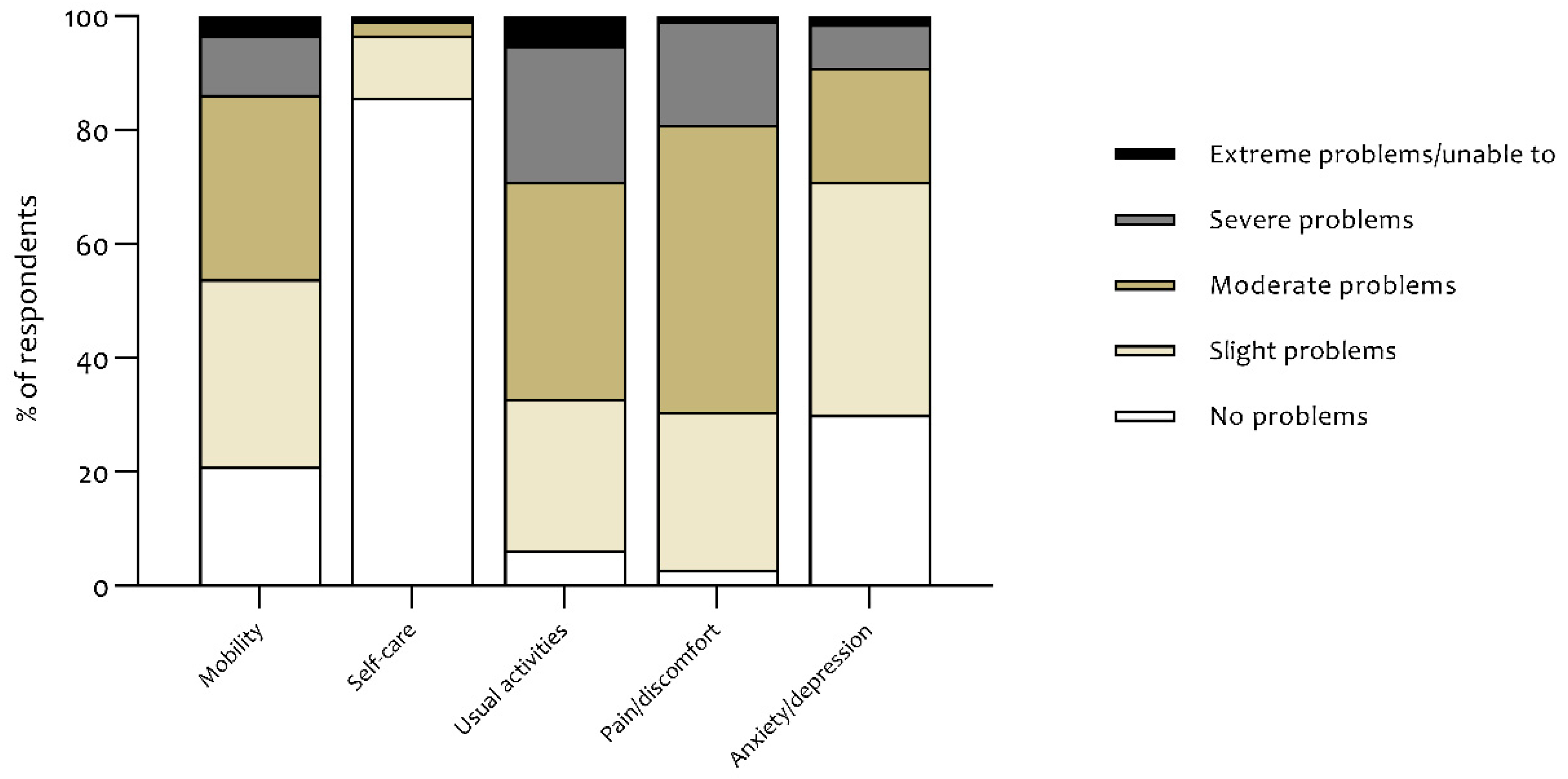
3.1. Generic Quality of Life Scores
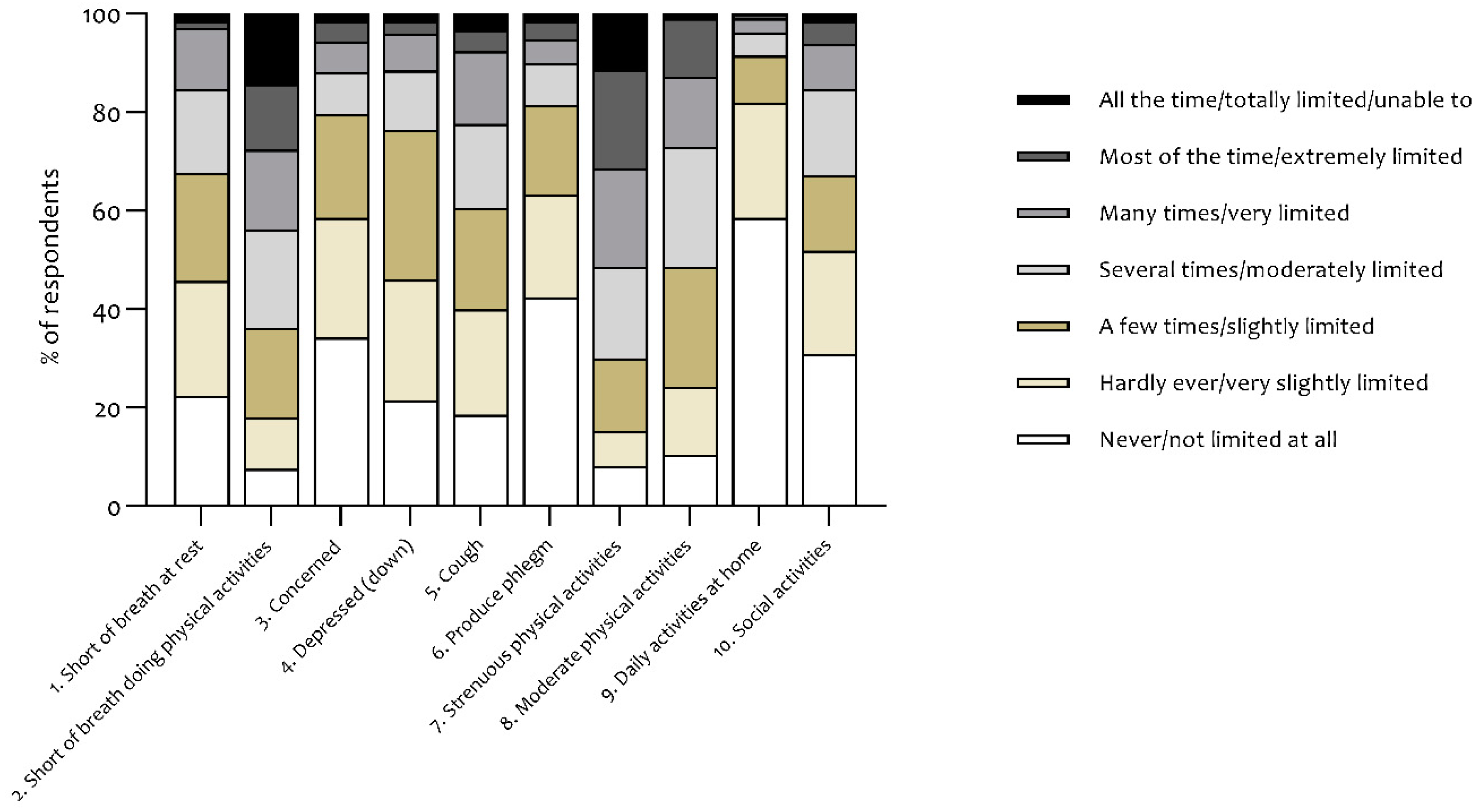
3.2. Respiratory-Specific Quality of Life Scores
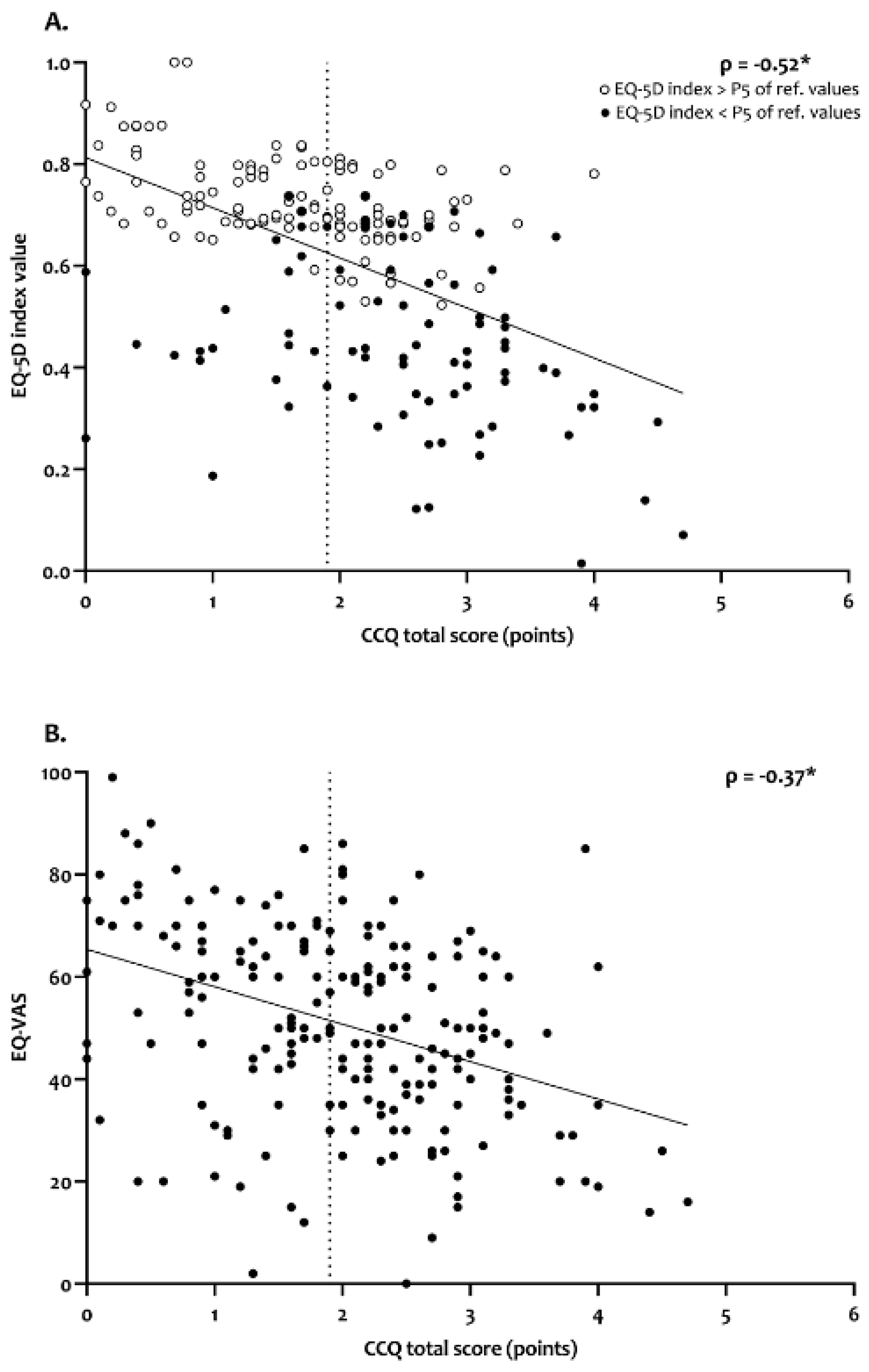
3.3. Associations between Generic and Respiratory-Specific Quality of Life
4. Discussion
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Stringhini, S.; Wisniak, A.; Piumatti, G.; Azman, A.S.; Lauer, S.A.; Baysson, H.; De Ridder, D.; Petrovic, D.; Schrempft, S.; Marcus, K.; et al. Seroprevalence of anti-SARS-CoV-2 IgG antibodies in Geneva, Switzerland (SEROCoV-POP): A population-based study. Lancet 2020, 396, 313–319. [Google Scholar] [CrossRef]
- Rodriguez-Morales, A.J.; Cardona-Ospina, J.A.; Gutiérrez-Ocampo, E.; Villamizar-Peña, R.; Holguin-Rivera, Y.; Escalera-Antezana, J.P.; Alvarado-Arnez, L.E.; Bonilla-Aldana, D.K.; Franco-Paredes, C.; Henao-Martinez, A.F.; et al. Clinical, laboratory and imaging features of COVID-19: A systematic review and meta-analysis. Travel Med. Infect. Dis. 2020, 34, 101623. [Google Scholar] [CrossRef]
- Goërtz, Y.M.J.; Van Herck, M.; Delbressine, J.M.; Vaes, A.W.; Meys, R.; Machado, F.V.C.; Houben-Wilke, S.; Burtin, C.; Posthuma, R.; Franssen, F.M.E.; et al. Persistent symptoms 3 months after a SARS-CoV-2 infection: The post-COVID-19 syndrome? ERJ Open Res. 2020, 6. [Google Scholar] [CrossRef]
- Vaes, A.W.; Machado, F.V.C.; Meys, R.; Delbressine, J.M.; Goertz, Y.M.J.; Van Herck, M.; Houben-Wilke, S.; Franssen, F.M.E.; Vijlbrief, H.; Spies, Y.; et al. Care Dependency in Non-Hospitalized Patients with COVID-19. J. Clin.Med. 2020, 9, 2964. [Google Scholar] [CrossRef]
- Van Hoek, A.J.; Underwood, A.; Jit, M.; Miller, E.; Edmunds, W.J. The impact of pandemic influenza H1N1 on health-related quality of life: A prospective population-based study. PLoS ONE 2011, 6, e17030. [Google Scholar] [CrossRef] [Green Version]
- Carfì, A.; Bernabei, R.; Landi, F.; Gemelli Against COVID-19 Post-Acute Care Study Group. Persistent Symptoms in Patients After Acute COVID-19. JAMA 2020, 324, 603–605. [Google Scholar] [CrossRef] [PubMed]
- Wong, A.W.; Shah, A.S.; Johnston, J.C.; Carlsten, C.; Ryerson, C.J. Patient-reported outcome measures after COVID-19: A prospective cohort study. Eur. Respir. J. 2020, 56, 2003276. [Google Scholar] [CrossRef] [PubMed]
- Frija-Masson, J.; Debray, M.-P.; Gilbert, M.; Lescure, F.-X.; Travert, F.; Borie, R.; Khalil, A.; Crestani, B.; d’Ortho, M.-P.; Bancal, C. Functional characteristics of patients with SARS-CoV-2 pneumonia at 30 days post infection. Eur. Respir. J. 2020, 56, 2001754. [Google Scholar] [CrossRef] [PubMed]
- Mo, X.; Jian, W.; Su, Z.; Chen, M.; Peng, H.; Peng, P.; Lei, C.; Chen, R.; Zhong, N.; Li, S. Abnormal pulmonary function in COVID-19 patients at time of hospital discharge. Eur. Respir. J. 2020, 55, 2001217. [Google Scholar] [CrossRef]
- Public Facebook Group: Corona Patiënten met Langdurige Klachten (Vlaanderen). 2020. Available online: https://www.facebook.com/groups/241043323639334/ (accessed on 4 June 2020).
- Herdman, M.; Gudex, C.; Lloyd, A.; Janssen, M.; Kind, P.; Parkin, D.E.; Bonsel, G.J.; Badia, X. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual. Life Res. 2011, 20, 1727–1736. [Google Scholar] [CrossRef] [Green Version]
- Versteegh, M.M.; Vermeulen, K.M.; Evers, S.M.A.A.; De Wit, G.A.; Prenger, H.C.; Stolk, E.A. Dutch Tariff for the Five-Level Version of EQ-5D. Value Health 2016, 19, 343–352. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grochtdreis, T.; Dams, J.; König, H.-H.; Konnopka, A. Health-related quality of life measured with the EQ-5D-5L: Estimation of normative index values based on a representative German population sample and value set. Eur. J. Health Econ. 2019, 20, 933–944. [Google Scholar] [CrossRef] [PubMed]
- Van Der Molen, T.; Willemse, B.; Schokker, S.; Hacken, N.H.T.; Postma, D.S.; Juniper, E.F. Development, validity and responsiveness of the Clinical COPD Questionnaire. Health Qual. Life Outcomes 2003, 1, 13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smid, D.E.; Franssen, F.M.E.; Gonik, M.; Miravitlles, M.; Casanova, C.; Cosio, B.G.; De Lucas-Ramos, P.; Marin, J.M.; Martinez, C.; Vladimir, K.; et al. Redefining Cut-Points for High Symptom Burden of the Global Initiative for Chronic Obstructive Lung Disease Classification in 18,577 Patients with Chronic Obstructive Pulmonary Disease. J. Am. Med Dir. Assoc. 2017, 18, 1097.e11–1097.e24. [Google Scholar] [CrossRef] [Green Version]
- BMJ. Correlation and Regression. Available online: https://www.bmj.com/about-bmj/resources-readers/publications/statistics-square-one/11-correlation-and-regression (accessed on 20 June 2020).
- Nolan, C.M.; Longworth, L.; Lord, J.; Canavan, J.L.; Jones, S.E.; Kon, S.S.C.; Man, W.D.-C. The EQ-5D-5L health status questionnaire in COPD: Validity, responsiveness and minimum important difference. Thorax 2016, 71, 493–500. [Google Scholar] [CrossRef] [Green Version]
- Houben-Wilke, S.; Janssen, D.J.A.; Wouters, E.F.; Schols, J.M.G.A.; Franssen, F.M.; Spruit, M.A. Correlations between disease-specific and generic health status questionnaires in patients with advanced COPD: A one-year observational study. Health Qual. Life Outcomes 2012, 10, 98. [Google Scholar] [CrossRef] [Green Version]
- Hernandez, G.; Garin, O.; Dima, A.L.; Pont, A.; Martí-Pastor, M.; Alonso, J.; Van Ganse, E.; Laforest, L.; De Bruin, M.; Mayoral, K.; et al. EuroQol (EQ-5D-5L) Validity in Assessing the Quality of Life in Adults with Asthma: Cross-Sectional Study. J. Med. Internet Res. 2019, 21, e10178. [Google Scholar] [CrossRef]
- Szentes, B.; Schultz, K.; Nowak, D.; Schuler, M.; Schwarzkopf, L. How does the EQ-5D-5L perform in asthma patients compared with an asthma-specific quality of life questionnaire? BMC Pulm. Med. 2020, 20, 168. [Google Scholar] [CrossRef]
- Chen, J.; Wu, J.; Hao, S.; Yang, M.; Lu, X.; Chen, X.; Li, L. Long term outcomes in survivors of epidemic Influenza A (H7N9) virus infection. Sci. Rep. 2017, 7, 17275. [Google Scholar] [CrossRef]
- Boland, M.R.S.; Van Boven, J.F.M.; Kocks, J.W.; Van Der Molen, T.; Goossens, L.M.; Chavannes, N.H.; Mölken, M.P.R.-V. Mapping the Clinical Chronic Obstructive Pulmonary Disease Questionnaire onto Generic Preference-Based EQ-5D Values. Value Health 2015, 18, 299–307. [Google Scholar] [CrossRef] [Green Version]
- Greenhalgh, T.; Knight, M.; A’Court, C.; Buxton, M.; Husain, L. Management of post-acute covid-19 in primary care. BMJ 2020, 370, m3026. [Google Scholar] [CrossRef] [PubMed]
- WHO. COVID-19 Weekly Surveillance Report: Data for the Week of 8–14 June 2020 (Epi Week 24). 2020. Available online: https://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/weekly-surveillance-report (accessed on 24 June 2020).
- Tsiligianni, I.G.; Van Der Molen, T.; Moraitaki, D.; Lopez, I.; Kocks, J.W.H.; Karagiannis, K.; Siafakas, N.; Tzanakis, N. Assessing health status in COPD. A head-to-head comparison between the COPD assessment test (CAT) and the clinical COPD questionnaire (CCQ). BMC Pulm. Med. 2012, 12, 20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| All Subjects (n = 210) | Confirmed COVID-19 (n = 49) | Symptom-Based COVID-19 (n = 105) | Suspected COVID-19 (n = 56) | |
|---|---|---|---|---|
| Female, n (%) | 184 (87.6) | 45 (91.8) | 93 (88.6) | 46 (82.1) |
| Age (years) | 45 ± 11 | 43 ± 10 | 45 ± 10 | 46 ± 12 |
| 18–39 years, n (%) | 71 (33.8) | 22 (44.9) | 34 (32.4) | 15 (26.8) |
| 40–59 years, n (%) | 116 (55.2) | 24 (49.0) | 60 (57.1) | 32 (57.1) |
| 60 + years, n (%) | 23 (11.0) | 3 (6.1) | 11 (10.5) | 9 (16.1) |
| Body Mass Index (kg/m2) | 25.6 ± 4.3 | 26.3 ± 3.8 | 25.5 ± 4.5 | 25.0 ± 4.1 |
| Pre-existing comorbidities | ||||
| None, n (%) | 129 (61.4) | 33 (67.3) | 60 (57.1) | 36 (64.3) |
| One, n (%) | 49 (23.3) | 6 (12.2) | 31 (29.5) | 12 (21.4) |
| Two or more, n (%) | 32 (15.2) | 10 (20.4) | 14 (13.4) | 8 (14.3) |
| Symptoms | ||||
| Time since first symptoms (days) | 79 ± 17 | 74 ± 19 | 78 ± 15 | 84 ± 19 * |
| Symptoms during the infection, n (%) | 14 (11–17) | 14 (11–17) | 14 (11–18) | 14 (9–16) |
| Symptoms at this moment (after mean of 79 days), n (%) | 6 (4–9) | 6 (4–8) | 7 (5–10) | 6 (4–9) |
| Marital Status | ||||
| Alone, n (%) | 43 (20.5) | 11 (22.4) | 19 (18.1) | 13 (23.2) |
| Married/Living together, n (%) | 147 (70.0) | 34 (69.4) | 77 (73.3) | 36 (64.3) |
| Divorced, n (%) | 18 (8.6) | 4 (8.2) | 8 (7.6) | 6 (10.7) |
| Widow(er), n (%) | 2 (1.0) | 0 (o) | 1 (1.0) | 1 (1.8) |
| Level of Education | ||||
| Low, n (%) | 15 (7.1) | 1 (2.0) | 6 (5.7) | 8 (14.3) |
| Medium, n (%) | 61 (29.0) | 14 (28.6) | 33 (31.4) | 14 (25.0) |
| High, n (%) | 133 (63.3) | 33 (67.3) | 66 (62.9) | 34 (60.7) |
| Not specified, n (%) | 1 (0.5) | 1 (2.0) | 0 (0) | 0 (0) |
| Smoking Status | ||||
| Current smoker, n (%) | 16 (7.6) | 4 (8.2) | 10 (9.5) | 7 (12.5) |
| Stopped smoking after COVID-19, n (%) | 39 (18.6) | 14 (28.6) | 31 (29.5) | 11 (19.6) |
| Never smoker, n (%) | 155 (73.8) | 31 (63.3) | 64 (61.0) | 38 (67.9) |
| Variables | All Subjects (n = 210) | Confirmed COVID-19 (n = 49) | Symptom-Based COVID-19 (n = 105) | Suspected COVID-19 (n = 56) |
|---|---|---|---|---|
| Five-level EQ-5D (EQ-5D-5L) | ||||
| EQ-5D index-score (range: −0.329–1) | 0.62 ± 0.19 | 0.63 ± 0.20 | 0.61 ± 0.17 | 0.61 ± 0.20 |
| Index-score <P5 of reference values, n (%) [13] | 84 (40.0) | 17 (34.7) | 44 (41.9) | 23 (41.1) |
| EQ-5D dimension scores (range: 1–5 *) | ||||
| Mobility | 2.42 ± 1.04 | 2.39 ± 1.02 | 2.56 ± 1.02 | 2.20 ± 1.07 |
| Self-care | 1.19 ± 0.54 | 1.16 ± 0.51 | 1.24 ± 0.61 | 1.13 ± 0.38 |
| Usual activities | 2.95 ± 0.98 | 2.96 ± 1.00 | 3.09 ± 0.92 | 2.70 ± 1.04 |
| Pain/Discomfort | 2.87 ± 0.77 | 2.84 ± 0.80 | 2.90 ± 0.75 | 2.84 ± 0.80 |
| Anxiety/Depression | 2.10 ± 0.96 | 1.96 ± 0.87 | 2.05 ± 0.96 | 2.30 ± 1.03 |
| EQ-VAS score (range: 0–100) | 50.71 ± 18.87 | 51.27 ± 17.86 | 50.26 ± 20.06 | 51.09 ± 17.71 |
| Clinical COPD Questionnaire (CCQ) | ||||
| CCQ total score (range: 0–6) | 2.01 ± 0.98 | 2.00 ± 0.96 | 2.05 ± 0.95 | 1.93 ± 1.05 |
| CCQ total score ≥1.9, n (%) [15] | 123 (58.6) | 29 (59.2) | 67 (63.8) | 27 (48.2) |
| CCQ domain scores (range: 0–6) | ||||
| Symptoms (items 1, 2, 5, 6) | 2.13 ± 1.12 | 2.14 ± 1.09 | 2.18 ± 1.08 | 2.02 ± 1.23 |
| Functional state (items 7, 8, 9, 10) | 2.12 ± 1.22 | 2.10 ± 1.34 | 2.23 ± 1.20 | 1.90 ± 1.14 |
| Mental state (items 3, 4) | 1.56 ± 1.31 | 1.50 ± 1.13 | 1.45 ± 1.30 | 1.81 ± 1.47 |
| CCQ item scores (range: 0–6) | ||||
| CCQ-1 Shortness of breath at rest | 1.84 ± 1.46 | 1.84 ± 1.49 | 1.81 ± 1.43 | 1.89 ± 1.52 |
| CCQ-2 Shortness of breath doing physical activities | 3.24 ± 1.80 | 3.37 ± 1.89 | 3.26 ± 1.77 | 3.09 ± 1.78 |
| CCQ-3 Concerned about getting a cold or your breathing getting worse | 1.47 ± 1.51 | 1.39 ± 1.26 | 1.31 ± 1.44 | 1.82 ± 1.79 |
| CCQ-4 Depressed (down) because of your breathing problems | 1.65 ± 1.40 | 1.61 ± 1.32 | 1.58 ± 1.40 | 1.80 ± 1.49 |
| CCQ-5 Cough | 2.14 ± 1.62 | 2.12 ± 1.58 | 2.23 ± 1.60 | 2.00 ± 1.72 |
| CCQ-6 Produce phlegm | 1.30 ± 1.51 | 1.22 ± 1.54 | 1.43 ± 1.55 | 1.11 ± 1.38 |
| CCQ-7 Strenuous physical activities | 3.41 ± 1.74 | 3.57 ± 1.63 | 3.53 ± 1.86 | 3.04 ± 1.58 |
| CCQ-8 Moderate physical activities | 2.58 ± 1.51 | 2.63 ± 1.54 | 2.74 ± 1.49 | 2.21 ± 1.47 |
| CCQ-9 Daily activities at home | 0.73 ± 1.10 | 0.65 ± 1.27 | 0.74 ± 1.02 | 0.77 ± 1.11 |
| CCQ-10 Social activities | 1.73 ± 1.61 | 1.55 ± 1.76 | 1.89 ± 1.61 | 1.59 ± 1.46 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Meys, R.; Delbressine, J.M.; Goërtz, Y.M.J.; Vaes, A.W.; Machado, F.V.C.; Van Herck, M.; Burtin, C.; Posthuma, R.; Spaetgens, B.; Franssen, F.M.E.; et al. Generic and Respiratory-Specific Quality of Life in Non-Hospitalized Patients with COVID-19. J. Clin. Med. 2020, 9, 3993. https://doi.org/10.3390/jcm9123993
Meys R, Delbressine JM, Goërtz YMJ, Vaes AW, Machado FVC, Van Herck M, Burtin C, Posthuma R, Spaetgens B, Franssen FME, et al. Generic and Respiratory-Specific Quality of Life in Non-Hospitalized Patients with COVID-19. Journal of Clinical Medicine. 2020; 9(12):3993. https://doi.org/10.3390/jcm9123993
Chicago/Turabian StyleMeys, Roy, Jeannet M. Delbressine, Yvonne M.J. Goërtz, Anouk W. Vaes, Felipe V.C. Machado, Maarten Van Herck, Chris Burtin, Rein Posthuma, Bart Spaetgens, Frits M.E. Franssen, and et al. 2020. "Generic and Respiratory-Specific Quality of Life in Non-Hospitalized Patients with COVID-19" Journal of Clinical Medicine 9, no. 12: 3993. https://doi.org/10.3390/jcm9123993
APA StyleMeys, R., Delbressine, J. M., Goërtz, Y. M. J., Vaes, A. W., Machado, F. V. C., Van Herck, M., Burtin, C., Posthuma, R., Spaetgens, B., Franssen, F. M. E., Spies, Y., Vijlbrief, H., van’t Hul, A. J., Janssen, D. J. A., Spruit, M. A., & Houben-Wilke, S. (2020). Generic and Respiratory-Specific Quality of Life in Non-Hospitalized Patients with COVID-19. Journal of Clinical Medicine, 9(12), 3993. https://doi.org/10.3390/jcm9123993





