Anatomographic Variants of Sphenoid Sinus in Ethiopian Population
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Jaworek-Troć, J.; Zarzecki, M.; Zamojska, I.; IIwanaga, J.; Przybycień, W.; Mazur, M.; Chrzan, R.; Walocha, J.A. The dimensions of the sphenoid sinuses—Evaluation before the functional endoscopic sinus surgery. Folia Morphol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Anusha, B.; Baharudin, A.; Philip, R.; Harvinder, S.; Shaffie, B.M. Anatomical variations of the sphenoid sinus and its adjacent structures: A review of existing literature. Surg. Radiol. Anat. 2014, 36, 419–427. [Google Scholar] [CrossRef] [PubMed]
- Ozturan, O.; Yenigun, A.; Degirmenci, N.; Aksoy, F.; Veyseller, B. Co-existence of the Onodi cell with the variation of perisphenoidal structures. Eur. Arch. Otorhinolaryngol. 2013, 270, 2057–2063. [Google Scholar] [CrossRef] [PubMed]
- Fasunla, A.J.; Ameye, S.A.; Adebola, O.S.; Ogbole, G.; Adeleye, A.O.; Adekanmi, A.J. Anatomical variations of the sphenoid sinus and nearby neurovascular structures seen on computed tomography of black Africans. East Cent. Afr. J. Surg. 2012, 17, 57–64. [Google Scholar] [CrossRef]
- Awadalla, A.M.; Hussein, Y.; ELKammash, T.H. Anatomical and radiological parameters of the sphenoid sinus among Egyptians and its impact on sellar region surgery. Egypt. J. Neurosurg. 2015, 30, 1–12. [Google Scholar]
- Štoković, N.; Trkulja, V.; Dumić-Čule, I.; Čuković-Bagić, I.; Lauc, T.; Vukičević, S.; Grgurević, L. Sphenoid sinus types, dimensions and relationship with surrounding structures. Ann. Anat. 2016, 203, 69–76. [Google Scholar] [CrossRef]
- Sevinc, O.; Is, M.; Barut, C.; Erdogan, A. Anatomic Variations of Sphenoid Sinus Pneumatization in a Sample of Turkish Population: MRI Study. Int. J. Morphol. 2014, 32, 1140–1143. [Google Scholar] [CrossRef] [Green Version]
- Budu, V.; Mogoantă, C.A.; Fănuţă, B.; Bulescu, I. The anatomical relations of the sphenoid sinus and their implications in sphenoid endoscopic surgery. Rom. J. Morphol. Embryol. 2013, 54, 13–16. [Google Scholar]
- Seddighi, A.; Seddighi, A.S.; Mellati, O.; Ghorbani, J.; Raad, N.; Soleimani, M.M. Sphenoid Sinus: Anatomic Variations and Their Importance in Trans-sphenoid Surgery. Int. Clin. Neurosci. J. 2014, 1, 31–34. [Google Scholar]
- Craiu, C.; Sandulescu, M.; Rusu, M.C. Variations of sphenoid pneumatization: A CBCT study. Rom. J. Rhinol. 2015, 5, 107–113. [Google Scholar] [CrossRef] [Green Version]
- Pérez-Piñas, I.; Sabaté, J.; Carmona, A.; Catalina-Herrera, C.J.; Jiménez-Castellanos, J. Anatomical variations in the human paranasal sinus region studied by CT. J. Anat. 2000, 197, 221–227. [Google Scholar] [CrossRef] [PubMed]
- Kayalioglu, G.; Erturk, M.; Varol, T. Variations in sphenoid sinus anatomy with special emphasis on pneumatization and endoscopic anatomic distances. Neurosciences (Riyadh) 2005, 10, 79–84. [Google Scholar] [PubMed]
- Chougule, M.S.; Dixit, D. A Cross-Sectional Study of Sphenoid Sinus through Gross and Endoscopic Dissection in North Karnataka, India. J. Clin. Diagn. Res. 2014, 8, AC01–AC5. [Google Scholar] [CrossRef] [PubMed]
- Kantarci, M.; Karasen, R.M.; Alper, F.; Onbas, O.; Okur, A.; Karaman, A. Remarkable anatomic variations in paranasal sinus region and their clinical importance. Eur. J. Radiol. 2004, 50, 296–302. [Google Scholar] [CrossRef]
- Raudaschl, P.F.; Zaffino, P.; Sharp, G.C.; Spadea, M.F.; Chen, A.; Dawant, B.M.; Albrecht, T.; Gass, T.; Langguth, C.; Lüthi, M.; et al. Evaluation of segmentation methods on head and neck CT: Auto-segmentation challenge 2015. Med. Phys. 2017, 44, 2020–2036. [Google Scholar] [CrossRef]
- Lokwani, M.S.; Patidar, J.; Parihar, V. Anatomical variations of sphenoid sinus on multi-detector computed tomography and its usefulness in trans-sphenoidal endoscopic skull base surgery. Int. J. Res. Med. Sci. 2018, 6, 3063–3071. [Google Scholar] [CrossRef]
- Kajoak, S.A.; Ayad, C.E.; Najmeldeen, M.; Abdalla, E.A. Computerized tomography morphometric analysis of the sphenoid sinus and related structures in Sudanese population. Glob. Adv. Res. J. Med. Med. Sci. 2014, 3, 160–167. [Google Scholar]
- Hewaidi, G.; Omami, G. Anatomic Variation of Sphenoid Sinus and Related Structures in Libyan Population: CT Scan Study. Libyan J. Med. 2008, 3, 128–133. [Google Scholar] [CrossRef]
- Tomovic, S.; Esmaeili, A.; Chan, N.J.; Shukla, P.A.; Choudhry, O.J.; Liu, J.K.; Eloy, J.A. High-resolution computed tomography analysis of variations of the sphenoid sinus. J. Neurol. Surg. Part. B Skull Base 2013, 74, 82–90. [Google Scholar] [CrossRef] [Green Version]
- Hamid, O.; El Fiky, L.; Hassan, O.; Kotb, A.; El Fiky, S. Anatomic Variations of the Sphenoid Sinus and Their Impact on Trans-sphenoid Pituitary Surgery. Skull Base 2008, 18, 9–15. [Google Scholar] [CrossRef] [Green Version]
- Shpilberg, K.A.; Daniel, S.C.; Doshi, A.H.; Lawson, W.; Som, P.M. CT of Anatomic Variants of the Paranasal Sinuses and Nasal Cavity: Poor Correlation with Radiologically Significant Rhinosinusitis but Importance in Surgical Planning. AJR Am. J. Roentgenol. 2015, 204, 1255–1260. [Google Scholar] [CrossRef]
- Heskova, G.; Mellova, Y.; Holomanova, A.; Vybohova, D.; Kunertova, L.; Marcekova, M.; Mello, M. Assessment of the relation of the optic nerve to the posterior ethmoid and sphenoid sinuses by computed tomography. Biomed. Pap. Med. Fac. Univ. Palacky Olomouc. Czech. Repub. 2009, 153, 149–152. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jaworek-Troć, J.; Zarzecki, M.; Bonczar, A.; Kaythampillai, L.N.; Rutowicz, B.; Mazur, M.; Urbaniak, J.; Przybycień, W.; Piątek-Koziej, K.; Kuniewicz, M.; et al. Sphenoid bone and its sinus-anatomo-clinical review of the literature including application to FESS. Folia Med. Cracov. 2019, 59, 45–59. [Google Scholar] [PubMed]
- Raseman, J.; Guryildirim, M.; Beer-Furlan, A.; Jhaveri, M.; Tajudeen, B.A.; Byrne, R.W.; Batra, P.S. Preoperative Computed Tomography Imaging of the Sphenoid Sinus: Striving Towards Safe Transsphenoidal Surgery. J. Neurol. Surg. B Skull Base 2020, 81, 251–262. [Google Scholar] [CrossRef] [PubMed]
- Lupascu, M.; Comsa, G.I.; Zainea, V. Anatomical variations of the sphenoid sinus-a study of 200 cases. ARS Medica Tomitana 2014, 20, 57–62. [Google Scholar] [CrossRef] [Green Version]
- Rysz, M.; Bakoń, L. Maxillary sinus anatomy variation and nasal cavity width: Structural computed tomography imaging. Folia Morphol. (Warsz) 2009, 68, 260–264. [Google Scholar] [PubMed]
- Hiremath, S.B.; Gautam, A.A.; Sheeja, K.; Benjamin, G. Assessment of variations in sphenoid sinus pneumatization in Indian population: A multidetector computed tomography study. Indian J. Radiol. Imaging 2018, 28, 273–279. [Google Scholar] [CrossRef]
- Ngubane, N.P.; Lazarus, L.; Rennie, C.O.; Satyapal, K.S. The Septation of the Sphenoidal Air Sinus. A Cadaveric Study. Int. J. Morphol. 2018, 36, 1413–1422. [Google Scholar] [CrossRef] [Green Version]
- Jaworek-Troć, J.; Zarzecki, M.; Mróz, I.; Troć, P.; Chrzan, R.; Zawiliński, J.; Walocha, J.; Urbanik, A. The total number of septa and antra in the sphenoid sinuses-evaluation before the FESS. Folia Med. Cracov. 2018, 58, 67–81. [Google Scholar] [CrossRef]
- Guga Priya, T.S.; Kumar, N.V.; Guru, A.T.; NalinaKumari, S.D. An Anatomo-Imagistic Study of Intersphenoidal Sinus Septum. Int. J. Anat. Res. 2016, 4, 2015–2020. [Google Scholar] [CrossRef]
- Akanni, D.; Souza, C.; Savi de Tove, K.M.; N’zi, K.; Yèkpè, P.; Biaou, O.; Boco, V. Sphenoid Sinuses Pneumatization and Association with the Protrusion of Surrounding Neurovascular Structures amongst Beninese. Open J. Radiol. 2018, 8, 209–216. [Google Scholar] [CrossRef] [Green Version]
- Riza, D.; Erkan, K.; Fatih, S.; Mehmet, A.; Ahmet, K.; Engin, S.; Haflmet, Y.; Abdülkadir, E. Radiological evaluation of septal bone variations in the sphenoid sinus. J. Med. Updates 2014, 4, 6–10. [Google Scholar] [CrossRef] [Green Version]
- Hengerer, A.S. Surgical anatomy of the paranasal sinuses. Ear Nose Throat J. 1984, 63, 137–143. [Google Scholar]
- Bedawi, K.; Madani, G.A.; Seddeg, Y. The Radiological Study of Onodi Cells Among Adult Sudanese Subjects. OSR-JDMS 2017, 16, 106–109. [Google Scholar] [CrossRef]

| Age in Years | Minimum | Mean | Maximum |
|---|---|---|---|
| Male | 18 | 51 | 79 |
| Female | 18 | 37 | 74 |
| Both | 18 | 43 | 79 |
| Anatomographic Variants of the Sphenoid Sinus | |||||
|---|---|---|---|---|---|
| Pneumatization | Septation | ||||
| Type | Frequency | Type | Midline | Right Side | Left Side |
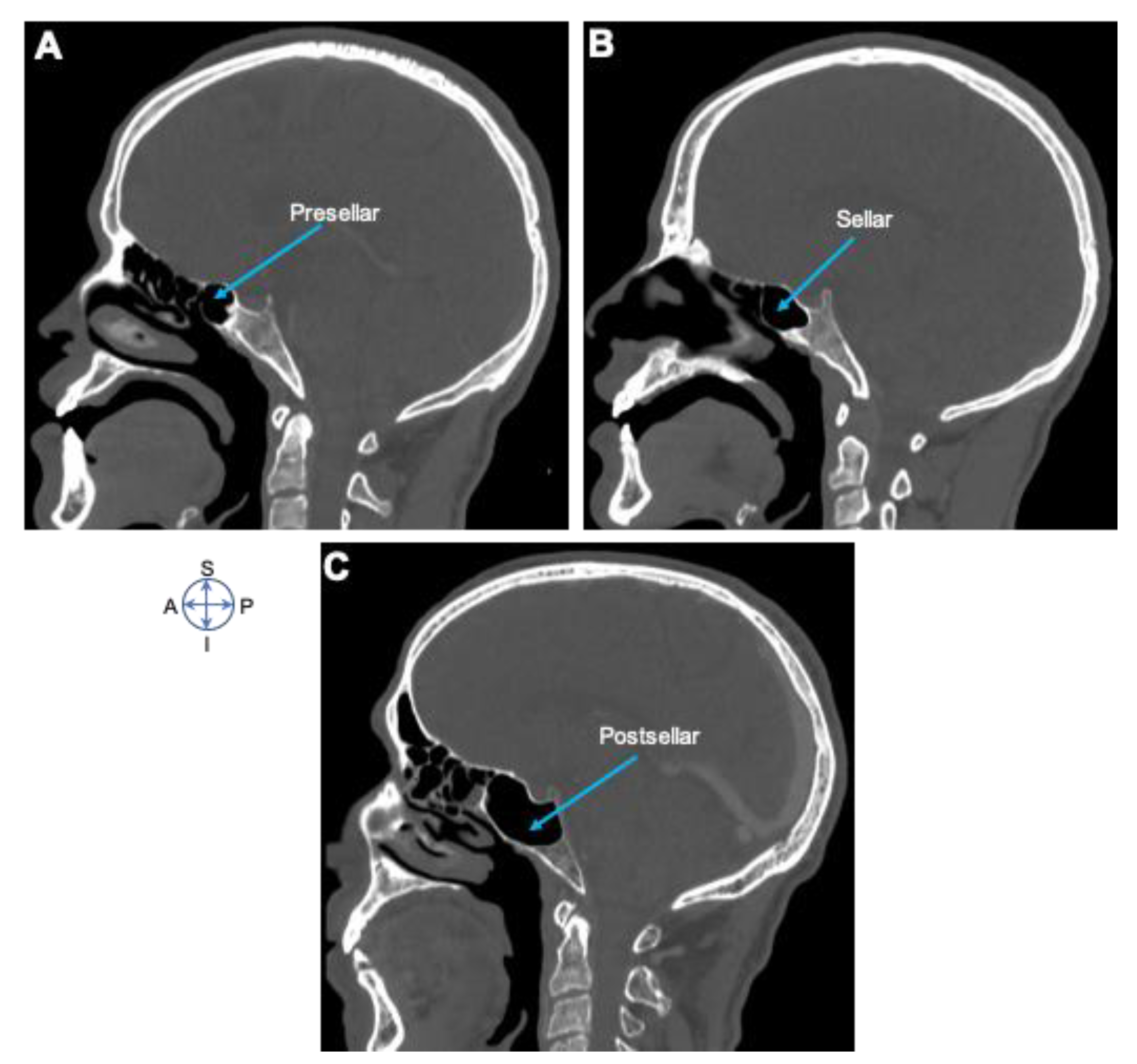
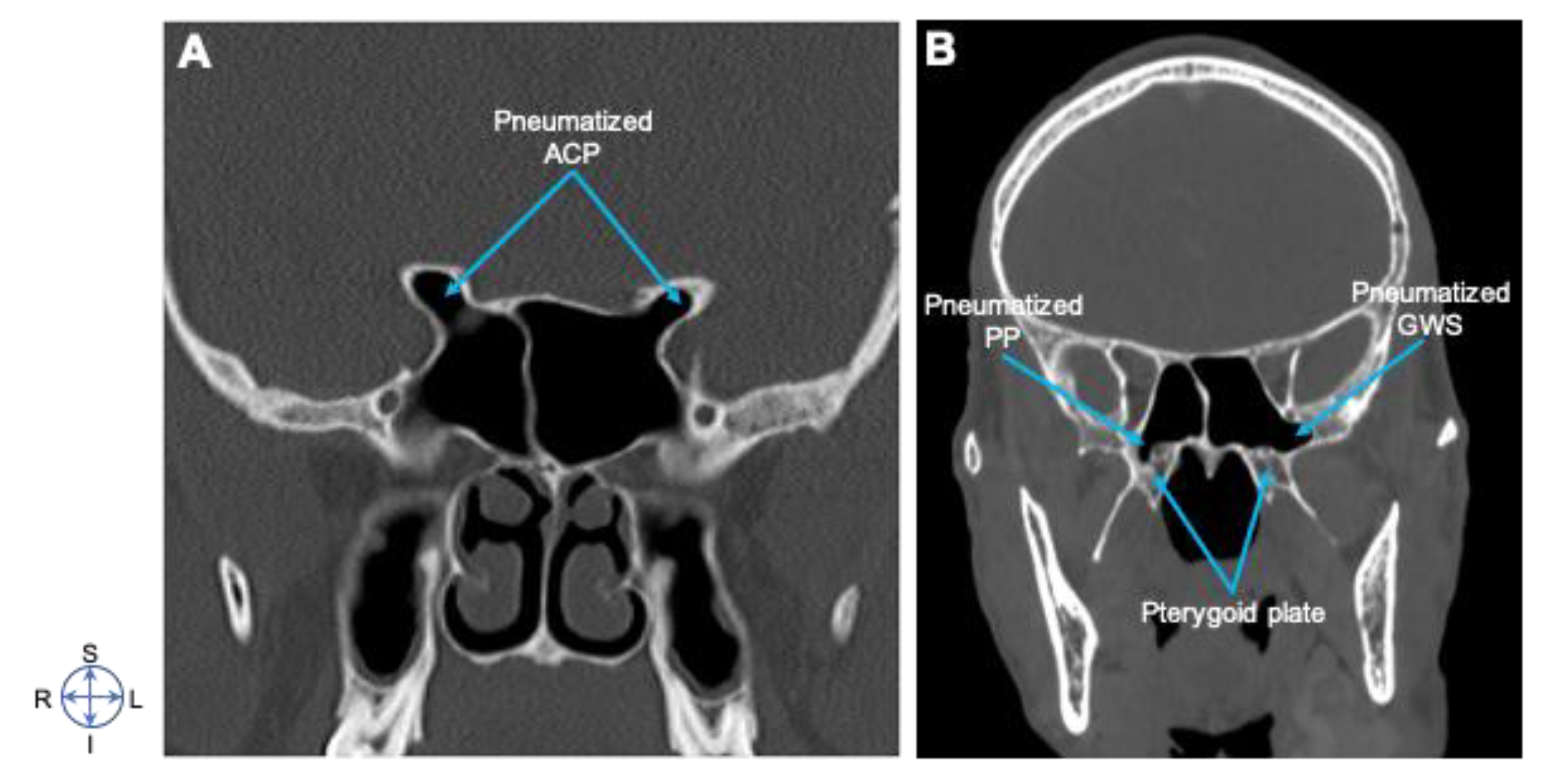
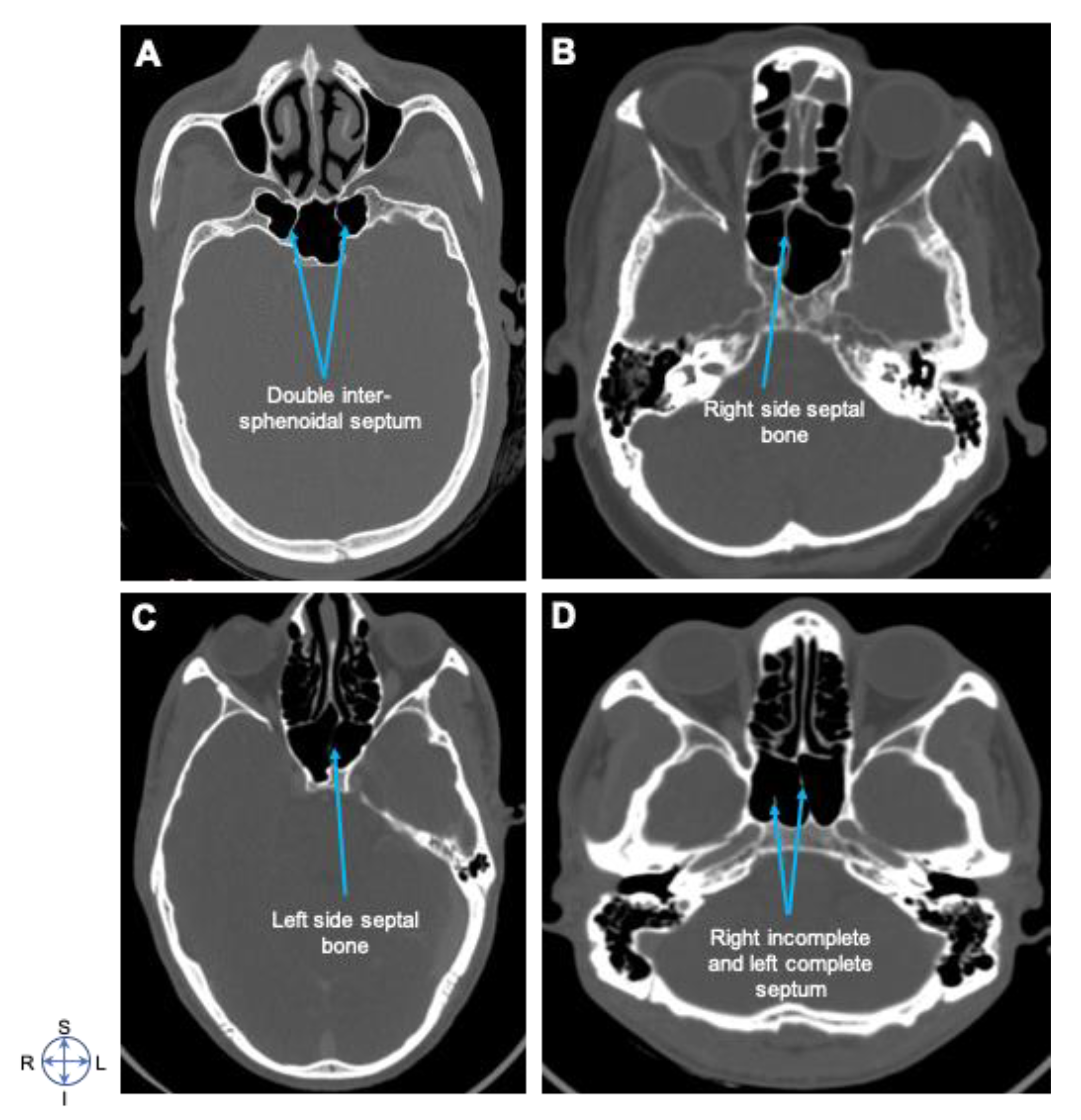
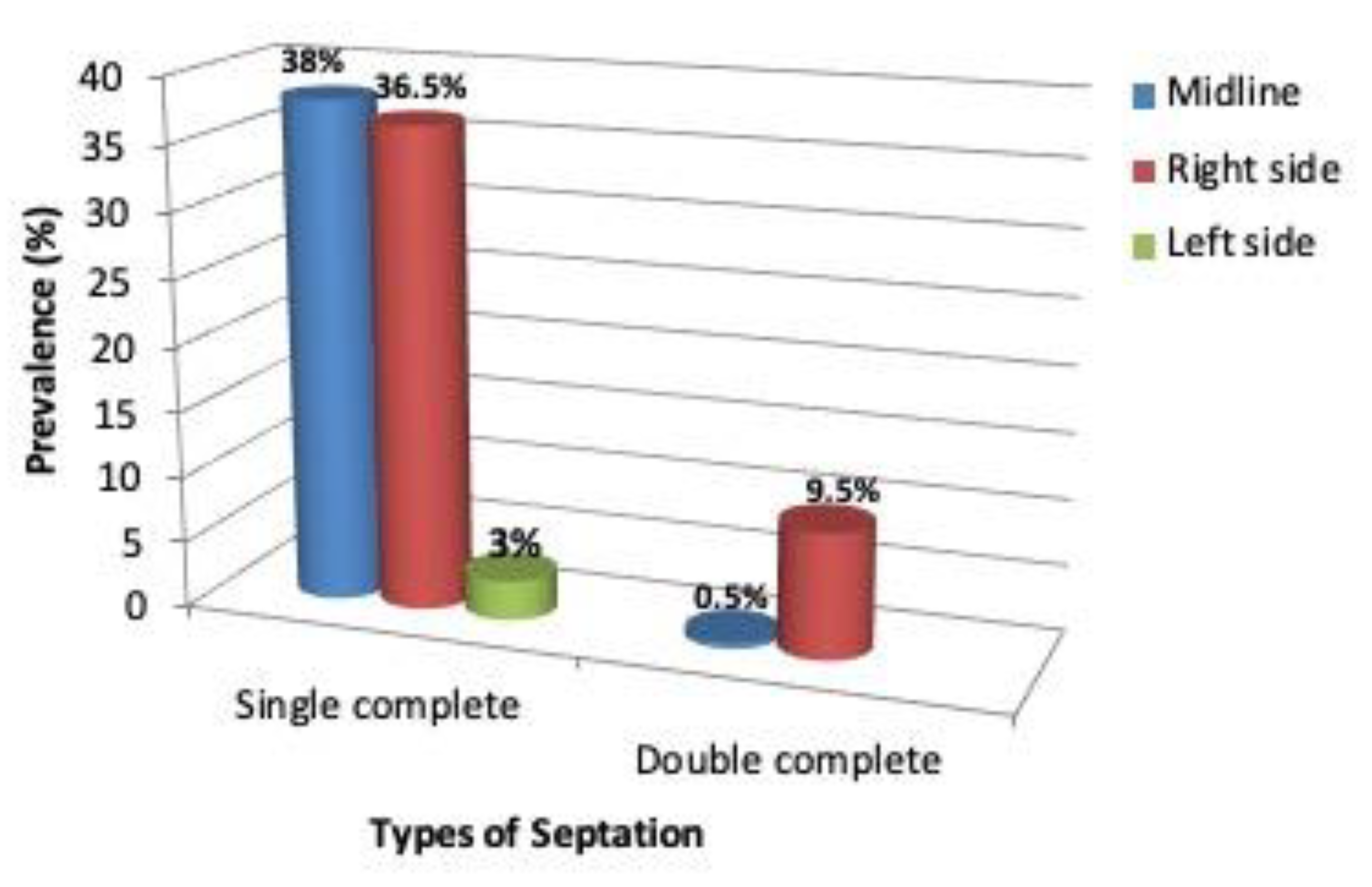
| Conchal | 4 (2%) | Single complete | 76 (38%) | 73 (36.5%) | 6 (3%) |
| Presellar | 51 (25.5%) | Double complete | 1 (0.5%) | 19 (9.5%) | 0 (0%) |
| Sellar | 100 (50%) | No septa | 2(1%) | 0 (0%) | 0 (0%) |
| Postsellar | 45 (22.5%) | ||||
| Sides | |||||
|---|---|---|---|---|---|
| Structure | Right Side | Left Side | Bilateral | Total | |
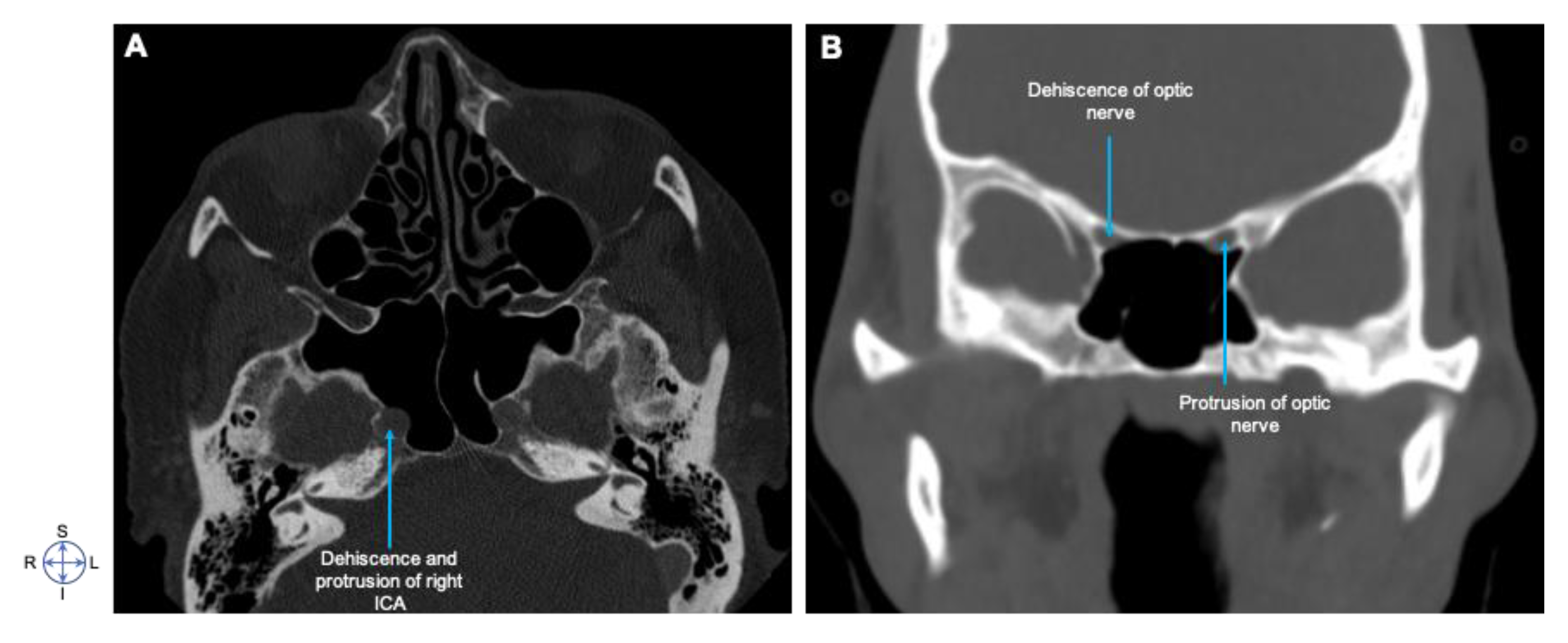
| ICA * | Protrusion | 12 (32.4%) | 9 (24.3%) | 16 (43.2%) | 37 (18.5%) |
| Dehiscence | 7 (29.17%) | 10 (41.7%) | 7 (29.17%) | 24 (12%) | |
| OPN * | Protrusion | 1 (5.26%) | 10 (52.63%) | 8 (42.1%) | 19 (9.5%) |
| Dehiscence | 12 (38.7%) | 9 (29%) | 10 (32.25%) | 31 (15.5%) | |
| V2 * | Protrusion | 7 (28%) | 8 (32%) | 10 (40%) | 25 (12.5%) |
| Dehiscence | 4 (16%) | 11 (44%) | 10 (40%) | 25 (12.5%) | |
| (df = 1) | Pearson Chi-Square-χ2 | p 95% Confidence Interval |
|---|---|---|
| Dehiscence of VDC * pneumatization PP * | 7.864 | 0.049 |
| Protrusion of OPN * pneumatization of ACP * | 0.584 | 0.747 |
| Dehiscence of OPN * pneumatization of ACP * | 7.945 | 0.046 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Degaga, T.K.; Zenebe, A.M.; Wirtu, A.T.; Woldehawariat, T.D.; Dellie, S.T.; Gemechu, J.M. Anatomographic Variants of Sphenoid Sinus in Ethiopian Population. Diagnostics 2020, 10, 970. https://doi.org/10.3390/diagnostics10110970
Degaga TK, Zenebe AM, Wirtu AT, Woldehawariat TD, Dellie ST, Gemechu JM. Anatomographic Variants of Sphenoid Sinus in Ethiopian Population. Diagnostics. 2020; 10(11):970. https://doi.org/10.3390/diagnostics10110970
Chicago/Turabian StyleDegaga, Tizita K., Abay M. Zenebe, Amenu T. Wirtu, Tequam D. Woldehawariat, Seife T. Dellie, and Jickssa M. Gemechu. 2020. "Anatomographic Variants of Sphenoid Sinus in Ethiopian Population" Diagnostics 10, no. 11: 970. https://doi.org/10.3390/diagnostics10110970
APA StyleDegaga, T. K., Zenebe, A. M., Wirtu, A. T., Woldehawariat, T. D., Dellie, S. T., & Gemechu, J. M. (2020). Anatomographic Variants of Sphenoid Sinus in Ethiopian Population. Diagnostics, 10(11), 970. https://doi.org/10.3390/diagnostics10110970





