Liver Regeneration after Hepatectomy and Partial Liver Transplantation
Abstract
1. Introduction
2. Discussion and Literature Review
2.1. Liver Regeneration after PHx or PLTx
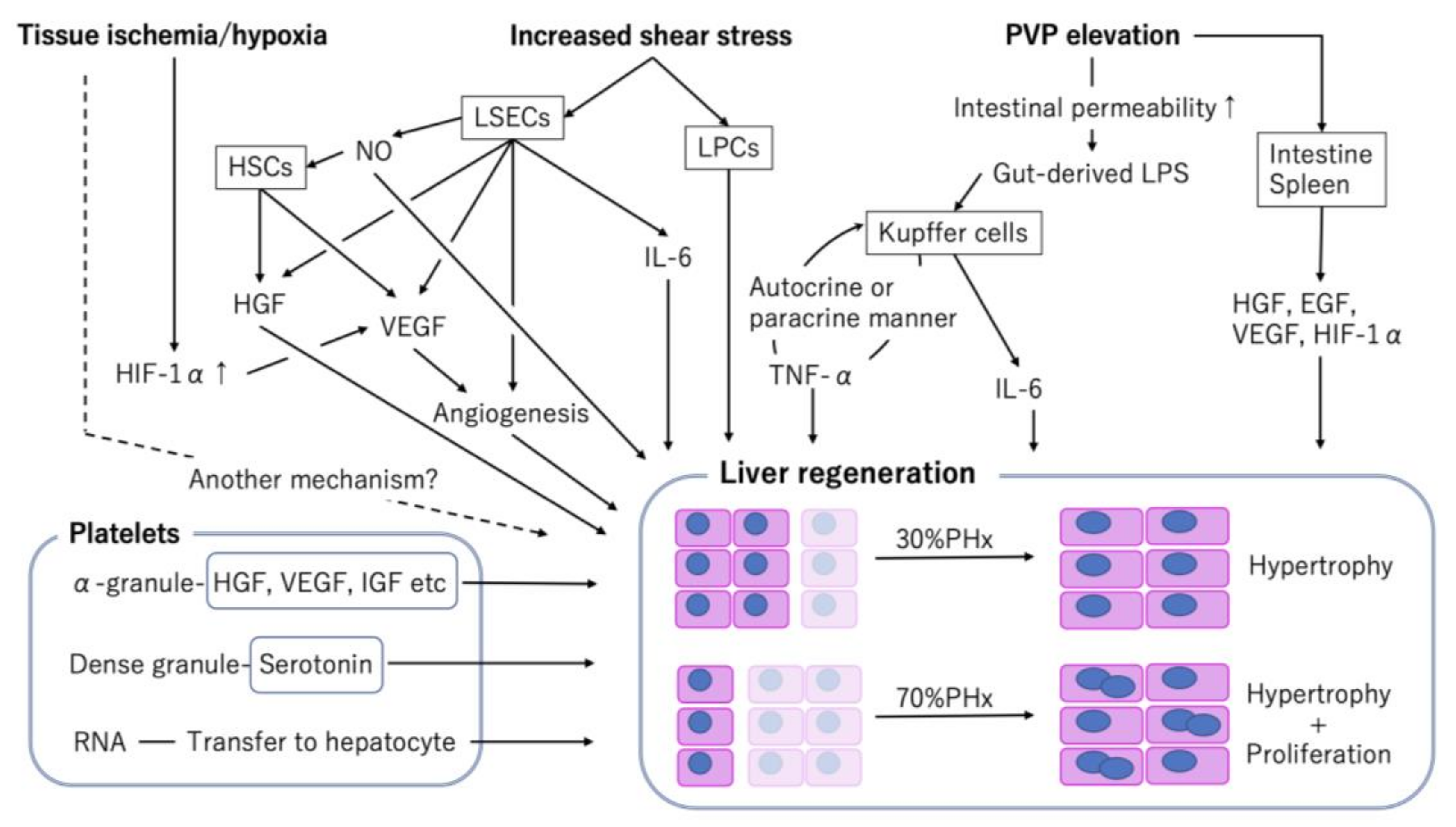
2.2. Hemodynamic Changes in Portal Venous Flow and Increase in Shear Stress
2.3. Influence of Portal Venous Pressure (PVP) Elevation on Extrahepatic Organs
2.4. Liver Hypoxia
2.5. Factors Associated with Hemostasis
2.6. The Role of Bile Acid
2.7. Major Signaling Pathways Associated with Liver Regeneration after PHx and PLTx
2.7.1. Ras/Raf/MEK/ERK Pathway
2.7.2. Janus Kinase (JAK)/Signal Transducer and Activator of Transcription 3 (STAT3) Pathway
2.7.3. PI3K/Akt Pathway
2.7.4. Nuclear Factor-κB (NF-κB) Pathway
2.7.5. Wnt/β-Catenin Pathway
2.7.6. Hippo Signaling Pathway
2.8. Marginal Liver: Aged or Steatotic Liver
2.8.1. Aged Liver
2.8.2. Steatotic Liver
2.9. Impact of Immunosuppressants
2.9.1. CNIs
2.9.2. mTOR Inhibitor
3. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| ALPPS | associating liver partition and portal vein ligation for staged hepatectomy |
| BrdU | bromodeoxyuridine 5-bromo-2’-deoxyuridine |
| BubR1 | budding uninhibited by benzimidazole-related 1 |
| C/EBP | CCAAT/enhancer-binding protein |
| CNI | calcineurin inhibitor |
| CyA | cyclosporine A |
| EGF | epidermal growth factor |
| EFGR | epidermal growth factor receptor |
| eNOS | endothelial nitric oxide synthetase |
| eIF4E | eukaryotic translation initiation factor 4E |
| FGF | fibroblast growth factor |
| FXR | farnesoid X receptor |
| GH | growth hormone |
| Gp | glycoprotein |
| HGF | hepatic growth factor |
| HIF-1α | hypoxia-inducible factor-1alpha |
| HSCs | hepatic stellate cells |
| IFN | interferon |
| IL | interleukin |
| iNOS | inducible nitric oxide synthetase |
| JAK | Janus kinase |
| LATS1/2 | large tumor suppressor 1/2 |
| LPCs | liver progenitor cells |
| LPS | lipopolysaccharide |
| LSECs | liver sinusoidal endothelial cells |
| MCDD | methionine- and choline-deficient diet |
| MMF | mycophenolate mofetil |
| MST1/2 | mammalian Ste20-like kinases 1/2 |
| mTOR | mammalian/mechanistic target of rapamycin |
| NF-κB | nuclear factor-κB |
| NK | natural killer cells |
| NO | nitric oxide |
| PAMPs | pathogen-associated molecular patterns |
| PCNA | proliferating cell nuclear antigen |
| PHx | partial hepatectomy |
| PI3K | phosphatidylinositol 3’-kinase |
| PLTx | partial liver transplantation |
| PRRs | pattern recognition receptors |
| PVL+T | portal vein ligation + hepatic transection |
| PVP | portal venous pressure |
| RTK | receptor tyrosine kinase |
| sIL-6R | soluble IL-6 receptor |
| S6Ks | S6 kinase |
| STAT | signal transducer and activator of transcription |
| TAZ | transcriptional coactivator with PDZ-binding motif |
| TEAD | transcriptional enhanced associate domain |
| TGF | transforming growth factor |
| TLRs | Toll-like receptors |
| TNF | tumor necrosis factor |
| VEGF | vascular endothelial growth factor |
| YAP | Yes-associated protein |
| 4E-BPs | eIF4E-binding proteins |
References
- Fausto, N.; Campbell, J.S.; Riehle, K.J. Liver regeneration. Hepatology 2006, 43, S45–S53. [Google Scholar] [CrossRef] [PubMed]
- Fausto, N.; Campbell, J.S.; Riehle, K.J. Liver regeneration. J. Hepatol. 2012, 57, 692–694. [Google Scholar] [CrossRef] [PubMed]
- Haga, J.; Shimazu, M.; Wakabayashi, G.; Tanabe, M.; Kawachi, S.; Fuchimoto, Y.; Hoshino, K.; Morikawa, Y.; Kitajima, M.; Kitagawa, Y. Liver regeneration in donors and adult recipients after living donor liver transplantation. Liver Transplant. 2008, 14, 1718–1724. [Google Scholar] [CrossRef] [PubMed]
- Miyaoka, Y.; Ebato, K.; Kato, H.; Arakawa, S.; Shimizu, S.; Miyajima, A. Hypertrophy and unconventional cell division of hepatocytes underlie liver regeneration. Curr. Biol. 2012, 22, 1166–1175. [Google Scholar] [CrossRef] [PubMed]
- Mao, S.A.; Glorioso, J.M.; Nyberg, S.L. Liver regeneration. Transl. Res. 2014, 163, 352–362. [Google Scholar] [CrossRef]
- Forbes, S.J.; Newsome, P.N. Liver regeneration—Mechanisms and models to clinical application. Nat. Rev. Gastroenterol. Hepatol. 2016, 13, 473–485. [Google Scholar] [CrossRef]
- Tao, Y.; Wang, M.; Chen, E.-Q.; Tang, H. Liver Regeneration: Analysis of the main relevant signaling molecules. Mediat. Inflamm. 2017, 2017, 1–9. [Google Scholar] [CrossRef]
- Gilgenkrantz, H.; De L’Hortet, A.C. Understanding liver regeneration: From mechanisms to regenerative medicine. Am. J. Pathol. 2018, 188, 1316–1327. [Google Scholar] [CrossRef]
- Van Haele, M.; Snoeck, J.; Roskams, T. Human liver regeneration: An etiology dependent process. Int. J. Mol. Sci. 2019, 20, 2332. [Google Scholar] [CrossRef]
- Ozaki, M. Cellular and molecular mechanisms of liver regeneration: Proliferation, growth, death and protection of hepatocytes. Semin. Cell Dev. Biol. 2020, 100, 62–73. [Google Scholar] [CrossRef]
- Shi, J.; Line, P.-D. Hallmarks of postoperative liver regeneration: An updated insight on the regulatory mechanisms. J. Gastroenterol. Hepatol. 2019, 35, 960–966. [Google Scholar] [CrossRef] [PubMed]
- Bhushan, B.; Apte, U. Liver regeneration after acetaminophen hepatotoxicity. Am. J. Pathol. 2019, 189, 719–729. [Google Scholar] [CrossRef] [PubMed]
- Sato, Y.; Tsukada, K.; Hatakeyama, K. Role of shear stress and immune responses in liver regeneration after a partial hepatectomy. Surg. Today 1999, 29, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Sato, Y.; Koyama, S.; Tsukada, K.; Hatakeyama, K. Acute portal hypertension reflecting shear stress as a trigger of liver regeneration following partial hepatectomy. Surg. Today 1997, 27, 518–526. [Google Scholar] [CrossRef] [PubMed]
- Morsiani, E.; Aleotti, A.; Ricci, D. Haemodynamic and ultrastructural observations on the rat liver after two-thirds partial hepatectomy. J. Anat. 1998, 192, 507–515. [Google Scholar] [CrossRef]
- Schoen, J.M.; Wangb, H.H.; Minukac, G.Y.; Lautt, W. Shear stress-induced nitric oxide release triggers the liver regeneration cascade. Nitric Oxide 2001, 5, 453–464. [Google Scholar] [CrossRef]
- Golse, N.; Bucur, P.O.; Adam, R.; Castaing, D.; Cunha, A.S.; Vibert, E. New paradigms in post-hepatectomy liver failure. J. Gastrointest. Surg. 2012, 17, 593–605. [Google Scholar] [CrossRef]
- Poisson, J.; Lemoinne, S.; Boulanger, C.; Durand, F.; Moreau, R.; Valla, D.; Rautou, P.-E. Liver sinusoidal endothelial cells: Physiology and role in liver diseases. J. Hepatol. 2017, 66, 212–227. [Google Scholar] [CrossRef]
- Rai, R.M.; Lee, F.Y.J.; Rosen, A.; Yang, S.Q.; Lin, H.Z.; Koteish, A.; Liew, F.Y.; Zaragoza, C.; Lowenstein, C.; Diehl, A.M. Impaired liver regeneration in inducible nitric oxide synthase deficient mice. Proc. Natl. Acad. Sci. USA 1998, 95, 13829–13834. [Google Scholar] [CrossRef]
- Mei, Y.; Thevananther, S. Endothelial nitric oxide synthase is a key mediator of hepatocyte proliferation in response to partial hepatectomy in mice. Hepatology 2011, 54, 1777–1789. [Google Scholar] [CrossRef]
- Carnovale, C.E.; Ronco, M.T. Role of nitric oxide in liver regeneration. Ann. Hepatol. 2012, 11, 636–647. [Google Scholar] [CrossRef]
- Kawai, M.; Naruse, K.; Komatsu, S.; Kobayashi, S.; Nagino, M.; Nimura, Y.; Sokabe, M. Mechanical stress-dependent secretion of interleukin 6 by endothelial cells after portal vein embolization: Clinical and experimental studies. J. Hepatol. 2002, 37, 240–246. [Google Scholar] [CrossRef]
- Nishii, K.; Brodin, E.; Renshaw, T.; Weesner, R.; Moran, E.; Soker, S.; Sparks, J.L. Shear stress upregulates regeneration-related immediate early genes in liver progenitors in 3D ECM-like microenvironments. J. Cell Physiol. 2017, 233, 4272–4281. [Google Scholar] [CrossRef] [PubMed]
- Abu Rmilah, A.; Zhou, W.; Nelson, E.; Lin, L.; Amiot, B.; Nyberg, S.L. Understanding the marvels behind liver regeneration. Wiley Interdiscip. Rev. Dev. Biol. 2019, 8, e340. [Google Scholar] [CrossRef]
- Arab, J.P.; Martin-Mateos, R.M.; Shah, V.H. Gut–liver axis, cirrhosis and portal hypertension: The chicken and the egg. Hepatol. Int. 2017, 12, 24–33. [Google Scholar] [CrossRef]
- Cornell, R.P. Gut-derived endotoxin elicits hepatotrophic factor secretion for liver regeneration. Am. J. Physiol. Integr. Comp. Physiol. 1985, 249, R551–R562. [Google Scholar] [CrossRef]
- Cornell, R.P.; Liljequist, B.L.; Bartizal, K.F. Depressed liver regeneration after partial hepatectomy of germ-free, athymic and lipopolysaccharide-resistant mice. Hepatology 1990, 11, 916–922. [Google Scholar] [CrossRef]
- Seki, E.; Tsutsui, H.; Iimuro, Y.; Naka, T.; Son, G.; Akira, S.; Kishimoto, T.; Nakanishi, K.; Fujimoto, J. Contribution of Toll-like receptor/myeloid differentiation factor 88 signaling to murine liver regeneration. Hepatology 2005, 41, 443–450. [Google Scholar] [CrossRef]
- Campbell, J.S.; Riehle, K.J.; Brooling, J.T.; Bauer, R.L.; Mitchell, C.; Fausto, N. Proinflammatory cytokine production in liver regeneration is Myd88-dependent, but independent ofvCd14, Tlr2, and Tlr. J. Immunol. 2006, 176, 2522–2528. [Google Scholar] [CrossRef]
- Yamamoto, C.; Yagi, S.; Hori, T.; Iida, T.; Taniguchi, K.; Isaji, S.; Uemoto, S. Significance of portal venous VEGF during liver regeneration after hepatectomy. J. Surg. Res. 2010, 159, e37–e43. [Google Scholar] [CrossRef][Green Version]
- Liu, H.-X.; Keane, R.; Sheng, L.; Wan, Y.-J.Y. Implications of microbiota and bile acid in liver injury and regeneration. J. Hepatol. 2015, 63, 1502–1510. [Google Scholar] [CrossRef] [PubMed]
- Rahbari, N.N.; Garden, O.J.; Padbury, R.; Brooke-Smith, M.; Crawford, M.; Adam, R.; Koch, M.; Makuuchi, M.; DeMatteo, R.P.; Christophi, C.; et al. Posthepatectomy liver failure: A definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery 2011, 149, 713–724. [Google Scholar] [CrossRef] [PubMed]
- Dahm, F.; Georgiev, P.; Clavien, P.-A. Small-for-size syndrome after partial liver transplantation: Definition, mechanisms of disease and clinical implications. Arab. Archaeol. Epigr. 2005, 5, 2605–2610. [Google Scholar] [CrossRef] [PubMed]
- Yagi, S.; Iida, T.; Taniguchi, K.; Hori, T.; Hamada, T.; Fujii, K.; Mizuno, S.; Uemoto, S. Impact of portal venous pressure on regeneration and graft damage after living-donor liver transplantation. Liver Transplant. 2004, 11, 68–75. [Google Scholar] [CrossRef]
- Yagi, S.; Iida, T.; Hori, T.; Taniguchi, K.; Nagahama, M.; Isaji, S.; Uemoto, S. Effect of portal haemodynamics on liver graft and intestinal mucosa after small-for-size liver transplantation in swine. Eur. Surg. Res. 2012, 48, 163–170. [Google Scholar] [CrossRef]
- Abshagen, K.; Eipel, C.; Vollmar, B. A critical appraisal of the hemodynamic signal driving liver regeneration. Langenbeck’s Arch. Surg. 2012, 397, 579–590. [Google Scholar] [CrossRef]
- Dold, S.; Richter, S.; Kollmar, O.; Von Heesen, M.; Scheuer, C.; Laschke, M.W.; Vollmar, B.; Schilling, M.K.; Menger, M.D. Portal hyperperfusion after extended hepatectomy does not induce a hepatic arterial buffer response (HABR) but impairs mitochondrial redox state and hepatocellular oxygenation. PLoS ONE 2015, 10, e0141877. [Google Scholar] [CrossRef]
- Dirscherl, K.; Schläpfer, M.; Z’Graggen, B.R.; Wenger, R.H.; Booy, C.; Flury-Frei, R.; Fatzer, R.; Aloman, C.; Bartosch, B.; Parent, R.; et al. Hypoxia sensing by hepatic stellate cells leads to VEGF-dependent angiogenesis and may contribute to accelerated liver regeneration. Sci. Rep. 2020, 10, 1–13. [Google Scholar] [CrossRef]
- Iyer, N.V.; Kotch, L.E.; Agani, F.; Leung, S.W.; Laughner, E.; Wenger, R.H.; Gassmann, M.; Gearhart, J.D.; Lawler, A.M.; Yu, A.Y.; et al. Cellular and developmental control of O2 homeostasis by hypoxia-inducible factor 1alpha. Genes Dev. 1998, 12, 149–162. [Google Scholar] [CrossRef]
- Schodel, J.; Oikonomopoulos, S.; Ragoussis, J.; Pugh, C.W.; Ratcliffe, P.J.; Mole, D.R. High-resolution genome-wide mapping of hif-binding sites by chip-seq. Blood 2011, 117, e207–e217. [Google Scholar] [CrossRef]
- Nath, B.D.; Szabo, G. Hypoxia and hypoxia inducible factors: Diverse roles in liver diseases. Hepatology 2012, 55, 622–633. [Google Scholar] [CrossRef] [PubMed]
- Maeno, H.; Ono, T.; Dhar, D.K.; Sato, T.; Yamanoi, A.; Nagasue, N. Expression of hypoxia inducible factor-1alpha during liver regeneration induced by partial hepatectomy in rats. Liver Int. 2005, 25, 1002–1009. [Google Scholar] [CrossRef] [PubMed]
- Schadde, E.; Tsatsaris, C.; Swiderska-Syn, M.; Breitenstein, S.; Urner, M.; Schimmer, R.; Booy, C.; Z’Graggen, B.R.; Wenger, R.H.; Spahn, D.R.; et al. Hypoxia of the growing liver accelerates regeneration. Surgery 2017, 161, 666–679. [Google Scholar] [CrossRef] [PubMed]
- Ren, P.; Kang, Z.; Gu, G.; Liu, Y.; Xu, W.; Tao, H.; Zhang, F.; Sun, X.; Ji, H. Hyperbaric oxygen preconditioning promotes angiogenesis in rat liver after partial hepatectomy. Life Sci. 2008, 83, 236–241. [Google Scholar] [CrossRef]
- Kron, P.; Linecker, M.; Limani, P.; Schlegel, A.; Kambakamba, P.; Lehn, J.-M.; Nicolau, C.; Graf, R.; Humar, B.; Clavien, P.-A. Hypoxia-driven Hif2a coordinates mouse liver regeneration by coupling parenchymal growth to vascular expansion. Hepatology 2016, 64, 2198–2209. [Google Scholar] [CrossRef]
- Starlinger, P.; Luyendyk, J.P.; Groeneveld, D.J. Hemostasis and liver regeneration. Semin. Thromb. Hemost. 2020, 46, 735–742. [Google Scholar] [CrossRef]
- Groeneveld, D.; Pereyra, D.; Veldhuis, Z.; Adelmeijer, J.; Ottens, P.; Kopec, A.K.; Starlinger, P.; Lisman, T.; Luyendyk, J.P. Intrahepatic fibrin(ogen) deposition drives liver regeneration after partial hepatectomy in mice and humans. Blood 2019, 133, 1245–1256. [Google Scholar] [CrossRef]
- Kirschbaum, M.; Jenne, C.N.; Veldhuis, Z.J.; Sjollema, K.A.; Lenting, P.J.; Porte, R.J.; Kubes, P.; Denis, C.V.; Lisman, T.; Giepmans, B.N.G. Transient von Willebrand factor-mediated platelet influx stimulates liver regeneration after partial hepatectomy in mice. Liver Int. 2017, 37, 1731–1737. [Google Scholar] [CrossRef]
- Tatsumi, K.; Ohashi, K.; Taminishi, S.; Sakurai, Y.; Ogiwara, K.; Yoshioka, A.; Okano, T.; Shima, M. Regulation of coagulation factors during liver regeneration in mice: Mechanism of factor VIII elevation in plasma. Thromb. Res. 2011, 128, 54–61. [Google Scholar] [CrossRef]
- Lesurtel, M.; Graf, R.; Aleil, B.; Walther, D.J.; Tian, Y.; Jochum, W.; Gachet, C.; Bader, M.; Clavien, P.-A. Platelet-derived serotonin mediates liver regeneration. Science 2006, 312, 104–107. [Google Scholar] [CrossRef]
- Matsuo, R.; Nakano, Y.; Ohkohchi, N. Platelet administration via the portal vein promotes liver regeneration in rats after 70% hepatectomy. Ann. Surg. 2011, 253, 759–763. [Google Scholar] [CrossRef] [PubMed]
- Han, S.; Park, H.-W.; Song, J.H.; Gwak, M.S.; Lee, W.J.; Kim, G.; Lee, S.-K.; Ko, J.S. Association between intraoperative platelet transfusion and early graft regeneration in living donor liver transplantation. Ann. Surg. 2016, 264, 1065–1072. [Google Scholar] [CrossRef] [PubMed]
- Lisman, T.; Porte, R.J. Mechanisms of platelet-mediated liver regeneration. Blood 2016, 128, 625–629. [Google Scholar] [CrossRef] [PubMed]
- Fang, Y.; Liu, C.; Shu, B.; Zhai, M.; Deng, C.; He, C.; Luo, M.; Han, T.; Zheng, W.; Zhang, J.; et al. Axis of serotonin -pERK-YAP in liver regeneration. Life Sci. 2018, 209, 490–497. [Google Scholar] [CrossRef] [PubMed]
- Kirschbaum, M.; Karimian, G.; Adelmeijer, J.; Giepmans, B.N.G.; Porte, R.J.; Lisman, T. Horizontal RNA transfer mediates platelet-induced hepatocyte proliferation. Blood 2015, 126, 798–806. [Google Scholar] [CrossRef]
- Dong, X.; Zhao, H.; Ma, X.; Wang, S. Reduction in bile acid pool causes delayed liver regeneration accompanied by down-regulated expression of FXR and c-Jun mRNA in rats. J. Huazhong Univ. Sci. Technolog. Med. Sci. 2010, 30, 55–60. [Google Scholar] [CrossRef]
- Naugler, W.E. Bile acid flux is necessary for normal liver regeneration. PLoS ONE 2014, 9, e97426. [Google Scholar] [CrossRef]
- Takagi, T.; Yokoyama, Y.; Kokuryo, T.; Yamaguchi, J.; Nagino, M. Liver regeneration following experimental major hepatectomy with choledochojejunostomy. Br. J. Surg. 2015, 102, 1410–1417. [Google Scholar] [CrossRef]
- Van De Laarschot, L.F.M.; Jansen, P.L.M.; Schaap, F.G.; Damink, S.W.M.O. The role of bile salts in liver regeneration. Hepatol. Int. 2016, 10, 733–740. [Google Scholar] [CrossRef]
- Otao, R.; Beppu, T.; Isiko, T.; Mima, K.; Okabe, H.; Hayashi, H.; Masuda, T.; Chikamoto, A.; Takamori, H.; Baba, H. External biliary drainage and liver regeneration after major hepatectomy. Br. J. Surg. 2012, 99, 1569–1574. [Google Scholar] [CrossRef]
- Watanabe, K.; Yokoyama, Y.; Kokuryo, T.; Kawai, K.; Kitagawa, T.; Seki, T.; Nakagawa, A.; Nagino, M. Segmental cholangitis impairs hepatic regeneration capacity after partial hepatectomy in rats. HPB 2010, 12, 664–673. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bednarsch, J.; Blüthner, E.; Malinowski, M.; Seehofer, D.; Pratschke, J.; Stockmann, M. Regeneration of liver function capacity after partial liver resection is impaired in case of postoperative bile leakage. World J. Surg. 2016, 40, 2221–2228. [Google Scholar] [CrossRef] [PubMed]
- Yoshikawa, J.; Hata, K.; Nakamura, K.; Okamura, Y.; Uemoto, S. The impact of biliary reconstruction methods on small partial liver grafts. Transplant. Direct 2020, 6, e523. [Google Scholar] [CrossRef] [PubMed]
- Asati, V.; Mahapatra, D.K.; Bharti, S.K. ChemInform Abstract: PI3K/Akt/mTOR and Ras/Raf/MEK/ERK signaling pathways inhibitors as anticancer agents: Structural and pharmacological perspectives. Eur. J. Med. Chem. 2016, 47, 314–341. [Google Scholar] [CrossRef] [PubMed]
- Simanshu, D.K.; Nissley, D.V.; McCormick, F. RAS proteins and their regulators in human disease. Cell 2017, 170, 17–33. [Google Scholar] [CrossRef]
- Ersahin, T.; Tuncbag, N.; Cetin-Atalay, R. The PI3K/AKT/mTOR interactive pathway. Mol. BioSyst. 2015, 11, 1946–1954. [Google Scholar] [CrossRef]
- Kolch, W. Meaningful relationships: The regulation of the Ras/Raf/Mek/Erk pathway by protein interactions. Biochem. J. 2000, 351, 289–305. [Google Scholar] [CrossRef]
- Blindenbacher, A.; Wang, X.; Langer, I.; Savino, R.; Terracciano, L.; Heim, M.H. Interleukin 6 is important for survival after partial hepatectomy in mice. Hepatology 2003, 38, 674–682. [Google Scholar] [CrossRef]
- Gao, B.; Wang, H.; Lafdil, F.; Feng, D. STAT proteins—Key regulators of anti-viral responses, inflammation, and tumorigenesis in the liver. J. Hepatol. 2012, 57, 430–441. [Google Scholar] [CrossRef]
- Schmidt-Arras, D.; Rose-John, S. IL-6 pathway in the liver: From physiopathology to therapy. J. Hepatol. 2016, 64, 1403–1415. [Google Scholar] [CrossRef]
- Mackiewicz, A.; Schooltink, H.; Heinrich, P.C.; Rose-John, S. Complex of soluble human IL-6-receptor/IL-6 up-regulates expression of acute-phase proteins. J. Immunol. 1992, 149, 2021–2027. [Google Scholar] [PubMed]
- Modares, N.F.; Polz, R.; Haghighi, F.; Lamertz, L.; Behnke, K.; Zhuang, Y.; Kordes, C.; Häussinger, D.; Sorg, U.R.; Pfeffer, K.; et al. IL-6 Trans-signaling controls liver regeneration after partial hepatectomy. Hepatology 2019, 70, 2075–2091. [Google Scholar] [CrossRef] [PubMed]
- Jackson, L.N.; Larson, S.D.; Silva, S.R.; Rychahou, P.G.; Chen, L.A.; Qiu, S.; Rajaraman, S.; Evers, B.M. PI3K/Akt activation is critical for early hepatic regeneration after partial hepatectomy. Am. J. Physiol. Liver Physiol. 2008, 294, G1401–G1410. [Google Scholar] [CrossRef] [PubMed]
- Fruman, D.A.; Mauvais-Jarvis, F.; Pollard, D.A.; Yballe, C.M.; Brazil, D.; Bronson, R.T.; Kahn, C.R.; Cantley, L.C. Hypoglycaemia, liver necrosis and perinatal death in mice lacking all isoforms of phosphoinositide 3-Kinase P85 alpha. Nat. Genet. 2000, 26, 379–382. [Google Scholar] [CrossRef] [PubMed]
- Haga, S.; Ogawa, W.; Inoue, H.; Terui, K.; Ogino, T.; Igarashi, R.; Takeda, K.; Akira, S.; Enosawa, S.; Furukawa, H.; et al. Compensatory recovery of liver mass by Akt-mediated hepatocellular hypertrophy in liver-specific STAT3-deficient mice. J. Hepatol. 2005, 43, 799–807. [Google Scholar] [CrossRef]
- Morita, M.; Gravel, S.-P.; Hulea, L.; Larsson, O.; Pollak, M.; St-Pierre, J.; Topisirovic, I. mTOR coordinates protein synthesis, mitochondrial activity and proliferation. Cell Cycle 2015, 14, 473–480. [Google Scholar] [CrossRef]
- Crino, P.B. The mTOR signalling cascade: Paving new roads to cure neurological disease. Nat. Rev. Neurol. 2016, 12, 379–392. [Google Scholar] [CrossRef]
- Solt, L.A.; May, M.J. The Ikappab kinase complex: Master regulator of Nf-kappab signaling. Immunol. Res. 2008, 42, 3–18. [Google Scholar] [CrossRef]
- Taniguchi, K.; Karin, M. NF-κB, inflammation, immunity and cancer: Coming of age. Nat. Rev. Immunol. 2018, 18, 309–324. [Google Scholar] [CrossRef]
- Monga, S.P.; Pediaditakis, P.; Mule, K.; Stolz, D.B.; Michalopoulos, G.K. Changes in Wnt/beta-catenin pathway during regulated growth in rat liver regeneration. Hepatology 2001, 33, 1098–1109. [Google Scholar] [CrossRef]
- Preziosi, M.; Okabe, H.; Poddar, M.; Singh, S.; Monga, S.P. Endothelial Wnts regulate beta-catenin signaling in murine liver zonation and regeneration: A sequel to the Wnt-Wnt situation. Hepatol. Commun. 2018, 2, 845–860. [Google Scholar] [CrossRef] [PubMed]
- Zhao, L.; Jin, Y.; Donahue, K.; Tsui, M.; Fish, M.; Logan, C.Y.; Wang, B.; Nusse, R. Tissue repair in the mouse liver following acute carbon tetrachloride depends on injury-induced Wnt/beta-catenin signaling. Hepatology 2019, 69, 2623–2635. [Google Scholar] [PubMed]
- Ma, Y.; Lv, X.; He, J.; Liu, T.; Wen, S.; Wang, L. Wnt agonist stimulates liver regeneration after small-for-size liver transplantation in rats. Hepatol. Res. 2015, 46, 154–164. [Google Scholar] [CrossRef] [PubMed]
- Monga, S.P. Beta-catenin signaling and roles in liver homeostasis, injury, and tumorigenesis. Gastroenterology 2015, 148, 1294–1310. [Google Scholar] [CrossRef]
- Nejak-Bowen, K.; Kikuchi, A.; Monga, S.P. Beta-catenin-Nf-kappab interactions in murine hepatocytes: A complex to die for. Hepatology 2013, 57, 763–774. [Google Scholar] [CrossRef]
- Zheng, Y.; Pan, D. The hippo signaling pathway in development and disease. Dev. Cell 2019, 50, 264–282. [Google Scholar] [CrossRef]
- Manmadhan, S.; Ehmer, U. Hippo signaling in the liver—A long and ever-expanding story. Front. Cell Dev. Biol. 2019, 7, 33. [Google Scholar] [CrossRef]
- Meng, Z.; Moroishi, T.; Guan, K.-L. Mechanisms of Hippo pathway regulation. Genes Dev. 2016, 30, 1–17. [Google Scholar] [CrossRef]
- Mizuno, T.; Murakami, H.; Fujii, M.; Ishiguro, F.; Tanaka, I.; Kondo, Y.; Akatsuka, S.; Toyokuni, S.; Yokoi, K.; Osada, H.; et al. YAP induces malignant mesothelioma cell proliferation by upregulating transcription of cell cycle-promoting genes. Oncogene 2012, 31, 5117–5122. [Google Scholar] [CrossRef]
- Moya, I.M.; Halder, G. Hippo–YAP/TAZ signalling in organ regeneration and regenerative medicine. Nat. Rev. Mol. Cell Biol. 2019, 20, 211–226. [Google Scholar] [CrossRef]
- Loforese, G.; Malinka, T.; Keogh, A.; Baier, F.; Simillion, C.; Montani, M.; Halazonetis, T.D.; Candinas, D.; Stroka, D. Impaired liver regeneration in aged mice can be rescued by silencing Hippo core kinases MST1 and MST2. EMBO Mol. Med. 2016, 9, 46–60. [Google Scholar] [CrossRef] [PubMed]
- Lu, L.; Finegold, M.J.; Johnson, R.L. Hippo pathway coactivators Yap and Taz are required to coordinate mammalian liver regeneration. Exp. Mol. Med. 2018, 50, e423. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.M.; Choi, Y.J.; Hwang, J.-H.; Kim, A.R.; Cho, H.J.; Hwang, E.S.; Park, J.Y.; Lee, S.-H.; Hong, J.-H. Shear stress induced by an interstitial level of slow flow increases the osteogenic differentiation of mesenchymal stem cells through TAZ activation. PLoS ONE 2014, 9, e92427. [Google Scholar] [CrossRef] [PubMed]
- Sabine, A.; Bovay, E.; Demir, C.S.; Kimura, W.; Jaquet, M.; Agalarov, Y.; Zangger, N.; Scallan, J.P.; Graber, W.; Gulpinar, E.; et al. FOXC2 and fluid shear stress stabilize postnatal lymphatic vasculature. J. Clin. Investig. 2015, 125, 3861–3877. [Google Scholar] [CrossRef] [PubMed]
- Oh, S.H.; Swiderska-Syn, M.; Jewell, M.L.; Premont, R.T.; Diehl, A.M. Liver regeneration requires Yap1-Tgfbeta-dependent epithelial-mesenchymal transition in hepatocytes. J. Hepatol. 2018, 69, 359–367. [Google Scholar] [CrossRef] [PubMed]
- Yimlamai, D.; Fowl, B.H.; Camargo, F.D. Emerging evidence on the role of the Hippo/YAP pathway in liver physiology and cancer. J. Hepatol. 2015, 63, 1491–1501. [Google Scholar] [CrossRef]
- Kim, N.-G.; Gumbiner, B.M. Adhesion to fibronectin regulates Hippo signaling via the FAK–Src–PI3K pathway. J. Cell Biol. 2015, 210, 503–515. [Google Scholar] [CrossRef]
- Hong, A.W.; Meng, Z.; Guan, K.-L. The Hippo pathway in intestinal regeneration and disease. Nat. Rev. Gastroenterol. Hepatol. 2016, 13, 324–337. [Google Scholar] [CrossRef]
- Dodig, S.; Čepelak, I.; Pavić, I. Hallmarks of senescence and aging. Biochem. Med. (Zagreb) 2019, 29, 483–497. [Google Scholar] [CrossRef]
- Pibiri, M. Liver regeneration in aged mice: New insights. Aging (Albany NY) 2018, 10, 1801–1824. [Google Scholar] [CrossRef]
- Le Lay, J.; Kaestner, K.H. The fox genes in the liver: From organogenesis to functional integration. Physiol. Rev. 2010, 90, 1–22. [Google Scholar] [CrossRef] [PubMed]
- Gartel, A.L. FOXM1 in Cancer: Interactions and vulnerabilities. Cancer Res. 2017, 77, 3135–3139. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Quail, E.; Hung, N.-J.; Tan, Y.; Ye, H.; Costa, R.H. Increased levels of forkhead box M1B transcription factor in transgenic mouse hepatocytes prevent age-related proliferation defects in regenerating liver. Proc. Natl. Acad. Sci. USA 2001, 98, 11468–11473. [Google Scholar] [CrossRef]
- Iakova, P.; Awad, S.S.; Timchenko, N.A. Aging reduces proliferative capacities of liver by switching pathways of C/EBPα growth arrest. Cell 2003, 113, 495–506. [Google Scholar] [CrossRef]
- Overlack, K.; Bange, T.; Weissmann, F.; Faesen, A.C.; Maffini, S.; Primorac, I.; Müller, F.; Peters, J.-M.; Musacchio, A. BubR1 promotes Bub3-dependent APC/C inhibition during spindle assembly checkpoint signaling. Curr. Biol. 2017, 27, 2915–2927. [Google Scholar] [CrossRef]
- Ikawa-Yoshida, A.; Matsumoto, T.; Okano, S.; Aoyagi, Y.; Matsubara, Y.; Furuyama, T.; Nakatsu, Y.; Tsuzuki, T.; Onimaru, M.; Ohkusa, T.; et al. BubR1 insufficiency impairs liver regeneration in aged mice after hepatectomy through intercalated disc abnormality. Sci. Rep. 2016, 6, 32399. [Google Scholar] [CrossRef]
- Pibiri, M.; Sulas, P.; Leoni, V.P.; Perra, A.; Kowalik, M.A.; Cordella, A.; Saggese, P.; Nassa, G.; Ravo, M. Global gene expression profile of normal and regenerating liver in young and old mice. AGE 2015, 37, 9796. [Google Scholar] [CrossRef]
- Conboy, I.M.; Conboy, M.J.; Wagers, A.J.; Girma, E.R.; Weissman, I.L.; Rando, T.A. Rejuvenation of aged progenitor cells by exposure to a young systemic environment. Nat. Cell Biol. 2005, 433, 760–764. [Google Scholar] [CrossRef]
- Liu, A.; Guo, E.; Yang, J.; Yang, Y.; Liu, S.; Jiang, X.; Hu, Q.; Dirsch, O.; Dahmen, U.; Zhang, C.; et al. Young plasma reverses age-dependent alterations in hepatic function through the restoration of autophagy. Aging Cell 2017, 17. [Google Scholar] [CrossRef]
- Ibrahim, S.; Chen, C.-L.; Wang, C.-C.; Wang, S.-H.; Lin, C.-C.; Liu, Y.-W.; Yang, C.-H.; Yong, C.-C.; Concejero, A.M.; Cheng, Y.-F. Liver regeneration and splenic enlargement in donors after living-donor liver transplantation. World J. Surg. 2005, 29, 1658–1666. [Google Scholar] [CrossRef]
- Kele, P.G.; Van Der Jagt, E.J.; Gouw, A.S.H.; Lisman, T.; Porte, R.J.; De Boer, M.T. The impact of hepatic steatosis on liver regeneration after partial hepatectomy. Liver Int. 2013, 33, 469–475. [Google Scholar] [CrossRef] [PubMed]
- Zhang, B.; Weltman, M.; Farrell, G. Does steatohepatitis impair liver regeneration? A study in a dietary model of non-alcoholic steatohepatitis in rats. J. Gastroenterol. Hepatol. 2002, 14, 133–137. [Google Scholar] [CrossRef] [PubMed]
- Selzner, M.; Clavien, P.-A. Failure of regeneration of the steatotic rat liver: Disruption at two different levels in the regeneration pathway. Hepatology 2000, 31, 35–42. [Google Scholar] [CrossRef] [PubMed]
- Rao, M.; Papreddy, K.; Abecassis, M.; Hashimoto, T. Regeneration of liver with marked fatty change following partial hepatectomy in rats. Dig. Dis. Sci. 2001, 46, 1821–1826. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.Q.; Lin, H.Z.; Mandal, A.K.; Huang, J.; Diehl, A.M. Disrupted signaling and inhibited regeneration in obese mice with fatty livers: Implications for nonalcoholic fatty liver disease pathophysiology. Hepatology 2001, 34, 694–706. [Google Scholar] [CrossRef] [PubMed]
- Torbenson, M.; Yang, S.Q.; Liu, H.Z.; Huang, J.; Gage, W.; Diehl, A.M. STAT-3 Overexpression and p21 up-regulation accompany impaired regeneration of fatty livers. Am. J. Pathol. 2002, 161, 155–161. [Google Scholar] [CrossRef]
- Picard, C.; Lambotte, L.; Starkel, P.; Sempoux, C.; Saliez, A.; Berge, V.V.D.; Horsmans, Y. Steatosis is not sufficient to cause an impaired regenerative response after partial hepatectomy in rats. J. Hepatol. 2002, 36, 645–652. [Google Scholar] [CrossRef]
- Yamauchi, H.; Uetsuka, K.; Okada, T.; Nakayama, H.; Doi, K. Impaired liver regeneration after partial hepatectomy in db/db mice. Exp. Toxicol. Pathol. 2003, 54, 281–286. [Google Scholar] [CrossRef]
- DeAngelis, R.A.; Markiewski, M.M.; Taub, R.; Lambris, J.D. A high-fat diet impairs liver regeneration in C57bl/6 mice through overexpression of the Nf-kappab inhibitor, ikappabalpha. Hepatology 2005, 42, 1148–1157. [Google Scholar] [CrossRef]
- Tanoue, S.; Uto, H.; Kumamoto, R.; Arima, S.; Hashimoto, S.; Nasu, Y.; Takami, Y.; Moriuchi, A.; Sakiyama, T.; Oketani, M.; et al. Liver regeneration after partial hepatectomy in rat is more impaired in a steatotic liver induced by dietary fructose compared to dietary fat. Biochem. Biophys. Res. Commun. 2011, 407, 163–168. [Google Scholar] [CrossRef]
- Sydor, S.; Gu, Y.; Schlattjan, M.; Bechmann, L.P.; Rauen, U.; Best, J.; Paul, A.; Baba, H.A.; Sowa, J.-P.; Gerken, G.; et al. Steatosis does not impair liver regeneration after partial hepatectomy. Lab. Investig. 2012, 93, 20–30. [Google Scholar] [CrossRef] [PubMed]
- De L’Hortet, A.C.; Zerrad-Saadi, A.; Prip-Buus, C.; Fauveau, V.; Helmy, N.; Ziol, M.; Vons, C.; Billot, K.; Baud, V.; Gilgenkrantz, H.; et al. GH Administration rescues fatty liver regeneration impairment by restoring GH/EGFR pathway deficiency. Endocrinolology 2014, 155, 2545–2554. [Google Scholar] [CrossRef]
- Zimmers, T.A.; Jin, X.; Zhang, Z.; Jiang, Y.; Koniaris, L.G. Epidermal growth factor receptor restoration rescues the fatty liver regeneration in mice. Am. J. Physiol. Endocrinol. Metab. 2017, 313, E440–E449. [Google Scholar] [CrossRef] [PubMed]
- Valdecantos, M.P.; Pardo, V.; Ruiz, L.; Castro-Sanchez, L.; Lanzon, B.; Fernandez-Millan, E.; Garcia-Monzon, C.; Arroba, A.I.; Gonzalez-Rodriguez, A.; Escriva, F.; et al. A novel glucagon-like peptide 1/glucagon receptor dual agonist improves steatohepatitis and liver regeneration in mice. Hepatology 2017, 65, 950–968. [Google Scholar] [CrossRef] [PubMed]
- Akhurst, B.; Croager, E.J.; Farley-Roche, C.A.; Ong, J.K.; Dumble, M.L.; Knight, B.; Yeoh, G.C. A modified choline-deficient, ethionine-supplemented diet protocol effectively induces oval cells in mouse liver. Hepatology 2001, 34, 519–522. [Google Scholar] [CrossRef] [PubMed]
- Farrell, G.C.; Robertson, G.R.; Leclercq, I.; Horsmans, Y. Liver regeneration in obese mice with fatty livers: Does the impairment have relevance for other types of fatty liver disease? Hepatology 2002, 35, 731. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Huang, X.; He, L.; Pu, W.; Li, Y.; Liu, Q.; Li, Y.; Zhang, L.; Yu, W.; Zhao, H.; et al. Genetic tracing of hepatocytes in liver homeostasis, injury, and regeneration. J. Biol. Chem. 2017, 292, 8594–8604. [Google Scholar] [CrossRef]
- Kort, W.J.; Van der Post, J. Influences of azathiprine and prednisone on rat liver regeneration. Eur. Surg. Res. 1973, 5, 373–383. [Google Scholar] [CrossRef]
- Azzarone, A.; Francavilla, A.; Zeng, Q.H.; Starzl, T.E. Hepatic growth effects of methylprednisolone, azathioprine, mycophenolic acid, and mizoribine. Transplantation 1993, 56, 219–221. [Google Scholar] [CrossRef]
- Motale, P.; Mall, A.; Spearman, C.W.; Lotz, Z.; Tyler, M.; Shepherd, E.; Kahn, D. The effect of mycophenolate mofetil on liver regeneration. Transplant. Proc. 2001, 33, 1054–1055. [Google Scholar] [CrossRef]
- Kirimlioglu, H.; Kirimlioglu, V.; Yilmaz, S.; Coban, S.; Türkmen, E.; Ara, C. Liver pathology and cell proliferation after calcineurin inhibitors and antiproliferative drugs following partial hepatectomy in rats. Transplant. Proc. 2006, 38, 622–626. [Google Scholar] [CrossRef] [PubMed]
- Tannuri, A.; Tannuri, U.; Coelho, M.; Mello, E.; Santos, N. Effects of Immunosuppressants on Hepatocyte Cell Mitosis During Liver Regeneration in Growing Animal Models of Partial Hepatectomy. Transplant. Proc. 2008, 40, 1641–1644. [Google Scholar] [CrossRef] [PubMed]
- Tannuri, U.; Tannuri, A.; Coelho, M.C.M.; Mello, E.S.; Dos Santos, N.A.S.R. Effect of the immunosuppressants on hepatocyte cells proliferation and apoptosis during liver regeneration after hepatectomy—Molecular studies. Pediatr. Transplant. 2008, 12, 73–79. [Google Scholar] [CrossRef] [PubMed]
- Demiray, M.; Kucuk, H.; Yildirim, M.; Barisik, N. No harmful effect of mycophenolate mofetil on liver regeneration: An experimental study. Transplant. Proc. 2012, 44, 1743–1746. [Google Scholar] [CrossRef]
- Azzi, J.R.; Sayegh, M.H.; Mallat, S.G. Calcineurin inhibitors: 40 years later, can’t live without…. J. Immunol. 2013, 191, 5785–5791. [Google Scholar] [CrossRef]
- Francavilla, A.; Todo, S.; Porter, K.A.; Barone, M.; Zeng, Q.; Starzl, T.E. Augmentation of rat liver regeneration by fk 506 compared with cyclosporin. Lancet 1989, 2, 1248–1249. [Google Scholar] [CrossRef]
- Tamura, F.; Masuhara, A.; Sakaida, I.; Fukumoto, E.; Nakamura, T.; Okita, K. FK506 promotes liver regeneration by suppressing natural killer cell activity. J. Gastroenterol. Hepatol. 1998, 13, 703–708. [Google Scholar] [CrossRef]
- Morii, Y.; Kawano, K.; Kim, Y.-I.; Aramaki, M.; Yoshida, T.; Kitano, S. Augmentative effect of cyclosporin A on rat liver regeneration: Influence on hepatocyte growth factor and transforming growth factor-beta(1). Eur. Surg. Res. 1999, 31, 399–405. [Google Scholar] [CrossRef]
- Francavilla, A.; Starzl, T.E.; Barone, M.; Zeng, Q.-H.; Porter, K.A.; Zeevi, A.; Markus, P.M.; Brink, M.R.M.V.D.; Todo, S. Studies on mechanisms of augmentation of liver regeneration by cyclosporine and FK. Hepatology 1991, 14, 140–143. [Google Scholar] [CrossRef]
- Alvira, L.G.; Herrera, N.; Salas, C.; Pereira, F.; Herrera, J.; Suárez-Massa, M.D.; Castillo-Olivares, J.L. Influence of cyclosporine on graft regeneration and function after liver transplantation: Trial in pigs. Transplant. Proc. 2002, 34, 315–316. [Google Scholar] [CrossRef]
- Karadeniz, E.; Ozbilgin, M.; Egeli, T.; Agalar, C.; Cevlik, A.D.; Aysal, A.; Ellidokuz, H.; Unek, T.; Astarcioglu, I. Assessment of effect of intraperitoneal tacrolimus on liver regeneration in major (70%) hepatectomy model after experimental pringle maneuver in rats. Transplant. Proc. 2019, 51, 1172–1179. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Perálvarez, M.; Guerrero, M.; Barrera, L.; Ferrín, G.; Álamo, J.M.; Ayllón, M.D.; Artacho, G.S.; Montero, J.L.; Briceño, J.; Bernal, C.; et al. Impact of early initiated everolimus on the recurrence of hepatocellular carcinoma after liver transplantation. Transplantation 2018, 102, 2056–2064. [Google Scholar] [CrossRef] [PubMed]
- Francavilla, A.; Carr, B.I.; Starzl, T.E.; Azzarone, A.; Carrieri, G.; Zeng, Q.-H. Effects of rapamycin on cultured hepatocyte proliferation and gene expression. Hepatology 1992, 15, 871–877. [Google Scholar] [CrossRef] [PubMed]
- Palmes, D.; Zibert, A.; Budny, T.; Bahde, R.; Minin, E.; Kebschull, L.; Hölzen, J.; Schmidt, H.; Spiegel, H.-U. Impact of rapamycin on liver regeneration. Virchows Arch. 2008, 452, n545–n557. [Google Scholar] [CrossRef] [PubMed]
- Fouraschen, S.M.; De Ruiter, P.E.; Kwekkeboom, J.; De Bruin, R.W.; Kazemier, G.; Metselaar, H.J.; Tilanus, H.W.; Van Der Laan, L.J.; De Jonge, J. mTOR signaling in liver regeneration: Rapamycin combined with growth factor treatment. World J. Transplant. 2013, 3, 36–47. [Google Scholar] [CrossRef] [PubMed]
- Saliba, F.; Duvoux, C.; Dharancy, S.; Dumortier, J.; Calmus, Y.; Gugenheim, J.; Kamar, N.; Salamé, E.; Neau-Cransac, M.; Vanlemmens, C.; et al. Early switch from tacrolimus to everolimus after liver transplantation: Outcomes at 2 years. Liver Transplant. 2019, 25, 1822–1832. [Google Scholar] [CrossRef] [PubMed]
- Jeng, L.-B.; Lee, S.-G.; Soin, A.S.; Lee, W.-C.; Suh, K.-S.; Joo, D.J.; Uemoto, S.; Joh, J.; Yoshizumi, T.; Yang, H.-R.; et al. Efficacy and safety of everolimus with reduced tacrolimus in living-donor liver transplant recipients: 12-month results of a randomized multicenter study. Am. J. Transplant. 2018, 18, 1435–1446. [Google Scholar] [CrossRef]
- Rupertus, K.; Dahlem, C.; Menger, M.D.; Schilling, M.K.; Kollmar, O. Rapamycin inhibits hepatectomy-induced stimulation of metastatic tumor growth by reduction of angiogenesis, microvascular blood perfusion, and tumor cell proliferation. Ann. Surg. Oncol. 2009, 16, 2629–2637. [Google Scholar] [CrossRef]
- Dar, W.A.; Sullivan, E.; Bynon, J.S.; Eltzschig, H.; Ju, C. Ischaemia reperfusion injury in liver transplantation: Cellular and molecular mechanisms. Liver Int. 2019, 39, 788–801. [Google Scholar] [CrossRef]
- Yagi, S.; Uemoto, S. Small-for-size syndrome in living donor liver transplantation. Hepatobiliary Pancreat. Dis. Int. 2012, 11, 570–576. [Google Scholar] [CrossRef]
- Huang, W.; Ma, K.; Zhang, J.; Qatanani, M.; Cuvillier, J.; Liu, J.; Dong, B.; Huang, X.; Moore, D.D. Nuclear receptor-dependent bile acid signaling is required for normal liver regeneration. Science 2006, 312, 233–236. [Google Scholar] [CrossRef] [PubMed]
- Bedogni, G.; Nobili, V.; Tiribelli, C. Epidemiology of fatty liver: An update. World J. Gastroenterol. 2014, 20, 9050–9054. [Google Scholar]

| Author | Published Year | Animal | Induction of Steatosis | Degree of Steatosis * | PHx | Evaluation of Liver Regeneration | Timing of Evaluation | Liver Regeneration | |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Zhang et al. [104] | 1999 | rats | MCDD for 4 weeks | Not mentioned | 68% | Liver weight, [3H]-thymidine incorporation | 24 h | Not impaired |
| 2 | Selzner et al. [105] | 2000 | rats | fa/fa rats, 20 weeks old | Severe | 70% | Liver weight, mitotic index, BrdU, PCNA | 24, 48, 96 h | Impaired |
| 3 | Rao et al. [106] | 2001 | rats | Choline-deficient diet for 4 weeks | Severe | 70% | Mitotic index, BrdU | 24, 36, 48, 72, 96 h | Not impaired |
| 4 | Yang et al. [107] | 2001 | mice | ob/ob mice, 8-10 weeks old | Severe | 70% | BrdU, PCNA | 24, 36 h | Impaired |
| 5 | Torbenson et al. [108] | 2002 | mice | ob/ob mice, 10 weeks old | Moderate | 70% | BrdU | 24, 36 h | Impaired |
| 6 | Picard et al. [109] | 2002 | rats | fa/fa rats, 13 weeks old | Moderate | 70% | Liver weight, BrdU, PCNA(WB) | 24 h | Impaired |
| Orotic acid for 4 weeks | Severe | Not impaired | |||||||
| MCDD | Severe | Not impaired | |||||||
| 7 | Yamauchi et al. [110] | 2003 | mice | db/db mice, 10 weeks old | Severe | 70% | Liver weight, mitotic index, BrdU, PCNA | 24, 48, 72, 120, 168, 240 h | Impaired |
| 8 | DeAngelis et al. [111] | 2005 | mice | High-fat diet, for 8-12 weeks | Severe | 70% | Liver weight, BrdU | 12, 24, 36, 48, 60, 72, 96, 120 h | Impaired |
| 9 | Tanoue et al. [112] | 2011 | rats | High-fructose diet for 4 weeks | Mild | 70% | Liver weight, PCNA | 24, 72, 168 h | Impaired |
| High-fat diet for 4 weeks | Severe | Not impaired | |||||||
| 10 | Sydor et al. [113] | 2013 | mice | Western diet for 6 weeks | Mild | 70% | Ki67, PHH3 | 24, 48, 168 h | Enhanced |
| 11 | Collin de l’Hortet et al. [114] | 2014 | mice | ob/ob mice, 13-14 weeks old | Severe | 55% | Liver weight, mitotic index, BrdU, PHH3 | 32, 44, 56, 68 h | Impaired |
| MCDD for 5 weeks | Severe | Delayed | |||||||
| 12 | Zimmers et al. [115] | 2017 | mice | High-fat diet for 11-13 weeks | Not mentioned | 70% and 80% | Liver weight, BrdU, PCNA(WB) | 6, 24, 48, 72, 96, 120 h | Impaired |
| 13 | Valdecantos et al. [116] | 2017 | mice | MCDD for 3 weeks § | Moderate | 70% | Liver weight, BrdU, PCNA(WB) | 48, 336 h | Impaired ‡ |
| High fat diet for 13 weeks § | Mild | Impaired |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yagi, S.; Hirata, M.; Miyachi, Y.; Uemoto, S. Liver Regeneration after Hepatectomy and Partial Liver Transplantation. Int. J. Mol. Sci. 2020, 21, 8414. https://doi.org/10.3390/ijms21218414
Yagi S, Hirata M, Miyachi Y, Uemoto S. Liver Regeneration after Hepatectomy and Partial Liver Transplantation. International Journal of Molecular Sciences. 2020; 21(21):8414. https://doi.org/10.3390/ijms21218414
Chicago/Turabian StyleYagi, Shintaro, Masaaki Hirata, Yosuke Miyachi, and Shinji Uemoto. 2020. "Liver Regeneration after Hepatectomy and Partial Liver Transplantation" International Journal of Molecular Sciences 21, no. 21: 8414. https://doi.org/10.3390/ijms21218414
APA StyleYagi, S., Hirata, M., Miyachi, Y., & Uemoto, S. (2020). Liver Regeneration after Hepatectomy and Partial Liver Transplantation. International Journal of Molecular Sciences, 21(21), 8414. https://doi.org/10.3390/ijms21218414





