Developing a Physical Activity Intervention Strategy for Pregnant Women in Buffalo City Municipality, South Africa: A Study Protocol
Abstract
:1. Introduction
2. Research Questions
- What are the patterns and correlates of PA of women during pregnancy?
- What are the beliefs and sources of information about PA and exercise of women during pregnancy?
- What are the perceived benefits of PA and exercise participation of women during pregnancy?
- What are the barriers to PA and exercise participation of women during pregnancy?
- What knowledge and attitudes do pregnant women have about PA and exercise?
- What beliefs, knowledge and practices do healthcare providers have toward PA and exercise participation of women during pregnancy? Do women speak to their healthcare providers about PA and get recommendations? Do healthcare providers prescribe PA restrictions or choose to restrict activity during prenatal sessions?
- What context-specific intervention strategy would be relevant to enhance the understanding and promotion of PA and exercise, and to mitigate the barriers associated with PA and exercise participation during pregnancy among women in Buffalo City Municipality?
- How valid would the developed physical activity intervention strategy be in the promotion of physical activity and exercise among pregnant women in Buffalo City Municipality?
3. Theoretical Framework: Theory of Planned Behaviour
4. Problem Statement
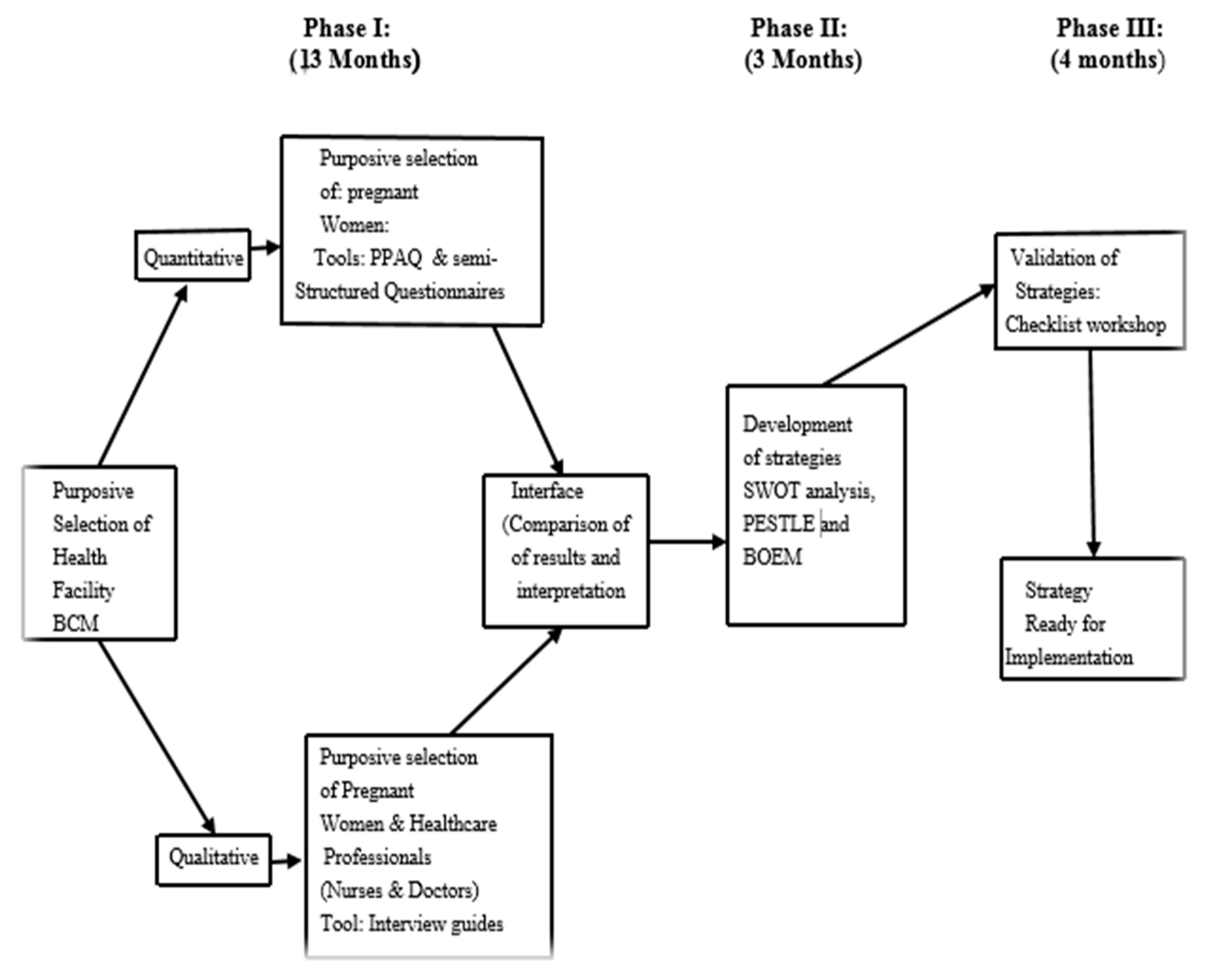
5. Methods and Designs
5.1. Phase I (Empirical Investigations)
- To assess the physical activity patterns of pregnant women and to verify what characteristics (age, residential status, race, marital status, education, employment status, religion, social support, smoking, alcohol use, parity, mode of pregnancy delivery, PA advice and pregravid weight status) are related to physical activity.
- To examine the beliefs and sources of information about PA and exercise of women during pregnancy.
- To examine the perceived benefits of PA and exercise of women during pregnancy.
- To examine the barriers to PA and exercise of women during pregnancy.
- To assess the knowledge and attitudes about PA and exercise of women during pregnancy.
- To explore the beliefs, knowledge and practices of healthcare providers toward PA and exercise participation during pregnancy.
5.2. Phase II (Intervention Strategy)
- To design and develop intervention strategies to enhance the understanding and promotion of PA and exercise, particularly during pregnancy, and to mitigate the barriers associated with PA and exercise participation of women during pregnancy.
5.3. Phase III (Validation of Intervention Strategy)
- To validate the intervention strategies to promote participation of PA and exercise participation of women during pregnancy.
6. Study Setting
7. Participant Recruitment and Study Population
7.1. Pregnant Women
- “Persistent excessive shortness of breath
- Severe chest pain
- Regular and painful uterine contractions
- Vaginal bleeding
- Persistent loss of fluid from the vagina indicating rupture of the membranes
- Persistent dizziness or faintness that does not resolve on rest”
7.2. Healthcare Providers
8. Data Collection Instruments
8.1. Quantitative Data Collection
8.1.1. Demographic, Obstetric and Lifestyle Information
8.1.2. Outcome Measure: Physical Activity
8.1.3. Sample Size
8.2. Qualitative Data Collection
8.2.1. Pregnant Women
8.2.2. Healthcare Providers
- Knowledge on prenatal PA, particularly the American College of Obstetricians and Gynaecologists (ACOG) guidelines and recommendation
- Counselling on general aspects of PA (benefits, contraindications, types of PA or exercises, intensity, duration, types of antenatal exercises or activities)
- Barriers and facilitators for PA
- Pregnant women’s concerns about PA
- Prescription of activity restriction
8.3. Data Analysis
8.3.1. Quantitative
8.3.2. Qualitative
9. Phase II: Development of a Physical Activity Intervention Strategy
10. Phase III: Validation of the Developed Intervention Strategy
10.1. Delphi Technique
10.2. Key Stakeholder Consultation
11. Ethics Approval and Consent to Participate
12. Discussion
13. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- World Health Organisation. World Health Statistics 2010. Available online: http://www.who.int/whosis/whostat/2010/en/ (accessed on 29 December 2018).
- Watson, E.D.; Norris, S.A.; Draper, C.E.; Jones, R.A.; van Poppel, M.N.M.; Micklesfield, L.K. “Just because you’re pregnant, doesn’t mean you’re sick!” A qualitative study of beliefs regarding physical activity in black South African women. BMC Pregnancy Childbirth 2016, 16, 174. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, I.M.; Shiroma, E.J.; Lobelo, F.; Puska, P.; Blair, S.N.; Katzmarzyk, P.T. Effect of physical inactivity on major non-communicable diseases worldwide: An analysis of burden of disease and life expectancy. Lancet 2012, 380, 219–229. [Google Scholar] [CrossRef] [Green Version]
- Ding, D.; Lawson, K.D.; Kolbe-Alexander, T.L.; Finkelstein, E.A.; Katzmarzyk, P.T.; van Mechelen, W.; Pratt, M. The economic burden of physical inactivity: A global analysis of major non-communicable diseases. Lancet 2016, 388, 1311–1324. [Google Scholar] [CrossRef]
- World Health Organization. Global Action Plan on Physical Activity 2018–2030: More Active People for a Healthier World. Geneva: Licence: CC BY-NC-SA 3.0 IGO. 2018. Available online: file:///C:/Users/home/Downloads/9789241514187-eng.pdf (accessed on 13 January 2020).
- Todorovic, J.; Terzic-Supic, Z.; Bjegovic-Mikanovic, V.; Piperac, P.; Dugalic, S.; Gojnic-Dugalic, M. Factors Associated with the Leisure-Time Physical Activity (LTPA) during the First Trimester of the Pregnancy: The Cross-Sectional Study among Pregnant Women in Serbia. Int. J. Environ. Res. Public Health 2020, 17, 1366. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- da Silva, S.G.; Ricardo, L.I.; Evenson, K.R.; Hallal, P.C. Leisure time physical activity in pregnancy and maternal-child health: A systematic review and meta-analysis of randomized controlled trials and cohort studies. Sports Med. 2017, 47, 295–317. [Google Scholar] [CrossRef]
- Yin, Y.; Huang, Y.; Liu, X.; Luo, B. Assessment of physical activity status among pregnant women in southwestern China. Front. Nurse 2019, 6, 135–141. [Google Scholar] [CrossRef] [Green Version]
- Gebregziabher, D.; Berhe, H.; Kassa, M.; Berhanie, E. Level of physical activity and associated factors during pregnancy among women who gave birth in Public Zonal Hospitals of Tigray. BMC Res. Notes 2019, 12, 454. [Google Scholar] [CrossRef] [Green Version]
- Hailemariam, T.T.; Gebregiorgis, Y.S.; Gebremeskel, B.F.; Haile, T.G.; Spitznagle, T.M. Physical activity and associated factors among pregnant women in Ethiopia: Facility-based cross-sectional study. BMC Pregnancy Childbirth 2020, 20, 92. [Google Scholar] [CrossRef] [Green Version]
- Adeniyi, A.F.; Ogwumike, O.O.; Osinike, C.I. Physical activity and energy expenditure: Findings from the Ibadan pregnant women’s survey. Afr. J. Reprod. Health 2014, 18, 117–126. [Google Scholar]
- Lawan, A.; Awotidebe, A.W.; Oyeyemi, A.L.; Rufa, A.A.; Oyeyemi, A.Y. Relationship between physical activity and health related quality of life among pregnant women. Afr. J. Reprod. Health 2018, 22, 80–89. [Google Scholar]
- Gjestland, K.; Bo, K.; Owe, K.M.; Eberhard-Gran, M. Do pregnant women follow exercise guidelines? Prevalence data among 3482 women, and prediction of low-back pain, pelvic girdle pain and depression. Br. J. Sports Med. 2012, 47, 515–520. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- International Weight Management in Pregnancy (i-WIP) Collaborative Group. Effect of diet and physical activity based interventions in pregnancy on gestational weight gain and pregnancy outcomes: Meta-analysis of individual participant data from randomised trials. Br. Med. J. 2017, 23, 358. [Google Scholar]
- Catov, J.M.; Parker, C.B.; Gibbs, B.B.; Bann, C.M.; Carper, B.; Silver, R.M.; Simhan, H.N.; Parry, S.; Chung, J.H.; Haas, D.M.; et al. Patterns of leisure-time physical activity across pregnancy and adverse pregnancy outcomes. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 68–78. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mizgier, M.; Mruczyk, K.; Jarzabek-Bielecka, G.; Jeszka, J. The impact of physical activity during pregnancy on maternal weight and obstetric outcomes. Ginekol. Pol. 2018, 89, 80–88. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pastorino, S.; Bishop, T.; Crozier, S.R.; Granström, C.; Kordas, K.; Küpers, L.K.; O’Brien, E.C.; Polanska, K.; Sauder, K.A.; Zafarmand, M.H.; et al. Associations between maternal physical activity in early and late pregnancy and offspring birth size: Remote federated individual level meta-analysis from eight cohort studies. BJOG 2019, 126, 459–470. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nguyen, C.L.; Pham, N.M.; Lee, A.H.; Nguyen, P.T.H.; Chu, T.K.; Ha, A.V.V.; Duong, D.V.; Duong, T.H.; Binns, C.W. Physical activity during pregnancy is associated with a lower prevalence of gestational diabetes mellitus in Vietnam. Acta Diabetol. 2018, 55, 955–962. [Google Scholar] [CrossRef] [PubMed]
- Dipietro, L.; Evenson, K.R.; Bloodgood, B.; Sprow, K.; Troiano, R.P.; Piercy, K.L.; Vaux-Bjerke, A.; Powell, K.E. Benefits of Physical Activity during Pregnancy and Postpartum: An Umbrella Review. Med. Sci. Sports Exerc. 2019, 51, 1292–1302. [Google Scholar] [CrossRef]
- Du, M.C.; Ouyang, Y.Q.; Nie, X.F.; Huang, Y.; Redding, S.R. Effects of physical exercise during pregnancy on maternal and infant outcomes in overweight and obese pregnant women: A meta-analysis. Birth 2018, 46, 211–221. [Google Scholar] [CrossRef]
- Walasik, I.; Kwiatkowska, K.; Szymusik, I. Physical Activity Patterns among 9000 Pregnant Women in Poland: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2020, 17, 1771. [Google Scholar] [CrossRef] [Green Version]
- Davenport, M.H.; Ruchat, S.M.; Sobierajski, F.; Poitras, V.J.; Gray, C.E.; Yoo, C.; Skow, R.J.; Garcia, A.J.; Barrowman, N.; Meah, V.L.; et al. Impact of prenatal exercise on maternal harms, labour and delivery outcomes: A systematic review and meta-analysis. Br. J. Sports Med. 2019, 53, 99–107. [Google Scholar] [CrossRef]
- Collings, P.J.; Farrar, D.; Gibson, J.; West, J.; Barber, S.E.; Wright, J. Associations of pregnancy physical activity with maternal cardiometabolic health, neonatal delivery outcomes and body composition in a Biethnic Cohort of 7305 Mother–Child Pairs: The Born in Bradford Study. Sports Med. 2020, 50, 615–628. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Collings, P.J.; Farrar, D.; Gibson, J.; West, J.; Barber, S.E.; Wright, J. Maternal Physical Activity and Neonatal Cord Blood Lipid Levels: Findings from a Prospective Pregnancy Cohort. J. Phys. Act. Health. 2020, 17, 236–241. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Davenport, M.H.; Meah, V.L.; Ruchat, S.M.; Davies, G.A.; Skow, R.J.; Barrowman, N.; Adamo, K.B.; Poitras, V.J.; Gray, C.E.; Garcia, A.J.; et al. Impact of prenatal exercise on neonatal and childhood outcomes: A systematic review and meta-analysis. Br. J. Sports Med. 2018, 52, 1386–1396. [Google Scholar] [CrossRef] [PubMed]
- Aune, D.; Schlesinger, S.; Henriksen, T.; Saugstad, O.; Tonstad, S. Physical activity and the risk of preterm birth: A systematic review and meta-analysis of epidemiological studies. BJOG Int. J. Obstet. Gynaecol. 2017, 124, 1816–1826. [Google Scholar] [CrossRef] [PubMed]
- Takami, M.; Tsuchida, A.; Takamori, A.; Aoki, S.; Ito, M. Effects of physical activity during pregnancy on preterm delivery and mode of delivery: The Japan Environment and Children’s Study, birth cohort study. PLoS ONE 2018, 13, e02066160. [Google Scholar] [CrossRef] [Green Version]
- Davenport, M.H.; McCurdy, A.P.; Mottola, M.F.; Skow, R.J.; Meah, V.L.; Poitras, V.J.; Jaramillo Garcia, A.; Gray, C.E.; Barrowman, N.; Riske, L.; et al. Impact of prenatal exercise on both prenatal and postnatal anxiety and depressive symptoms: A systematic review and meta-analysis. Br. J. Sports Med. 2018, 52, 1376–1385. [Google Scholar] [CrossRef]
- Taylor, P.; Ko, Y.; Chen, C.; Lin, P. Physical activities during pregnancy and type of delivery in nulliparae. Eur. J. Sport Sci. 2016, 16, 374–380. [Google Scholar]
- Rajabi, A.; Maharlouei, N.; Rezaianzadeh, A. Physical activities (exercises or choreses) during pregnancy and mode of delivery in nulliparous women: A prospective cohort study. Taiwan J. Obstet. Gynecol. 2018, 57, 18–22. [Google Scholar] [CrossRef]
- Wiebe, H.W.; Boulé, N.G.; Chari, R.; Davenport, M.H. The Effect of Supervised Prenatal Exercise on Fetal Growth. Obstet. Gynecol. 2015, 125, 1185–1194. [Google Scholar] [CrossRef]
- Ramirez-Velez, R.; Aguilar de Plata, A.C.; Escudero, M.M.; Echeverry, I.; Ortega, J.G.; Salazar, B.; José Rey, J.; Hormig, C.; López-Jaramillo, P. Influence of regular aerobic exercise on endothelium-dependent vasodilation and cardiorespiratory fitness in pregnant women. J. Obstet. Gynaecol. Res. 2011, 37, 1601–1608. [Google Scholar] [CrossRef]
- American College of Obstetricians and Gynaecologists. Physical activity and exercise during pregnancy and the postpartum period. Committee Opinion No. 804. Obstet. Gynaecol. 2020, 135, e178–e188. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baker, J.H.; Rothenberger, S.D.; Kline, C.E.; Okun, M.L. Exercise during Early Pregnancy is Associated with Greater Sleep Continuity. Behav. Sleep Med. 2018, 16, 482–493. [Google Scholar] [CrossRef] [PubMed]
- Gobierno Vasco. Guía del Embarazo, Preconcepción, Parto y Puerperio Saludable; Basque Government: Vitoria-Gasteiz, Spain, 2017; p. 48.
- Cid, M.; González, M. Potential benefits of physical activity during pregnancy for the reduction of gestational diabetes prevalence and oxidative stress. Early Hum. Dev. 2016, 94, 57–62. [Google Scholar] [CrossRef] [PubMed]
- Vargas-terrones, M.; Barakat, R.; Santacruz, B.; Fernandez-buhigas, I.; Mottola, M.F. Physical exercise programme during pregnancy decreases perinatal depression risk: A randomised controlled trial. Br. J. Sports Med. 2018, 53, 348–353. [Google Scholar] [CrossRef] [PubMed]
- Szegda, K.; Bertone-johnson, E.R.; Pekow, P.; Powers, S.; Markenson, G.; Dole, N.; Chasan-Taber, L. Physical activity and depressive symptoms during pregnancy among Latina women: A prospective cohort study. BMC Pregnancy Childbirth 2018, 18, 252–263. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sinclair, I.; St-Pierre, M.; Elgbeili, G.; Bernard, P.; Vaillancourt, C.; Gagnon, S.; Dancause, K.N. Psychosocial stress, sedentary behavior, and physical activity during pregnancy among canadian women: Relationships in a diverse cohort and a nationwide sample. Int. J. Environ. Res. Public Health 2019, 16, 5150. [Google Scholar] [CrossRef] [Green Version]
- Puchalski, S. Physical activity: Utilizing guidelines to promote health among pregnant women. J. Pregnancy Reprod. 2017, 1, 1–3. [Google Scholar] [CrossRef] [Green Version]
- Patrícia, V.; De Sousa, S.; Cury, A.; Eufrásio, L.S. The influence of gestational trimester, physical activity practice and weight gain on the low back and pelvic pain intensity in low risk pregnant women. J. Back Musculoskelet. Rehabil. 2019, 32, 671–676. [Google Scholar]
- Thorell, E.; Kristiansson, P. Pregnancy related back pain, is it related to aerobic fitness? A longitudinal cohort study. BMC Pregnancy Childbirth 2012, 12, 30. [Google Scholar] [CrossRef]
- Davenport, M.H.; Marchand, A.A.; Mottola, M.F.; Poitras, V.J.; Gray, C.E.; Jaramillo Garcia, A.; Barrowman, N.; Sobierajski, F.; James, M.; Meah, V.L.; et al. Exercise for the prevention and treatment of low back, pelvic girdle and lumbopelvic pain during pregnancy: A systematic review and meta-analysis. Br. J. Sports Med. 2019, 53, 90–98. [Google Scholar] [CrossRef] [Green Version]
- Price, B.B.; Amini, S.B.; Kappeler, K. Exercise in pregnancy effect on fitness and obstetric outcomes. Aust. Fam. Physician 2014, 43, 541–542. [Google Scholar]
- Artal, R. The role of exercise in reducing the risks of gestational diabetes mellitus in obese women. Best Pract. Res. Clin. Obstet. Gynaecol. 2015, 29, 123–132. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, P.T.H.; Binns, C.W.; Nguyen, C.L.; Van Ha, A.V.; Chu, K.T.; Duong, D.V.; Do, D.V.; Lee, A.H. Physical Activity during pregnancy is associated with improved breastfeeding outcomes: A prospective Cohort Study. Int. J. Environ. Res. Public Health 2019, 16, 1740. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Di Fabio, D.R.; Blomme, C.K.; Smith, K.M.; Welk, G.J.; Campbell, C.G. Adherence to physical activity guidelines in mid-pregnancy does not reduce sedentary time: An observational study. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 27. [Google Scholar] [CrossRef] [Green Version]
- Hayes, L.; Mcparlin, C.; Kinnunen, T.; Poston, L.; Robso, S.C.; Bell, R.; Unbeat Consortium. Change in level of physical activity during pregnancy in obese women: Findings from the UPBEAT pilot trial. BMC Pregnancy Childbirth 2015, 15, 52. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bauer, C.; Graf, C.; Platschek, A.M.; Struder, H.K.; Ferrari, N. Reasons, motivational factors, and perceived personal barriers to engagement in physical activity during pregnancy vary within the BMI classes: The Prenatal Prevention Project Germany. J. Phys. Act. Health 2018, 15, 204–211. [Google Scholar] [CrossRef]
- Schmidt, T.; Heilmann, T.; Savelsberg, L.; Maass, N.; Weisser, B.; Eckmann-Scholz, C. Physical exercise during pregnancy—How active are pregnant women in Germany and how well informed? Geburtshilfe Frauenheilkd 2017, 77, 508–515. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Y.; Dong, S.; Zuo, J.; Hu, X.; Zhang, H.; Zhao, Y. Physical activity level of urban pregnant women in Tianjin, China: A cross-sectional study. PLoS ONE 2014, 9, e109624. [Google Scholar] [CrossRef] [Green Version]
- Padmapriya, N.; Shen, L.; Soh, S.E.; Shen, Z.; Kwek, K.; Godfrey, K.M.; Gluckman, P.D.; Chong, Y.S.; Saw, S.M.; Müller-Riemenschneide, F. Physical activity and sedentary behaviour patterns before and during pregnancy in a multi-ethnic sample of Asian women in Singapore. Matern. Child Health J. 2015, 19, 2523–2535. [Google Scholar] [CrossRef]
- Watson, E.D.; Van Poppel, M.N.M.; Jones, R.A.; Norris, S.A.; Micklesfield, L.K. Are South African mothers moving? Patterns and correlates of physical activity and sedentary behaviour in pregnant black South African women. J. Phys. Act. Health 2017, 14, 329–335. [Google Scholar] [CrossRef]
- Nascimento, S.L.; Surita, F.G.; Godoy, A.C.; Kasawara, K.T.; Morais, S.S. Physical activity patterns and factors related to exercise during pregnancy: A cross sectional study. PLoS ONE 2015, 10, e0128953. [Google Scholar]
- Mendinueta, A.; Esnal, H.; Arrieta, H.; Arrue, M.; Urbieta, N.; Ubillos, I.; Whitworth, K.W.; Delclòs-Alió, X.; Vich, G.; Ibarluzea, J. What Accounts for Physical Activity during Pregnancy? A Study on the Sociodemographic Predictors of Self-Reported and Objectively Assessed Physical Activity during the 1st and 2nd Trimesters of Pregnancy. Int. J. Environ. Res. Public Health 2020, 17, 2517. [Google Scholar] [CrossRef]
- Brunette, E.L.; Kotze, J.; Wood, P.S.; Du Toit, P.J.; Grant, C.C. An epidemiological study of physical activity patterns and weight gain in physically active and sedentary pregnant women in Tshwane, South Africa. Afr. J. Phy. Health Edu. Recrea Dance 2012, 18 (Suppl. 1), 132–143. [Google Scholar]
- Muzigaba, M.; Kolbe-Alexander, T.L.; Wong, F. The perceived role and influencers of physical activity among pregnant women from low socioeconomic status communities in South Africa. J. Phys. Act. Health 2014, 11, 1276–1283. [Google Scholar] [CrossRef] [PubMed]
- Most, J.; Dervis, S.; Haman, F.; Adamo, K.B.; Redman, L.M. Energy Intake Requirements in Pregnancy. Nutrients 2019, 11, 1812. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Flannery, C.; McHugh, S.; Anaba, A.E.; Clifford, E.O.; Riordan, M.; Kenny, L.C.; McAuliffe, F.M.; Kearney, P.; Byrne, M. Enablers and barriers to physical activity in overweight and obese pregnant women: An analysis informed by the theoretical domains framework and COM-B model. BMC Pregnancy Childbirth 2018, 18, 178. [Google Scholar] [CrossRef] [PubMed]
- Sytsma, T.T.; Zimmerman, K.P.; Manning, J.B.; Jenkins, S.M.; Nelson, N.C.; Clark, M.M.; Boldt, K.; Borowski, K.S. Perceived Barriers to Exercise in the First Trimester of Pregnancy. J. Perinat. Educ. 2018, 27, 198–206. [Google Scholar] [CrossRef]
- Da Costa, D.; Ireland, K. Perceived benefits and barriers to leisure-time physical activity during pregnancy in previously inactive and active women. Women Health 2013, 53, 185–202. [Google Scholar] [CrossRef]
- Fathnezhad-Kazemi, A.; Hajian, S. Factors influencing the adoption of health promoting behaviors in overweight pregnant women: A qualitative study. BMC Pregnancy Childbirth 2019, 19, 43. [Google Scholar] [CrossRef]
- White, E.; Pfeifer, K.; Holzman, C.; Pivarnik, J. Motives for and barriers to exercising across trimesters of pregnancy in health club members. Hum. Mov. 2020, 21, 21–30. [Google Scholar] [CrossRef] [Green Version]
- Saligheh, M.; McNamara, B.; Rooney, R. Perceived barriers and enablers of physical activity in postpartum women: A qualitative approach. BMC Pregnancy Childbirth 2016, 16, 131. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Babbar, S.; Chauhan, S.P. Exercise and yoga during pregnancy: A survey. J. Matern. Fetal Neonatal Med. 2015, 28, 431–435. [Google Scholar] [CrossRef] [PubMed]
- Makinde, O.; Adeyemo, F.; Ogundele, B. Perception of pregnant mothers attending antenatal clinic on usefulness of prenatal exercise in Osogbo, Osun state, Nigeria. J. Health Sci. 2014, 8, 229–239. [Google Scholar]
- Put, W.; Chuan, S.; Chan, L. Physical activity in pregnancy: Attitudes and practices of Hong Kong Chinese women. Hong Kong J. Gynaecol. Obstet. Midwifery 2015, 15, 138–147. [Google Scholar]
- Mbada, C.E.; Adebayo, O.E.; Adeyemi, A.B.; Arije, O.O.; Dada, O.O.; Akinwande, O.A.; Awotidebe, T.O.; Alonge, I.B. Knowledge and attitude of Nigerian pregnant women towards antenatal exercise: A cross sectional survey. Obstet. Gynecol. 2014, 1, 8. [Google Scholar] [CrossRef] [PubMed]
- Chasan-Taber, L. Physical activity and dietary behaviours associated with weight gain and impaired glucose tolerance among pregnant Latinas. Adv. Nutr. 2012, 3, 108–118. [Google Scholar] [CrossRef] [Green Version]
- Ojukwu, C.P.; Anekwu, E.M.; Okemuo, A.J.; Nwabueze, J.O.; John, D.O.; Ezugwu, U.A.; Uchenwoke, C.I. Antenatal exercise practices: Associated factors and correlation with antenatal quality of life. J. Appl. Life Sci. Int. 2018, 18, 1–9. [Google Scholar]
- Leppanen, M.; Aittasalo, M.; Raitanen, J.; Kinnunen, T.I.; Kujala, U.M.; Luoto, R. Physical activity during pregnancy: Predictors of change, perceived support and barriers among women at increased risk of gestational diabetes. Matern. Child Health J. 2014, 18, 2158–2166. [Google Scholar] [CrossRef]
- Harrison, A.L.; Taylor, N.F.; Nora Shields, N.; Frawley, H.C. Attitudes, barriers and enablers to physical activity in pregnant women: A systematic review. Physiotherapy 2018, 64, 24–32. [Google Scholar] [CrossRef]
- Sujindra, E.; Bupathy, A.; Suganya, A.; Praveena, R. Knowledge, attitude, and practice of exercise during pregnancy among antenatal mothers. Int. J. Edu. Psychol. Res. 2018, 1, 234–237. [Google Scholar] [CrossRef]
- Halse, R.E.; Wallman, K.E.; Dimmock, J.A.; Newnham, J.P.; Guelfi, K.J. Home-based exercise improves fitness and exercise attitude and intention in women with GDM. Med. Sci. Sports Exerc. 2015, 47, 1698–1704. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alvarado, M.; Murphy, M.M.; Guell, C. Barriers and facilitors to physical activity amongst overweight and obese women in an Afro-Caribbean population: A qualitative study. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 97. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Whitaker, K.M.; Wilcox, S.; Liu, J.; Blair, S.N.; Pate, R.R. Pregnant women’s perceptions of weight gain, physical activity, and nutrition using Theory of Planned Behaviour constructs. J. Behav. Med. 2016, 39, 41–54. [Google Scholar] [CrossRef] [PubMed]
- Watson, E.D.; Brage, S.; White, T.; Westgate, K.; Norris, S.A.; Van Poppel, M.N.M.; Micklesfield, L.K. The influence of objectively measured physical activity during pregnancy on maternal and birth outcomes in urban black South African women. Matern. Child Health J. 2018, 22, 1190–1199. [Google Scholar] [CrossRef]
- Herold, F.; Müller, P.; Gronwald, T.; Müller, N.G. Dose-response matters!—A perspective on the exercise prescription in exercise-cognition research. Front. Psychol. 2019. [Google Scholar] [CrossRef] [Green Version]
- Gronwald, T.; Budde, H. Commentary: Physical Exercise as Personalized Medicine for Dementia Prevention? Front. Physiol. 2019, 10, 726. [Google Scholar] [CrossRef] [Green Version]
- Herold, F.; Törpel, A.; Schega, L.; Müller, N.G. Functional and/or structural brain changes in response to resistance exercises and resistance training lead to cognitive improvements—A systematic review. Eur. Rev. Aging Phys. Act. 2019, 16, 1676. [Google Scholar] [CrossRef]
- Godin, G. Theories of reasoned action and planned behaviour: Usefulness for exercise promotion. Med. Sci. Sports Exerc. 1994, 26, 1391–1394. [Google Scholar] [CrossRef]
- Ajzen, I. The theory of planned behaviour: Reactions and reflections. Psychol. Health 2011, 26, 1113–1127. [Google Scholar] [CrossRef]
- Downs, D.S.; Hausenblas, H.A. Exercising for two: Examining pregnant women’s second trimester exercise intention and behaviour using the framework of the theory of planned behaviour. Women’s Health Issues 2003, 13, 222–228. [Google Scholar] [CrossRef]
- Choi, J.; Lee, J.H.; Vittinghoff, E.; Fukuoka, Y. mHealth Physical Activity Intervention: A randomized pilot study in physically inactive pregnant women. Matern. Child Health J. 2016, 20, 1091–1101. [Google Scholar] [CrossRef] [PubMed]
- Bisson, M.; Croteau, J.; Guinhouya, B.C.; Bujold, E.; Audibert, F.; Fraser, W.D.; Marc, I. Physical activity during pregnancy and infant’s birth weight: Results from the 3D Birth Cohort. BMJ Open Sport Exerc. Med. 2017, 3, e000242. [Google Scholar] [CrossRef] [PubMed]
- Laredo-Aguilera, J.A.; Gallardo-Bravo, M.; Rabanales-Sotos, J.A.; Cobo-Cuenca, A.I.; Carmona-Torres, J.M. Physical Activity Programs during Pregnancy Are Effective for the Control of Gestational Diabetes Mellitus. Int. J. Environ. Res. Public Health 2020, 17, 6151. [Google Scholar] [CrossRef] [PubMed]
- Poyatos-León, R.; Sanabria-Martínez, G.; García-Prieto, J.C.; Álvarez-Bueno, C.; Pozuelo-Carrascosa, D.P.; Cavero-Redondo, I.; García-Hermoso, A.; Gómez-Cantarino, S.; Garrido-Migue, M.; Martínez-Vizcaíno, V. A follow-up study to assess the determinants and consequences of physical activity in pregnant women of Cuenca, Spain. BMC Public Health 2016, 16, 437. [Google Scholar] [CrossRef] [Green Version]
- Mishra, S.; Kishore, S. Effect of physical activity during pregnancy on gestational diabetes. Indian J. Endocrinol. Metabol. 2018, 22, 866. [Google Scholar] [CrossRef]
- Fantuzzi, G.; Righi, E.; Aggazzotti, G. A case-control study on leisure time physical activity (LTPA) during the last three months of pregnancy and foetal outcomes in Italy. Health 2016, 8, 133–143. [Google Scholar] [CrossRef] [Green Version]
- Statistics South Africa. South African Statistics. South Africa, 1–190; 2011. Available online: http://www.statssa.gov.za/publications/SAStatistics/SAStatistics2011.pdf (accessed on 24 August 2020).
- Eastern Cape Socio Economic Consultative Council. Buffalo City Metro Municipality Socio Economic Review and Outlook. 2017. Available online: https://www.ecsecc.org/documentrepository/informationcentre/buffalo-city-metro-municipality_44557.pdf (accessed on 18 December 2018).
- Mottola, M.; Davenport, M.; Ruchat, S.; Davies, G.; Poitras., V.; Gray., C. Canadian guideline for physical activity throughout pregnancy. Br. J. Sports Med. 2019, 40, 1549–1559. [Google Scholar]
- Institute of Medicine and National Research Council. Weight Gain during Pregnancy: Reexamining the Guidelines; The National Academies Press: Washington, DC, USA, 2009. [Google Scholar]
- Chasan-Taber, L.; Schmidt, M.D.; Roberts, D.E.; Hosmer, D.; Markenson, G.; Freedson, P.S. Development and validation of a Pregnancy Physical Activity Questionnaire. Med. Sci. Sports Exerc. 2004, 36, 1750–1760. [Google Scholar] [CrossRef]
- Chen, K.Y.; Janz, K.F.; Zhu, W.; Brychta., R.J. Redefining the roles of sensors in objective physical activity monitoring. Med. Sci. Sports Exerc. 2012, 44 (Suppl. 1), S13–S23. [Google Scholar] [CrossRef] [Green Version]
- Chandonnet, N.; Saey, D.; Almeras, N.; Marc, I. French Pregnancy Physical Activity Questionnaire compared with an accelerometer cut point to classify physical activity among pregnant obese women. PLoS ONE 2012, 7, e38818. [Google Scholar] [CrossRef] [Green Version]
- Sarmah, H.K.; Hazarika, B.B.; Choudhury, G. An investigation on effect of bais on determination of sample size on the basis of data related to the students of schools of Guwahati. Int. J. Appl. Math Stat. Sci. 2013, 2, 33–48. [Google Scholar]
- Farmer, T.; Robinson, K.; Elliott, S.J.; Eyles, J. Developing and implementing a triangulation protocol for qualitative health research. Qual. Health Res. 2006, 16, 377–394. [Google Scholar] [CrossRef] [PubMed]
- O’Cathain, A.; Murphy, E.; Nicholl, J. Three techniques for integrating data in mixed methods studies. Br. Med. J. 2010, 341, c4587. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Healthy Pregnant or Postpartum Women. 2015. Available online: cdc.gov/physicalactivity/basics/pregnancy/index.htm (accessed on 17 July 2020).
- Creswell, J.W. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches, 4th ed.; Sage Publication Inc.: Thousand Oaks, CA, USA, 2014. [Google Scholar]
- Wehmeier, S.; Mcintosh, C.; Turnbull, J.; Ashby., M. Oxford Advanced Learner’s Dictionary, International Student Edition, 7th ed.; Oxford University Press: Oxford, UK, 2010. [Google Scholar]
- Gurel, E.; Tat, M. SWOT Analysis: A theoretical review. J. Int. Soc. Res. 2017, 10, 994–1006. [Google Scholar] [CrossRef]
- Nunu, W.J.; Makhado, L.; Mabunda, J.T.; Lebese, R.T. Strategies to facilitate safe sexual practices in adolescents through integrated health systems in selected districts of Zimbabwe: A mixed method study protocol. Reprod. Health 2020, 17. [Google Scholar] [CrossRef] [Green Version]
- Peggy, J.; Chinn, M.K.; Kramer, M.K. Integrated Theory Knowledge Development, 5th ed.; Mosby: London, UK, 2011. [Google Scholar]
- Izaryk, K.; Skarakis-Doyle, E. Using the Delphi technique to explore complex concepts in speech-language pathology: An illustrative example from Children’s social communication. Am. J. Speech Lang Pathol. 2017, 26, 1–11. [Google Scholar] [CrossRef]
- Njuangang, S.; Liyanage, C.; Akintoye, A. Application of the Delphi technique in healthcare maintenance. Int. J. Health Care Qual. Assur. 2017, 30, 737–754. [Google Scholar] [CrossRef]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Okafor, U.B.; Goon, D.T. Developing a Physical Activity Intervention Strategy for Pregnant Women in Buffalo City Municipality, South Africa: A Study Protocol. Int. J. Environ. Res. Public Health 2020, 17, 6694. https://doi.org/10.3390/ijerph17186694
Okafor UB, Goon DT. Developing a Physical Activity Intervention Strategy for Pregnant Women in Buffalo City Municipality, South Africa: A Study Protocol. International Journal of Environmental Research and Public Health. 2020; 17(18):6694. https://doi.org/10.3390/ijerph17186694
Chicago/Turabian StyleOkafor, Uchenna Benedine, and Daniel Ter Goon. 2020. "Developing a Physical Activity Intervention Strategy for Pregnant Women in Buffalo City Municipality, South Africa: A Study Protocol" International Journal of Environmental Research and Public Health 17, no. 18: 6694. https://doi.org/10.3390/ijerph17186694
APA StyleOkafor, U. B., & Goon, D. T. (2020). Developing a Physical Activity Intervention Strategy for Pregnant Women in Buffalo City Municipality, South Africa: A Study Protocol. International Journal of Environmental Research and Public Health, 17(18), 6694. https://doi.org/10.3390/ijerph17186694




