Mercury Exposure and Associations with Hyperlipidemia and Elevated Liver Enzymes: A Nationwide Cross-Sectional Survey
Abstract
1. Introduction
2. Material and Methods
2.1. Survey Data
2.2. Measurement
2.3. Criteria for Hyperlipidemia and Definition of the Elevated Liver Enzymes
2.4. Statistical Analyses
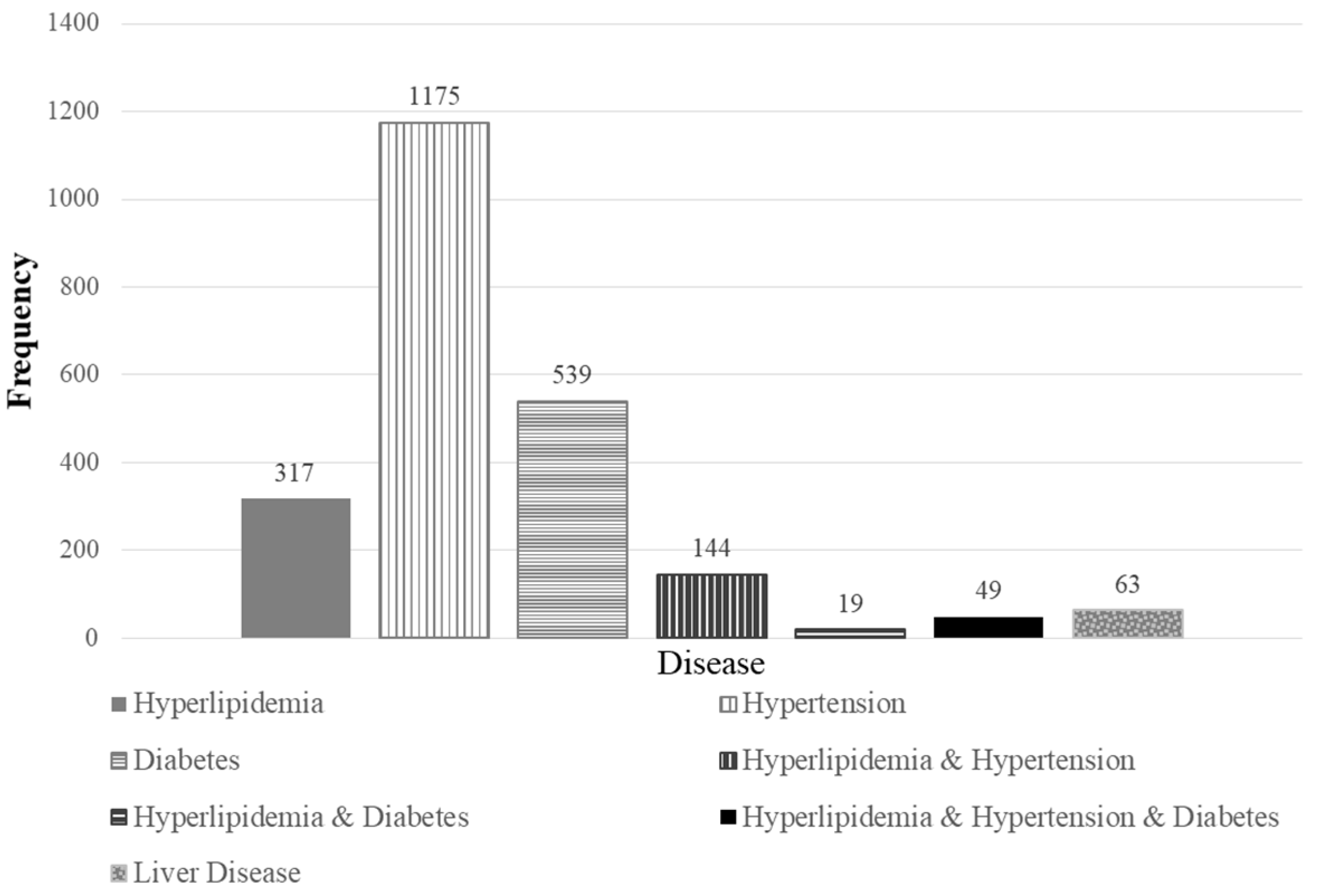
3. Results
3.1. The Distribution of Blood Hg
3.2. The Distribution of Lipid Profiles and Hepatic Enzymes
3.3. Associations between the Blood Hg Levels and Lipid Profiles
3.4. Association between Blood Hg and the Hepatic Enzymes
3.5. The Risks of Hyperlipidemia and Elevated Liver Enzymes
3.6. Relationships between the Lipid Profiles and Hepatic Enzymes across Blood Hg Groups
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Lee, S.E.; Han, K.; Kang, Y.M.; Kim, S.O.; Cho, Y.K.; Ko, K.S.; Park, J.Y.; Lee, K.U.; Koh, E.H. Taskforce Team of Diabetes Fact Sheet of the Korean Diabetes, A. Trends in the prevalence of metabolic syndrome and its components in South Korea: Findings from the Korean National Health Insurance Service Database (2009–2013). PLoS ONE 2018, 13, e0194490. [Google Scholar] [CrossRef]
- Janesick, A.S.; Blumberg, B. Obesogens: An emerging threat to public health. Am. J. Obstet. Gynecol. 2016, 214, 559–565. [Google Scholar] [CrossRef] [PubMed]
- Poursafa, P.; Ataee, E.; Motlagh, M.E.; Ardalan, G.; Tajadini, M.H.; Yazdi, M.; Kelishadi, R. Association of serum lead and mercury level with cardiometabolic risk factors and liver enzymes in a nationally representative sample of adolescents: The CASPIAN-III study. Environ. Sci. Pollut. Res. Int. 2014, 21, 13496–13502. [Google Scholar] [CrossRef] [PubMed]
- Rothenberg, S.E.; Korrick, S.A.; Fayad, R. The influence of obesity on blood mercury levels for U.S. non-pregnant adults and children: NHANES 2007–2010. Environ. Res. 2015, 138, 173–180. [Google Scholar] [CrossRef] [PubMed]
- National Institute of Environmental Research. Integrated Report on Korean National Environmental Health Survey—The 1st Stage (2009–2011); National Institute of Environmental Research: Incheon, Korea, 2011.
- Centers for Disease Control and Prevention. Fourth National Report on Human Exposure to Environmental Chemicals, Updated Tables; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2017; Volume 1.
- Health Canada. Fourth Report on Human Biomonitoring of Environmental Chemicals in Canada; Results of the Canadian Health Measures Survey Cycle 4 (2014–2015); Health Canada: Ottawa, ON, Canada, 2017.
- Park, J.H.; Hwang, M.S.; Ko, A.; Jeong, D.H.; Kang, H.S.; Yoon, H.J.; Hong, J.H. Total mercury concentrations in the general Korean population, 2008–2011. Regul. Toxicol. Pharm. RTP 2014, 70, 681–686. [Google Scholar] [CrossRef] [PubMed]
- Kim, N.Y.; Ahn, S.J.; Ryu, D.Y.; Choi, B.S.; Kim, H.; Yu, I.J.; Park, J.D. Effect of lifestyles on the blood mercury level in Korean adults. Hum. Exp. Toxicol. 2013, 32, 591–599. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Tan, Y.M.; Phillips, M.B.; Sobus, J.R.; Kim, S. Estimating Methylmercury Intake for the General Population of South Korea Using Physiologically Based Pharmacokinetic Modeling. Toxicol. Sci. 2017, 159, 6–15. [Google Scholar] [CrossRef]
- Mergler, D.; Anderson, H.A.; Chan, L.H.; Mahaffey, K.R.; Murray, M.; Sakamoto, M.; Stern, A.H. Panel on Health, R.; Toxicological Effects of, M. Methylmercury exposure and health effects in humans: A worldwide concern. Ambio 2007, 36, 3–11. [Google Scholar] [CrossRef]
- Hong, Y.S.; Kim, Y.M.; Lee, K.E. Methylmercury exposure and health effects. J. Prev. Med. Public Health 2012, 45, 353–363. [Google Scholar] [CrossRef]
- Kim, S.-J.; Han, S.-W.; Lee, D.-J.; Kim, K.-M.; Joo, N.-S. Higher Serum Heavy Metal May Be Related with Higher Serum gamma-Glutamyltransferase Concentration in Koreans: Analysis of the Fifth Korea National Health and Nutrition Examination Survey (KNHANES V-1, 2, 2010, 2011). Korean J. Fam. Med. 2014, 35, 74–80. [Google Scholar] [CrossRef]
- Oh, H.J.; Kim, T.H.; Sohn, Y.W.; Kim, Y.S.; Oh, Y.R.; Cho, E.Y.; Shim, S.Y.; Shin, S.R.; Han, A.L.; Yoon, S.J. Association of serum alanine aminotransferase and γ-glutamyltransferase levels within the reference range with metabolic syndrome and nonalcoholic fatty liver disease. Korean J. Hepatol. 2011, 17, 27–36. [Google Scholar] [CrossRef] [PubMed]
- Mason, J.E.; Starke, R.D.; Van Kirk, J.E. Gamma-glutamyl transferase: A novel cardiovascular risk biomarker. Prev. Cardiol. 2010, 13, 36–41. [Google Scholar] [CrossRef] [PubMed]
- Nakanishi, N.; Suzuki, K.; Tatara, K. Serum gamma-glutamyltransferase and risk of metabolic syndrome and type 2 diabetes in middle-aged Japanese men. Diabetes Care 2004, 27, 1427–1432. [Google Scholar] [CrossRef] [PubMed]
- Choi, W.; Kim, S.; Baek, Y.W.; Choi, K.; Lee, K.; Kim, S.; Yu, S.D.; Choi, K. Exposure to environmental chemicals among Korean adults-updates from the second Korean National Environmental Health Survey (2012–2014). Int. J. Hyg. Environ. Health 2017, 220, 29–35. [Google Scholar] [CrossRef] [PubMed]
- National Institute of Environmental Research. Guideline for Biological Specimens Management on the Second Stage Korean National Environmental Health Survey; National Institute of Environmental Research: Incheon, Korea, 2014.
- Friedewald, W.T.; Levy, R.I.; Fredrickson, D.S. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin. Chem. 1972, 18, 499–502. [Google Scholar] [CrossRef] [PubMed]
- National Institutes of Health. Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Final Report. Circulation 2002, 106, 3143–3421. [Google Scholar]
- National Institute of Environmental Research. Manual for Laboratory Procedures on the Second Stage Korean National Environmental Health Survey (Heavy Metals); National Institute of Environmental Research: Incheon, Korea, 2015.
- Schulz, C.; Angerer, J.; Ewers, U.; Kolossa-Gehring, M. The German Human Biomonitoring Commission. Int. J. Hyg. Environ. Health 2007, 210, 373–382. [Google Scholar] [CrossRef]
- Eom, S.Y.; Choi, S.H.; Ahn, S.J.; Kim, D.K.; Kim, D.W.; Lim, J.A.; Choi, B.S.; Shin, H.J.; Yun, S.W.; Yoon, H.J.; et al. Reference levels of blood mercury and association with metabolic syndrome in Korean adults. Int. Arch. Occup. Environ. Health 2014, 87, 501–513. [Google Scholar] [CrossRef]
- Bae, S.; Park, S.J.; Yeum, K.J.; Choi, B.; Kim, Y.S.; Joo, N.S. Cut-off values of blood mercury concentration in relation to increased body mass index and waist circumference in Koreans. J. Investig. Med. 2016, 64, 867–871. [Google Scholar] [CrossRef]
- You, C.-H.; Kim, B.-G.; Kim, J.-M.; Yu, S.-D.; Kim, Y.-M.; Kim, R.-B.; Hong, Y.-S. Relationship between blood mercury concentration and waist-to-hip ratio in elderly Korean individuals living in coastal areas. J. Prev. Med. Public Health 2011, 44, 218. [Google Scholar] [CrossRef]
- Park, S.; Lee, B.K. Body fat percentage and hemoglobin levels are related to blood lead, cadmium, and mercury concentrations in a Korean Adult Population (KNHANES 2008–2010). Biol. Trace Elem. Res. 2013, 151, 315–323. [Google Scholar] [CrossRef]
- Moon, S.S. Additive effect of heavy metals on metabolic syndrome in the Korean population: The Korea National Health and Nutrition Examination Survey (KNHANES) 2009–2010. Endocrine 2014, 46, 263–271. [Google Scholar] [CrossRef] [PubMed]
- IPCS. International Programme on Chemical Safety-Methylmercury; United Nations Environment Programme: Nairobi, Kenya; the International Labour Organisation and World Health Organization: Geneva, Switzerland, 1990; Available online: http://www.inchem.org/documents/ehc/ehc/ehc101.htm (accessed on 8 April 2019).
- Jung, S.A.; Chung, D.; On, J.; Moon, M.H.; Lee, J.; Pyo, H. Correlation Between Total Mercury and Methyl Mercury-In Whole Blood of South Korean. Bull. Korean Chem. Soc. 2013, 34, 1101–1107. [Google Scholar] [CrossRef]
- Ayotte, P.; Carrier, A.; Ouellet, N.; Boiteau, V.; Abdous, B.; Sidi, E.A.; Chateau-Degat, M.L.; Dewailly, E. Relation between methylmercury exposure and plasma paraoxonase activity in inuit adults from Nunavik. Environ. Health Perspect 2011, 119, 1077–1083. [Google Scholar] [CrossRef]
- Maqbool, F.; Bahadar, H.; Niaz, K.; Baeeri, M.; Rahimifard, M.; Navaei-Nigjeh, M.; Ghasemi-Niri, S.F.; Abdollahi, M. Effects of methyl mercury on the activity and gene expression of mouse Langerhans islets and glucose metabolism. Food Chem. Toxicol. 2016, 93, 119–128. [Google Scholar] [CrossRef]
- Agency for Toxic Substances and Disease Registry. Toxicological Profile for Mercury; Agency for Toxic Substances and Disease Registry: Atlanta, GA, USA, 1999.
- Clarkson, T.W.; Vyas, J.B.; Ballatori, N. Mechanisms of mercury disposition in the body. Am. J. Ind. Med. 2007, 50, 757–764. [Google Scholar] [CrossRef] [PubMed]
- Aschner, M.; Aschner, J.L. Mercury neurotoxicity: Mechanisms of blood-brain barrier transport. Neurosci. Biobehav. Rev. 1990, 14, 169–176. [Google Scholar] [CrossRef]
- Singh, V.; Joshi, D.; Shrivastava, S.; Shukla, S. Effect of monothiol along with antioxidant against mercury-induced oxidative stress in rat. Indian J. Exp. Biol. 2007, 45, 1037–1044. [Google Scholar] [PubMed]
- Wadaan, M.A. Effects of mercury exposure on blood chemistry and liver histopathology of male rats. J. Pharmacol. Toxicol. 2009, 4, 126–131. [Google Scholar] [CrossRef]
- Schaefer, A.M.; Stavros, H.C.; Bossart, G.D.; Fair, P.A.; Goldstein, J.D.; Reif, J.S. Associations between mercury and hepatic, renal, endocrine, and hematological parameters in Atlantic bottlenose dolphins (Tursiops truncatus) along the eastern coast of Florida and South Carolina. Arch. Environ. Con. Tox. 2011, 61, 688–695. [Google Scholar] [CrossRef]
- Lee, S.; Shin, M.; Hong, Y.C.; Kim, J.H. Temporal variability of blood lead, mercury, and cadmium levels in elderly panel study (2008–2014). Int. J. Hyg. Environ. Health 2017, 220, 407–414. [Google Scholar] [CrossRef]

| Variables | N | GM | 95 % Confidence Interval | P75 | P95 | p-Value a | |
|---|---|---|---|---|---|---|---|
| All | 6454 | 3.11 | (3.02, 3.20) | 4.69 | 9.01 | - | |
| Sex | <0.0001 | ||||||
| Male | 2767 | 3.70 | (3.57, 3.84) | 5.48 | 10.2 | ||
| Female | 3687 | 2.63 | (2.54, 2.72) | 3.83 | 7.11 | ||
| Age | <0.0001 | ||||||
| 19–29 | 536 | 2.37 | (2.23, 2.52) | 3.22 | 6.93 | ||
| 30–39 | 1053 | 3.18 | (3.04, 3.33) | 4.71 | 8.10 | ||
| 40–49 | 1224 | 3.58 | (3.43, 3.75) | 5.25 | 9.56 | ||
| 50–59 | 1434 | 3.64 | (3.47, 3.82) | 5.21 | 10.4 | ||
| 60–69 | 1326 | 3.23 | (3.05, 3.43) | 4.85 | 9.17 | ||
| 70+ | 881 | 2.54 | (2.38, 2.71) | 3.86 | 8.40 | ||
| BMI | <0.0001 | ||||||
| <18.5 | 159 | 2.13 | (1.85, 2.45) | 2.76 | 5.61 | ||
| 18.5 to < 23.0 | 2209 | 2.74 | (2.64, 2.85) | 4.08 | 7.61 | ||
| 23.0 to < 25.0 | 1602 | 3.27 | (3.13, 3.41) | 4.90 | 9.05 | ||
| ≥25.0 | 2484 | 3.54 | (3.41, 3.68) | 5.24 | 9.95 | ||
| Smoke | <0.0001 | ||||||
| Non-smoker | 4244 | 2.74 | (2.65, 2.83) | 4.03 | 7.62 | ||
| Past | 1053 | 3.92 | (3.71, 4.14) | 5.82 | 11.0 | ||
| Current | 1157 | 3.81 | (3.64, 4.00) | 5.71 | 10.03 | ||
| Alcohol frequency | <0.0001 | ||||||
| Never | 2219 | 2.68 | (2.57, 2.79) | 4.07 | 7.49 | ||
| <1 time/month | 709 | 2.68 | (2.53, 2.84) | 3.78 | 6.90 | ||
| 1–3 times/month | 1033 | 2.94 | (2.79, 3.09) | 4.28 | 7.83 | ||
| 1–2 times/week | 1400 | 3.47 | (3.30, 3.64) | 5.25 | 9.67 | ||
| >3 times/week | 612 | 4.03 | (3.80, 4.27) | 5.93 | 11.5 | ||
| Daily | 481 | 4.08 | (3.77, 4.43) | 5.85 | 13.3 | ||
| Household income (USD/month) | <0.0001 | ||||||
| <1500 | 1792 | 2.76 | (2.62, 2.92) | 4.29 | 8.98 | ||
| 1500 to < 3000 | 1621 | 3.01 | (2.84, 3.18) | 4.52 | 8.79 | ||
| 3000 to < 5000 | 1765 | 3.21 | (3.08, 3.35) | 4.70 | 7.91 | ||
| 5000 to < 10,000 | 1103 | 3.37 | (3.19, 3.56) | 5.01 | 9.50 | ||
| ≥10,000 | 173 | 3.47 | (3.06, 3.92) | 5.19 | 9.97 | ||
| Fish consumption frequency | <0.0001 | ||||||
| Rarely | 622 | 2.17 | (2.03, 2.32) | 3.07 | 6.95 | ||
| 1–3 times/month | 2030 | 2.88 | (2.77, 2.99) | 4.36 | 7.76 | ||
| 1–3 times/week | 3377 | 3.41 | (3.30, 3.53) | 5.03 | 9.37 | ||
| 4–6 times/week | 425 | 4.04 | (3.68, 4.43) | 6.20 | 11.2 | ||
| Biomarkers (units) | Blood Hg | Male | Female | All | p-Value b | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Group a | N | GM | (P5 | P95) | N | GM | (P5 | P95) | N | GM | (P5 | P95) | ||
| LDL (mg/dL) | Low | 613 | 82.7 | (45.3 | 143) | 1534 | 89.6 | (52.1 | 144) | 2156 | 87.3 | (48.8 | 143) | 0.0085 |
| Middle | 895 | 84.5 | (40.1 | 146) | 1236 | 92.3 | (53.8 | 150) | 2142 | 88.4 | (45.8 | 148) | ||
| High | 1234 | 86.7 | (40.1 | 146) | 905 | 91.2 | (50.0 | 152) | 2156 | 88.2 | (43.3 | 149) | ||
| HDL (mg/dL) | Low | 613 | 48.9 | (33.2 | 73.6) | 1534 | 56.0 | (36.5 | 83.5) | 2156 | 53.6 | (35.0 | 80.6) | 0.0012 |
| Middle | 895 | 49.6 | (33.6 | 72.8) | 1236 | 56.4 | (37.8 | 85.8) | 2142 | 52.9 | (34.7 | 80.5) | ||
| High | 1234 | 49.2 | (33.3 | 72.4) | 905 | 55.7 | (37.2 | 84.4) | 2156 | 51.3 | (34.1 | 77.1) | ||
| Total cholesterol (mg/dL) | Low | 613 | 171 | (126 | 234) | 1534 | 178 | (129 | 240) | 2156 | 176 | (128 | 238) | <0.0001 |
| Middle | 895 | 180 | (129 | 244) | 1236 | 183 | (135 | 248) | 2142 | 181 | (132 | 246) | ||
| High | 1234 | 184 | (132 | 246) | 905 | 186 | (137 | 242) | 2156 | 185 | (134 | 245) | ||
| TG (mg/dL) | Low | 613 | 139 | (49.6 | 370) | 1534 | 119 | (49.2 | 303) | 2156 | 125 | (49.4 | 331) | 0.5822 |
| Middle | 895 | 160 | (63.2 | 496) | 1236 | 127 | (49.2 | 365) | 2142 | 143 | (56.5 | 415) | ||
| High | 1234 | 176 | (72.8 | 461) | 905 | 134 | (53.8 | 393) | 2156 | 160 | (62.6 | 437) | ||
| ALT (U/L) | Low | 613 | 22.2 | (10.3 | 62.4) | 1534 | 16.5 | (8.54 | 33.8) | 2156 | 18.2 | (8.99 | 42.7) | 0.0002 |
| Middle | 895 | 25.5 | (11.7 | 71.6) | 1236 | 18.1 | (9.39 | 38.2) | 2142 | 21.5 | (10.0 | 55.4) | ||
| High | 1234 | 27.4 | (12.6 | 69.7) | 905 | 19.7 | (9.93 | 45.0) | 2156 | 24.5 | (11.1 | 60.9) | ||
| AST (U/L) | Low | 613 | 24.0 | (16.0 | 39.1) | 1534 | 21.4 | (14.1 | 32.9) | 2156 | 22.2 | (14.6 | 34.9) | 0.0226 |
| Middle | 895 | 25.8 | (16.2 | 45.0) | 1236 | 21.9 | (15.0 | 34.2) | 2142 | 23.8 | (15.3 | 39.0) | ||
| High | 1234 | 26.1 | (16.7 | 46.0) | 905 | 23.1 | (15.0 | 36.5) | 2156 | 25.0 | (16.0 | 44.0) | ||
| GGT (U/L) | Low | 613 | 25.7 | (11.1 | 106) | 1534 | 15.9 | (7.93 | 41.7) | 2156 | 18.6 | (8.36 | 56.5) | <0.0001 |
| Middle | 895 | 32.6 | (12.6 | 132) | 1236 | 17.8 | (8.60 | 51.5) | 2142 | 24.0 | (9.46 | 88.7) | ||
| High | 1234 | 39.2 | (13.9 | 152) | 905 | 19.9 | (9.04 | 58.2) | 2156 | 31.1 | (10.7 | 134) | ||
| Lipid Profiles | Criteria | Male | Female | p-Value a | p-Value b | |||
|---|---|---|---|---|---|---|---|---|
| N | GM | N | GM | |||||
| LDL | <100 | Optimal | 1640 | 3.70 | 1982 | 2.70 | 0.0009 | 0.1054 |
| 100–129 | Above optimal | 791 | 3.85 | 1161 | 2.84 | |||
| 130–159 | Borderline high | 285 | 4.31 | 434 | 2.80 | |||
| 160–189 | High | 40 | 4.19 | 95 | 3.13 | |||
| ≥190 | Very high | 11 | 4.05 | 15 | 2.79 | |||
| HDL | <40 | Low | 552 | 3.53 | 321 | 2.59 | 0.0004 | 0.1730 |
| 40–60 | Optimal | 1658 | 3.87 | 2023 | 2.77 | |||
| ≥60 | High | 557 | 3.92 | 1343 | 2.82 | |||
| Total | <200 | Desirable | 1955 | 3.64 | 2504 | 2.71 | <0.0001 | <0.0001 |
| cholesterol | 200–239 | Borderline high | 654 | 4.28 | 909 | 2.86 | ||
| ≥240 | High | 158 | 4.13 | 274 | 2.95 | |||
| TG | <150 | Normal | 1286 | 3.59 | 2235 | 2.73 | <0.0001 | <0.0001 |
| 150–199 | Borderline high | 519 | 4.01 | 599 | 2.71 | |||
| 200–499 | High | 854 | 4.00 | 794 | 2.94 | |||
| ≥500 | Very high | 107 | 4.02 | 58 | 2.63 | |||
| Hyperlipidemia c | No | 1057 | 3.48 | 1698 | 2.69 | <0.0001 | <0.0001 | |
| Yes | 1710 | 4.03 | 1989 | 2.83 | ||||
| Hepatic Enzymes | Male | Female | p-Value a | p-Value b | ||||
|---|---|---|---|---|---|---|---|---|
| Criteria | N | GM | Criteria | N | GM | |||
| ALT | ≤49 | 2513 | 3.78 | ≤49 | 3583 | 2.75 | <0.0001 | <0.0001 |
| >49 | 254 | 4.14 | >49 | 104 | 3.56 | |||
| AST | <34 | 2373 | 3.76 | <34 | 3446 | 2.74 | <0.0001 | <0.0001 |
| ≥34 | 394 | 4.14 | ≥34 | 241 | 3.22 | |||
| GGT | <73 | 2361 | 3.67 | <38 | 3305 | 2.71 | <0.0001 | <0.0001 |
| ≥73 | 406 | 4.73 | ≥38 | 382 | 3.30 | |||
| Elevated | No | 2096 | 3.64 | No | 3169 | 2.70 | <0.0001 | <0.0001 |
| Liver enzymes c | Yes | 671 | 4.38 | Yes | 518 | 3.25 | ||
| Disease | Personal Medication a | GM | OR | 95 % CI | p-Value b |
|---|---|---|---|---|---|
| Hyperlipidemia (n = 3699) | |||||
| Unadjusted | 3.33 | 1.105 | (1.013, 1.206) | 0.0252 | |
| Hyperlipidemia | 3.12 | 1.104 | (1.012, 1.206) | 0.0266 | |
| Hyperlipidemia and Hypertension | 2.95 | 1.104 | (1.011, 1.205) | 0.0275 | |
| Hyperlipidemia and Diabetes | 3.60 | 1.105 | (1.013, 1.207) | 0.0250 | |
| Hyperlipidemia and Hypertension and Diabetes | 3.16 | 1.104 | (1.012, 1.206) | 0.0263 | |
| One of the Hyperlipidemia, Hypertension, Diabetes | 3.19 | 1.100 | (1.007, 1.201) | 0.0335 | |
| Elevated liver enzymes (n = 1189) | |||||
| Unadjusted | 3.84 | 1.345 | (1.206, 1.500) | <0.0001 | |
| Liver disease | 3.24 | 1.350 | (1.210, 1.506) | <0.0001 | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, S.; Cho, S.-R.; Jeong, I.; Park, J.B.; Shin, M.-Y.; Kim, S.; Kim, J.H. Mercury Exposure and Associations with Hyperlipidemia and Elevated Liver Enzymes: A Nationwide Cross-Sectional Survey. Toxics 2020, 8, 47. https://doi.org/10.3390/toxics8030047
Lee S, Cho S-R, Jeong I, Park JB, Shin M-Y, Kim S, Kim JH. Mercury Exposure and Associations with Hyperlipidemia and Elevated Liver Enzymes: A Nationwide Cross-Sectional Survey. Toxics. 2020; 8(3):47. https://doi.org/10.3390/toxics8030047
Chicago/Turabian StyleLee, Seungho, Sung-Ran Cho, Inchul Jeong, Jae Bum Park, Mi-Yeon Shin, Sungkyoon Kim, and Jin Hee Kim. 2020. "Mercury Exposure and Associations with Hyperlipidemia and Elevated Liver Enzymes: A Nationwide Cross-Sectional Survey" Toxics 8, no. 3: 47. https://doi.org/10.3390/toxics8030047
APA StyleLee, S., Cho, S.-R., Jeong, I., Park, J. B., Shin, M.-Y., Kim, S., & Kim, J. H. (2020). Mercury Exposure and Associations with Hyperlipidemia and Elevated Liver Enzymes: A Nationwide Cross-Sectional Survey. Toxics, 8(3), 47. https://doi.org/10.3390/toxics8030047








