The Possible Influence of Mediterranean Diet on Extracellular Vesicle miRNA Expression in Breast Cancer Survivors
Abstract
:1. Introduction
2. Methods
2.1. Study Overview and Participants
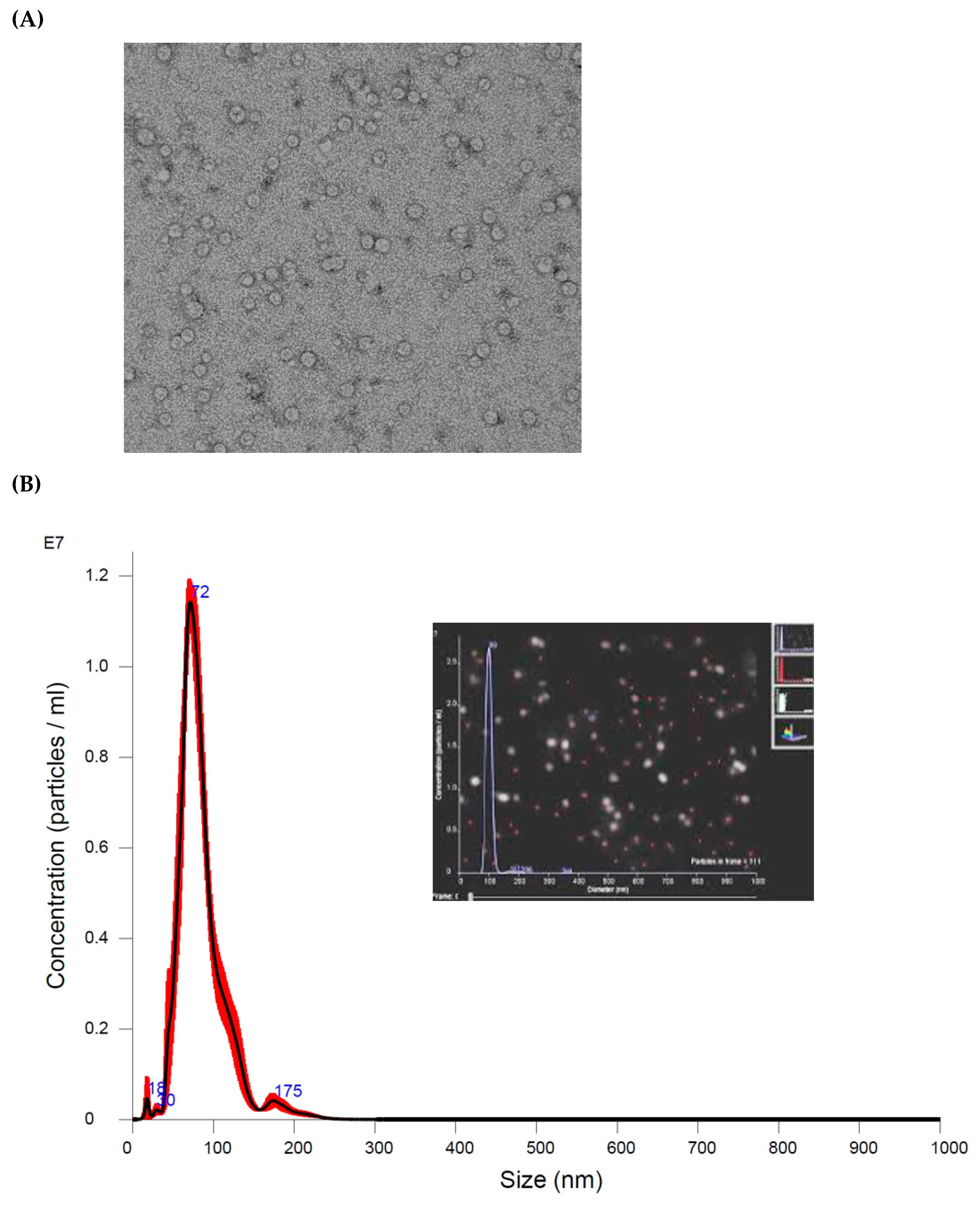
2.2. Extracellular Vesicle RNAs Measurement
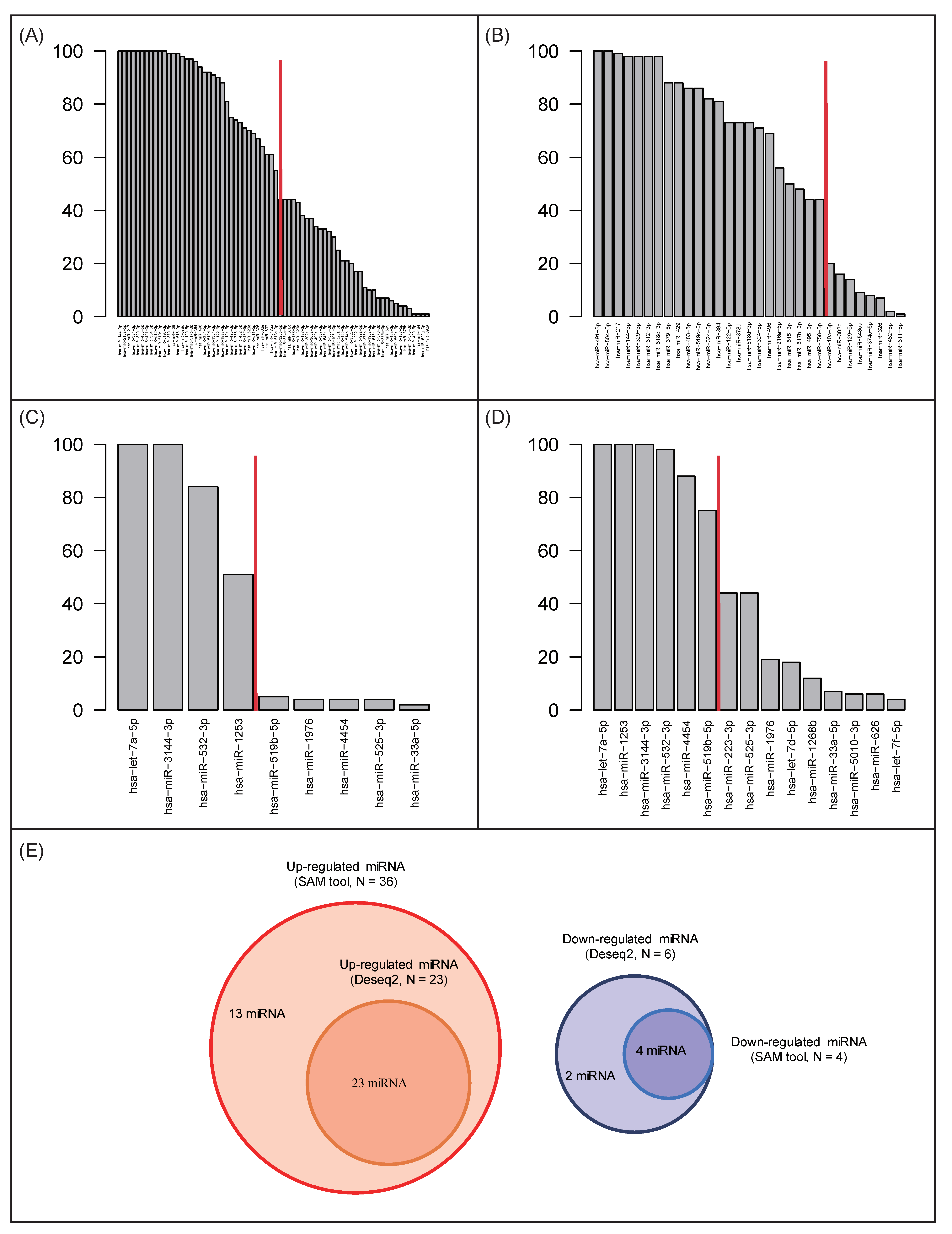
2.3. Identification of Differentially Expressed miRNAs
- Step (1): Sixteen samples (same number in all subjects) were randomly selected with replacement.
- Step (2): Differentially expressed miRNAs were curated by using SAM and DESeq2 with adjusted p-value (FDR) < 0.05 and |log2(fold change)| > 1.
- Step (3): The above steps were repeated 100 times, yielding a list that included selected miRNAs.
2.4. Curation of miRNA Target Genes
2.5. Pathway Analysis
3. Results
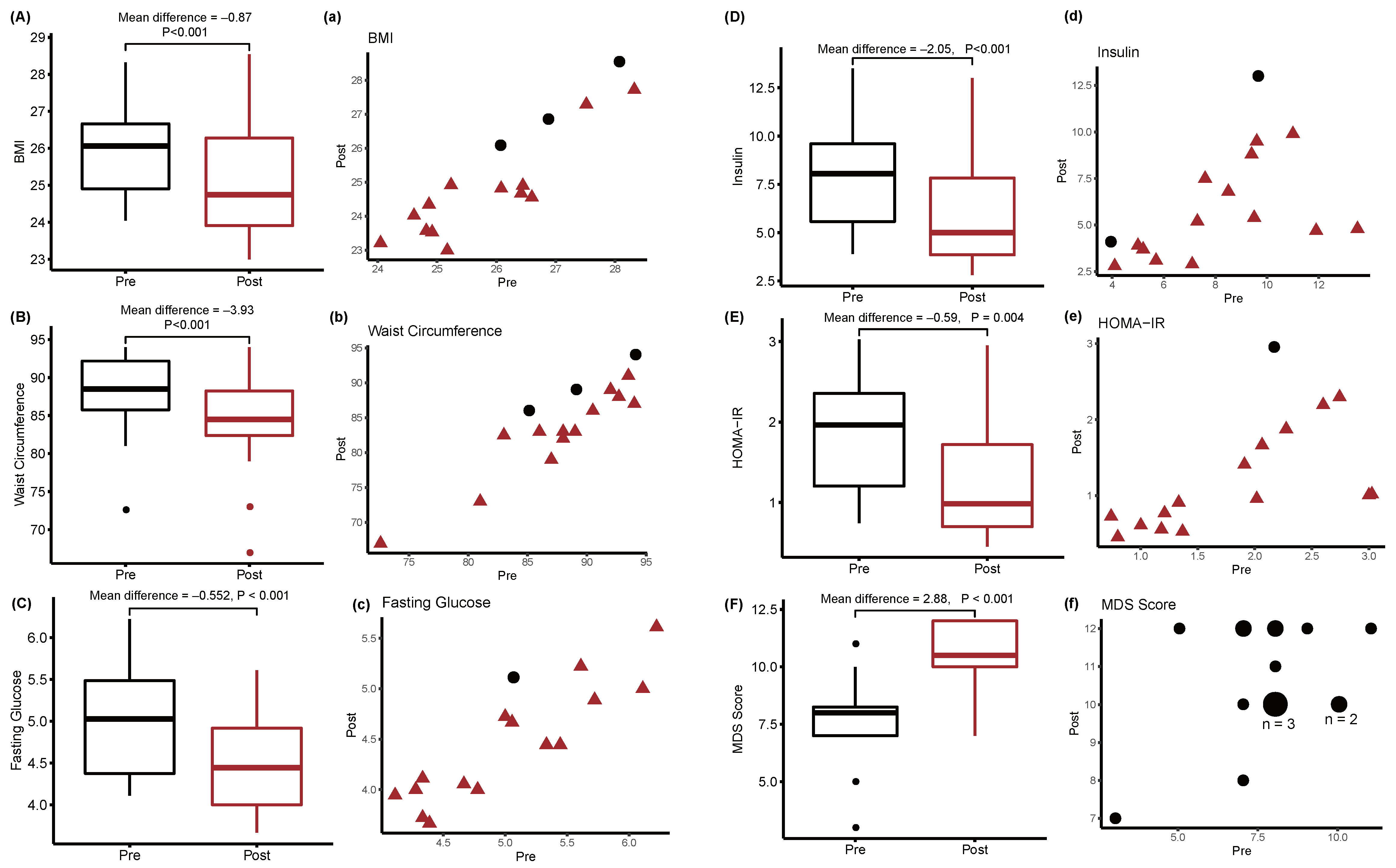
3.1. Clinical Characteristics of the Study Population
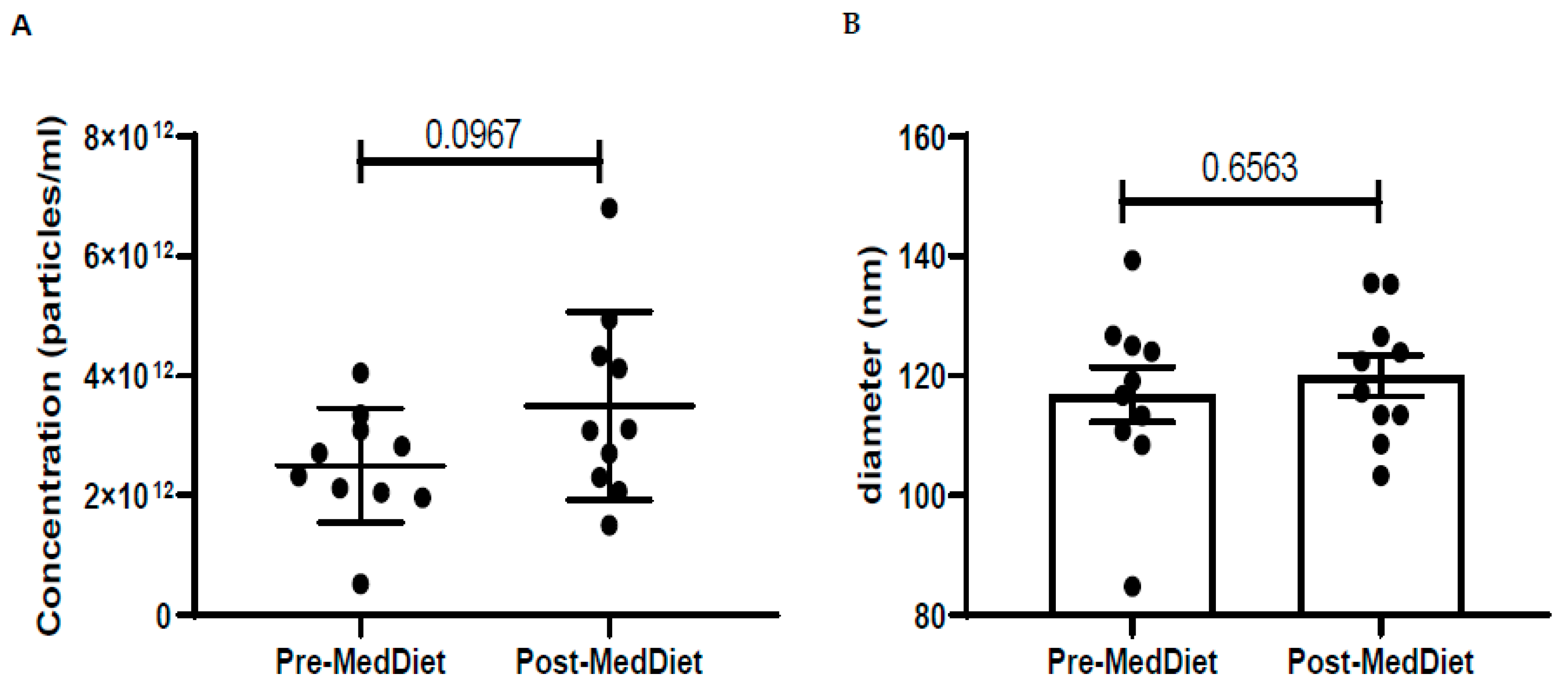
3.2. Plasma Extracellular Vesicle miRNA Changes and Mediterranean Diet
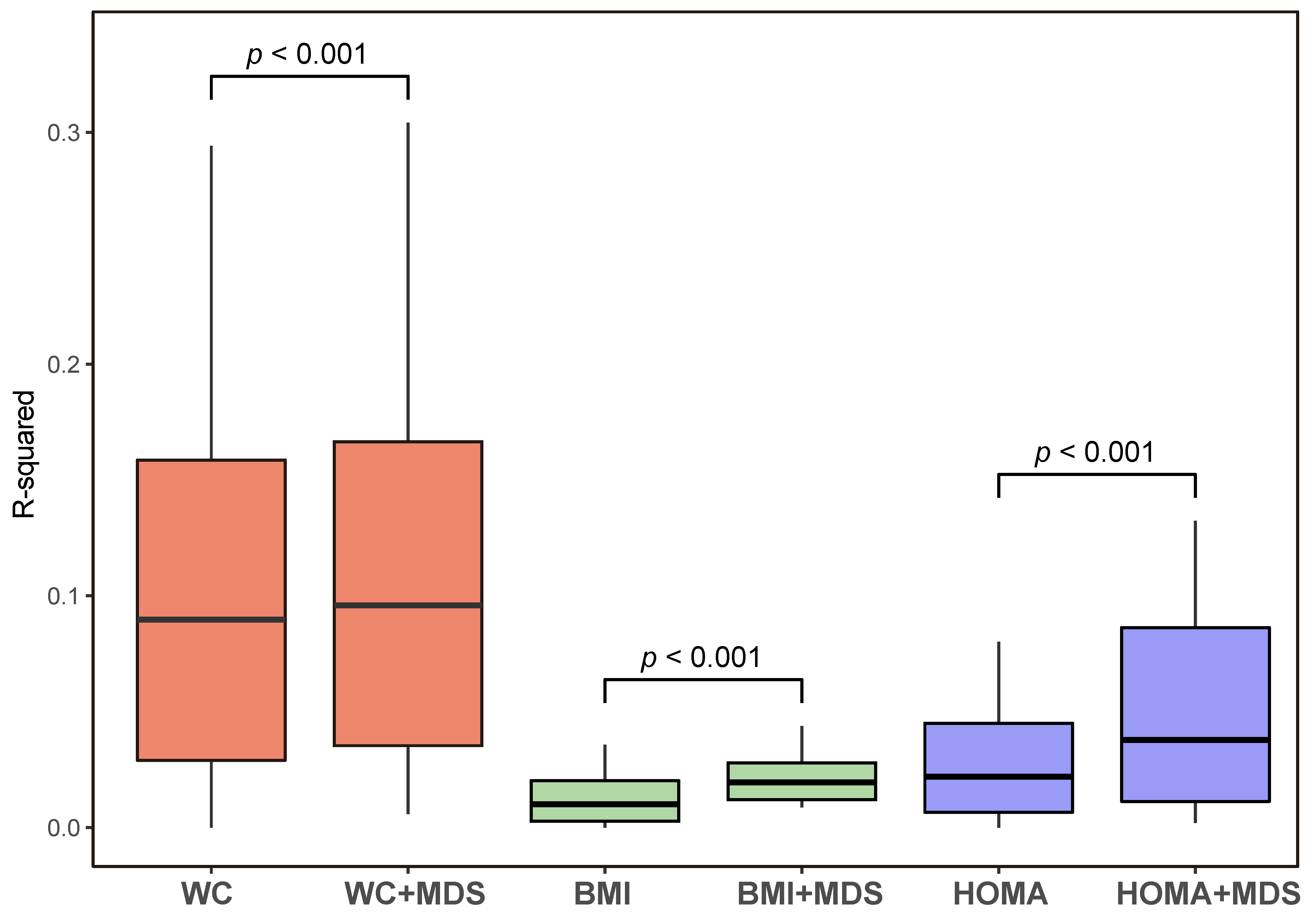
3.3. Identification of Expressed Extracellular Vesicle miRNAs
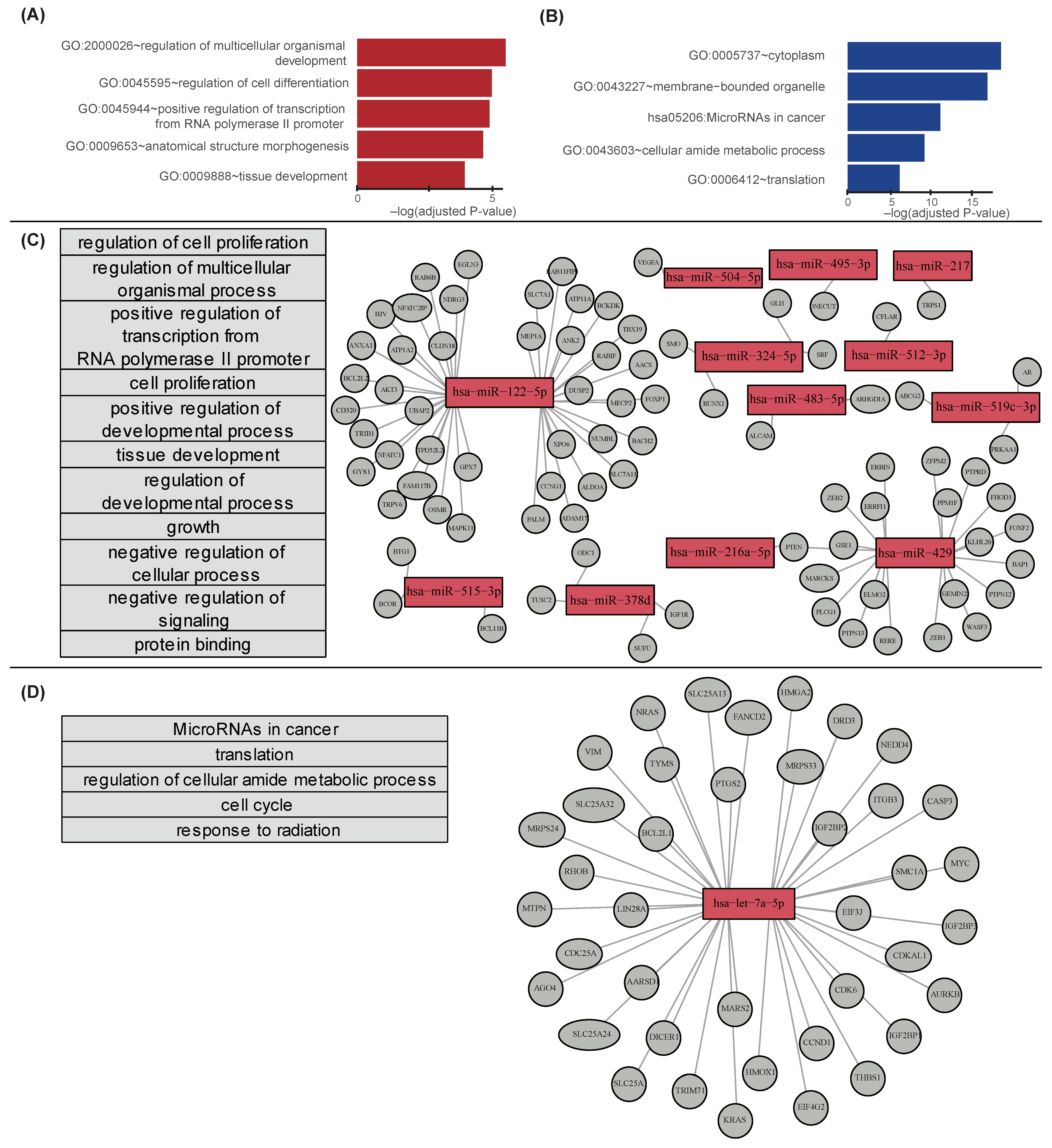
3.4. Extracellular Vesicle miRNAs and Their Target Genes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
References
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: Globocan estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [Green Version]
- Miller, K.D.; Nogueira, L.; Mariotto, A.B.; Rowland, J.H.; Yabroff, K.R.; Alfano, C.M.; Jemal, A.; Kramer, J.L.; Siegel, R.L. Cancer treatment and survivorship statistics, 2019. CA Cancer J. Clin. 2019, 69, 363–385. [Google Scholar] [CrossRef] [Green Version]
- Shapiro, C.L. Cancer survivorship. N. Engl. J. Med. 2018, 379, 2438–2450. [Google Scholar] [CrossRef]
- Ligibel, J.A.; Alfano, C.M.; Courneya, K.S.; Demark-Wahnefried, W.; Burger, R.A.; Chlebowski, R.T.; Fabian, C.J.; Gucalp, A.; Hershman, D.L.; Hudson, M.M.; et al. American society of clinical oncology position statement on obesity and cancer. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2014, 32, 3568–3574. [Google Scholar] [CrossRef]
- Burke, S.; Wurz, A.; Bradshaw, A.; Saunders, S.; West, M.A.; Brunet, J. Physical activity and quality of life in cancer survivors: A meta-synthesis of qualitative research. Cancers 2017, 9, 53. [Google Scholar] [CrossRef] [Green Version]
- Mehta, L.S.; Watson, K.E.; Barac, A.; Beckie, T.M.; Bittner, V.; Cruz-Flores, S.; Dent, S.; Kondapalli, L.; Ky, B.; Okwuosa, T.; et al. Cardiovascular disease and breast cancer: Where these entities intersect: A scientific statement from the american heart association. Circulation 2018, 137, e30–e66. [Google Scholar] [CrossRef]
- Chlebowski, R.T.; Reeves, M.M. Weight loss randomized intervention trials in female cancer survivors. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2016, 34, 4238–4248. [Google Scholar] [CrossRef] [Green Version]
- Martinez-Gonzalez, M.A.; Corella, D.; Salas-Salvado, J.; Ros, E.; Covas, M.I.; Fiol, M.; Warnberg, J.; Aros, F.; Ruiz-Gutierrez, V.; Lamuela-Raventos, R.M.; et al. Cohort profile: Design and methods of the predimed study. Int. J. Epidemiol. 2012, 41, 377–385. [Google Scholar] [CrossRef] [Green Version]
- Martinez-Gonzalez, M.A.; Gea, A.; Ruiz-Canela, M. The mediterranean diet and cardiovascular health. Circ. Res. 2019, 124, 779–798. [Google Scholar] [CrossRef]
- Kris-Etherton, P.; Eckel, R.H.; Howard, B.V.; St Jeor, S.; Bazzarre, T.L. Aha science advisory: Lyon diet heart study. Benefits of a mediterranean-style, national cholesterol education program/american heart association step i dietary pattern on cardiovascular disease. Circulation 2001, 103, 1823–1825. [Google Scholar] [CrossRef] [Green Version]
- Menotti, A.; Puddu, P.E. How the seven countries study contributed to the definition and development of the mediterranean diet concept: A 50-year journey. Nutr. Metab. Cardiovasc. Dis. 2015, 25, 245–252. [Google Scholar] [CrossRef]
- Toledo, E.; Salas-Salvado, J.; Donat-Vargas, C.; Buil-Cosiales, P.; Estruch, R.; Ros, E.; Corella, D.; Fito, M.; Hu, F.B.; Aros, F.; et al. Mediterranean diet and invasive breast cancer risk among women at high cardiovascular risk in the predimed trial: A randomized clinical trial. JAMA Intern. Med. 2015, 175, 1752–1760. [Google Scholar] [CrossRef]
- Van den Brandt, P.A.; Schulpen, M. Mediterranean diet adherence and risk of postmenopausal breast cancer: Results of a cohort study and meta-analysis. Int. J. Cancer 2017, 140, 2220–2231. [Google Scholar] [CrossRef]
- Haridass, V.; Ziogas, A.; Neuhausen, S.L.; Anton-Culver, H.; Odegaard, A.O. Diet quality scores inversely associated with postmenopausal breast cancer risk are not associated with premenopausal breast cancer risk in the california teachers study. J. Nutr. 2018, 148, 1830–1837. [Google Scholar] [CrossRef] [Green Version]
- Butler, L.M.; Wu, A.H.; Wang, R.; Koh, W.P.; Yuan, J.M.; Yu, M.C. A vegetable-fruit-soy dietary pattern protects against breast cancer among postmenopausal singapore chinese women. Am. J. Clin. Nutr. 2010, 91, 1013–1019. [Google Scholar] [CrossRef] [Green Version]
- Raposo, G.; Stoorvogel, W. Extracellular vesicles: Exosomes, microvesicles, and friends. J. Cell Biol. 2013, 200, 373–383. [Google Scholar] [CrossRef] [Green Version]
- Condrat, C.E.; Thompson, D.C.; Barbu, M.G.; Bugnar, O.L.; Boboc, A.; Cretoiu, D.; Suciu, N.; Cretoiu, S.M.; Voinea, S.C. Mirnas as biomarkers in disease: Latest findings regarding their role in diagnosis and prognosis. Cells 2020, 9, 276. [Google Scholar] [CrossRef] [Green Version]
- Ortega, F.J.; Cardona-Alvarado, M.I.; Mercader, J.M.; Moreno-Navarrete, J.M.; Moreno, M.; Sabater, M.; Fuentes-Batllevell, N.; Ramirez-Chavez, E.; Ricart, W.; Molina-Torres, J.; et al. Circulating profiling reveals the effect of a polyunsaturated fatty acid-enriched diet on common micrornas. J. Nutr. Biochem. 2015, 26, 1095–1101. [Google Scholar] [CrossRef]
- Marques-Rocha, J.L.; Milagro, F.I.; Mansego, M.L.; Zulet, M.A.; Bressan, J.; Martinez, J.A. Expression of inflammation-related mirnas in white blood cells from subjects with metabolic syndrome after 8 wk of following a mediterranean diet-based weight loss program. Nutrition 2016, 32, 48–55. [Google Scholar] [CrossRef] [Green Version]
- Schroder, H.; Fito, M.; Estruch, R.; Martinez-Gonzalez, M.A.; Corella, D.; Salas-Salvado, J.; Lamuela-Raventos, R.; Ros, E.; Salaverria, I.; Fiol, M.; et al. A short screener is valid for assessing mediterranean diet adherence among older spanish men and women. J. Nutr. 2011, 141, 1140–1145. [Google Scholar] [CrossRef] [Green Version]
- Tusher, V.G.; Tibshirani, R.; Chu, G. Significance analysis of microarrays applied to the ionizing radiation response. Proc. Natl. Acad. Sci. USA 2001, 98, 5116–5121. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Love, M.I.; Huber, W.; Anders, S. Moderated estimation of fold change and dispersion for rna-seq data with deseq2. Genome Biol. 2014, 15, 550. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kanehisa, M.; Goto, S. Kegg: Kyoto encyclopedia of genes and genomes. Nucleic Acids Res. 2000, 28, 27–30. [Google Scholar] [CrossRef] [PubMed]
- Harris, M.A.; Clark, J.; Ireland, A.; Lomax, J.; Ashburner, M.; Foulger, R.; Eilbeck, K.; Lewis, S.; Marshall, B.; Mungall, C.; et al. The gene ontology (go) database and informatics resource. Nucleic Acids Res. 2004, 32, D258–D261. [Google Scholar]
- Fresno, C.; Fernández, E.A. RDAVIDWebService: A versatile R interface to DAVID. Bioinformatics 2013, 29, 2810–2811. [Google Scholar] [CrossRef] [Green Version]
- Kim, J.; Kim, J.J.; Lee, H. An analysis of disease-gene relationship from medline abstracts by digsee. Sci. Rep. 2017, 7, 40154. [Google Scholar] [CrossRef] [Green Version]
- Gerber, B.; Freund, M.; Reimer, T. Recurrent breast cancer: Treatment strategies for maintaining and prolonging good quality of life. Dtsch. Arztebl. Int. 2010, 107, 85–91. [Google Scholar]
- McShane, L.M.; Altman, D.G.; Sauerbrei, W.; Taube, S.E.; Gion, M.; Clark, G.M. Reporting recommendations for tumor marker prognostic studies (remark). Breast Cancer Res. Treat. 2006, 100, 229–235. [Google Scholar] [CrossRef]
- Borrebaeck, C.A. Precision diagnostics: Moving towards protein biomarker signatures of clinical utility in cancer. Nat. Rev. Cancer 2017, 17, 199–204. [Google Scholar] [CrossRef]
- Asiaf, A.; Ahmad, S.T.; Arjumand, W.; Zargar, M.A. Micrornas in breast cancer: Diagnostic and therapeutic potential. Methods Mol. Biol. 2018, 1699, 23–43. [Google Scholar]
- Slack, F.J.; Chinnaiyan, A.M. The role of non-coding rnas in oncology. Cell 2019, 179, 1033–1055. [Google Scholar] [CrossRef]
- Veronesi, U.; Boyle, P.; Goldhirsch, A.; Orecchia, R.; Viale, G. Breast cancer. Lancet 2005, 365, 1727–1741. [Google Scholar] [CrossRef]
- Brennan, S.F.; Woodside, J.V.; Lunny, P.M.; Cardwell, C.R.; Cantwell, M.M. Dietary fat and breast cancer mortality: A systematic review and meta-analysis. Crit. Rev. Food Sci. Nutr. 2017, 57, 1999–2008. [Google Scholar] [CrossRef] [Green Version]
- Cole, S.W. Chronic inflammation and breast cancer recurrence. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2009, 27, 3418–3419. [Google Scholar] [CrossRef] [PubMed]
- Gennari, A.; Sormani, M.; Pronzato, P.; Bruzzi, P.; Ferrannini, E.; Iozzo, P.; Roncella, M.; Ghilli, M.; Mirisola, V.; Pfeffer, U. Association between expression of insulin resistance (ir) related genes and breast cancer outcome. J. Clin. Oncol. 2007, 25, 10597. [Google Scholar] [CrossRef]
- Esposito, K.; Kastorini, C.M.; Panagiotakos, D.B.; Giugliano, D. Mediterranean diet and weight loss: Meta-analysis of randomized controlled trials. Metab. Syndr. Relat. Disord. 2011, 9, 1–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Salas-Salvado, J.; Diaz-Lopez, A.; Ruiz-Canela, M.; Basora, J.; Fito, M.; Corella, D.; Serra-Majem, L.; Warnberg, J.; Romaguera, D.; Estruch, R.; et al. Effect of a lifestyle intervention program with energy-restricted mediterranean diet and exercise on weight loss and cardiovascular risk factors: One-year results of the predimed-plus trial. Diabetes Care 2019, 42, 777–788. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mitjavila, M.T.; Fandos, M.; Salas-Salvado, J.; Covas, M.I.; Borrego, S.; Estruch, R.; Lamuela-Raventos, R.; Corella, D.; Martinez-Gonzalez, M.A.; Sanchez, J.M.; et al. The mediterranean diet improves the systemic lipid and DNA oxidative damage in metabolic syndrome individuals. A randomized, controlled, trial. Clin. Nutr. 2013, 32, 172–178. [Google Scholar] [CrossRef] [PubMed]
- Fasanaro, P.; D’Alessandra, Y.; Magenta, A.; Pompilio, G.; Capogrossi, M.C. Micrornas: Promising biomarkers and therapeutic targets of acute myocardial ischemia. Curr. Vasc. Pharmacol. 2015, 13, 305–315. [Google Scholar] [CrossRef]
- Hulsmans, M.; Holvoet, P. Micrornas as early biomarkers in obesity and related metabolic and cardiovascular diseases. Curr. Pharm. Des. 2013, 19, 5704–5717. [Google Scholar] [CrossRef]
- Uen, Y.; Wang, J.W.; Wang, C.; Jhang, Y.; Chung, J.Y.; Tseng, T.; Sheu, M.; Lee, S. Mining of potential micrornas with clinical correlation—Regulation of syndecan-1 expression by mir-122-5p altered mobility of breast cancer cells and possible correlation with liver injury. Oncotarget 2018, 9, 28165–28175. [Google Scholar] [CrossRef] [PubMed]
- Kuo, W.T.; Yu, S.Y.; Li, S.C.; Lam, H.C.; Chang, H.T.; Chen, W.S.; Yeh, C.Y.; Hung, S.F.; Liu, T.C.; Wu, T.; et al. Microrna-324 in human cancer: Mir-324-5p and mir-324-3p have distinct biological functions in human cancer. Anticancer Res. 2016, 36, 5189–5196. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xia, Y.; Zhu, Y.; Zhou, X.; Chen, Y. Low expression of let-7 predicts poor prognosis in patients with multiple cancers: A meta-analysis. Tumour Biol. J. Int. Soc. Oncodevelop. Biol. Med. 2014, 35, 5143–5148. [Google Scholar] [CrossRef] [PubMed]
- Chirshev, E.; Oberg, K.C.; Ioffe, Y.J.; Unternaehrer, J.J. Let-7 as biomarker, prognostic indicator, and therapy for precision medicine in cancer. Clin. Transl. Med. 2019, 8, 24. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dusaulcy, R.; Handgraaf, S.; Visentin, F.; Vesin, C.; Philippe, J.; Gosmain, Y. Mir-132-3p is a positive regulator of alpha-cell mass and is downregulated in obese hyperglycemic mice. Mol. Metab. 2019, 22, 84–95. [Google Scholar] [CrossRef] [PubMed]
- Arias, N.; Aguirre, L.; Fernández-Quintela, A.; González, M.; Lasa, A.; Miranda, J.; Macarulla, M.; Portillo, M. Micrornas involved in the browning process of adipocytes. J. Physiol. Biochem. 2016, 72, 509–521. [Google Scholar] [CrossRef]
- Mansego, M.L.; Garcia-Lacarte, M.; Milagro, F.I.; Marti, A.; Martinez, J.A. DNA methylation of mirna coding sequences putatively associated with childhood obesity. Pediatric Obes. 2017, 12, 19–27. [Google Scholar] [CrossRef]
- Estep, M.; Armistead, D.; Hossain, N.; Elarainy, H.; Goodman, Z.; Baranova, A.; Chandhoke, V.; Younossi, Z.M. Differential expression of mirnas in the visceral adipose tissue of patients with non-alcoholic fatty liver disease. Aliment. Pharmacol. Ther. 2010, 32, 487–497. [Google Scholar] [CrossRef]
- Frost, R.J.; Olson, E.N. Control of glucose homeostasis and insulin sensitivity by the let-7 family of micrornas. Proc. Natl. Acad. Sci. USA 2011, 108, 21075–21080. [Google Scholar] [CrossRef] [Green Version]
- Mononen, N.; Lyytikainen, L.P.; Seppala, I.; Mishra, P.P.; Juonala, M.; Waldenberger, M.; Klopp, N.; Illig, T.; Leiviska, J.; Loo, B.M.; et al. Whole blood microrna levels associate with glycemic status and correlate with target mrnas in pathways important to type 2 diabetes. Sci. Rep. 2019, 9, 8887. [Google Scholar] [CrossRef]
- Zhu, H.; Shyh-Chang, N.; Segre, A.V.; Shinoda, G.; Shah, S.P.; Einhorn, W.S.; Takeuchi, A.; Engreitz, J.M.; Hagan, J.P.; Kharas, M.G.; et al. The lin28/let-7 axis regulates glucose metabolism. Cell 2011, 147, 81–94. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, B.; Chen, M.Y.; Shen, Y.J.; Zhuo, X.B.; Gao, P.; Zhou, F.S.; Liang, B.; Zu, J.; Zhang, Q.; Suleman, S.; et al. A large-scale, exome-wide association study of han chinese women identifies three novel loci predisposing to breast cancer. Cancer Res. 2018, 78, 3087–3097. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dong, P.; Yu, B.; Pan, L.; Tian, X.; Liu, F. Identification of key genes and pathways in triple-negative breast cancer by integrated bioinformatics analysis. BioMed Res. Int. 2018, 2018, 2760918. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, G.R.; Ku, Y.J.; Cho, S.G.; Kim, S.J.; Min, B.S. Associations between gene expression profiles of invasive breast cancer and breast imaging reporting and data system mri lexicon. Ann. Surg. Treat. Res. 2017, 93, 18–26. [Google Scholar] [CrossRef] [Green Version]
- Yang, M.; Li, H.; Li, Y.; Ruan, Y.; Quan, C. Identification of genes and pathways associated with mdr in mcf-7/mdr breast cancer cells by rna-seq analysis. Mol. Med. Rep. 2018, 17, 6211–6226. [Google Scholar] [CrossRef] [Green Version]
- Denkiewicz, M.; Saha, I.; Rakshit, S.; Sarkar, J.P.; Plewczynski, D. Identification of breast cancer subtype specific micrornas using survival analysis to find their role in transcriptomic regulation. Front. Genet. 2019, 10, 1047. [Google Scholar] [CrossRef] [Green Version]
- Aaroe, J.; Lindahl, T.; Dumeaux, V.; Saebo, S.; Tobin, D.; Hagen, N.; Skaane, P.; Lonneborg, A.; Sharma, P.; Borresen-Dale, A.L. Gene expression profiling of peripheral blood cells for early detection of breast cancer. Breast Cancer Res. 2010, 12, R7. [Google Scholar] [CrossRef] [Green Version]
- Jiang, C.; Wu, S.; Jiang, L.; Gao, Z.; Li, X.; Duan, Y.; Li, N.; Sun, T. Network-based approach to identify biomarkers predicting response and prognosis for her2-negative breast cancer treatment with taxane-anthracycline neoadjuvant chemotherapy. PeerJ 2019, 7, e7515. [Google Scholar] [CrossRef]
- Bjorklund, S.S.; Panda, A.; Kumar, S.; Seiler, M.; Robinson, D.; Gheeya, J.; Yao, M.; Alnaes, G.I.G.; Toppmeyer, D.; Riis, M.; et al. Widespread alternative exon usage in clinically distinct subtypes of invasive ductal carcinoma. Sci. Rep. 2017, 7, 5568. [Google Scholar] [CrossRef]
- Menche, J.; Sharma, A.; Kitsak, M.; Ghiassian, S.D.; Vidal, M.; Loscalzo, J.; Barabasi, A.L. Disease networks. Uncovering disease-disease relationships through the incomplete interactome. Science 2015, 347, 1257601. [Google Scholar] [CrossRef] [Green Version]
| Body Composition | Patients’ Data | Nutritional Status | Patients’ Data |
|---|---|---|---|
| Age (Years) | 55.2 ± 7.2 | Total energy intake(kcal) | 1646 ± 411 |
| SBP (mmHg) | 126.4 ± 13.4 | Carbohydrate (%) | 51.4 ± 14.7 |
| DBP (mmHg) | 83.8 ± 11.9 | Protein (%) | 16.3 ± 2.0 |
| Hear rate (bpm) | 75.0 (68.3, 80.8) | Fat (%) | 28.8 ± 10.6 |
| Metabolic parameters | SFA (%) | 5.2 (2.1, 7.3) | |
| BMI (kg/m2) | 26.0 ± 1.3 | MUFA (%) | 6.1 (4.1, 8.7) |
| Waist circumference(cm) | 87.8 ± 5.6 | PUFA (%) | 8.7 (5.0, 14.8) |
| Skeletal muscle (kg) | 22.2 (21.5, 22.9) | Omega-6 (%) | 0.5 (0.1, 1.6) |
| Fat mass (kg) | 23.4 ± 3.5 | Omega-3 (%) | 2.2 (0.8, 9.3) |
| Fat percentage (%) | 36.3 ± 4.3 | Hormone status | |
| GLTEQ score (MET-h/week) | 9.3 (0, 28) | ER−/PR− | 4 (25%) |
| Glucose (mg/dL) | 90.1 ± 12.0 | ER+/PR− | 2 (12.5%) |
| Insulin (mU/L) | 8.1 ± 2.8 | ER−/PR+ | 1 (6.25%) |
| HOMA-IR | 1.8 ± 0.8 | ER+/PR+ | 9 (56.25%) |
| Total cholesterol (mg/dL) | 198.0 ± 26.3 | Staging | |
| Triglyceride (mg/dL) | 148.4 ± 67.6 | IA | 9(56.3%) |
| HDL cholesterol (mg/dL) | 56.0 ± 9.9 | IIA | 4(25%) |
| LDL cholesterol (mg/dL) | 112.3 ± 24.3 | IIB | 3 (18.7%) |
| MicroRNAs | Log2(FC) | p Value | Putative Target Genes by IPA |
|---|---|---|---|
| hsa-miR-122-5p | 1.095 | <0.001 | AACS, ADAM17, AKT3, ALDOA, ANK2, ANXA11, AP3M2, ATP11A, ATP1A2, BACH2, BCKDK, BCL2L2, CCNG1, CD320, CERS6, CLDN18, CS, DSTYK, DUSP2, EGLN3, ENTPD4, FAM117B, FOXJ3, FOXP1, FUNDC2, G6PC3, GALNT10, GPX7, GYS1, HJV, MAPK11, MECP2, MEP1A, NCAM1, NDRG3, NFATC1, NFATC2IP, NUMBL, OSMR, PALM, RAB11FIP1, RAB6B, RABIF, SLC35A4, SLC7A1, SLC7A11, TBX19, TMED3, TMEM50B, TPD52L2, TRIB1, TRPV6, TTYH3, UBAP2, XPO6 |
| hsa-miR-429 | 1.145 | <0.001 | BAP1, ELMO2, ERBIN, ERRFI1, FHOD1, FOXF2, GEMIN2, GSE1, KLHL20, MARCKS, PLCG1, PPM1F, PTEN, PTPN12, PTPN13, PTPRD, RERE, WASF3, WDR37, ZEB1, ZEB2, ZFPM2 |
| hsa-miR-324-5p | 1.003 | <0.001 | GLI1, RUNX1, SMO, SRF |
| hsa-miR-378d | 0.933 | <0.001 | IGF1R, ODC1, SUFU, TUSC2 |
| hsa-miR-483-5p | 1.019 | <0.001 | ALCAM, ARHGDIA |
| hsa-miR-515-3p | 0.89 | <0.001 | BCL11B, BCOR, BTG1 |
| hsa-miR-519c-3p | 1.007 | <0.001 | ABCG2, AR, PRKAA1 |
| hsa-miR-144-3p | 1.359 | <0.001 | ENPP6 |
| hsa-miR-216a-5p | 0.996 | <0.001 | PTEN |
| hsa-miR-217 | 1.308 | <0.001 | TRPS1 |
| hsa-miR-495-3p | 0.891 | <0.001 | ONECUT1 |
| hsa-miR-504-5p | 1.207 | <0.001 | VEGFA |
| hsa-miR-512-3p | 1.403 | <0.001 | CFLAR |
| hsa-let-7a-5p | −3.794 | <0.001 | AARSD1, ACP1, ADGRG1, AGO4, AKAP8, ANAPC1, ATAD3B, ATP6V0A1, ATP6V1F, AURKB, BCL2L1, BCL7A, BMP2K, BSG, CALCOCO2, CAPG, CARHSP1, CASP3, CCND1, CDC25A, CDIPT, CDK6, CDKAL1, CEMIP2, CHMP2A, CIAO2A, COIL, COL1A2, COMMD9, CSDE1, CSNK1D, DAD1, DHX57, DICER1, DOCK5, DRD3, DSP, DUSP12, DUSP23, EIF3J, EIF4G2, F2, FADS2, FANCD2, FNDC3A, GAK, GEMIN7, GRPEL2, GTPBP3, GYS1, HMGA1, HMGA2, Hmga2, HMOX1, HYOU1, IFIT5, IFRD1, IGF2BP1, IGF2BP2, IGF2BP3, IPO4, ITGB3, KCNJ16, KLK10, KRAS, KRT19, LIN28A, MARS2, MED28, MLLT1, MRM1, MRPS24, MRPS33, MTPN, MTRR, MYC, NEDD4, NF2, NRAS, NXN, OTULINL, PGRMC1, POLD2, POLR2C, POM121/POM121C, PPP1R7, PRDM1, PRIM1, PRRC2A, PTGS2, PXDN, RABGAP1L, RAS, RBM19, RDH10, RHOB, RHOG, RPP38, RRP8, RTCA, SCYL1, SEPT3, SIGMAR1, SLC1A4, SLC25A1, SLC25A13, SLC25A24, SLC25A32, SLC38A1, SMC1A, SMOX, SNAP23, SPCS3, SPRYD4, SYPL1, TAF9B, TAGLN, TGFBR1, THBS1, TLR4, TPM2, TRIM71, TRMT1, TTC9C, TUSC2, TYMS, UGT8, UHRF1, VIM, VPS39, WNT1 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kwon, Y.-J.; Cho, Y.-E.; Cho, A.-R.; Choi, W.J.; Yun, S.; Park, H.; Kim, H.-S.; Cashion, A.K.; Gill, J.; Lee, H.; et al. The Possible Influence of Mediterranean Diet on Extracellular Vesicle miRNA Expression in Breast Cancer Survivors. Cancers 2020, 12, 1355. https://doi.org/10.3390/cancers12061355
Kwon Y-J, Cho Y-E, Cho A-R, Choi WJ, Yun S, Park H, Kim H-S, Cashion AK, Gill J, Lee H, et al. The Possible Influence of Mediterranean Diet on Extracellular Vesicle miRNA Expression in Breast Cancer Survivors. Cancers. 2020; 12(6):1355. https://doi.org/10.3390/cancers12061355
Chicago/Turabian StyleKwon, Yu-Jin, Young-Eun Cho, A-Ra Cho, Won Jun Choi, Sijung Yun, Hyunki Park, Hyung-Suk Kim, Ann K. Cashion, Jessica Gill, Hyangkyu Lee, and et al. 2020. "The Possible Influence of Mediterranean Diet on Extracellular Vesicle miRNA Expression in Breast Cancer Survivors" Cancers 12, no. 6: 1355. https://doi.org/10.3390/cancers12061355
APA StyleKwon, Y.-J., Cho, Y.-E., Cho, A.-R., Choi, W. J., Yun, S., Park, H., Kim, H.-S., Cashion, A. K., Gill, J., Lee, H., & Lee, J.-W. (2020). The Possible Influence of Mediterranean Diet on Extracellular Vesicle miRNA Expression in Breast Cancer Survivors. Cancers, 12(6), 1355. https://doi.org/10.3390/cancers12061355





