Improved Understanding of Interactions between Risk Factors for Child Obesity May Lead to Better Designed Prevention Policies and Programs in Indonesia
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population and Survey
2.2. Case-Control Selection
2.3. Measurements
2.4. Variable Categories
2.5. Statistical Analysis
2.6. Ethical Approvals
3. Results
3.1. Dose-Response Related to Obesity Risk Behaviors
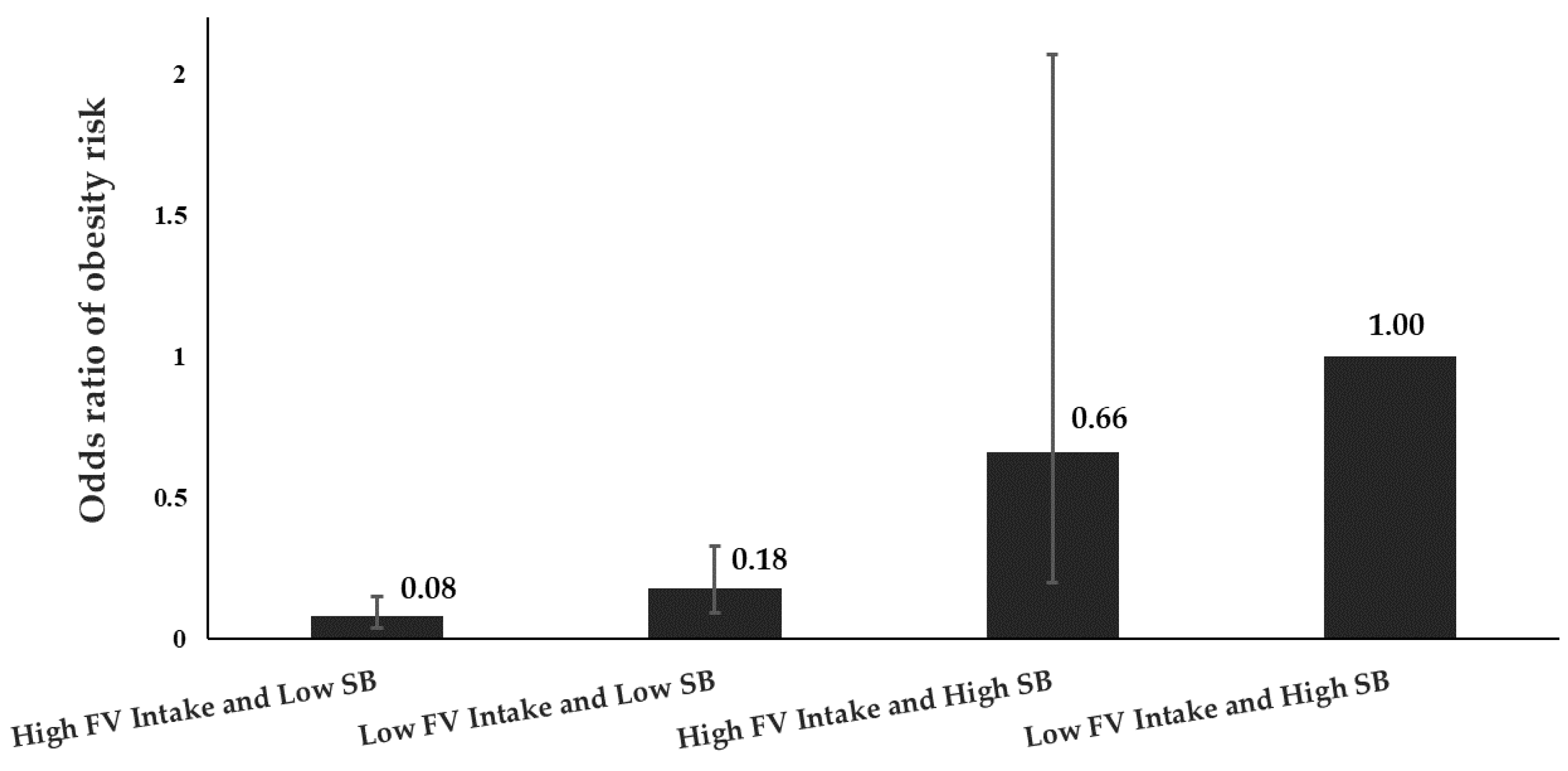
3.2. Interactions between FV Intake and Sedentary Behavior
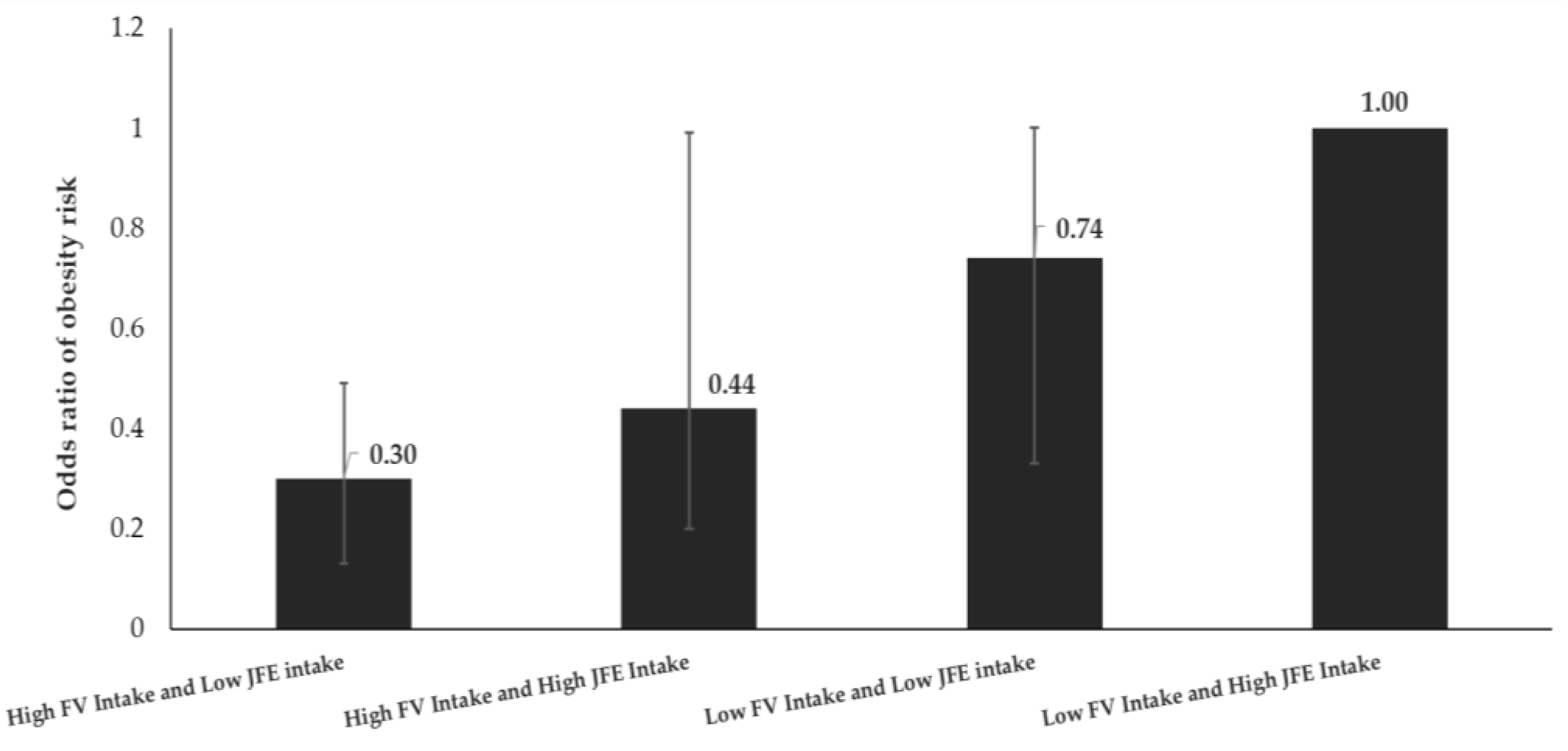
3.3. Interaction between FV Intake and Junk Food Energy Intake
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ng, M.; Fleming, T.; Robinson, M.; Thomson, B.; Graetz, N.; Margono, C.; Mullany, E.C.; Biryukov, S.; Abbafati, C.; Abera, S.F.; et al. Global, regional and national prevalence of overweight and obesity in children and adults 1980–2013: A systematic analysis. Lancet 2014, 384, 766–781. [Google Scholar] [CrossRef]
- WHO. Taking Action on Childhood Obesity Report; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Simmonds, M.; Llewellyn, A.; Owen, C.G.; Woolacott, N. Predicting adult obesity from childhood obesity: A systematic review and meta-analysis. Obes. Rev. 2016, 17, 95–107. [Google Scholar] [CrossRef] [PubMed]
- Gupta, N.; Goel, K.; Shah, P.; Misra, A. Childhood obesity in developing countries: Epidemiology, determinants, and prevention. Endocr. Rev. 2012, 33, 48–70. [Google Scholar] [CrossRef] [PubMed]
- National Institute of Health Research and Development. Riset Kesehatan Dasar (Riskesdas) 2013; National Institute of Health Research and Development: Jakarta, Indonesia, 2013. [Google Scholar]
- National Institute of Health Research and Development. Riset Kesehatan Dasar (Riskesdas) 2018; National Institute of Health Research and Development: Jakarta, Indonesia, 2018. [Google Scholar]
- Roemling, C.; Qaim, M. Obesity trends and determinants in Indonesia. Appetite 2012, 58, 1005–1013. [Google Scholar] [CrossRef] [PubMed]
- Popkin, B.M.; Gordon-Larsen, P. The nutrition transition: Worldwide obesity dynamics and their determinants. Int. J. Obes. 2004, 28, S2–S9. [Google Scholar] [CrossRef] [PubMed]
- Rachmi, C.N.; Li, M.; Alison Baur, L. Overweight and obesity in Indonesia: Prevalence and risk factors—A literature review. Public Health 2017, 147, 20–29. [Google Scholar] [CrossRef] [PubMed]
- Simmonds, M.; Burch, J.; Llewellyn, A.; Griffiths, C.; Yang, H.; Owen, C.; Duffy, S.; Woolacott, N. The use of measures of obesity in childhood for predicting obesity and the development of obesity-related diseases in adulthood: A systematic review and meta-analysis. Health Technol. Assess. (Rockv.) 2015, 19, 43. [Google Scholar] [CrossRef] [PubMed]
- Hall, M.E.; do Carmo, J.M.; da Silva, A.A.; Juncos, L.A.; Wang, Z.; Hall, J.E. Obesity, hypertension, and chronic kidney disease. Int. J. Nephrol. Renovasc. Dis. 2014, 18, 75–88. [Google Scholar] [CrossRef]
- Kepper, M.; Tseng, T.S.; Volaufova, J.; Scribner, R.; Nuss, H.; Sothern, M. Pre-school obesity is inversely associated with vegetable intake, grocery stores and outdoor play. Pediatr. Obes. 2016, 11, e6–e8. [Google Scholar] [CrossRef]
- Nour, M.; Lutze, S.A.; Grech, A.; Allman-Farinelli, M. The Relationship between Vegetable Intake and Weight Outcomes: A Systematic Review of Cohort Studies. Nutrients 2018, 10, 1626. [Google Scholar] [CrossRef]
- Mytton, O.T.; Nnoaham, K.; Eyles, H.; Scarborough, P.; Mhurchu, C.N. Systematic review and meta-analysis of the effect of increased vegetable and fruit consumption on body weight and energy intake. BMC Public Health 2014, 14, 886. [Google Scholar] [CrossRef] [PubMed]
- Nuraeni, I.; Hadi, H.; Paratmanitya, Y. Perbedaan konsumsi buah dan sayur pada anak sekolah dasar yang obes dan tidak obes di Kota Yogyakarta dan Kabupaten Bantul. J. Gizi Dan Diet. Indones. (Indones. J. Nutr. Diet.) 2016, 1, 81–92. [Google Scholar] [CrossRef][Green Version]
- Flood-Obbagy, J.E.; Rolls, B.J. The effect of fruit in different forms on energy intake and satiety at a meal. Appetite 2009, 52, 416–422. [Google Scholar] [CrossRef] [PubMed]
- Chambers, L.; McCrickerd, K.; Yeomans, M.R. Optimising foods for satiety. Trends Food Sci. Technol. 2015, 41, 149–160. [Google Scholar] [CrossRef]
- Perlmutter, D. Guide to the Glycemic Index; David Perlmutter MD: Naples, FL, USA, 2013. [Google Scholar]
- Alkhalidy, H.; Wang, Y.; Liu, D. Dietary flavonoids in the prevention of T2D: An overview. Nutrients 2018, 10, 438. [Google Scholar] [CrossRef] [PubMed]
- Bertoia, M.L.; Rimm, E.B.; Mukamal, K.J.; Hu, F.B.; Willett, W.C.; Cassidy, A. Dietary flavonoid intake and weight maintenance: Three prospective cohorts of 124 086 US men and women followed for up to 24 years. BMJ 2016, 352, i17. [Google Scholar] [CrossRef]
- Panuccio, M.R.; Papalia, T.; Attinà, E.; Giuffrè, A.; Muscolo, A. Use of digestate as an alternative to mineral fertilizer: Effects on growth and crop quality. Arch. Agron. Soil Sci. 2019, 65, 700–711. [Google Scholar] [CrossRef]
- Giuffrè, A.M. Bergamot (Citrus bergamia, Risso): The effects of cultivar and harvest date on functional properties of juice and cloudy juice. Antioxidants 2019, 8, 221. [Google Scholar] [CrossRef]
- Giuffrè, A.M.; Zappia, C.; Capocasale, M. Physicochemical stability of blood orange juice during frozen storage. Int. J. Food Prop. 2017, 20, 1930–1943. [Google Scholar]
- Ioku, K.; Aoyama, Y.; Tokuno, A.; Terao, J.; Nakatani, N.; Takei, Y. Various cooking methods and the flavonoid content in onion. J. Nutr. Sci. Vitaminol. 2001, 47, 78–83. [Google Scholar] [CrossRef]
- Kelly, B.; Hebden, L.; King, L.; Xiao, Y.; Yu, Y.; He, G.; Li, L.; Zeng, L.; Hadi, H.; Karupaiah, T.; et al. Children’s exposure to food advertising on free-to-air television: An Asia-Pacific perspective. Health Promot Int. 2016, 31, 144–152. [Google Scholar] [CrossRef] [PubMed]
- Nurwanti, E. Paparan Iklan Junk Food Dan Pola Konsumsi Junk Food Sebagai Faktor Risiko Terjadinya Obesitas Pada Anak Sekolah Dasar Kota Dan Desa Di Daerah Istimewa Yogyakarta. J. Gizi Dan Diet. Indones. (Indonesian J. Nutr. Diet.) 2013, 1, 59–70. [Google Scholar] [CrossRef][Green Version]
- Costa, C.S.; Del-Ponte, B.; Assunção, M.C.F.; Santos, I.S. Consumption of ultra-processed foods and body fat during childhood and adolescence: A systematic review. Public Health Nutr. 2018, 21, 148–159. [Google Scholar] [CrossRef] [PubMed]
- Payab, M.; Kelishadi, R.; Qorbani, M.; Motlagh, M.E.; Ranjbar, S.H.; Ardalan, G.; Zahedi, H.; Chinian, M.; Asayesh, H.; Larijani, B.; et al. Association of junk food consumption with high blood pressure and obesity in Iranian children and adolescents: The CASPIAN-IV Study. J. Pediatr. (Rio. J.) 2015, 91, 196–205. [Google Scholar] [CrossRef]
- Montoye, A.H.; Pfeiffer, K.A.; Alaimo, K.; Betz, H.H.; Paek, H.J.; Carlson, J.J.; Eisenmann, J.C. Junk food consumption and screen time: Association with childhood adiposity. Am. J. Health Behav. 2013, 37, 395–403. [Google Scholar] [CrossRef]
- WHO. Steps in Applying Probability Proportional to Size (PPS) and Calculating Basic Probability Weights; WHO: Geneva, Switzerland, 2008. [Google Scholar]
- Lwanga, S.K.; Lemeshow, S. Sample Size Determination in Health Studies: A Practical Manual; WHO Library Cataloguing in Publication Data: Geneva, Switzerland, 1991; ISBN 92-4-154405-8. [Google Scholar]
- Arundhana, A.I.; Hadi, H.; Julia, M. Perilaku sedentari sebagai faktor risiko kejadian obesitas pada anak sekolah dasar di Kota Yogyakarta dan Kabupaten Bantul. J. Gizi Dan Diet. Indones. (Indones. J. Nutr. Diet.) 2016, 1, 71–80. [Google Scholar] [CrossRef]
- World Health Organization (WHO). AnthroPlus for Personal Computers. Manual: Software for Assessing Growth of the World’s Children and Adolescents; WHO: Geneva, Switzerland, 2009. [Google Scholar]
- Fatihah, F.; Ng, B.K.; Hazwanie, H.; Karim Norimah, A.; Shanita, S.N.; Ruzita, A.T.; Poh, B.K. Development and validation of a food frequency questionnaire for dietary intake assessment among multi-ethnic primary school-aged children. Singap. Med. J. 2015, 56, 687–694. [Google Scholar] [CrossRef]
- Kalantar-Zadeh, K.; Kovesdy, C.P.; Bross, R.; Benner, D.; Noori, N.; Murali, S.B.; Block, T.; Norris, J.; Kopple, J.D.; Block, G. Design and development of a dialysis food frequency questionnaire. J. Ren. Nutr. 2011, 21, 257–262. [Google Scholar] [CrossRef]
- Corder, K.; Van Sluijs, E.M.F.; Wright, A.; Whincup, P.; Wareham, N.J.; Ekelund, U. Is it possible to assess free-living physical activity and energy expenditure in young people by self-report? Am. J. Clin. Nutr. 2009, 89, 862–870. [Google Scholar] [CrossRef]
- Paffenbarger, R.S.; Blair, S.N.; Lee, I.M.; Hyde, R.T. Measurement of physical activity to assess health effects in free-living populations. Med. Sci. Sports Exerc. 1993, 25, 60–70. [Google Scholar] [CrossRef]
- Ministry of Health. Peraturan Menteri Kesehatan Republik Indonesia Nomor 75 Tahun 2013 Tentang Angka Kecukupan Gizi Yang Dianjurkan Bagi Bangsa Indonesia; Ministry of Health: Jakarta, Indonesia, 2013.
- Heo, M.; Kim, R.S.; Wylie-Rosett, J.; Allison, D.B.; Heymsfield, S.B.; Faith, M.S. Inverse association between fruit and vegetable intake and BMI even after controlling for demographic, socioeconomic and lifestyle factors. Obes. Facts 2011, 4, 449–455. [Google Scholar] [CrossRef] [PubMed]
- Wall, C.R.; Stewart, A.W.; Hancox, R.J.; Murphy, R.; Braithwaite, I.; Beasley, R.; Mitchell, E.A.; Gómez, M.; Weyler, J.; Pinto-Vargas, R.; et al. Association between Frequency of Consumption of Fruit, Vegetables, Nuts and Pulses and BMI: Analyses of the International Study of Asthma and Allergies in Childhood (ISAAC). Nutrients 2018, 10, 316. [Google Scholar] [CrossRef] [PubMed]
- Ledoux, T.A.; Hingle, M.D.; Baranowski, T. Relationship of fruit and vegetable intake with adiposity: A systematic review. Obes. Rev. 2011, 12, e143–e150. [Google Scholar] [CrossRef]
- Rautiainen, S.; Wang, L.; Lee, I.; Manson, J.; Buring, J.; Sesso, H. Higher Intake of Fruit, but Not Vegetables or Fiber, at Baseline Is Associated with Lower Risk of Becoming Overweight or Obese in Middle-Aged and Older Women of Normal BMI at Baseline. J. Nutr. 2015, 145, 960–968. [Google Scholar] [CrossRef] [PubMed]
- Collings, P.J.; Kelly, B.; West, J.; Wright, J. Associations of TV Viewing Duration, Meals and Snacks Eaten When Watching TV, and a TV in the Bedroom with Child Adiposity. Obesity 2018, 26, 1619–1628. [Google Scholar] [CrossRef]
- Feldman, S.; Eisenberg, M.E.; Neumark-Sztainer, D.; Story, M. Associations between Watching TV during Family Meals and Dietary Intake Among Adolescents. J. Nutr. Educ. Behav. 2007, 39, 257–263. [Google Scholar] [CrossRef]
- Popkin, B.M. The Nutrition Transition in the Developing World. Dev. Policy Rev. 2003, 21, 581–597. [Google Scholar] [CrossRef]
- Drewnowski, A.; Popkin, B.M. The Nutrition Transition: New Trends in the Global Diet. Nutr. Rev. 1997, 55, 31–43. [Google Scholar] [CrossRef]
- Popkin, B.M.; Adair, L.S.; Ng, S.W. Global nutrition transition and the pandemic of obesity in developing countries. Nutr. Rev. 2012, 70, 3–21. [Google Scholar] [CrossRef]
- Februhartanty, J. Nutrition transition: What challenges are faced by Indonesia? In Proceedings of the International Public Health Seminar, Palembang, Indonesia, 10–13 November 2011. [Google Scholar]
- Roemling, C.; Qaim, M. Dual burden households and intra-household nutritional inequality in Indonesia. Econ. Hum. Biol. 2013, 11, 563–573. [Google Scholar] [CrossRef]
- Lipoeto, N.I.; Geok Lin, K.; Angeles-Agdeppa, I. Food consumption patterns and nutrition transition in South-East Asia. Public Health Nutr. 2013, 16, 1637–1643. [Google Scholar] [CrossRef] [PubMed]
- Nurwanti, E.; Hadi, H.; Arundhana, A.I.; Gittelsohn, J. Fruit and Vegetable Intakes and Sedentary Behavior in Indonesian School Children and Adolescents. Unpublished work. 2019. [Google Scholar]
- Gordis, L. Epidemiology, 5th ed.; Elsevier Saunders: Philadelphia, PA, USA, 2013; ISBN 9781416040026. [Google Scholar]
- Nusaresearch. Report on Fast Food in Major Cities in Indonesia; PT Nusaresearch: Jakarta, Indonesia, 2014. [Google Scholar]
- Jackson, P.; Romo, M.M.; Castilio, A.M.; Castillo-Durán, C. Junk food consumption and child nutrition in Chile. Rev. Med. Chil. 2004, 132, 1235–1242. [Google Scholar] [PubMed]
- Martin, M.; Schlosser, E. Fast Food Nation: The Dark Side of the All-American Meal. J. Public Health Policy 2003, 24, 61–63. [Google Scholar] [CrossRef]
- Caspi, C.E.; Lenk, K.; Pelletier, J.E.; Barnes, T.L.; Harnack, L.; Erickson, D.J.; Laska, M.N. Association between store food environment and customer purchases in small grocery stores, gas-marts, pharmacies and dollar stores. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 76. [Google Scholar] [CrossRef]
| Obese a | %/Mean ± SE | Non-Obese b | %/Mean ± SE | χ2/t | p-Value | |
|---|---|---|---|---|---|---|
| Gender | ||||||
| Females | 90 | 42.5 | 122 | 57.5 | 8.54 | 0.003 |
| Males | 154 | 55.8 | 122 | 44.2 | ||
| Children’s age | ||||||
| ≥10 years | 106 | 49.5 | 108 | 50.5 | 0.03 | 0.855 |
| <10 years | 138 | 50.4 | 136 | 49.6 | ||
| School location | ||||||
| Bantul | 78 | 50.0 | 78 | 50.0 | 0.00 | 1 |
| Yogyakarta | 166 | 50.0 | 166 | 50.0 | ||
| Mother’s age | ||||||
| ≥40 years | 98 | 51.6 | 92 | 48.4 | 0.31 | 0.578 |
| <40 years | 146 | 49.0 | 152 | 51.0 | ||
| Mother’s education | ||||||
| Elementary school | 13 | 41.9 | 18 | 58.1 | 1.58 | 0.663 |
| Junior high school | 31 | 47.0 | 35 | 53.0 | ||
| Senior high school | 101 | 49.8 | 102 | 50.2 | ||
| University | 99 | 52.7 | 89 | 47.3 | ||
| Mother’s job | ||||||
| Unemployment | 101 | 47.6 | 111 | 52.4 | 10.34 | 0.066 |
| Farm workers | 10 | 43.5 | 13 | 56.5 | ||
| Private employee | 31 | 49.2 | 32 | 50.8 | ||
| Government employee | 30 | 68.2 | 14 | 31.8 | ||
| Entrepreneur | 64 | 52.9 | 57 | 47.1 | ||
| Others | 8 | 32.0 | 17 | 68.0 | ||
| Father’s age | ||||||
| ≥40 years | 142 | 49.8 | 143 | 50.2 | 0.01 | 0.927 |
| <40 years | 102 | 50.2 | 101 | 49.8 | ||
| Father’s education | ||||||
| Elementary school | 11 | 50.0 | 11 | 50.0 | 1.41 | 0.703 |
| Junior high school | 25 | 43.1 | 33 | 56.9 | ||
| Senior high school | 98 | 50.0 | 98 | 50.0 | ||
| University | 108 | 51.9 | 100 | 48.1 | ||
| TV ownership | ||||||
| None or 1 TV | 108 | 46.0 | 127 | 54.0 | 2.96 | 0.085 |
| >1 TV | 136 | 53.8 | 117 | 46.2 | ||
| Household Monthly Expenditure (Rp) | 244 | 2,519,699 ± 96,892 | 244 | 2,611,081 ± 158,086 | 0.50 | 0.622 |
| Mean of sedentary time (hours/d) | 244 | 5.3 ± 0.052 | 244 | 4.4 ± 0.06 | −10.8 | <0.001 |
| Mean of Fruit-and-Vegetable intake (serving/d) | 244 | 2.39 ± 0.12 | 244 | 3.35 ± 0.17 | 4.6 | <0.001 |
| Mean Fast Food Energy Intake (kcal/d) | 169 | 155.2 ± 14.6 | 161 | 112.4 ± 11.0 | −2.3 | 0.0210 |
| Mean Junk Food Energy Intake (kcal/d) | 244 | 821.2 ± 32.7 | 244 | 702.6 ± 23.4 | −2.9 | 0.0034 |
| Risk Factors | Obese n (%) | Non-Obese n (%) | Crude OR a (95% CI) | Adjusted OR b (95% CI) | Adjusted OR c (95% CI) | |
|---|---|---|---|---|---|---|
| Fruit & Vegetable intake as dichotomous variable | <3 serving/d | 155 (57.0) | 117 (43.0) | Ref | Ref | |
| ≥3 serving/d | 89 (41.2) | 127 (58.8) | 0.53 (0.37–0.76) | 0.46 (0.30–0.69) | ||
| Junk Food Energy (JFE) Intake as a dichotomous variable | ≥1050 kcal/d | 66 (58.9) | 46 (41.1) | Ref | Ref | |
| <1050 kcal/d | 178 (47.3) | 198 (52.7) | 0.63 (0.41–0.96) | 0.61 (0.37–0.98) | ||
| Sedentary Behavior as a dichotomous variable | ≥5 h/d | 155 (71.4) | 62 (28.6) | Ref | Ref | |
| <5 h/d | 89 (32.8) | 182 (67.2) | 0.20 (0.13–0.29) | 0.18 (0.12–0.28) | ||
| Fruit & Vegetable Intake | Never/d | 40 (69.0) | 18 (31.0) | Ref | Ref | |
| 1 serving/d | 52 (62.7) | 31 (37.4) | 0.75 (0.37–1.53) | 0.72 (0.32–1.60) | ||
| 2 serving/d | 63 (48.1) | 68 (51.9) | 0.42 (0.21–0.80) | 0.36 (0.17–0.77) | ||
| ≥3 serving/d | 89 (41.2) | 127 (58.8) | 0.31 (0.17–0.59) | 0.25 (0.12–0.50) | ||
| Junk Food Energy (JFE) Intake | High (≥1050 kcal/d) | 66 (58.9) | 46 (41.1) | Ref | Ref | |
| Moderate (700–1049 kcal/d) | 57 (53.8) | 49 (46.2) | 0.81 (0.47–1.39) | 0.69 (0.37–1.28) | ||
| Low (<700 kcal/d) | 121 (44.8) | 149 (55.2) | 0.57 (036–0.88) | 0.53 (0.28–0.99) | ||
| Sedentary Behavior | High (≥ 5 h/d) | 155 (71.4) | 62 (28.6) | Ref | Ref | |
| Moderate (3.75–<5 h/d) | 77 (35.8) | 138 (64.2) | 0.22 (0.15–0.33) | 0.19 (0.12–0.30) | ||
| Mild (<3.75 h/d) | 12 (21.4) | 44 (78.6) | 0.10 (0.05–0.22) | 0.09 (0.04–0.19) | ||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hadi, H.; Nurwanti, E.; Gittelsohn, J.; Arundhana, A.I.; Astiti, D.; West, K.P., Jr.; Dibley, M.J. Improved Understanding of Interactions between Risk Factors for Child Obesity May Lead to Better Designed Prevention Policies and Programs in Indonesia. Nutrients 2020, 12, 175. https://doi.org/10.3390/nu12010175
Hadi H, Nurwanti E, Gittelsohn J, Arundhana AI, Astiti D, West KP Jr., Dibley MJ. Improved Understanding of Interactions between Risk Factors for Child Obesity May Lead to Better Designed Prevention Policies and Programs in Indonesia. Nutrients. 2020; 12(1):175. https://doi.org/10.3390/nu12010175
Chicago/Turabian StyleHadi, Hamam, Esti Nurwanti, Joel Gittelsohn, Andi Imam Arundhana, Dewi Astiti, Keith P. West, Jr., and Michael J. Dibley. 2020. "Improved Understanding of Interactions between Risk Factors for Child Obesity May Lead to Better Designed Prevention Policies and Programs in Indonesia" Nutrients 12, no. 1: 175. https://doi.org/10.3390/nu12010175
APA StyleHadi, H., Nurwanti, E., Gittelsohn, J., Arundhana, A. I., Astiti, D., West, K. P., Jr., & Dibley, M. J. (2020). Improved Understanding of Interactions between Risk Factors for Child Obesity May Lead to Better Designed Prevention Policies and Programs in Indonesia. Nutrients, 12(1), 175. https://doi.org/10.3390/nu12010175





