Commercial Postural Devices: A Review
Abstract
1. Introduction
2. Principles of Wearable Devices in Posture Analysis
2.1. Accelerometers
2.2. Gyroscope
2.3. Magnetometers
2.4. Inertial Measurement Units
2.5. Movement Classification
2.6. Sensor Placement
3. Validity and Reliability of Wearable Devices for Postural Analysis
Biomechanical Studies in Postural Analysis
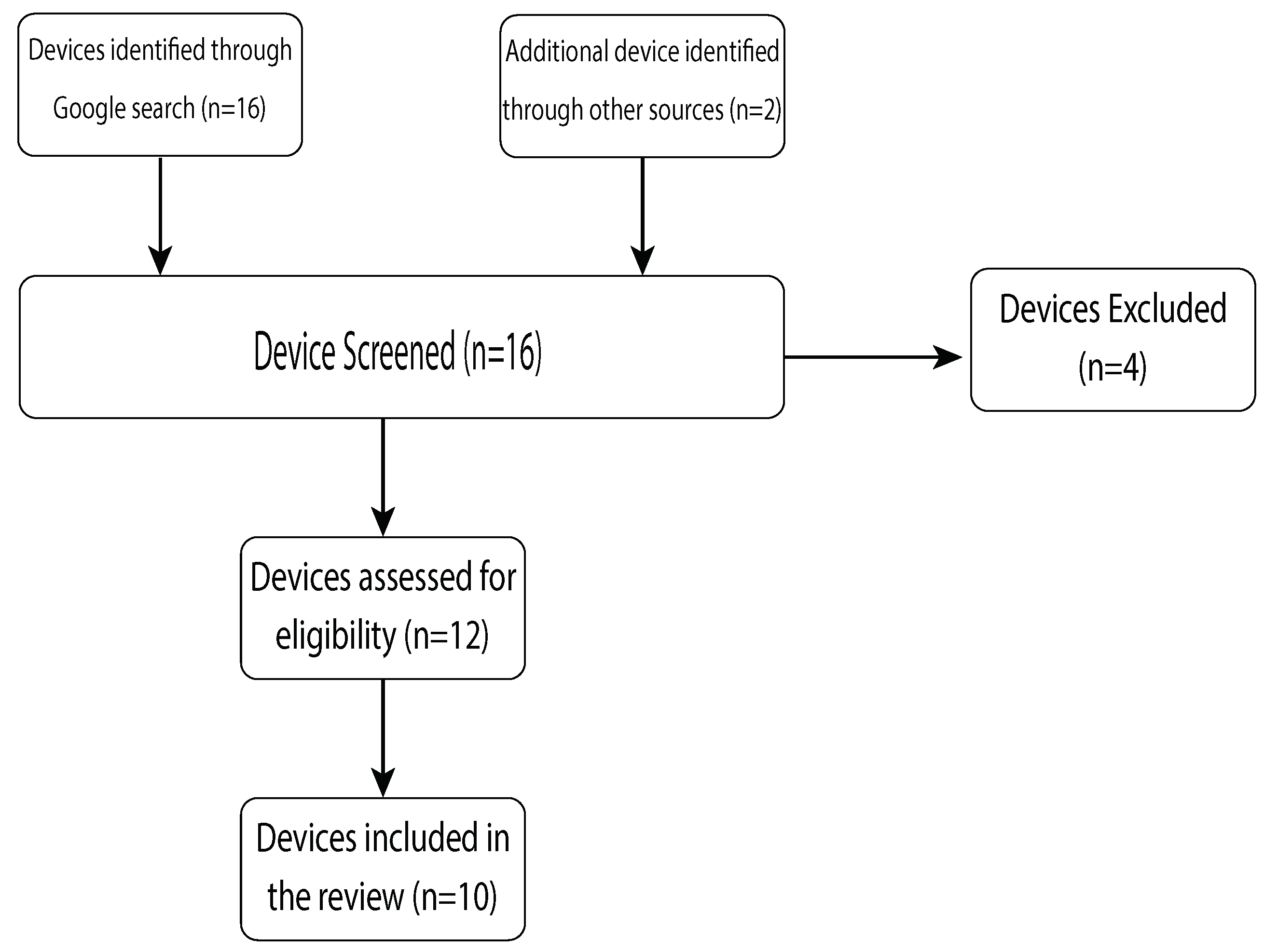
4. Methodology—Device Market Review
5. Commercially Available Postural Devices
5.1. Upright Go
5.2. Lumo Back
5.3. Lumo Lift
5.4. Zikto Walk
5.5. Prana
5.6. Jins Meme
5.7. Alex+
5.8. Nadi X
5.9. Sense-U
6. Clinical Applicability
6.1. Prevention of Spinal Conditions
6.2. Monitoring of Spinal Conditions
6.3. Treating Spinal Conditions
6.4. Other Uses of Posture Wearables in Healthcare
6.4.1. Falls Risk Assessment
6.4.2. Fall Detection
6.5. The Use of Wearables in Other Diseases
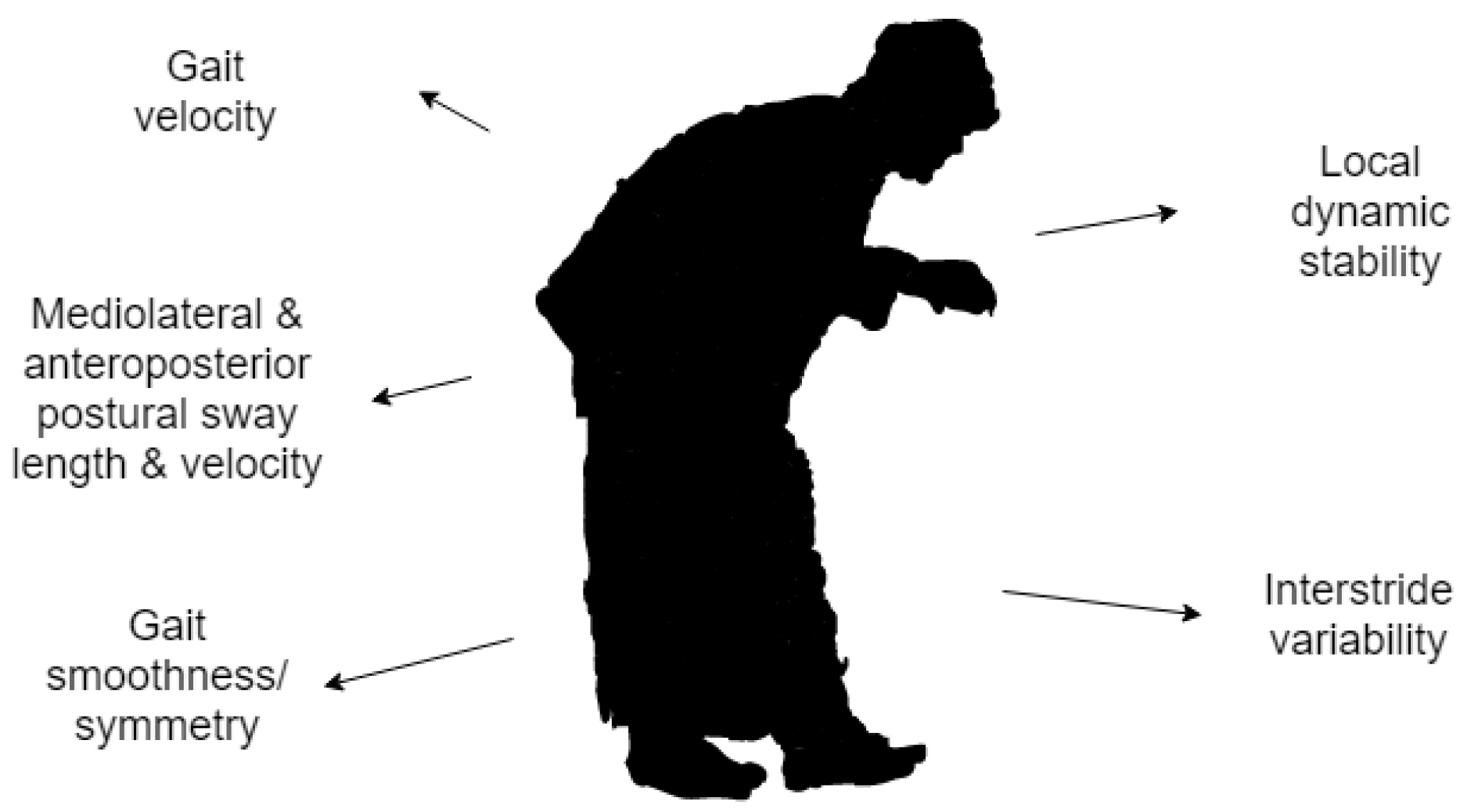
Parkinson’s Disease
6.6. Multiple Sclerosis
6.7. Stroke
7. Discussion
7.1. Challenges and Future Steps in Wearable Technology
7.2. Posture Wearables and Telemedicine
8. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Gilman, S.L. “Stand Up Straight”: Notes toward a history of posture. J. Med. Humanit. 2014, 35, 57–83. [Google Scholar] [CrossRef]
- White, T.D.; Asfaw, B.; Beyene, Y.; Haile-Selassie, Y.; Lovejoy, C.O.; Suwa, G.; WoldeGabriel, G. Ardipithecus Ramidus and the Paleobiology of Early Hominids. Science 2015, 326, 75–86. [Google Scholar] [CrossRef]
- Lockhart, T.E.; Soangra, R.; Zhang, J.; Wu, X. Wavelet based automated postural event detection and activity classification with single IMU. Biomed. Sci. Instrum. 2013, 49, 224–233. [Google Scholar]
- Simpson, L.; Maharaj, M.M.; Mobbs, R.J. The role of wearables in spinal posture analysis: A systematic review. BMC Musculoskelet. Disord. 2019, 20, 55. [Google Scholar] [CrossRef] [PubMed]
- Cureton, T.K., Jr. Bodily posture as an indicator of fitness. Res. Q. Am. Assoc. Health Phys. Educ. 1941, 12, 348–367. [Google Scholar] [CrossRef]
- Patel, M.S.; Asch, D.A.; Volpp, K.G. Wearable Devices as Facilitators, Not Drivers, of Health Behavior Change. JAMA 2015, 313, 459–460. [Google Scholar] [CrossRef] [PubMed]
- Piwek, L.; Ellis, D.A.; Andrews, S.; Joinson, A. The Rise of Consumer Health Wearables: Promises and Barriers. PLoS Med. 2016, 13, e1001783. [Google Scholar] [CrossRef] [PubMed]
- Insight, C. Optimistic Outlook for Wearables. 2019. Available online: https://www.ccsinsight.com/press/company-news/optimistic-outlook-for-wearables/ (accessed on 12 March 2019).
- Zhao, H.; Wang, Z. Motion measurement using inertial sensors, ultrasonic sensors, and magnetometers with extended kalman filter for data fusion. Eters Ext. 2011, 12, 943–953. [Google Scholar] [CrossRef]
- Cheung, V.H.; Gray, L.; Karunanithi, M. Review of accelerometry for determining daily activity among elderly patients. Arch. Phys. Med. Rehabil. 2011, 92, 998–1014. [Google Scholar] [CrossRef]
- Yang, C.C.; Hsu, Y.L. A review of accelerometry-based wearable motion detectors for physical activity monitoring. Sensors 2010, 10, 7772–7788. [Google Scholar] [CrossRef]
- Karantonis, D.M.; Narayanan, M.R.; Mathie, M.; Lovell, N.H.; Celler, B.G. Implementation of a real-time human movement classifier using a triaxial accelerometer for ambulatory monitoring. IEEE Trans. Inf. Technol. Biomed. 2006, 10, 156–167. [Google Scholar] [CrossRef] [PubMed]
- Lyons, G.M.; Culhane, K.M.; Hilton, D.; Grace, P.A.; Lyons, D. A description of an accelerometer-based mobility monitoring technique. Med. Eng. Phys. 2005, 27, 497–504. [Google Scholar] [CrossRef] [PubMed]
- Najafi, B.; Aminian, K.; Loew, F.; Blanc, Y.; Robert, P.A. Measurement of stand-sit and sit-stand transitions using a miniature gyroscope and its application in fall risk evaluation in the elderly. IEEE Trans. Biomed. Eng. 2002, 49, 843–851. [Google Scholar] [CrossRef]
- Incel, O. Analysis of movement, orientation and rotation-based sensing for phone placement recognition. Sensors 2015, 15, 25474–25506. [Google Scholar] [CrossRef]
- Sabatini, A.M. Quaternion-based extended Kalman filter for determining orientation by inertial and magnetic sensing. IEEE Trans. Biomed. Eng. 2006, 5, 1346–1356. [Google Scholar] [CrossRef]
- Felisberto, F.; Pereira, A. A Ubiquitous and Low-Cost Solution for Movement Monitoring and Accident Detection Based on Sensor Fusion. Sensors 2014, 14, 8961–8983. [Google Scholar] [CrossRef]
- Abyarjoo, F.; O-Larnnithipong, N.; Tangnimitchok, S.; Ortega, F.; Barreto, A. PostureMonitor: Real-Time IMU Wearable Technology to Foster Poise and Health. In Proceedings of the International Conference of Design, User Experience, and Usability, Los Angeles, CA, USA, 2–7 August 2015; pp. 543–552. [Google Scholar]
- Mathie, M.J.; Celler, B.G.; Lovell, N.H.; Coster, A.C.F. Classification of basic daily movements using a triaxal accelerometer. Med. Biol. Eng. Comput. 2004, 42, 679–687. [Google Scholar] [CrossRef]
- Wang, Z.; Yang, Z.; Dong, T. A review of wearable technologies for elderly care that can accurately track indoor position, recognize physical activities and monitor vital signs in real time. Sensors 2017, 17, 341. [Google Scholar] [CrossRef]
- Takasaki, H. Habitual pelvic posture and time spent sitting: Measurement test-retest reliability for the LUMOback device and preliminary evidence for slouched posture in individuals with low back pain. SAGE Open Med. 2017, 5. [Google Scholar] [CrossRef]
- Lugade, V.; Fortune, E.; Morrow, M.; Kaufman, K. Validity of using tri-axial accelerometers to measure human movement—Part I: Posture and movement detection. Med. Eng. Phys. 2014, 36, 169–176. [Google Scholar] [CrossRef]
- Koumantakis, G.A.; Nikoloudaki, M.; Thacheth, S.; Zagli, K.; Bitrou, K.; Nigritinos, A.; Botton, L. Reliability and Validity Measurement of Sagittal Lumbosacral Quiet Standing Posture with a Smartphone Application in a Mixed Population of 183 College Students and Personnel. Adv. Orthop. 2016, 2016. [Google Scholar] [CrossRef] [PubMed]
- Milani, P.; Coccetta, C.A.; Rabini, A.; Sciarra, T.; Massazza, G.; Ferriero, G. Mobile Smartphone Applications for Body Position Measurement in Rehabilitation: A Review of Goniometric Tools. PM&R 2014, 6, 1038–1043. [Google Scholar]
- Salamh, P.A.; Kolber, M. The reliability, minimal detectable change and concurrent validity of a gravity-based bubble inclinometer and iphone application for measuring standing lumbar lordosis. Physiother. Theory Pract. 2014, 30, 62–67. [Google Scholar] [CrossRef] [PubMed]
- Birsan, J.; Stavarache, D.; Dascalu, M.I.; Moldoveanu, A. SpiMO-Sitting Posture Monitoring System. In RoCHI 2017, 143–146. [Google Scholar]
- Park, S.; Hetzler, T.; Hammons, D.; Ward, G. Effects of biofeedback postural training on pre-existing low back pain in static-posture workers. J. Back Musculoskelet. 2018, 31, 849–857. [Google Scholar] [CrossRef]
- Hellstrom, P.A.R.; Åkerberg, A.; Folke, M. Posture sensor as feedback when lifting weights. In Proceedings of the 4th International Conference on Ambulatory Monitoring of Physical Activity and Movement, ICAMPAM 2015, Limerick, Ireland, 10–12 June 2015. [Google Scholar]
- Rhee, S.Y.; Chon, S.; Ahn, K.J.; Woo, J.T.; Korean Diabetes Prevention Study Investigators. Hospital-Based Korean Diabetes Prevention Study: A Prospective, Multi-Center, Randomized, Open-Label Controlled Study. Diabetes Metab. J. 2019, 43, 49–58. [Google Scholar] [CrossRef]
- Hansraj, K.K. Assessment of stresses in the cervical spine caused by posture and position of the head. Surg. Technol. Int. 2014, 25, 277–279. [Google Scholar]
- Kroemer, K.H.E. Personnel training for safer material handling. Ergonomics 1992, 35, 1119–1134. [Google Scholar] [CrossRef]
- Dunne, L.E.; Walsh, P.; Hermann, S.; Smyth, B.; Caulfield, B. Wearable monitoring of seated spinal posture. IEEE Trans. Biomed. Circuits Syst. 2008, 2, 97–105. [Google Scholar] [CrossRef]
- Yan, X.; Li, H.; Li, A.R.; Zhang, H. Wearable IMU-based real-time motion warning system for construction workers’ musculoskeletal disorders prevention. Autom. Constr. 2017, 74, 2–11. [Google Scholar] [CrossRef]
- Chakravorty, A.; Mobbs, R.J.; Anderson, D.B.; Rooke, K.; Phan, K.; Yoong, N.; Maharaj, M.; Choy, W.J. The role of wearable devices and objective gait analysis for the assessment and monitoring of patients with lumbar spinal stenosis: systematic review. BMC Musculoskelet. Disord. 2019, 20, 288. [Google Scholar] [CrossRef] [PubMed]
- Mobbs, R.J.; Mobbs, R.R.; Choy, W.J. Proposed objective scoring algorithm for assessment and intervention recovery following surgery for lumbar spinal stenosis based on relevant gait metrics from wearable devices: The Gait Posture index (GPi). J. Spine Surg. 2019, 5, 300–309. [Google Scholar] [CrossRef] [PubMed]
- Miladi, L. Round and angular kyphosis in paediatric patients. Orthop. Traumatol. Surg. Res. 2013, 99, 140–149. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Garoflid, N.; Fragniere, B.; Dutoit, M. “Round back” in children and adolescents. Rev. Med. Suisse 2000, 120, 815–820. [Google Scholar]
- Briggs, A.M.; Wrigley, T.V.; Tully, E.A.; Adams, P.E.; Greig, A.M.; Bennell, K.L. Radiographic measures of thoracic kyphosis in osteoporosis: Cobb and vertebral centroid angles. Skeletal Radiol. 2007, 36, 761–767. [Google Scholar] [CrossRef]
- Lewis, J.S.; Valentine, R.E. Clinical measurement of the thoracic kyphosis. A study of the intra-rater reliability in subjects with and without shoulder pain. BMC Musculoskelet. Disord. 2010, 11, 39. [Google Scholar] [CrossRef]
- Kamaci, S.; Yucekul, A.; Demirkiran, G. The evolution of sagittal spinal alignment in sitting position during childhood. Spine 2015, 40, 787–793. [Google Scholar] [CrossRef]
- Feng, Q.; Wang, M.; Zhang, Y.; Zhou, Y. The effect of a corrective functional exercise program on postural thoracic kyphosis in teenagers: A randomized controlled trial. Clin. Rehabil. 2018, 32, 48–56. [Google Scholar] [CrossRef]
- Howcroft, J.; Kofman, J.; Lemaire, E.D. Review of fall risk assessment in geriatric populations using inertial sensors. J. Neuroeng. Rehabil. 2013, 10, 91. [Google Scholar] [CrossRef]
- Del Din, S.; Godfrey, A.; Rochester, L. Validation of an accelerometer to quantify a comprehensive battery of gait characteristics in healthy older adults and Parkinson’s disease: Toward clinical and at home use. IEEE J. Biomed. Health 2015, 20, 838–847. [Google Scholar] [CrossRef]
- Rigas, G.; Tzallas, A.T.; Tsipouras, M.G.; Bougia, P.; Tripoliti, E.E.; Baga, D.; Fotiadis, D.I.; Tsouli, S.G.; Konitsiotis, S. Assessment of tremor activity in the Parkinson’s disease using a set of wearable sensors. IEEE Trans. Inf. Technol. Biomed. 2012, 16, 478–487. [Google Scholar] [CrossRef] [PubMed]
- Maetzler, W.; Domingos, J.; Srulijes, K.; Ferreira, J.J.; Bloem, B.R. Quantitative wearable sensors for objective assessment of Parkinson’s disease. Mov. Disord. 2013, 28, 1628–1637. [Google Scholar] [CrossRef] [PubMed]
- Chen, B.R.; Patel, S.; Buckley, T.; Rednic, R.; McClure, D.J.; Shih, L.; Tarsy, D.; Welsh, M.; Bonato, P. A web-based system for home monitoring of patients with Parkinson’s disease using wearable sensors. IEEE Trans. Biomed. Eng. 2010, 58, 831–836. [Google Scholar] [CrossRef] [PubMed]
- Quach, L.; Galica, A.M.; Jones, R.N.; Procter-Gray, E.; Manor, B.; Hannan, M.T.; Lipsitz, L.A. The nonlinear relationship between gait speed and falls: the maintenance of balance, independent living, intellect, and zest in the elderly of Boston study. J. Am. Geriatr. Soc. 2011, 59, 1069–1073. [Google Scholar] [CrossRef] [PubMed]
- Rispens, S.M.; van Schooten, K.S.; Pijnappels, M.; Daffertshofer, A.; Beek, P.J.; van Dieen, J.H. Identification of fall risk predictors in daily life measurements: Gait characteristics’ reliability and association with self-reported fall history. Neurorehabil. Neural Repair 2015, 29, 54–61. [Google Scholar] [CrossRef]
- Gregg, E.W.; Pereira, M.A.; Caspersen, C.J. Physical activity, falls, and fractures among older adults: A review of the epidemiologic evidence. J. Am. Geriatr. Soc. 2000, 48, 883–893. [Google Scholar] [CrossRef]
- Pierleoni, P.; Belli, A.; Palma, L.; Pellegrini, M.; Pernini, L.; Valenti, S. A high reliability wearable device for elderly fall detection. IEEE Sens. J. 2015, 15, 4544–4553. [Google Scholar] [CrossRef]
- Shany, T.; Redmond, S.J.; Narayanan, M.R.; Lovell, N.H. Sensors-based wearable systems for monitoring of human movement and falls. IEEE Sens. J. 2011, 12, 658–670. [Google Scholar] [CrossRef]
- Jankovic, J. Parkinson’s disease: Clinical features and diagnosis. J. Neurol. Neurosurg. Psychiatry 2008, 79, 368–376. [Google Scholar] [CrossRef]
- Mirelman, A.; Herman, T.; Nicolai, S.; Zijlstra, A.; Zijlstra, W.; Becker, C.; Chiari, L.; Hausdorff, J.M. Audio-biofeedback training for posture and balance in patients with Parkinson’s disease. J. Neuroeng. Rehabil. 2011, 8, 35. [Google Scholar] [CrossRef]
- Nanhoe-Mahabier, W.; Allum, J.H.; Pasman, E.P.; Overeem, S.; Bloem, B.R. The effects of vibrotactile biofeedback training on trunk sway in Parkinson’s disease patients. Parkinsonism Relat. Disord. 2012, 18, 1017–1021. [Google Scholar] [CrossRef] [PubMed]
- Carpinella, I.; Cattaneo, D.; Bonora, G.; Bowman, T.; Martina, L.; Montesano, A.; Ferrarin, M. Wearable sensor-based biofeedback training for balance and gait in Parkinson disease: A pilot randomized controlled trial. Arch. Phys. Med. Rehabil. 2017, 98, 622–630. [Google Scholar] [CrossRef] [PubMed]
- Cameron, M.H.; Lord, S. Postural control in multiple sclerosis: Implications for fall prevention. Curr. Neurol. Neurosci. Rep. 2010, 10, 407–412. [Google Scholar] [CrossRef]
- Sun, R.; Moon, Y.; McGinnis, R.S.; Seagers, K.; Motl, R.W.; Sheth, N.; Wright, J.A.; Ghaffari, R.; Patel, S.; Sosnoff, J.J. Assessment of postural sway in individuals with multiple sclerosis using a novel wearable inertial sensor. Digit. Biomark. 2018, 2, 1–10. [Google Scholar] [CrossRef]
- Brodie, M.A.; Psarakis, M.; Hoang, P. Gyroscopic corrections improve wearable sensor data prior to measuring dynamic sway in the gait of people with Multiple Sclerosis. Comput. Methods Biomech. Biomed. Engin. 2016, 19, 1339–1346. [Google Scholar] [CrossRef]
- Masse, F.; Gonzenbach, R.; Paraschiv-Ionescu, A.; Luft, A.R.; Aminian, K. Wearable barometric pressure sensor to improve postural transition recognition of mobility-impaired stroke patients. IEEE Trans. Neural Syst. Rehabil. Eng. 2016, 24, 1210–1217. [Google Scholar] [CrossRef]
- Karnath, H.O.; Broetz, D. Understanding and treating “pusher syndrome”. Phys. Ther. 2003, 83, 1119–1125. [Google Scholar]
- Arteaga, S.; Chevalier, J.; Coile, A.; Hill, A.W.; Sali, S.; Sudhakhrisnan, S.; Kurniawan, S.H. Low-cost accelerometry-based posture monitoring system for stroke survivors. In Proceedings of the 10th International ACM SIGACCESS Conference on Computers and Accessibility, Halifax, NS, Canada, 13–15 October 2008; pp. 243–244. [Google Scholar]
- Edgar, S.R.; Swyka, T.; Fulk, G.; Sazonov, E.S. Wearable shoe-based device for rehabilitation of stroke patients. In Proceedings of the 2010 Annual International Conference of the IEEE Engineering in Medicine and Biology, Buenos Aires, Argentina, 31 August– 4 September 2010; pp. 3722–3775. [Google Scholar]
- Giorgino, T.; Lorussi, F.; De Rossi, D.; Quaglini, S. Posture classification via wearable strain sensors for neurological rehabilitation. Conf. Proc. IEEE Eng. Med. Biol. Soc. 2006, 1, 6273–6276. [Google Scholar]
- Chang, H.C.; Hsu, Y.L.; Yang, S.C.; Lin, J.C.; Wu, Z.H. A wearable inertial measurement system with complementary filter for gait analysis of patients with stroke or Parkinson’s disease. IEEE 2016, 4, 8442–8453. [Google Scholar] [CrossRef]
- Nielsen, C. Tech-Styles: Are Consumers Really Interested in Wearing Tech on Their Sleeves. 2014. Available online: http://www. nielsen.com/us/en/newswire/2014/tech-styles-are-consumers-really-interested-in-wearing-tech-on-their-sleeves.html (accessed on 10 May 2019).
- Yip, H.L.; Fattah, I.R.; Yuen, A.C.; Yang, W.; Medwell, P.R.; Kook, S.; Yeoh, G.H.; Chan, Q.N. Flame–wall interaction effects on diesel post-injection combustion and soot formation processes. Energy Fuels 2019, 33, 7759–7769. [Google Scholar] [CrossRef]
- Yip, H.L.; Srna, A.; Yuen, A.C.Y.; Kook, S.; Taylor, R.A.; Yeoh, G.H.; Medwell, P.R.; Chan, Q.N. A Review of Hydrogen Direct Injection for Internal Combustion Engines: Towards Carbon-Free Combustion. Appl. Sci. 2019, 9, 4842. [Google Scholar] [CrossRef]
- Nielsen, D.; McCaffrey, D. Endeavour Partners Report: Inside Wearables: How the Science of Human Behavior Change Offers the Secret toLong-term Engagement. 2014. Available online: http://endeavourpartners.net/assets/Wearables-and-the-Science-of-Human-Behavior-Change-EP4.pdf (accessed on 10 May 2019).
- Argent, R.; Slevin, P.; Bevilacqua, A.; Neligan, M.; Daly, A.; Caulfield, B. Wearable Sensor-Based Exercise Biofeedback for Orthopaedic Rehabilitation: A Mixed Methods User Evaluation of a Prototype System. Sensors 2019, 19, 432. [Google Scholar] [CrossRef] [PubMed]
- Rao, P.J.; Phan, K.; Maharaj, M.M.; Pelletier, M.H.; Walsh, W.R.; Mobbs, R.J. Accelerometers for objective evaluation of physical activity following spine surgery. J. Clin. Neurosci. 2016, 26, 14–18. [Google Scholar] [CrossRef] [PubMed]
| Components | Function |
|---|---|
| Accelerometer | Measure proper acceleration: |
| — Gravitational force (static) and sensor movement (dynamic) | |
| — At least 1-D accelerometer | |
| Gyroscope | Measure angular velocity: |
| — At least 1-D gyroscope | |
| Magnetometer | Measure all magnetic fields: |
| — Optional |
| DoF | IMU Components |
|---|---|
| 9 | 3-D accelerometer, 3-D gyroscope & 3-D magnetometer: |
| — Most accurate type → able to measure proper acceleration, angular | |
| velocity and magnetic fields in three axes | |
| 6 | 3-D accelerometer & 3-D gyroscope: |
| — Less accurate than 9 DoF → lower accuracy in determining sensor orientation | |
| 5 | 3-D accelerometer & 2-D gyroscope: |
| — Less accurate than 6 DoF → gyroscope cannot measure in third dimension | |
| 4 | 3-D accelerometer & 1-D gyroscope: |
| — Less accurate than 5 DoF → gyroscope can only measure in one dimension |
| Upright Go | Upright Go 2 | LumoLift | LumoBack | Alex | Nadi X | Sense-U | Zikto Walk | Prana | Jins Meme | |
|---|---|---|---|---|---|---|---|---|---|---|
| Size (mm) | 55.3 × 33.2 | 48 × 28 | 44 × 25 | 415 × 100 | 80 × 160 | NA | 35.6 × 35.6 | 13.6 × 47.3 | 31.8 × 6.4 | NA |
| (Length × Width × Height) | ×11.6 | ×8.6 | ×13 | × 8 | ×170 | ×10.2 | ×11.1 | (Height × diameter) | ||
| Weight (g) | 12 | 11 | 13.6 | 25 | 25 | NA | 11.34 | 17.5 | I.N.A. | 36 |
| Accelerometer (acc.) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 1 |
| Type of acc. | NA | NA | MEMS | NA | MEMS | MEMS | NA | NA | I.N.A. | MEMS |
| No. of acc. axis | 3 | NA | 3 | 3 | NA | 3 | NA | 3 | 3 | 3 |
| Gyroscope (gyro.) | NA | 1 | NA | NA | NA | NA | NA | 1 | I.N.A. | 1 |
| Type of gyro. | NA | NA | NA | NA | NA | NA | NA | NA | I.N.A. | MEMS |
| No. of gyro. axis | – | – | – | – | – | – | – | 3 | – | 3 |
| Magnetometer (mgm.) | NA | NA | NA | NA | NA | NA | NA | NA | I.N.A. | 1 |
| Type of mgm. | NA | NA | NA | NA | NA | NA | NA | NA | I.N.A. | I.N.A. |
| No. of mgm. axis | – | – | – | – | – | – | – | I.N.A. | – | 3 |
| Sensor location | Upper back | Upper back | Clavicle | Waist | Neck | Hips, knees, ankles | Clavicle | Wrist | Waist | Nose bridge, ears |
| Battery type | Lithium (Li) ion | Li polymer | Li polymer | Li polymer | Li | Li ion | Li | Li polymer | Li ion | Li ion |
| Battery life (hours) | 12 | 30 | 96 | 120–168 | 168 | 1.5 | 240 | 72–120 | 168 | 16 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yoong, N.K.M.; Perring, J.; Mobbs, R.J. Commercial Postural Devices: A Review. Sensors 2019, 19, 5128. https://doi.org/10.3390/s19235128
Yoong NKM, Perring J, Mobbs RJ. Commercial Postural Devices: A Review. Sensors. 2019; 19(23):5128. https://doi.org/10.3390/s19235128
Chicago/Turabian StyleYoong, Nicole Kah Mun, Jordan Perring, and Ralph Jasper Mobbs. 2019. "Commercial Postural Devices: A Review" Sensors 19, no. 23: 5128. https://doi.org/10.3390/s19235128
APA StyleYoong, N. K. M., Perring, J., & Mobbs, R. J. (2019). Commercial Postural Devices: A Review. Sensors, 19(23), 5128. https://doi.org/10.3390/s19235128