Induction of Biofilm Formation in Klebsiella pneumoniae ATCC 13884 by Several Drugs: The Possible Role of Quorum Sensing Modulation
Abstract
1. Introduction
2. Materials and Methods
2.1. General
2.1.1. Drug Selection
2.1.2. Bacteria
2.1.3. Equipment
2.2. Effect of Drugs on K. pneumoniae ATCC 13884 Growth
2.3. Effect of Drugs on K. pneumoniae ATCC 13884 Biofilm Formation
2.3.1. Kinetics of Biofilm Formation
2.3.2. Biofilm Formation
2.4. Production of N-Hexanoyl-Homoserine Lactone, C6-AHL
2.4.1. Detection Using the Biosensor C. violaceum CV026
2.4.2. Detection of C6-AHL by HPLC/MS
2.4.3. Kinetics of C6-AHL Production
2.4.4. Production of C6-AHL in K. pneumoniae ATCC 13884 after Drug Treatment
2.5. Effect of Drugs on the Resistance of K. pneumoniae ATCC 13884 Mature Biofilms
2.5.1. Minimum Antibiotic Concentration Required to Eliminate Mature Biofilms
2.5.2. Mature Biofilms Formed under Biofilm-Inducing Drugs
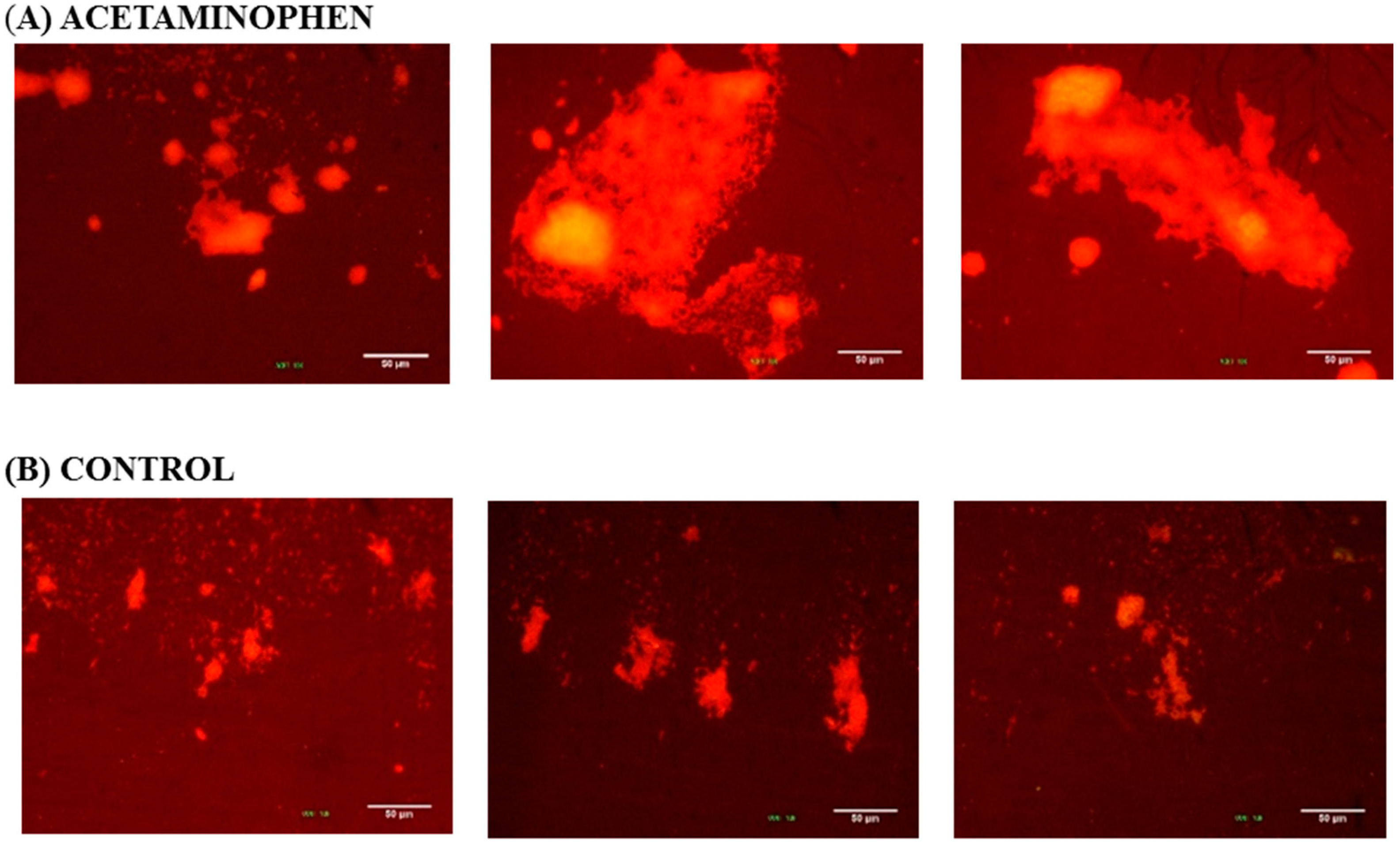
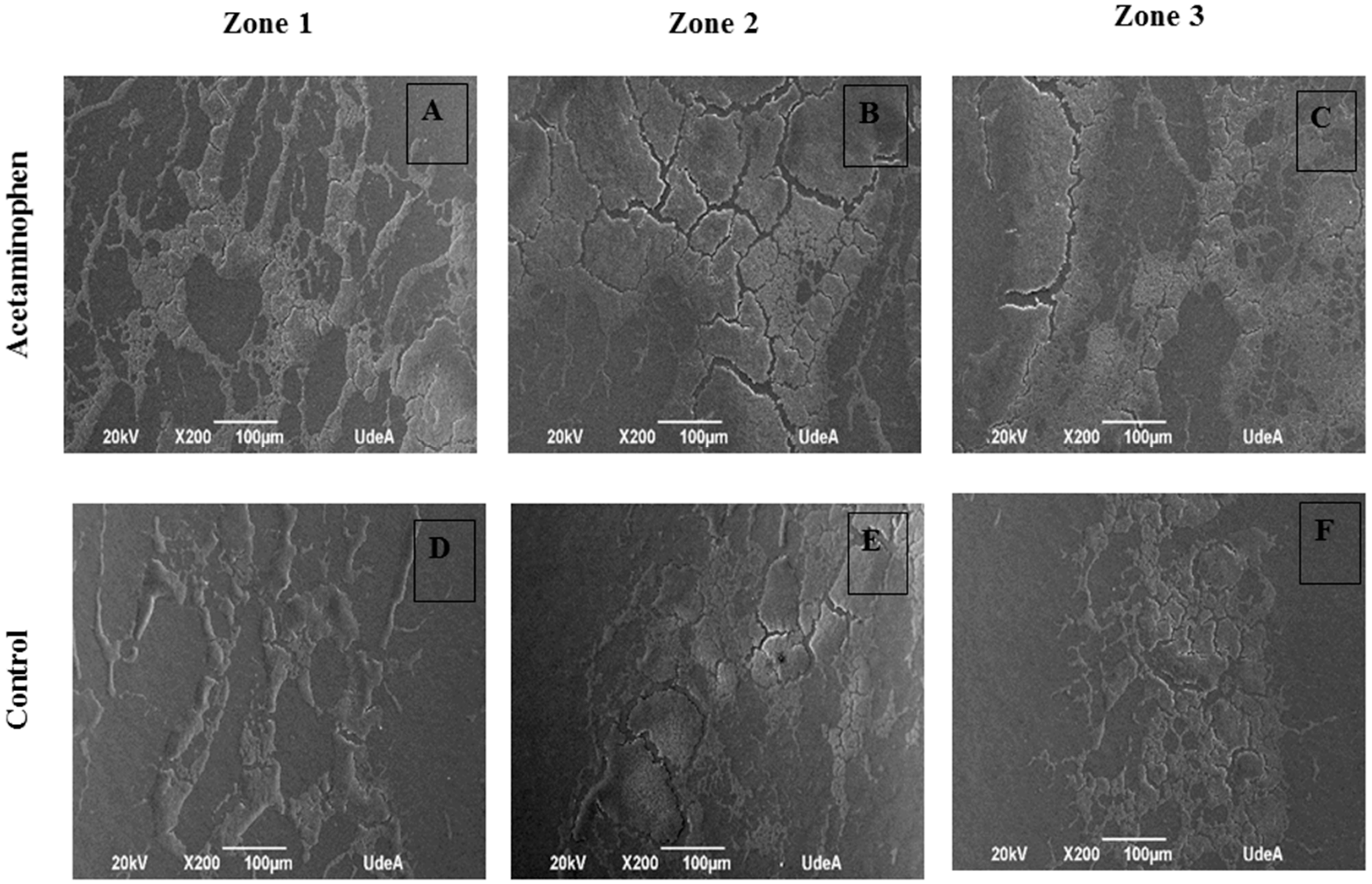
2.5.3. Architecture of the Mature Biofilm
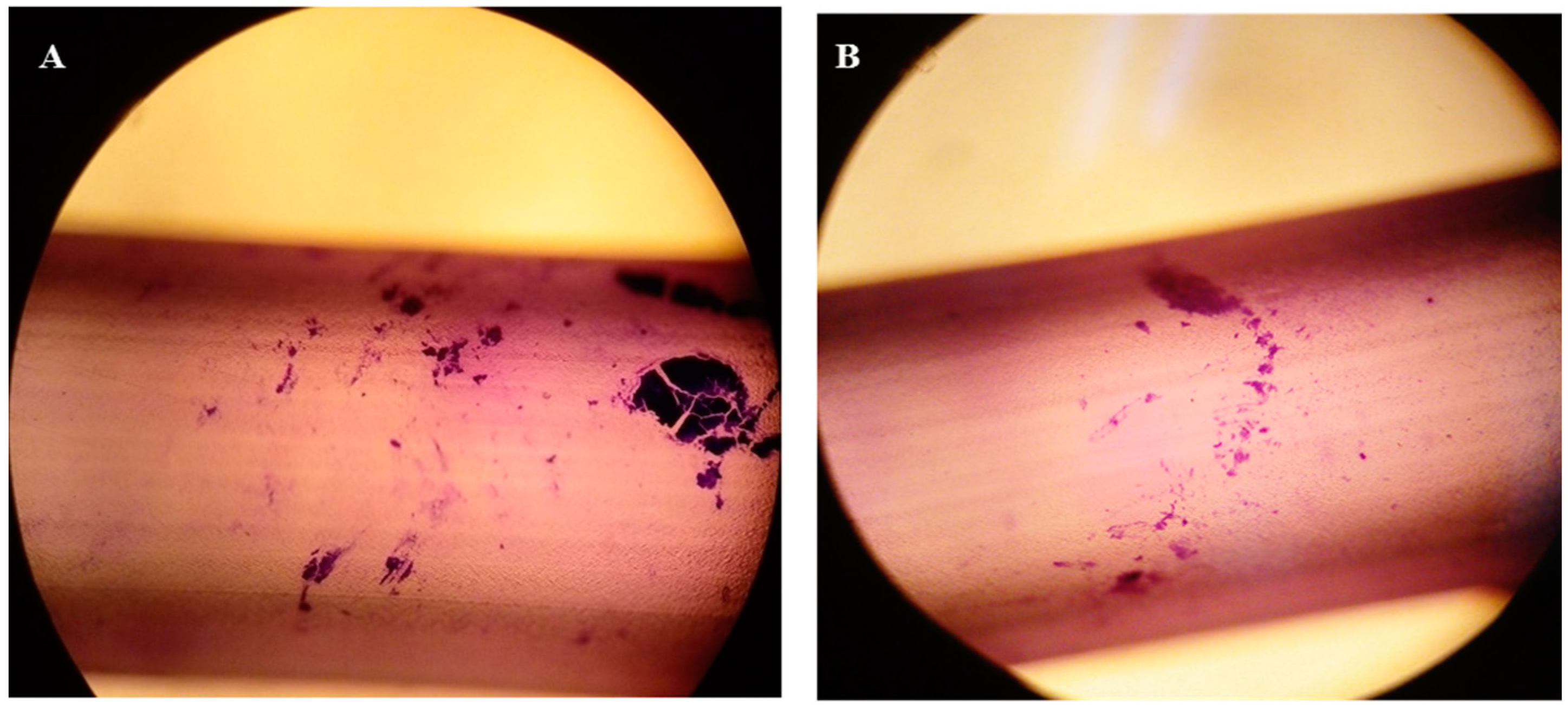
2.6. Effect of Acetaminophen on K. pneumoniae ATCC 13884 Adherence to Urethral Catheters
2.7. Statistical Analysis
3. Results
3.1. Effect of Drugs on K. pneumoniae ATCC 13884 Growth
3.2. Effect of Drugs on K. pneumoniae ATCC 13884 Biofilm Formation
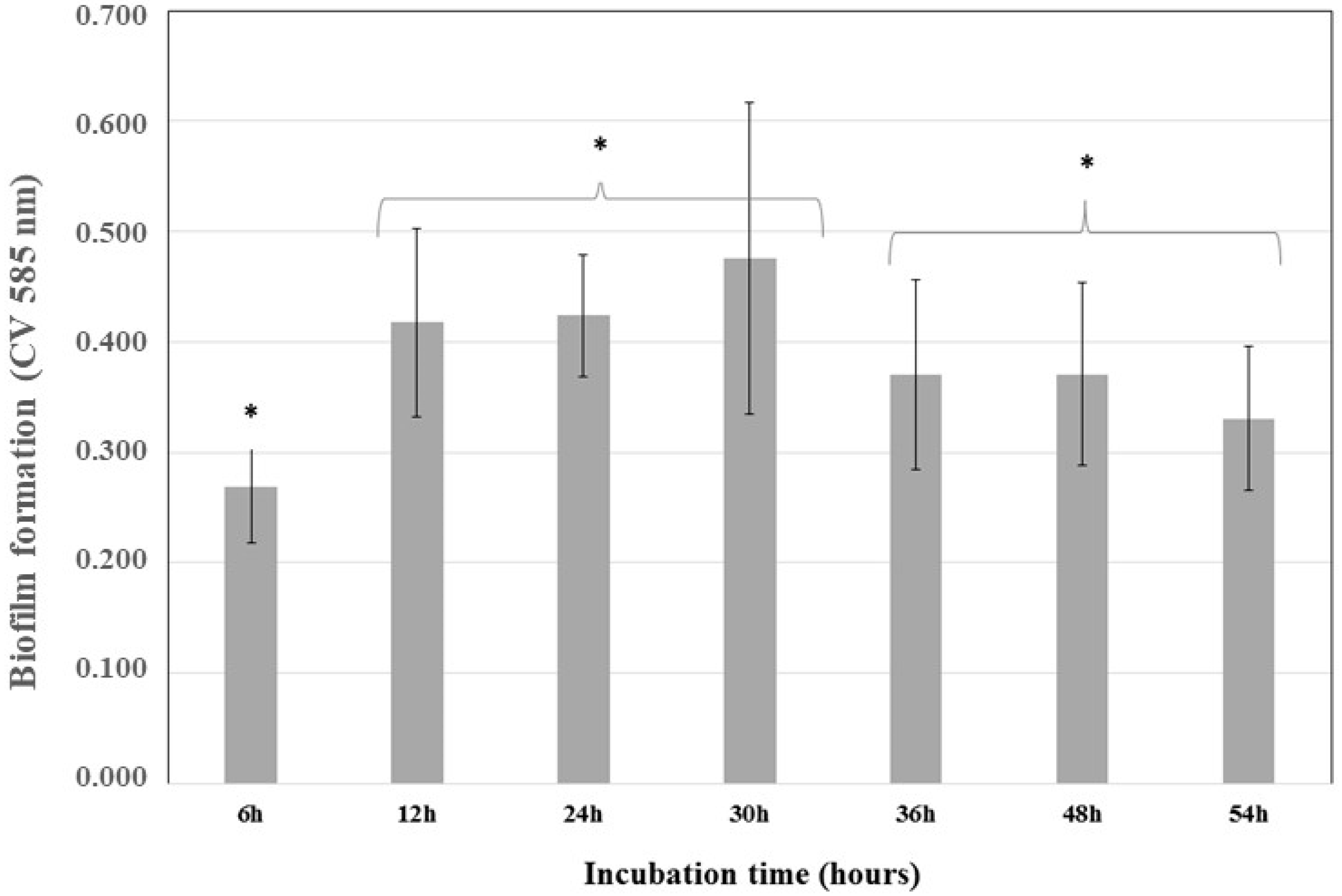
3.2.1. Kinetics of Biofilm Formation
3.2.2. Biofilm Formation
3.3. Production of C6-AHL
3.3.1. Detection of C6-AHL through the Biosensor C. violaceum
3.3.2. Detection by HPLC/MS
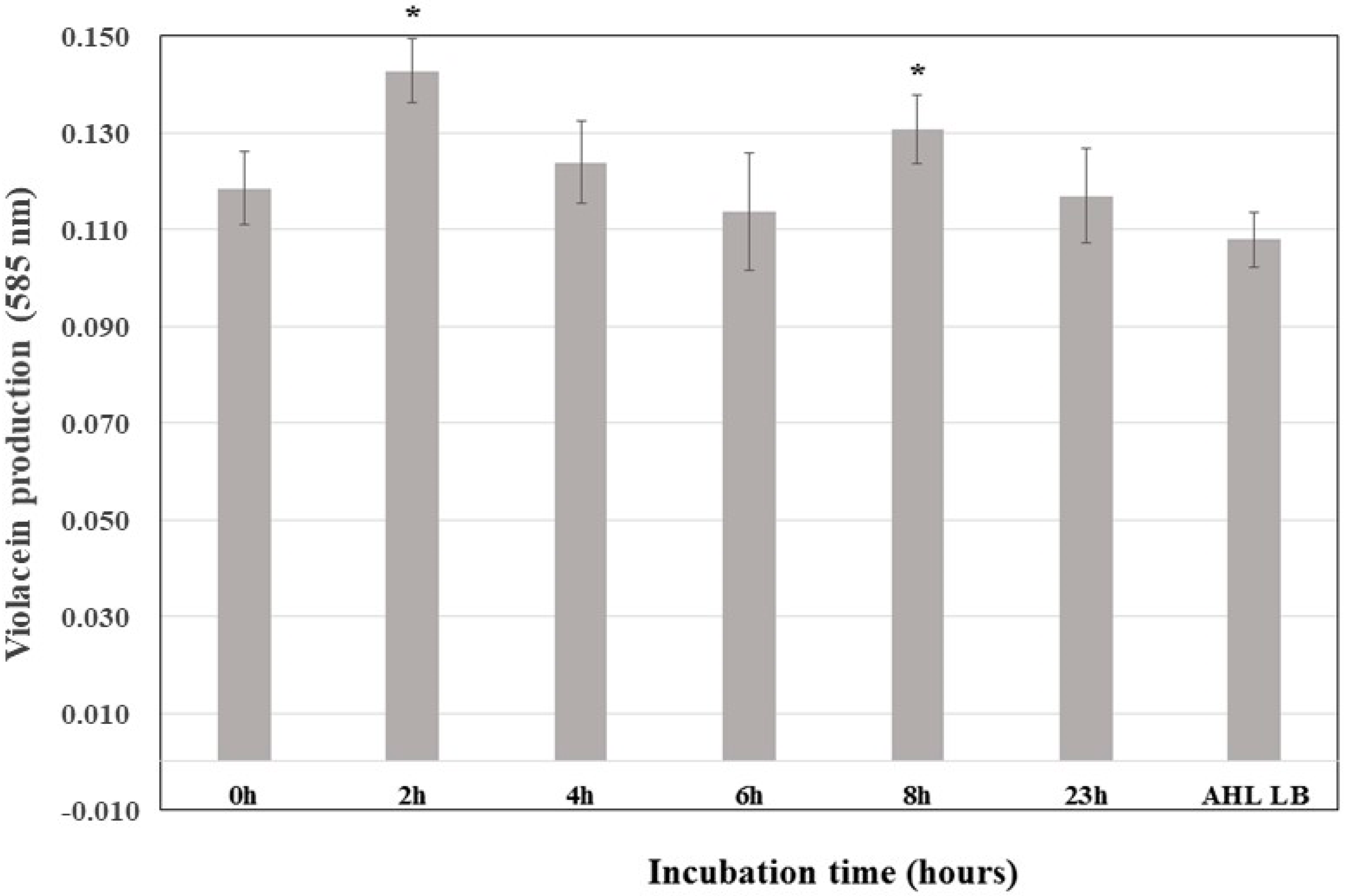
3.3.3. Kinetics of C6-AHL Production in K. pneumoniae ATCC 13884
3.3.4. Production of C6-AHL in K. pneumoniae ATCC 13884 after Drug Treatments
3.4. Effect of Drugs on Mature Biofilm Resistance in K. pneumoniae ATCC 13884
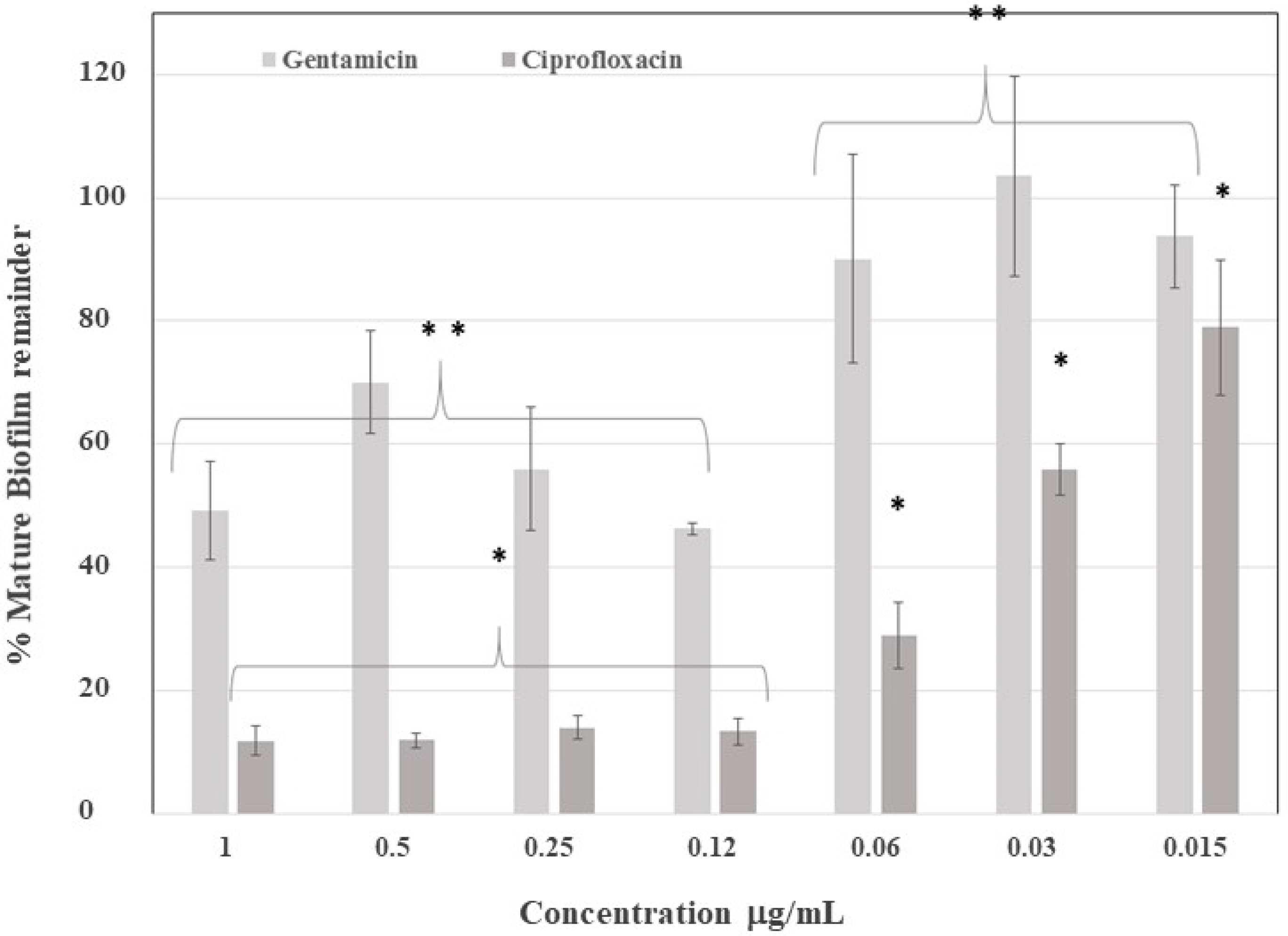
3.4.1. Minimum Antibiotic Concentration Required to Eliminate Mature Biofilms
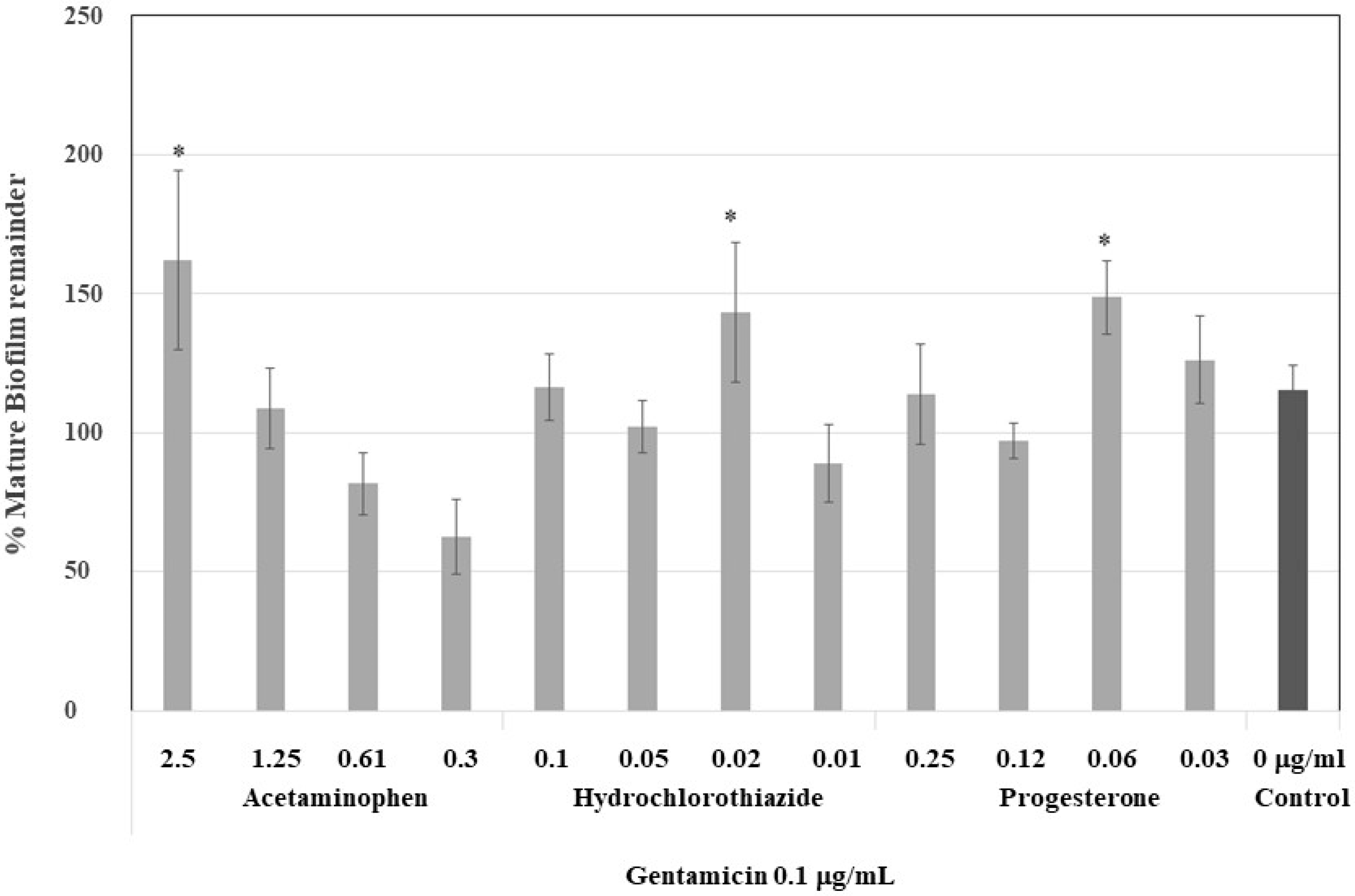
3.4.2. Effect of Antibiotics on Mature Biofilm Formed by Drugs
3.4.3. Effect on Mature Biofilm Architecture
3.5. Effect of the Drugs on K. pneumoniae ATCC 13884 Adherence to Urethral Catheters
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- McConville, T.H.; Sullivan, S.B.; Gomez-Simmonds, A.; Whittier, S.; Uhlemann, A.C. Carbapenem-resistant Enterobacteriaceae colonization (CRE) and subsequent risk of infection and 90-day mortality in critically ill patients, an observational study. PLoS ONE 2017, 12, e0186195. [Google Scholar] [CrossRef] [PubMed]
- Bandeira, B.; Borges, V.; Gomes, J.P.; Duarte, A.; Jordao, L. Insights on Klebsiella pneumoniae biofilms assembled on different surfaces using phenotypic and genotypic approaches. Microorganism 2017, 5, 16. [Google Scholar] [CrossRef] [PubMed]
- Bonkat, G.; Pickard, R.; Bartoletti, R.; Bruyère, F.; Geerlings, S.E.; Wagenlehner, F.; Wullt, B.; Cai, T.; Köves, B.; Pilatz, A.; et al. EAU Guidelines on Urological Infections. Available online: https://uroweb.org/wp-content/uploads/Urological-Infections-2017-pocket.pdf (accessed on 21 November 2018).
- World Health Organization (WHO). Antimicrobial Resistance. Global Report on Surveillance; WHO Library Cataloguing-in-Publication Data; WHO: Geneva, Switzerland, 2014. [Google Scholar]
- Abraham, W.R. Going beyond the control of quorum-sensing to combat biofilm infections. Antibiotics 2016, 5, 3. [Google Scholar] [CrossRef] [PubMed]
- Papenfort, K.; Bassler, B.L. Quorum sensing signal-response systems in Gram-negative bacteria. Nat. Rev. Microbiol. 2016, 14, 576–588. [Google Scholar] [CrossRef] [PubMed]
- Vuotto, C.; Longo, F.; Pascolini, C.; Donelli, G.; Balice, M.P.; Libori, M.F.; Tiracchia, V.; Salvia, A.; Varaldo, P.E. Biofilm formation and antibiotic resistance in Klebsiella pneumoniae urinary strains. J. Appl. Microbiol. 2017, 123, 1003–1018. [Google Scholar] [CrossRef] [PubMed]
- Soto, S.M. Importance of biofilms in urinary tract infections: New therapeutic approaches. J. Adv. Biol 2014, 2014. [Google Scholar] [CrossRef]
- Whiteley, M.; Diggle, S.P.; Greenberg, E.P. Progress in and promise of bacterial quorum sensing research. Nature 2017, 551, 313–320. [Google Scholar] [CrossRef] [PubMed]
- Wiegand, I.; Hilpert, K.; Hancock, R.E. Agar and broth dilution methods to determine the minimal inhibitory concentration (MIC) of antimicrobial substances. Nat. Protoc. 2008, 3, 163–175. [Google Scholar] [CrossRef] [PubMed]
- O’Toole, G.A. Microtiter Dish Biofilm Formation Assay. J. Vis. Exp. 2011, 47, 2437. [Google Scholar] [CrossRef] [PubMed]
- Yin, W.F.; Purmal, K.; Chin, S.; Chan, X.Y.; Koh, C.L.; Sam, C.K.; Chan, K.G. N-acyl homoserine lactone production by Klebsiella pneumoniae isolated from human tongue surface. Sensors 2012, 12, 3472–3483. [Google Scholar] [CrossRef] [PubMed]
- Vuotto, C.; Longo, F.; Balice, M.P.; Donelli, G.; Varaldo, P.E. Antibiotic resistance related to biofilm formation in Klebsiella pneumoniae. Pathogens 2014, 3, 743–758. [Google Scholar] [CrossRef] [PubMed]
- Anderl, J.N.; Franklin, M.J.; Stewart, P.S. Role of antibiotic penetration limitation in Klebsiella pneumoniae biofilm resistance to ampicillin and ciprofloxacin. Antimicrob. Agents Chemother. 2000, 44, 1818–1824. [Google Scholar] [CrossRef] [PubMed]
- Pitout, J.D.; Nordmann, P.; Poirel, L. Carbapenemase-producing Klebsiella pneumoniae, a key pathogen set for global nosocomial dominance. Antimicrob. Agents Chemother. 2015, 59, 5873–5884. [Google Scholar] [CrossRef] [PubMed]
- Stahlhut, S.G.; Struve, C.; Krogfelt, K.A.; Reisner, A. Biofilm formation of Klebsiella pneumoniae on urethral catheters requires either type 1 or type 3 fimbriae. FEMS Immunol. Med. Microbiol. 2012, 65, 350–359. [Google Scholar] [CrossRef] [PubMed]
- Solomon, S.L.; Oliver, K.B. Antibiotic resistance threats in the United States: Stepping back from the brink. Am. Fam. Physician 2014, 89, 938–941. [Google Scholar] [PubMed]
- Allegaert, K.; Mariska, Y.; Peeters, M.Y.; Beleyn, B.; Smits, A.; Kulo, A.; Van Calsteren, K.; Deprest, J.; De Hoon, J.; Knibbe, C.A.J. Paracetamol pharmacokinetics and metabolism in young women. BMC Anesthesiol. 2015, 15, 163. [Google Scholar] [CrossRef] [PubMed]
- Hennessy, E.; Adams, C.; Reen, F.J.; O’Gara, F. Is there potential for repurposing statins as novel antimicrobials? Antimicrob. Agents Chemother. 2016, 60, 5111–5121. [Google Scholar] [CrossRef] [PubMed]
- Reslinski, A.; Dabrowiecki, S.; Glowacka, K. The impact of diclofenac and ibuprofen on biofilm formation on the surface of polypropylene mesh. Hernia 2015, 19, 179–185. [Google Scholar] [CrossRef] [PubMed]
- Bellifa, S.; Hassaine, H.; Balestrino, D.; Charbonnel, N.; M’hamedi, I.; Terki, I.K.; Lachachi, M.; Didi, W.; Forestier, C. Evaluation of biofilm formation of Klebsiella pneumoniae isolated from medical devices at the University Hospital of Tlemcen, Algeria. Afr. J. Microbiol. Res. 2013, 7, 5558–5564. [Google Scholar]
- Rasmussen, T.B.; Givskov, M. Quorum-sensing inhibitors as anti-pathogenic drugs. Int. J. Med. Microbiol. 2006, 296, 149–161. [Google Scholar] [CrossRef] [PubMed]
- Cotar, A.I. Quorum sensing inhibitors as anti-pathogenic drugs in the fight against Pseudomonas aeruginosa infections. Clin. Microbiol. 2013, 2, e111. [Google Scholar]
- Silva, L.N.; Zimmer, K.R.; Macedo, A.J.; Trentin, D.S. Plant natural products targeting bacterial virulence factors. Chem. Rev. 2016, 116, 9162–9236. [Google Scholar] [CrossRef] [PubMed]
| Pharmacology Activity | Drug | Plasma Concentration (µg /mL) |
|---|---|---|
| Analgesic, Antipyretic/Anti-Inflammatory | Acetaminophen | 10.0–20.0 |
| Diclofenac | 0.015 | |
| Antibiotic | Amikacin | 10.0–25.0 |
| Gentamicin | 10.0–5.0 | |
| Ciprofloxacin | 1.6–2.9 | |
| Levofloxacin | 5.7–0.5 | |
| Nitrofurantoin | 30.0–250.0 | |
| Norfloxacin | 2.5–1.5 | |
| Tetracycline | 1.0–2.5 | |
| Anticonvulsant | Carbamazepine | 10.0 |
| Antihistamine | Cetirizine | 0.025–1.0 |
| Loratadine | 0.0025–0.1 | |
| Antihyperglycemic | Metformin | 2.0 |
| Antihypertensive | Captopril | 0.47 |
| Propranolol | 0.05–0.1 | |
| Verapamil | 0.0005–0.002 | |
| Enalapril | 0.055 | |
| Anti-Inflammatory | Dexamethasone | 0.002–0.01 |
| Bile Disorders | Cholic Acid | Up to 1.0 |
| Cholesterol-Lowering | Lovastatin | 0.022–0.036 |
| Hydrochlorothiazide | 0.03 | |
| Hormonal Treatment | Progesterone | Up to 0.5 |
| Antibiotic | Concentration Range (SubMIC *) (ng/mL) | Maximum Induction of Bacterial Growth (%) | Maximum Induction of Biofilm (%) |
|---|---|---|---|
| Gentamicin | 500.0–3.9 | 31.0 | 25.0 |
| Tetracycline | 170.0–1.3 | 31.0 | 46.0 |
| Amikacin | 500.0–3.9 | No effect | 56.0 |
| Norfloxacin | 12.0–0.09 | No effect | 50.0 |
| Nitrofurantoin | 12.0–0.09 | No effect | −15.0 ** |
| Levofloxacin | 12.0–0.09 | No effect | −15.0 ** |
| Ciprofloxacin | 1.02–0.09 | No effect | −35.0 ** |
| Drug | Concentration Range, SubMIC (µg /mL) | Maximum Induction of Bacterial Growth (%) | Maximum Induction of Biofilm (%) |
|---|---|---|---|
| Cetirizine | 1–0.008 | No effect | No effect |
| Loratadine | 0.050–0.004 | No effect | 14.0 |
| Lovastatin | 3.1–0.024 | No effect | No effect |
| Hydrochlorothiazide | 0.050–0.004 | 17.0 | 51.0 |
| Captopril | 0.5–0.0039 | 7.0 | 24.0 |
| Verapamil | 0.5–0.0039 | 21.0 | 10.0 |
| Propranolol | 0.5–0.0039 | No effect | No effect |
| Enalapril | 0.05–0.00040 | 15.0 | No effect |
| Diclofenac | 0.5–0.0039 | 15.0 | No effect |
| Acetaminophen | 5.0–0.039 | 27.0 | 49.0 |
| Carbamazepine | 5.0–0.039 | 22.0 | No effect |
| Metformin | 0.5–0.0039 | No effect | −21.0 * |
| Dexamethasone | 0.5–0.0039 | 11.0 | 14.0 |
| Progesterone | 0.5–0.0039 | 11.0 | 65.0 |
| Cholic Acid | 0.5–0.0039 | 21.0 | No effect |
| Drug | Concentration (µg/mL) | Violacein Abs ** ± SD | Equivalent Concentration to C6-AHL ± SD (µg/mL) |
|---|---|---|---|
| Control | 0.0 | 0.149 ± 0.030 | 0.259 ± 0.111 |
| Acetaminophen * | 0.6 | 0.165 ± 0.020 | 0.362 ± 0.064 |
| Hydrochlorothiazide | 0.025 | 0.154 ± 0.020 | 0.298 ± 0.065 |
| Progesterone | 0.1 | 0.144 ± 0.024 | 0.275 ± 0.097 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cadavid, E.; Robledo, S.M.; Quiñones, W.; Echeverri, F. Induction of Biofilm Formation in Klebsiella pneumoniae ATCC 13884 by Several Drugs: The Possible Role of Quorum Sensing Modulation. Antibiotics 2018, 7, 103. https://doi.org/10.3390/antibiotics7040103
Cadavid E, Robledo SM, Quiñones W, Echeverri F. Induction of Biofilm Formation in Klebsiella pneumoniae ATCC 13884 by Several Drugs: The Possible Role of Quorum Sensing Modulation. Antibiotics. 2018; 7(4):103. https://doi.org/10.3390/antibiotics7040103
Chicago/Turabian StyleCadavid, Elizabeth, Sara M. Robledo, Wiston Quiñones, and Fernando Echeverri. 2018. "Induction of Biofilm Formation in Klebsiella pneumoniae ATCC 13884 by Several Drugs: The Possible Role of Quorum Sensing Modulation" Antibiotics 7, no. 4: 103. https://doi.org/10.3390/antibiotics7040103
APA StyleCadavid, E., Robledo, S. M., Quiñones, W., & Echeverri, F. (2018). Induction of Biofilm Formation in Klebsiella pneumoniae ATCC 13884 by Several Drugs: The Possible Role of Quorum Sensing Modulation. Antibiotics, 7(4), 103. https://doi.org/10.3390/antibiotics7040103





