Cognitive Deficits Following a Post-Myocardial Infarct in the Rat Are Blocked by the Serotonin-Norepinephrine Reuptake Inhibitor Desvenlafaxine
Abstract
:1. Introduction
2. Results
2.1. Ischemic Damage
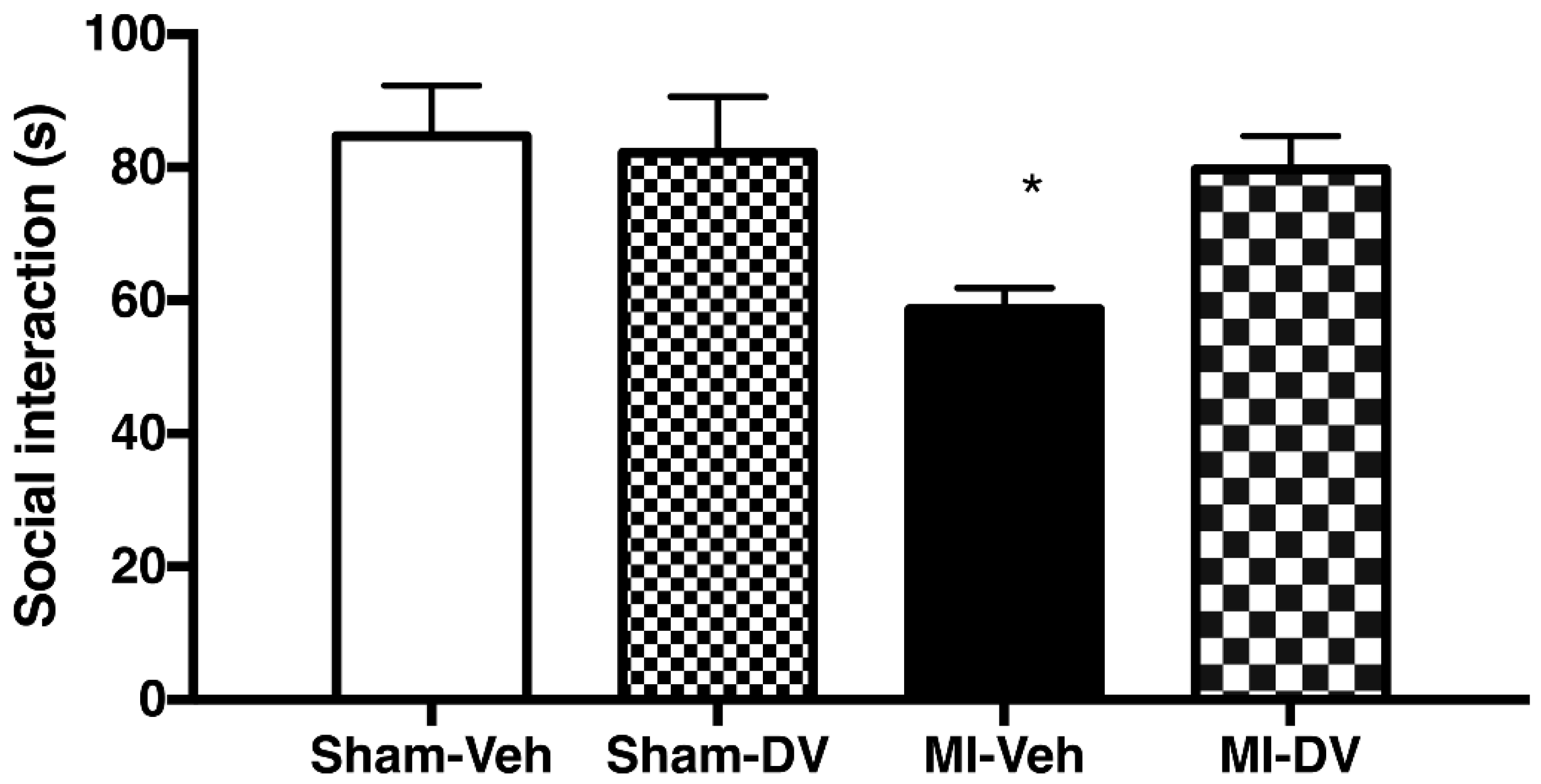
2.2. Social Interaction, 2 Weeks Post-MI
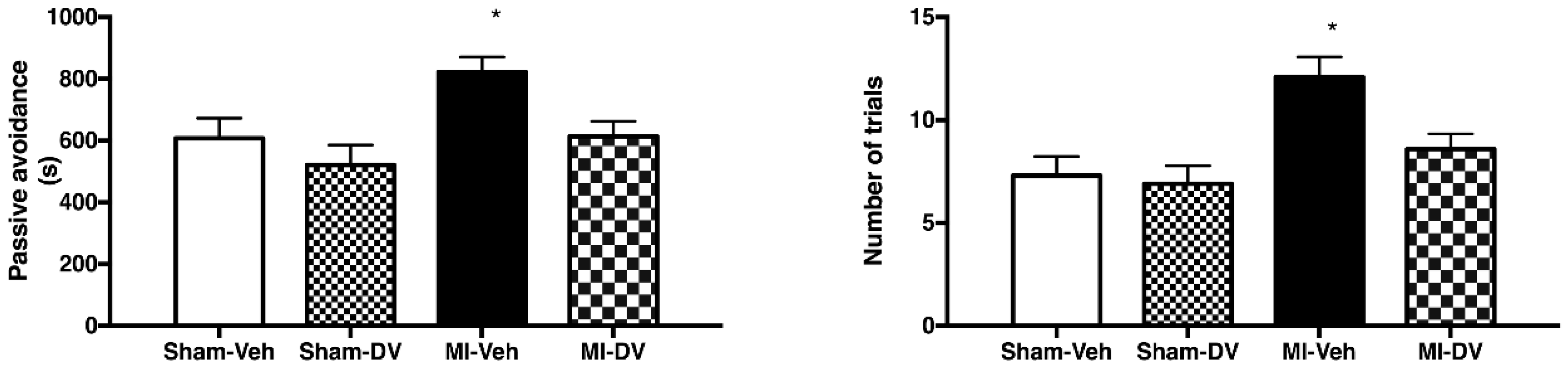
2.3. Passive-Avoidance Step-Down Test, 2 Weeks Post-MI
2.4. Forced Swimming Test, 4 Months Post-MI
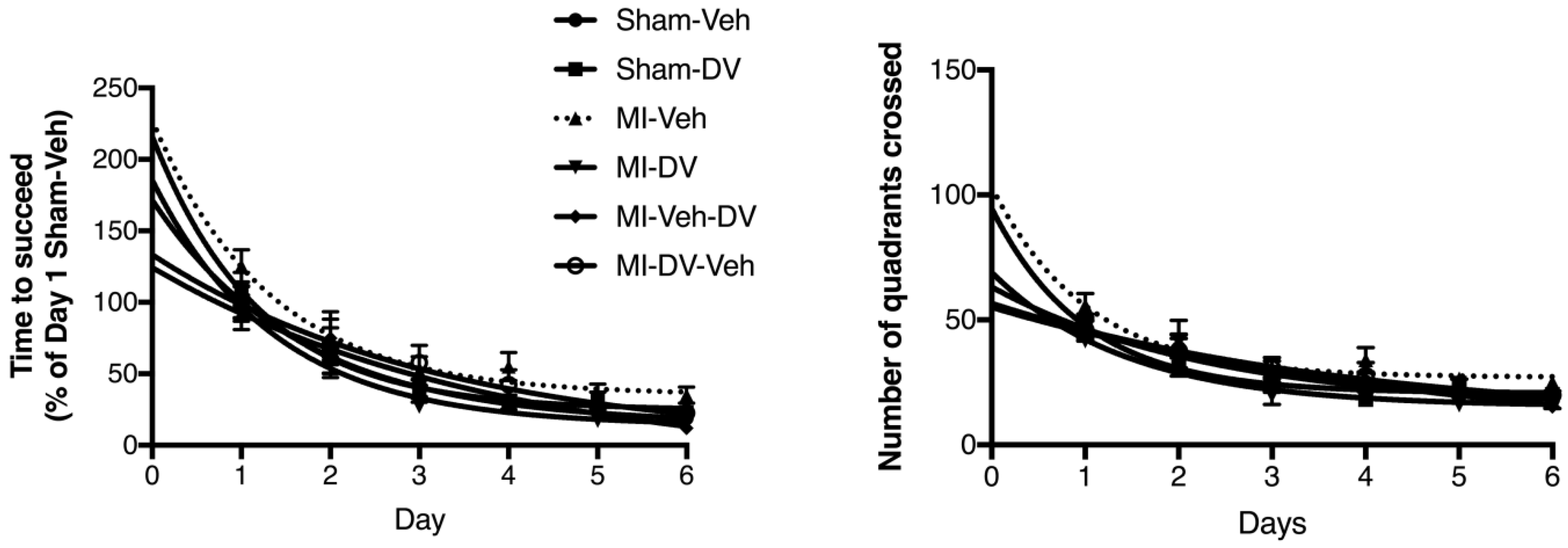
2.5. Morris Water Maze (MWM) Test, 4 Months Post-MI
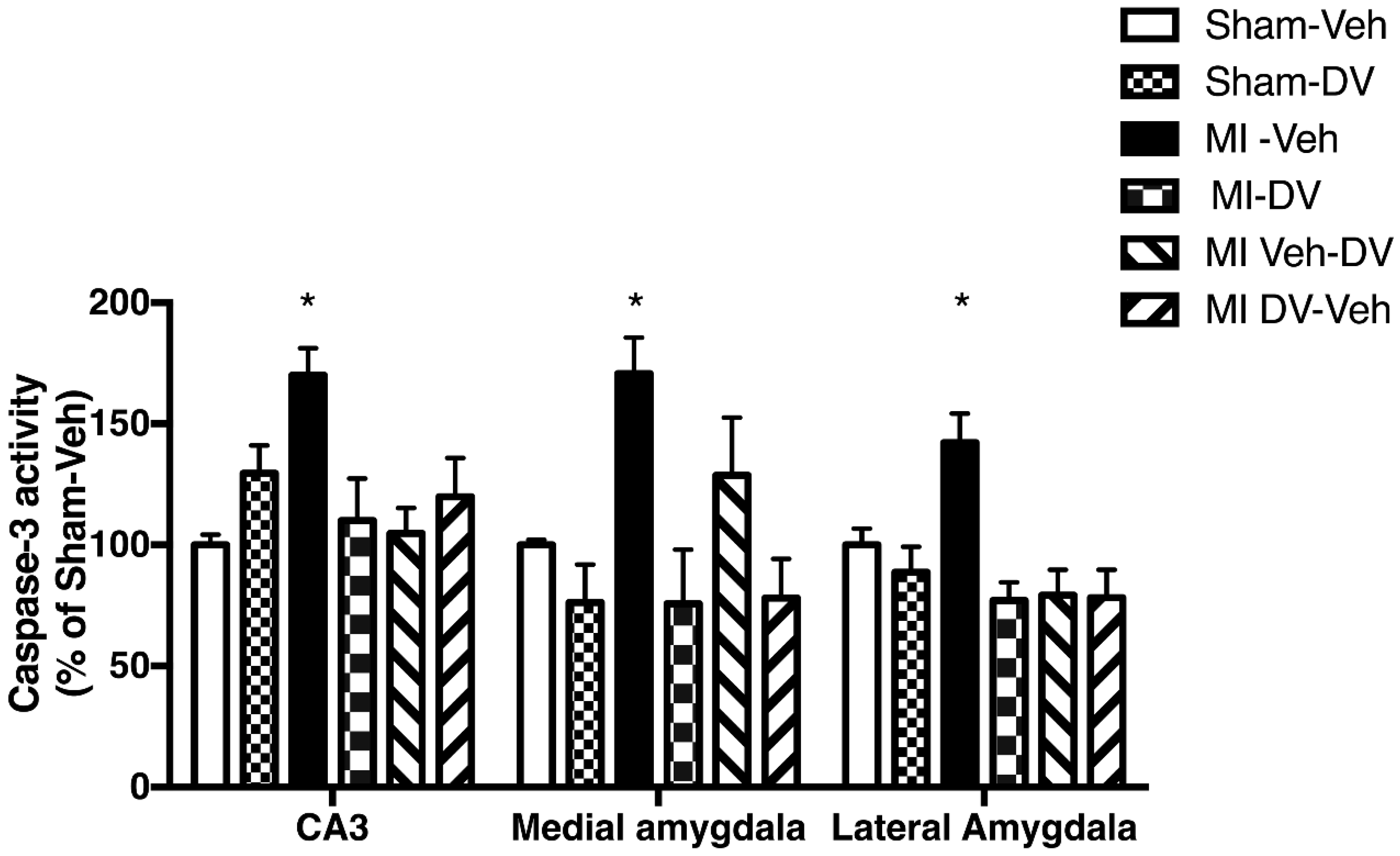
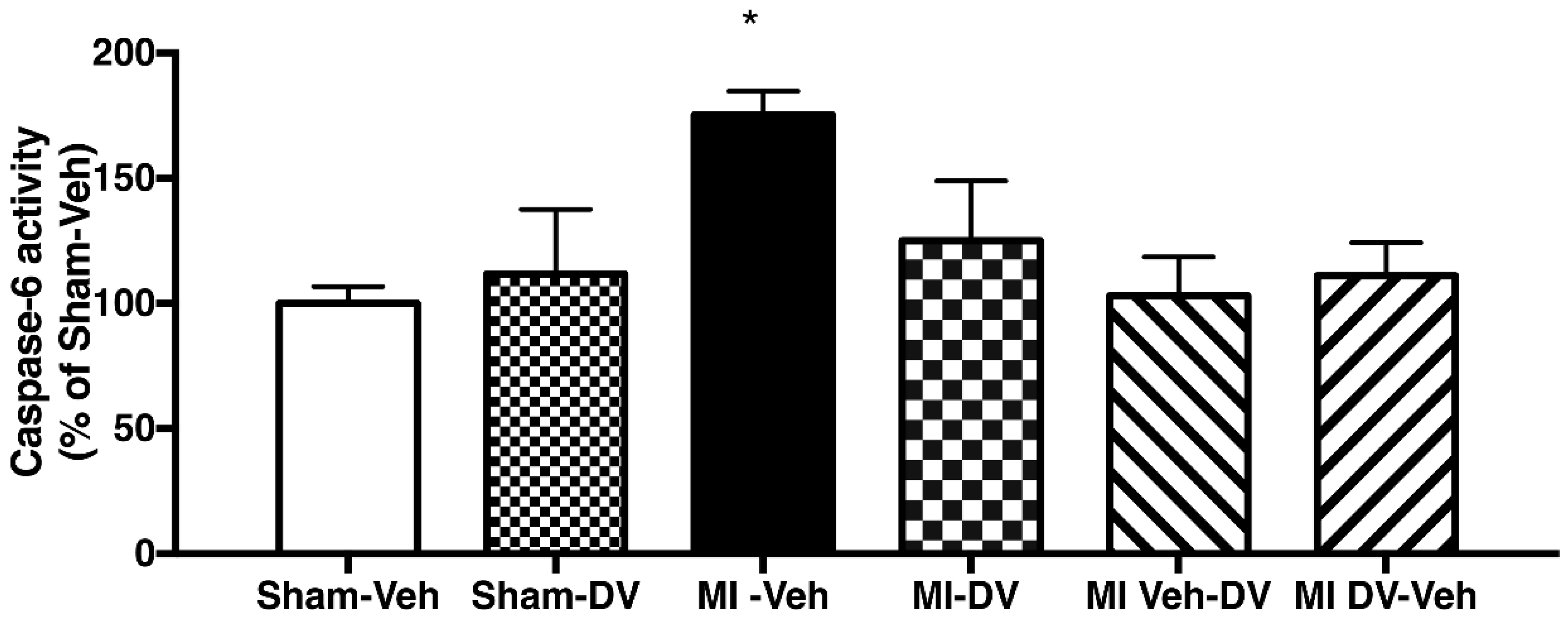
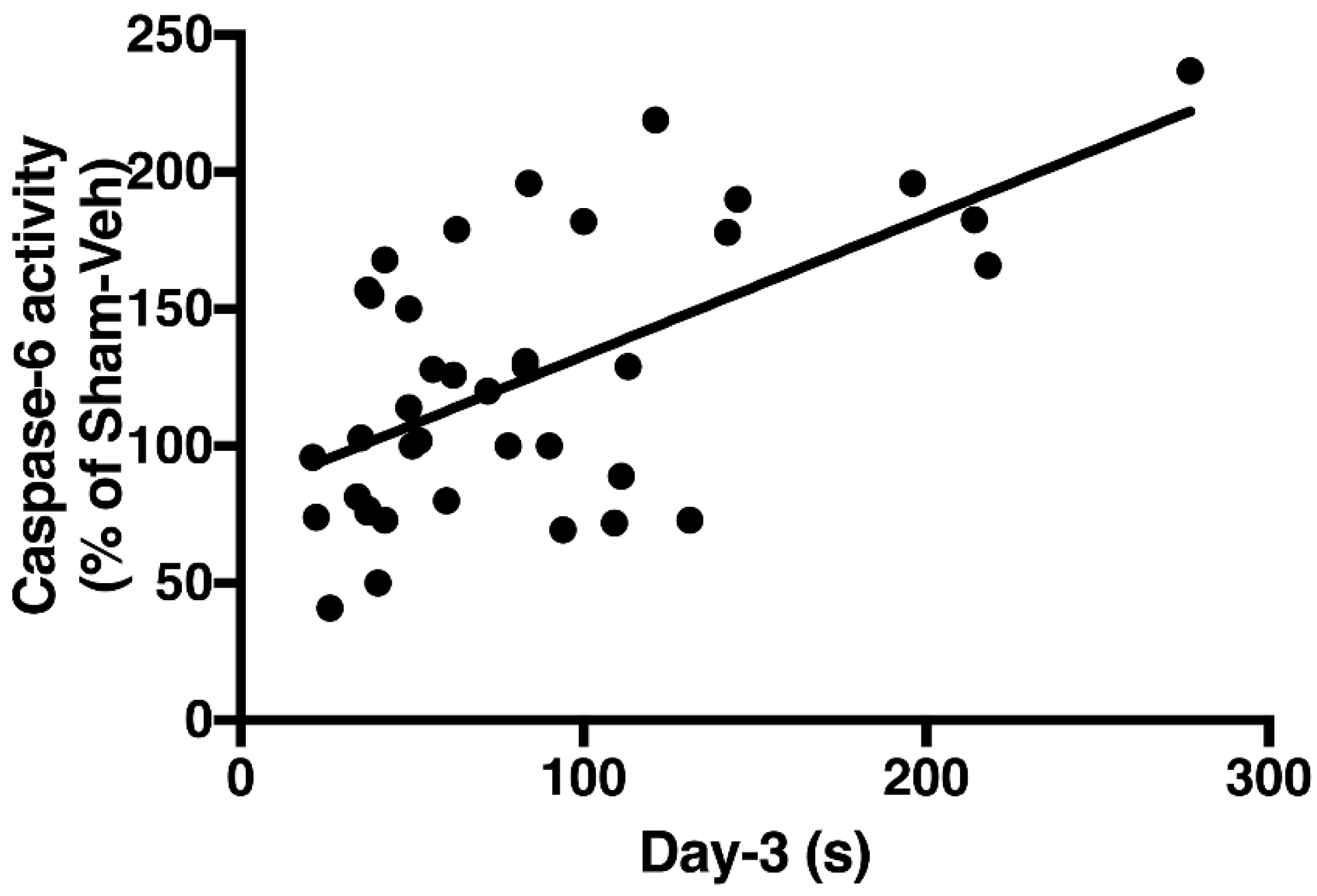
2.6. Caspase-3 and -6 Activities
3. Discussion
4. Materials and Methods
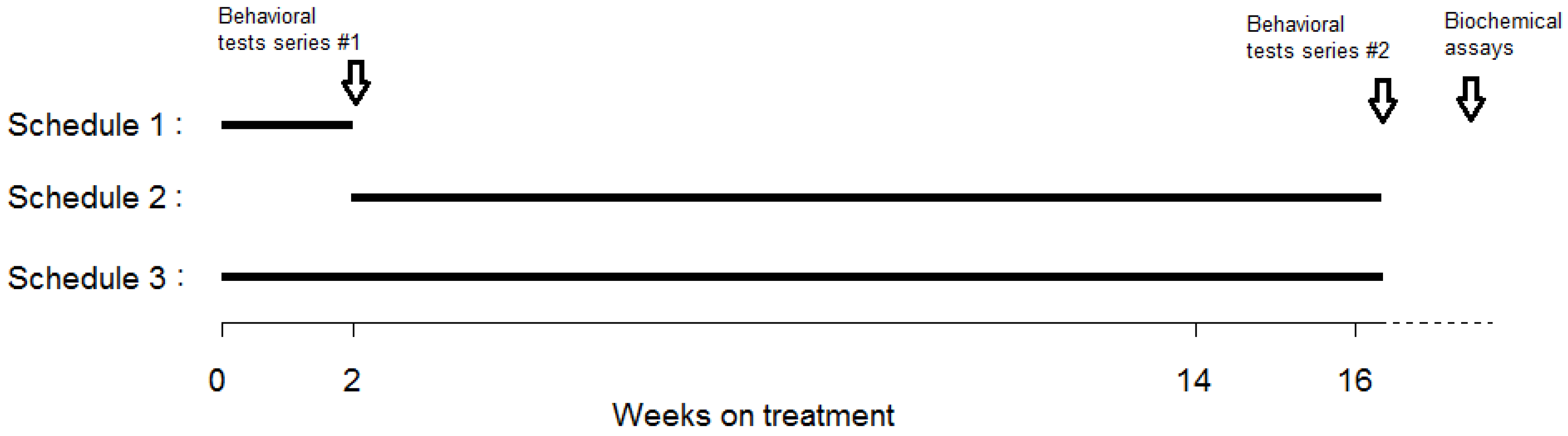
4.1. Experimental Groups
4.2. Surgical Procedure
4.3. Scar Sections (SS), Area at Risk (AR) Measurement and Brain Dissection
4.4. Behavioral Tests
4.4.1. Social Interaction Test
4.4.2. Passive-Avoidance Step-Down Test
4.4.3. Forced Swimming Test
4.4.4. MWM Test
4.5. Caspase-3 and Caspase-6 Activity
4.6. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Deckers, K.; Schievink, S.H.J.; Rodriquez, M.M.F.; van Oostenbrugge, R.J.; van Boxtel, M.P.J.; Verhey, F.R.J.; Kohler, S. Coronary heart disease and risk for cognitive impairment or dementia: Systematic review and meta-analysis. PLoS ONE 2017, 12, e0184244. [Google Scholar] [CrossRef] [PubMed]
- Wann, B.; Boucher, M.; Kaloustian, S.; Nim, S.; Godbout, R.; Rousseau, G. Apoptosis detected in the amygdala following myocardial infarction in the rat. Biol. Psychiatry 2006, 59, 430–433. [Google Scholar] [CrossRef] [PubMed]
- Wann, B.P.; Bah, T.M.; Boucher, M.; Courtemanche, J.; Le Marec, N.; Rousseau, G.; Godbout, R. Vulnerability for apoptosis in the limbic system after myocardial infarction in rats: A possible model for human postinfarct major depression. J. Psychiatry Neurosci. 2007, 32, 11–16. [Google Scholar] [PubMed]
- Wann, B.P.; Bah, T.M.; Kaloustian, S.; Boucher, M.; Dufort, A.M.; Le Marec, N.; Godbout, R.; Rousseau, G. Behavioural signs of depression and apoptosis in the limbic system following myocardial infarction: Effects of sertraline. J. Psychopharmacol. 2009, 23, 451–459. [Google Scholar] [CrossRef] [PubMed]
- Bah, T.M.; Benderdour, M.; Kaloustian, S.; Karam, R.; Rousseau, G.; Godbout, R. Escitalopram reduces circulating pro-inflammatory cytokines and improves depressive behavior without affecting sleep in a rat model of post-cardiac infarct depression. Behav. Brain Res. 2011, 225, 243–251. [Google Scholar] [CrossRef] [PubMed]
- Jacobson, M.D.; Weil, M.; Raff, M.C. Programmed cell death in animal development. Cell 1997, 88, 347–354. [Google Scholar] [CrossRef]
- Shabanzadeh, A.P.; D’Onofrio, P.M.; Monnier, P.P.; Koeberle, P.D. Targeting caspase-6 and caspase-8 to promote neuronal survival following ischemic stroke. Cell Death Dis. 2015, 6, e1967. [Google Scholar] [CrossRef] [PubMed]
- Beaudouin, J.; Liesche, C.; Aschenbrenner, S.; Horner, M.; Eils, R. Caspase-8 cleaves its substrates from the plasma membrane upon CD95-induced apoptosis. Cell Death Differ. 2013, 20, 599–610. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leblanc, A.C.; Ramcharitar, J.; Afonso, V.; Hamel, E.; Bennett, D.A.; Pakavathkumar, P.; Albrecht, S. Caspase-6 activity in the CA1 region of the hippocampus induces age-dependent memory impairment. Cell Death Differ. 2014, 21, 696. [Google Scholar] [CrossRef] [PubMed]
- Perry, R.; Cassagnol, M. Desvenlafaxine: A new serotonin-norepinephrine reuptake inhibitor for the treatment of adults with major depressive disorder. Clin. Ther. 2009, 31, 1374–1404. [Google Scholar] [CrossRef] [PubMed]
- Archer, D.F.; Pinkerton, J.V.; Guico-Pabia, C.J.; Hwang, E.; Cheng, R.F. Cardiovascular, cerebrovascular, and hepatic safety of desvenlafaxine for 1 year in women with vasomotor symptoms associated with menopause. Menopause 2013, 20, 47–56. [Google Scholar] [CrossRef] [PubMed]
- Malick, M.; Gilbert, K.; Barry, M.; Godbout, R.; Rousseau, G. Desvenlafaxine reduces apoptosis in amygdala after myocardial infarction. Brain Res. Bull. 2014, 109, 158–163. [Google Scholar] [CrossRef] [PubMed]
- Rousseau, G.; Bah, T.M.; Godbout, R. Post-myocardial infarction depression. In Novel Strategies in Ischemic Heart Disease; Lakshmanadoss, U., Ed.; InTech: Rijeka, Croatia, 2012; pp. 333–362. [Google Scholar]
- Wang, Y.; Liu, X.; Zhang, D.; Chen, J.; Liu, S.; Berk, M. The effects of apoptosis vulnerability markers on the myocardium in depression after myocardial infarction. BMC Med. 2013, 11, 32. [Google Scholar] [CrossRef] [PubMed]
- Parent, M.; Bah, T.M.; Rousseau, G.; Godbout, R. Myocardial infarct in middle age rats is followed by mild cognitive impairment compatible with neurodegenerative diseases of aging. In Proceedings of the Society for Neuroscience 43rd Annual Meeting, San Diego, CA, USA, 9–13 November 2013. [Google Scholar]
- Kaloustian, S.; Wann, B.P.; Bah, T.M.; Girard, S.A.; Apostolakis, A.; Ishak, S.; Mathieu, S.; Ryulin, P.; Godbout, R.; Rousseau, G. Apoptosis time course in the limbic system after myocardial infarction in the rat. Brain Res. 2008, 1216, 87–91. [Google Scholar] [CrossRef] [PubMed]
- Lipton, P. Ischemic cell death in brain neurons. Physiol. Rev. 1999, 79, 1431–1568. [Google Scholar] [CrossRef] [PubMed]
- Deckwerth, T.L.; Elliott, J.L.; Knudson, C.M.; Johnson, E.M., Jr.; Snider, W.D.; Korsmeyer, S.J. BAX is required for neuronal death after trophic factor deprivation and during development. Neuron 1996, 17, 401–411. [Google Scholar] [CrossRef]
- Guo, H.; Albrecht, S.; Bourdeau, M.; Petzke, T.; Bergeron, C.; LeBlanc, A.C. Active caspase-6 and caspase-6-cleaved tau in neuropil threads, neuritic plaques, and neurofibrillary tangles of Alzheimer’s disease. Am. J. Pathol. 2004, 165, 523–531. [Google Scholar] [CrossRef]
- Graham, R.K.; Ehrnhoefer, D.E.; Hayden, M.R. Caspase-6 and neurodegeneration. Trends Neurosci. 2011, 34, 646–656. [Google Scholar] [CrossRef] [PubMed]
- Monnier, P.P.; D’Onofrio, P.M.; Magharious, M.; Hollander, A.C.; Tassew, N.; Szydlowska, K.; Tymianski, M.; Koeberle, P.D. Involvement of caspase-6 and caspase-8 in neuronal apoptosis and the regenerative failure of injured retinal ganglion cells. J. Neurosci. 2011, 31, 10494–10505. [Google Scholar] [CrossRef] [PubMed]
- Wurstle, M.L.; Laussmann, M.A.; Rehm, M. The caspase-8 dimerization/dissociation balance is a highly potent regulator of caspase-8, -3, -6 signaling. J. Biol. Chem. 2010, 285, 33209–33218. [Google Scholar] [CrossRef] [PubMed]
- Alcocer-Gomez, E.; Casas-Barquero, N.; Williams, M.R.; Romero-Guillena, S.L.; Canadas-Lozano, D.; Bullon, P.; Sanchez-Alcazar, J.A.; Navarro-Pando, J.M.; Cordero, M.D. Antidepressants induce autophagy dependent-NLRP3-inflammasome inhibition in Major depressive disorder. Pharmacol. Res. 2017, 121, 114–121. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gilbert, K.; Arseneault-Breard, J.; Flores Monaco, F.; Beaudoin, A.; Bah, T.M.; Tompkins, T.A.; Godbout, R.; Rousseau, G. Attenuation of post-myocardial infarction depression in rats by n-3 fatty acids or probiotics starting after the onset of reperfusion. Br. J. Nutr. 2013, 109, 50–56. [Google Scholar] [CrossRef] [PubMed]
- Arseneault-Breard, J.; Rondeau, I.; Gilbert, K.; Girard, S.-A.; Tompkins, T.A.; Godbout, R.; Rousseau, G. Combination of Lactobacillus helveticus R0052 and Bifidobacterium longum R0175 reduces post-myocardial infarction depression symptoms and restores intestinal permeability in a rat model. Br. J. Nutr. 2012, 107, 1793–1799. [Google Scholar] [CrossRef] [PubMed]
- Gilbert, K.; Bernier, J.; Godbout, R.; Rousseau, G. Resolvin d1, a metabolite of omega-3 polyunsaturated Fatty Acid, decreases post-myocardial infarct depression. Mar. Drugs 2014, 12, 5396–5407. [Google Scholar] [CrossRef] [PubMed]
- Drzyzga, L.R.; Marcinowska, A.; Obuchowicz, E. Antiapoptotic and neurotrophic effects of antidepressants: A review of clinical and experimental studies. Brain Res. Bull. 2009, 79, 248–257. [Google Scholar] [CrossRef] [PubMed]
- Lee, F.S.; Chao, M.V. Activation of Trk neurotrophin receptors in the absence of neurotrophins. Proc. Natl. Acad. Sci. USA 2001, 98, 3555–3560. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bah, T.M.; Kaloustian, S.; Rousseau, G.; Godbout, R. Pretreatment with pentoxifylline has antidepressant-like effects in a rat model of acute myocardial infarction. Behav. Pharmacol. 2011, 22, 779–784. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Liu, J.; Suo, F.; Hu, H.S.; Xue, M.; Cheng, W.J.; Xuan, Y.L.; Yan, S.H. Metoprolol-mediated amelioration of sympathetic nerve sprouting after myocardial infarction. Cardiology 2013, 126, 50–58. [Google Scholar] [CrossRef] [PubMed]
- Gao, X.M.; Tsai, A.; Al-Sharea, A.; Su, Y.; Moore, S.; Han, L.P.; Kiriazis, H.; Dart, A.M.; Murphy, A.J.; Du, X.J. Inhibition of the Renin-Angiotensin System Post Myocardial Infarction Prevents Inflammation-Associated Acute Cardiac Rupture. Cardiovasc. Drugs Ther. 2017, 31, 145–156. [Google Scholar] [CrossRef] [PubMed]
- Diaper, A.; Rich, A.S.; Wilson, S.J.; Craig, K.; Dourish, C.T.; Dawson, G.R.; Nutt, D.J.; Bailey, J.E. Changes in cardiovascular function after venlafaxine but not pregabalin in healthy volunteers: A double-blind, placebo-controlled study of orthostatic challenge, blood pressure and heart rate. Hum. Psychopharmacol. 2013, 28, 562–575. [Google Scholar] [CrossRef] [PubMed]
- Unterecker, S.; Pfuhlmann, B.; Kopf, J.; Kittel-Schneider, S.; Reif, A.; Deckert, J. Increase of Heart Rate and QTc by Amitriptyline, But Not by Venlafaxine, Is Correlated to Serum Concentration. J. Clin. Psychopharmacol. 2015, 35, 460–463. [Google Scholar] [CrossRef] [PubMed]
- Ishikawa, K.; Chemaly, E.R.; Tilemann, L.; Fish, K.; Ladage, D.; Aguero, J.; Vahl, T.; Santos-Gallego, C.; Kawase, Y.; Hajjar, R.J. Assessing left ventricular systolic dysfunction after myocardial infarction: Are ejection fraction and dP/dt(max) complementary or redundant? Am. J. Physiol. Heart Circ. Physiol. 2012, 302, H1423–H1428. [Google Scholar] [CrossRef] [PubMed]

| Group | Scar Section/AR | AR/LV |
|---|---|---|
| MI-Veh | 31.3 ± 1.6 | 66.4 ± 1.5 |
| MI-DV | 29.0 ± 1.9 | 63.8 ± 1.5 |
| MI-Veh-DV | 31.1± 1.6 | 65.5 ± 2.3 |
| MI-DV-Veh | 26.3 ± 1.1 | 64.7 ± 2.0 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Malick, M.; Gilbert, K.; Brouillette, J.; Godbout, R.; Rousseau, G. Cognitive Deficits Following a Post-Myocardial Infarct in the Rat Are Blocked by the Serotonin-Norepinephrine Reuptake Inhibitor Desvenlafaxine. Int. J. Mol. Sci. 2018, 19, 3748. https://doi.org/10.3390/ijms19123748
Malick M, Gilbert K, Brouillette J, Godbout R, Rousseau G. Cognitive Deficits Following a Post-Myocardial Infarct in the Rat Are Blocked by the Serotonin-Norepinephrine Reuptake Inhibitor Desvenlafaxine. International Journal of Molecular Sciences. 2018; 19(12):3748. https://doi.org/10.3390/ijms19123748
Chicago/Turabian StyleMalick, Mandy, Kim Gilbert, Jonathan Brouillette, Roger Godbout, and Guy Rousseau. 2018. "Cognitive Deficits Following a Post-Myocardial Infarct in the Rat Are Blocked by the Serotonin-Norepinephrine Reuptake Inhibitor Desvenlafaxine" International Journal of Molecular Sciences 19, no. 12: 3748. https://doi.org/10.3390/ijms19123748





