Comparative Evaluation of Cold Dissection (Suture vs. Ligation) and Hot Dissection Tonsillectomy in Children: Postoperative Pain, Bleeding, and Operative Time
Abstract
1. Introduction
2. Materials and Methods
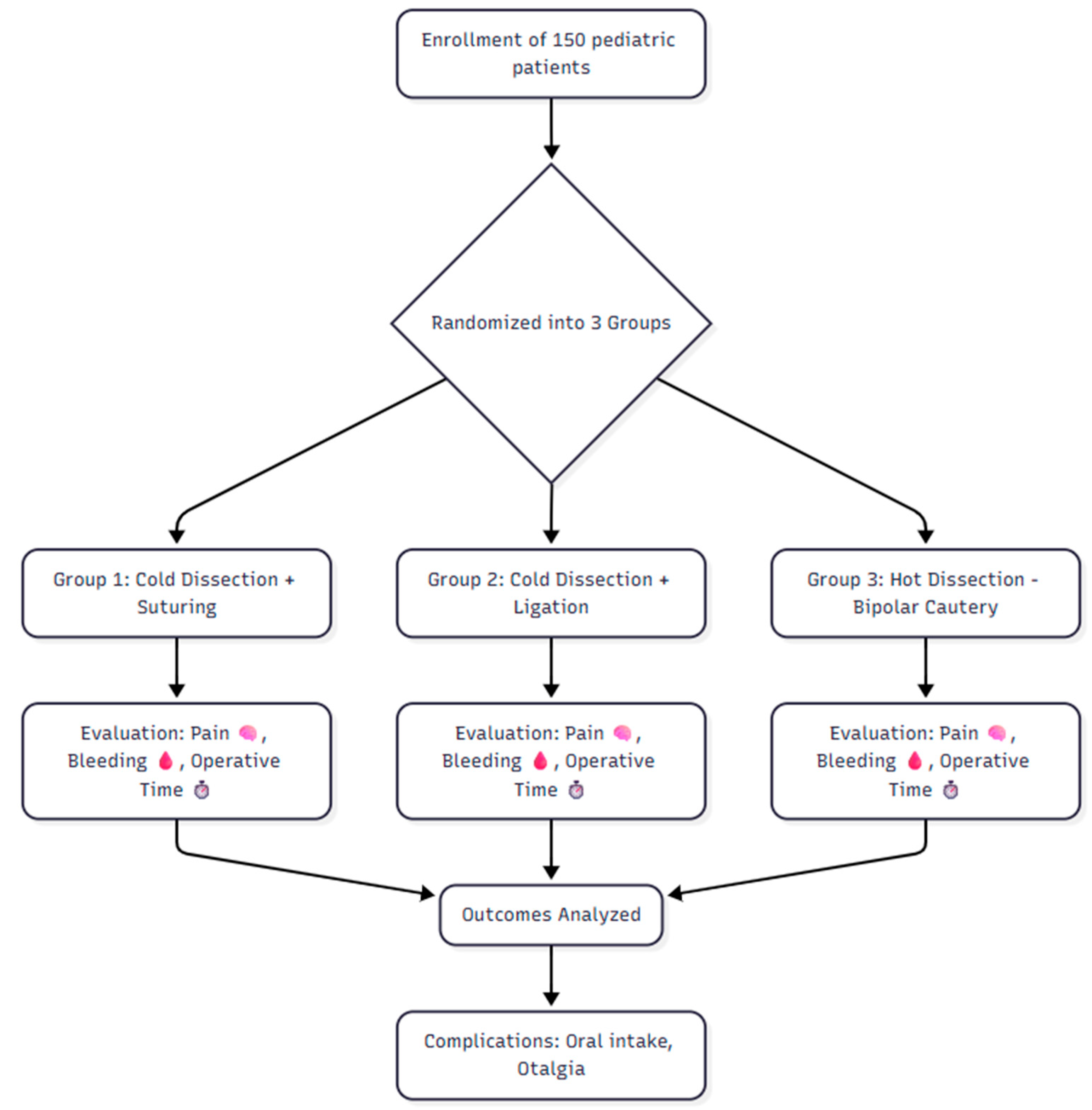
2.1. Study Design and Study Population
2.2. Randomization and Groups
- ➢
- Group 1 (Cold Dissection + Suturing): Standard cold-knife dissection was performed, followed by hemostasis using absorbable suture material (Vicryl 3-0, Ethicon) to approximate the anterior and posterior tonsillar pillars. No local anesthetic or topical hemostatic agents were applied.
- ➢
- Group 2 (Cold Dissection + Ligation): Standard cold dissection was performed, and bleeding vessels were ligated with the same absorbable suture material (Vicryl 3-0, Ethicon).
- ➢
- Group 3 (Hot Dissection—Bipolar Cautery): Bipolar cautery dissection was used for tissue separation and hemostasis, with energy settings adjusted to minimize thermal injury.
2.3. Outcome Measures
- Postoperative Pain:
- ➢
- Wong–Baker FACES Pain Rating Scale was used at postoperative hours 1, 6, and 24, and on days 3 and 7.
- ➢
- Parents’ Postoperative Pain Measure (PPPM) was administered at hours 1, 6, and 24 before meals, fluid intake, or analgesic use.
- Postoperative Bleeding:
- ➢
- Primary bleeding: Any hemorrhage within 24 h post-surgery.
- ➢
- Secondary bleeding: Any hemorrhage occurring from 24 h to 14 days postoperatively. All bleeding events were initially assessed by the operating surgeon during hospitalization and subsequently confirmed through outpatient follow-up visits or standardized parent reports, with final adjudication by an independent ENT consultant.
- Secondary Outcomes
- ➢
- Operative Time: Measured in minutes from the first incision to the completion of hemostasis.
- ➢
- Complications: Any postoperative events including readmission for oral intake difficulty, infection, or other adverse events (Figure 1).
2.4. Statistical Analysis
3. Results
4. Discussion
Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kou, Y.F.; Korpon, J.R.; Dabbous, H.; Johnson, R.F.; Mitchell, R.B.; Wani, A.; Chorney, S.R. Postoperative Respiratory Complications After Adenotonsillectomy in Children with High-Risk Obstructive Sleep Apnea. Otolaryngol. Head Neck Surg. 2024, 171, 1911–1917. [Google Scholar] [CrossRef]
- Wikner, E.; Nguyen, C.; Vazifedan, T.; Almirante, J.; Chilampath, B.; Mason, L.; Derkay, C. Risk Factors Associated with Pediatric Post-Tonsillectomy Complications: A Focus on Racial, Ethnic and Socioeconomic Factors. Ann. Otol. Rhinol. Laryngol. 2025, 134, 533–539. [Google Scholar] [CrossRef]
- Hathi, K.; Francis, G.; Douglas, J.; Nemeth, E.; Hong, P. Ninety-Day Emergency Department Rebound Following Adult Tonsillectomy: A Retrospective Cohort Study. J. Otolaryngol. Head Neck Surg. 2025, 54, 19160216251333350. [Google Scholar] [CrossRef] [PubMed]
- Attya, H.M.A. Short-Term Outcomes of Tonsillectomy in Large Paediatric Case Series. Indian J. Otolaryngol. Head Neck Surg. 2024, 76, 5148–5153. [Google Scholar] [CrossRef] [PubMed]
- Huang, G.J.; Yang, X.S.; Lu, B.Q. Patient Characteristics and Postoperative Mortality in Children Undergoing Tonsillectomy. JAMA 2022, 328, 1770–1771. [Google Scholar] [CrossRef]
- Akella, D.; Cottone, C.; Raghavan, M.; Varavenkataraman, G.; Marcus, C.A.; Erwin, D.Z.; Carr, M.M. Are More Adults Bleeding After Tonsillectomy Than in the Past? Laryngoscope 2025, 135, 1958–1963. [Google Scholar] [CrossRef]
- Alkheder, A.; Alia, N.; Abbas, M.; Shubat, A.; Aljammal, G. Subcutaneous Emphysema as a Complication of Tonsillectomy: Comprehensive Literature Review. Ear Nose Throat J. 2024, 11, 1455613241305602. [Google Scholar] [CrossRef]
- Alenezi, M.M.; Al-Harbi, F.A.; Almoshigeh, A.N.M.; Alruqaie, S.S.; Alshahrani, N.M.; Alamro, A.M.; Aljulajil, A.A.; Alsaqri, R.A.; Alharbi, L.A. Comparison of Post-Tonsillectomy Hemorrhage Rate After Different Tonsillectomy Techniques: Systematic Review and Meta Analysis. Clin. Pract. 2025, 15, 85. [Google Scholar] [CrossRef]
- Guest, J.F.; Rana, K.; Hopkins, C. Cost-effectiveness of Coblation compared with cold steel tonsillectomies in the UK. J. Laryngol. Otol. 2018, 132, 1119–1127. [Google Scholar] [CrossRef] [PubMed]
- Lundstrom, F.; Stalfors, J.; Ostvoll, E.; Sunnergren, O. Practice, complications and outcome in Swedish tonsil surgery 2009–2018. An observational longitudinal national cohort study. Acta Otolaryngol. 2020, 140, 589–596. [Google Scholar] [CrossRef]
- Kokong, D.D.; Adoga, A.A.; Ma’an, N.D.; Turaki, I.; Mgbachi, C.J.; Ajogwu, G.A.; Damulak, O.D. Tonsillectomy: Post-Operative Hemorrhage Reduction Strategy in Jos, North Central Nigeria. West Afr. J. Med. 2022, 39, 964–972. [Google Scholar] [PubMed]
- Gerhardsson, H.; Stalfors, J.; Sunnergren, O. Postoperative morbidity and mortality after adenoidectomy: A national population-based study of 51 746 surgeries. Int. J. Pediatr. Otorhinolaryngol. 2022, 163, 111335. [Google Scholar] [CrossRef]
- Patel, S.D.; Daher, G.S.; Engle, L.; Zhu, J.; Slonimsky, G. Adult tonsillectomy: An evaluation of indications and complications. Am. J. Otolaryngol. 2022, 43, 103403. [Google Scholar] [CrossRef] [PubMed]
- Chaudhary, K.; Singh, V.; Yadav, R.; Chaudhary, A.K.; Kumar, R.; Gupta, D.K.; Verma, J.K. Comparative Study of Complications Associated with Coblation Versus Conventional Tonsillectomy. Indian J. Otolaryngol. Head Neck Surg. 2023, 75, 2870–2877. [Google Scholar] [CrossRef]
- Edmonson, M.B.; Francis, D.O.; Coller, R.J. Patient Characteristics and Postoperative Mortality in Children Undergoing Tonsillectomy-Reply. JAMA 2022, 328, 1771. [Google Scholar] [CrossRef] [PubMed]
- Xu, B.; Bi, J.; Fu, Y.; Xu, Y.; Yu, L.; Han, Y.; Lin, X.; Hong, M. Risk factors and predictive models for secondary hemorrhage in pediatric coblation tonsillectomy. Int. J. Pediatr. Otorhinolaryngol. 2025, 192, 112327. [Google Scholar] [CrossRef]
- Unsal, N.; Baldir, E.H.; Bulut Cobden, S.; Kantekin, Y.; Kaya, A.; Yasar, M.; Ozcan, I.; Bayram, A. Retrospective Analysis of Hemorrhage After Pediatric Tonsillectomy. Turk. Arch. Otorhinolaryngol. 2025, 63, 75–79. [Google Scholar] [CrossRef]
- Li, N.; Wang, R.; Hu, P.; Lu, W.; Zhao, X.; Wang, L.; Song, M.; Gao, Y.; An, C.; Bashir, S.; et al. Effect of night shift work on metabolic syndrome in adults who suffered from earthquake stress in early life. Front. Public Health 2023, 11, 1139113. [Google Scholar] [CrossRef]
- Meeker, M.O.; McColl, L.F.; Malhotra, P.S. Spontaneous tonsillar hemorrhage in a patient with PTEN mutation: A case report and systematic literature review. Int. J. Pediatr. Otorhinolaryngol. 2025, 192, 112315. [Google Scholar] [CrossRef]
- Tan, G.X.; Tunkel, D.E. Control of Pain After Tonsillectomy in Children: A Review. JAMA Otolaryngol. Head Neck Surg. 2017, 143, 937–942. [Google Scholar] [CrossRef]
- Mathuna, E.; Corbett, M.; Byrne, L.O.; Aly, M.; Davey, M.G.; Khoo, S.G. Tie or do not tie: Comparing knot tying hemostasis in tonsillectomy with other methods of hemostasis. A systematic review and meta-analysis. Eur. Arch. Otorhinolaryngol. 2025, 282, 2627–2634. [Google Scholar] [CrossRef]
- Kandemir, S.; Pamuk, A.E.; Ozel, G.; Sencan, Z. Comparison of Three Tonsillectomy Techniques: Cold Dissection, Monopolar Electrocautery, and Coblation. Int. Arch. Otorhinolaryngol. 2023, 27, e694–e698. [Google Scholar] [CrossRef]
- Bhankhodia, B.P.; Aiyer, R.G.; Raval, J.B. Comparative Study of CO(2) LASER Assisted and Electrocautery Assisted Tonsillectomy with Conventional Tonsillectomy. Indian J. Otolaryngol. Head Neck Surg. 2022, 74, 5324–5328. [Google Scholar] [CrossRef] [PubMed]
- Rubinstein, B.J.; Derkay, C.S. Rethinking surgical technique and priorities for pediatric tonsillectomy. Am. J. Otolaryngol. 2017, 38, 233–236. [Google Scholar] [CrossRef]
- Iqbal, M.; Kumar, D.; Ansari, N.A. Tonsillectomy; Comparing the Effectiveness of Dissection and Diathermy Tonsillectomy. Prof. Med. J. 2017, 24, 1237–1240. [Google Scholar] [CrossRef]
- Gawel, E.M.; Keenehan, K.R.; Akella, D.S.; Carr, M.M. Adverse events related to suction electrocautery devices in adenotonsillectomy: Analysis of the MAUDE database. Am. J. Otolaryngol. 2024, 45, 104404. [Google Scholar] [CrossRef] [PubMed]
- Anwaegbu, O.S.; Clark, D.E.S.; Iyamah, S.O.; Ezenwukwa, C.; Etufugh, U.L.; McKinnon, B.J. Trends in postoperative complications following pediatric tonsillectomy & adenoidectomy: A 10-year analysis. Am. J. Otolaryngol. 2025, 46, 104712. [Google Scholar] [CrossRef] [PubMed]
- Lao, J.; Jian, F.; Ge, R.; Wu, S. Tonsillectomy Versus Tonsillotomy in Pediatric Sleep-Disordered Breathing: A Systematic Review and Multi-subgroup Meta-analysis. Laryngoscope 2025, 135, 529–539. [Google Scholar] [CrossRef]
| Variables | Group 1 | Group 2 | Group 3 | p Value |
|---|---|---|---|---|
| N (%) | ||||
| Gender | 0.771 ᵃ | |||
| Male | 31 (62.0) | 29 (58.0) | 27 (54.0) | |
| Female | 19 (38.0) | 21 (42.0) | 23 (46.0) | |
| Primary bleeding | — | |||
| No | 50 (100) | 50 (100) | 50 (100) | |
| Secondary bleeding | 0.167 ᵃ | |||
| No | 49 (98.0) | 50 (100) | 47 (94.0) | |
| Yes | 1 (2.0) | 0 (0) | 3 (6.0) | |
| Postoperative oral intake difficulty | 0.167 ᵃ | |||
| No | 49 (98.0) | 50 (100) | 47 (94.0) | |
| Yes | 1 (2.0) | 0 (0) | 3 (6.0) | |
| Postoperative otalgia | 0.364 ᵃ | |||
| No | 49 (98.0) | 50 (100) | 48 (96.0) | |
| Yes | 1 (2.0) | 0 (0) | 2 (4.0) | |
| Group | Surgical Technique | Mean ± SD (min) | Median (min) | p Value ᵃ |
|---|---|---|---|---|
| 1 | Cold dissection + suturing | 21.89 ± 1.64 | 22.10 | 0.001 * |
| 2 | Cold dissection + ligation | 18.60 ± 0.94 | 18.30 | |
| 3 | Hot dissection (bipolar cautery) | 17.53 ± 1.26 | 17.20 |
| Time Point | Group 1 | Group 2 | Group 3 | p Value ᵃ,* |
|---|---|---|---|---|
| Wong–Baker FACES Pain Rating Scale Median (IQR) | ||||
| Hour 1 | 4.0 (3.0–5.0) | 3.0 (3.0–4.0) | 4.0 (4.0–5.0) | 0.001 *, η2 = 0.12 |
| Hour 6 | 3.0 (2.0–4.0) | 3.0 (2.0–3.0) | 3.0 (3.0–4.0) | 0.002 * |
| Hour 24 | 2.0 (2.0–3.0) | 2.0 (1.0–2.0) | 3.0 (2.0–3.0) | 0.004 * |
| Day 3 | 2.0 (1.0–2.0) | 1.0 (1.0–2.0) | 2.0 (1.0–3.0) | 0.001 * |
| Day 7 | 1.0 (0–1.0) | 0.0 (0–1.0) | 1.0 (1.0–2.0) | 0.003 * |
| PPPM Median (IQR) | ||||
| Hour 1 | 10.0 (8.0–11.0) | 7.0 (6.0–9.0) | 11.0 (9.0–12.0) | 0.001 * |
| Hour 6 | 9.0 (7.0–10.0) | 6.0 (5.0–8.0) | 9.0 (8.0–10.0) | 0.001 * |
| Hour 24 | 8.0 (6.0–9.0) | 6.0 (5.0–7.0) | 8.0 (7.0–9.0) | 0.003 * |
| Time Point | Comparison | Median Difference (95% CI) | Adjusted z | Adj. p Value ᵃ |
|---|---|---|---|---|
| Hour 1 | Group 2 vs. Group 1 | 1.0 (0.5–1.5) | 3.54 | 0.001 *, η2 = 0.12 |
| Group 2 vs. Group 3 | −1.0 (−1.5–−0.5) | −4.66 | 0.000 *, η2 = 0.18 | |
| Group 1 vs. Group 3 | −0.5 (−1.0–0.5) | −1.15 | 0.750, η2 = 0.02 | |
| Hour 6 | Group 2 vs. Group 1 | 0.0 (−0.5–0.5) | 1.38 | 0.507 |
| Group 2 vs. Group 3 | −1.0 (−1.5–−0.5) | −3.48 | 0.002 * | |
| Group 1 vs. Group 3 | −0.5 (−1.0–0.0) | −2.13 | 0.099 | |
| Hour 24 | Group 2 vs. Group 1 | −0.5 (−1.0–0.0) | 2.00 | 0.136 |
| Group 2 vs. Group 3 | −1.0 (−1.5–−0.5) | −3.29 | 0.003 * | |
| Group 1 vs. Group 3 | −0.5 (−1.0–0.5) | −1.31 | 0.571 | |
| Day 3 | Group 2 vs. Group 1 | −1.0 (−1.5–−0.5) | 2.94 | 0.010 * |
| Group 2 vs. Group 3 | −1.0 (−1.5–−0.5) | −3.87 | 0.000 * | |
| Group 1 vs. Group 3 | −0.5 (−1.0–0.5) | −0.96 | 1.000 | |
| Day 7 | Group 2 vs. Group 1 | 0.0 (−0.5–0.5) | 1.35 | 0.533 |
| Group 2 vs. Group 3 | −1.0 (−1.5–−0.5) | −3.39 | 0.002 * | |
| Group 1 vs. Group 3 | −0.5 (−1.0–0.5) | −2.07 | 0.117 |
| Time Point | Comparison | Median Difference (95% CI) | Adjusted z | Adj. p Value ᵃ |
|---|---|---|---|---|
| Hour 1 | Group 2 vs. Group 1 | 2.0 (1.0–3.0) | 3.81 | 0.000 *, η2 = 0.15 |
| Group 2 vs. Group 3 | −3.0 (−4.0–−2.0) | −4.72 | 0.000 *, η2 = 0.20 | |
| Group 1 vs. Group 3 | −1.0 (−2.0–0.0) | −0.94 | 1.000 *, η2 = 0.04 | |
| Hour 6 | Group 2 vs. Group 1 | 2.0 (1.0–3.0) | 2.93 | 0.010 * |
| Group 2 vs. Group 3 | −3.0 (−4.0–−2.0) | −4.04 | 0.000 * | |
| Group 1 vs. Group 3 | −1.0 (−2.0–0.0) | −1.13 | 0.780 | |
| Hour 24 | Group 2 vs. Group 1 | −2.0 (−3.0–−1.0) | −2.49 | 0.039 * |
| Group 2 vs. Group 3 | 2.0 (1.0–3.0) | 3.25 | 0.003 * | |
| Group 1 vs. Group 3 | 0.0 (−1.0–1.0) | 0.76 | 1.000 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aytac, I.; Güzel, B.; Tunc, O.; Baysal, E.; Bescocuklu, F.U. Comparative Evaluation of Cold Dissection (Suture vs. Ligation) and Hot Dissection Tonsillectomy in Children: Postoperative Pain, Bleeding, and Operative Time. J. Clin. Med. 2025, 14, 6491. https://doi.org/10.3390/jcm14186491
Aytac I, Güzel B, Tunc O, Baysal E, Bescocuklu FU. Comparative Evaluation of Cold Dissection (Suture vs. Ligation) and Hot Dissection Tonsillectomy in Children: Postoperative Pain, Bleeding, and Operative Time. Journal of Clinical Medicine. 2025; 14(18):6491. https://doi.org/10.3390/jcm14186491
Chicago/Turabian StyleAytac, Ismail, Berkay Güzel, Orhan Tunc, Elif Baysal, and Fatih Ubeydullah Bescocuklu. 2025. "Comparative Evaluation of Cold Dissection (Suture vs. Ligation) and Hot Dissection Tonsillectomy in Children: Postoperative Pain, Bleeding, and Operative Time" Journal of Clinical Medicine 14, no. 18: 6491. https://doi.org/10.3390/jcm14186491
APA StyleAytac, I., Güzel, B., Tunc, O., Baysal, E., & Bescocuklu, F. U. (2025). Comparative Evaluation of Cold Dissection (Suture vs. Ligation) and Hot Dissection Tonsillectomy in Children: Postoperative Pain, Bleeding, and Operative Time. Journal of Clinical Medicine, 14(18), 6491. https://doi.org/10.3390/jcm14186491








