1. Introduction
Reconstructive approach after mastectomy must take into account the type and stage of breast cancer, need for neoadjuvant or adjuvant treatment, and aesthetic goals. Assessments must be coupled with breast volume and grade of ptosis. An inverted T-shaped surgical incision, known as the Wise pattern [
1], is often employed in large-volume ptotic breast reconstruction and reduction mammoplasties despite reported inferior aesthetic outcomes [
2,
3], decreased vascularity [
4], and major ischemic complications [
5].
Autologous reconstruction is relatively contraindicated in large-volume breasts due to increased weight associated with skin and nipple necrosis [
6]. Immediate direct-to-implant (DTI) reconstruction complication rates are 30% [
7]. Wise-pattern specific postoperative complications in this population include delayed wound healing [
7], partial or total areolar complex loss, and wound dehiscence [
8]. Unfavorable aesthetics result in an unnatural breast shape, causing pseudo-ptosis [
9].
The senior author in this study proposes a technical refinement to DTI breast reconstruction for those with large-volume breasts and high BMIs. This approach avoids a vertical incision, mitigating complications associated with the T-junction of a Wise pattern incision in large-volume reconstruction, which may obtain a superior cosmetic outcome. The proposed approach would allow for an increase in surface area by using a vascularized dermal flap with subcutaneous fat for areolar–nipple complex support after a nipple-sparing mastectomy.
The primary objective is to propose a technical refinement for a single-stage direct-to-implant reconstruction that preserves the nipple–areola complex (NAC) in extremely ptotic large-volume breasts without compromising aesthetic outcome. The senior author shares this approach via retrospective case series at a single academic institution.
The aim of the study is to evaluate the safety, viability, and feasibility of performing single-stage direct-to-implant pre-pectoral large-volume implant-based breast reconstruction by creating an intraoperative dermal pedicle.
2. Materials and Methods
This is a retrospective case series conducted at City of Hope, Duarte, California, from 2019 to 2024. Patients who underwent a direct-to-implant breast reconstruction without a Wise-pattern incision after a nipple-sparing mastectomy were included. Data was extracted from the electronic health record. The study was evaluated and approved for exempt status by the Institutional Review Board at City of Hope National Medical Center in Duarte, California (Protocol# 21567, Reference #220395). Informed consent was not required under the exempt status, as all patient information was deidentified.
Inclusion criteria included patients who were female, received a nipple-sparing mastectomy, had large-volume breasts, underwent a DTI reconstruction without the Wise pattern, a sternal notch to nipple distance of >35 cm, and implant sizes ranging from 750 to 850 cc. Exclusion criteria included diabetic patients, smokers, prior radiotherapy, males, and those who did not receive these procedures. Additional patient details collected included demographic information, surgical indications, age, BMI, mastectomy weight, breast width, distance from sternal notch to nipple in cm (SN-N), comorbidities, post-operative complications, and follow-up procedures.
Patient cosmetic outcomes were based on subjective surgeon reports. Due to the nature of a retrospective analysis, no questionnaires were obtained. Postoperative complications, readmissions, or reoperations were found within the electronic health record. No formal scoring system was implemented or statistical analyses performed for the equation, as this study focuses on presenting an updated surgical method that has not yet gone through standardization or validation.
Proposed Operative Technique: “The Carre Modification of the Passot Technique”
The author describes an equation to predict breast projection and overall shape based on the desired breast size.
Each implant style has a projection profile from low, moderate, full, to extra-full profile. Calculate the projection of the implant with equation Z’ = X + Y (
Figure 1). For an implant projection of 5 cm or more, the equation is adjusted to Z’ = Z + 4. For a projection less than 5 cm, the equation is adjusted to Z’ = Z + 2. Z is the inframammary fold (IMF). Z’ is the measurement width of the new breast pocket that will be created. X is the distance from the meridian to the edge of the medial triangle. Y is the distance from the meridian to the edge of the lateral triangle. These triangles allow for a predictable and proportional reduction in the circumference of the breast envelope.
The precise location of the new NAC will be in relation to the inframammary fold (IMF). The procedure begins with a careful marking of the breast envelope to be removed. A double incision is made, which allows for a wide vascularized pedicle base and ensures NAC viability.
The length between the nipple and IMF is predetermined by the desired breast size. This distance is found by dividing the new NAC and the upper incision of the double incision by half. This includes the 2.5 cm that is standard at the level of the meridian. This creates the upper pole of the new breast pocket.
The inferior incision of the double incision is made 1.5 cm superior to the IMF and incrementally increases up to 2.5 cm at the meridian, creating a total width of 3 cm before decreasing in size to 1.5 cm as it proceeds away from the meridian, in either a medial or lateral direction. This allows for concealment of the incision without disrupting the anatomical insertion of the native IMF. This technique creates the desired width, Z’.
Once the upper pole of the new breast pocket is defined, an acellular dermal matrix (ADM) is sutured in place using a locking 2-0 PDS on a CT-2 needle in a running fashion. This reconstructs the superior edge of the ADM to the pectoralis major muscle within the upper pole of the new breast pocket. The ADM is tailored to size, and the inferior edge of the ADM is reconstructed with the vascularized pedicle. This assures the location of the NAC and allows for control of the medial and lateral pre-pectoral neo-pocket spaces. The combination of the ADM and newly created flap is sufficient to support the weight of the breast and implant.
Excess tissue is removed via a lateral triangle. The vascularized dermal flap with underlying adipose tissue is then developed, taking care to preserve the blood supply to the NAC. The broad inferior vascularized dermal flap is maintained to ensure adequate blood flow. Once excess tissue is removed, the remaining breast envelope is redraped and sutured into the desired shape over the pre-pectoral construct to include the vascularized dermal flap at the inferior pole and a vascular dermal matrix at the superior pole. The NAC is then repositioned to a more aesthetically pleasing location, and incisions are closed in the usual fashion.
3. Results
Eight breasts from five patients fulfilled the inclusion criteria (
Table 1). The average BMI was 38 kg/m
2. Patient age ranged from 42 to 51 years, with a mean age of 50.4 years. Three of the five patients had bilateral mastectomies, and two had unilateral mastectomies. Initial cup sizes ranged from 42 F to 46 HH. The average breast width prior to surgery was 15.88 cm. The mean distance from the sternal notch to nipple (SN-N) was 37.13 cm. The average mastectomy weight for the eight individual breasts was 1178.38 g. Implant size ranged from 750 cc to 800 cc.
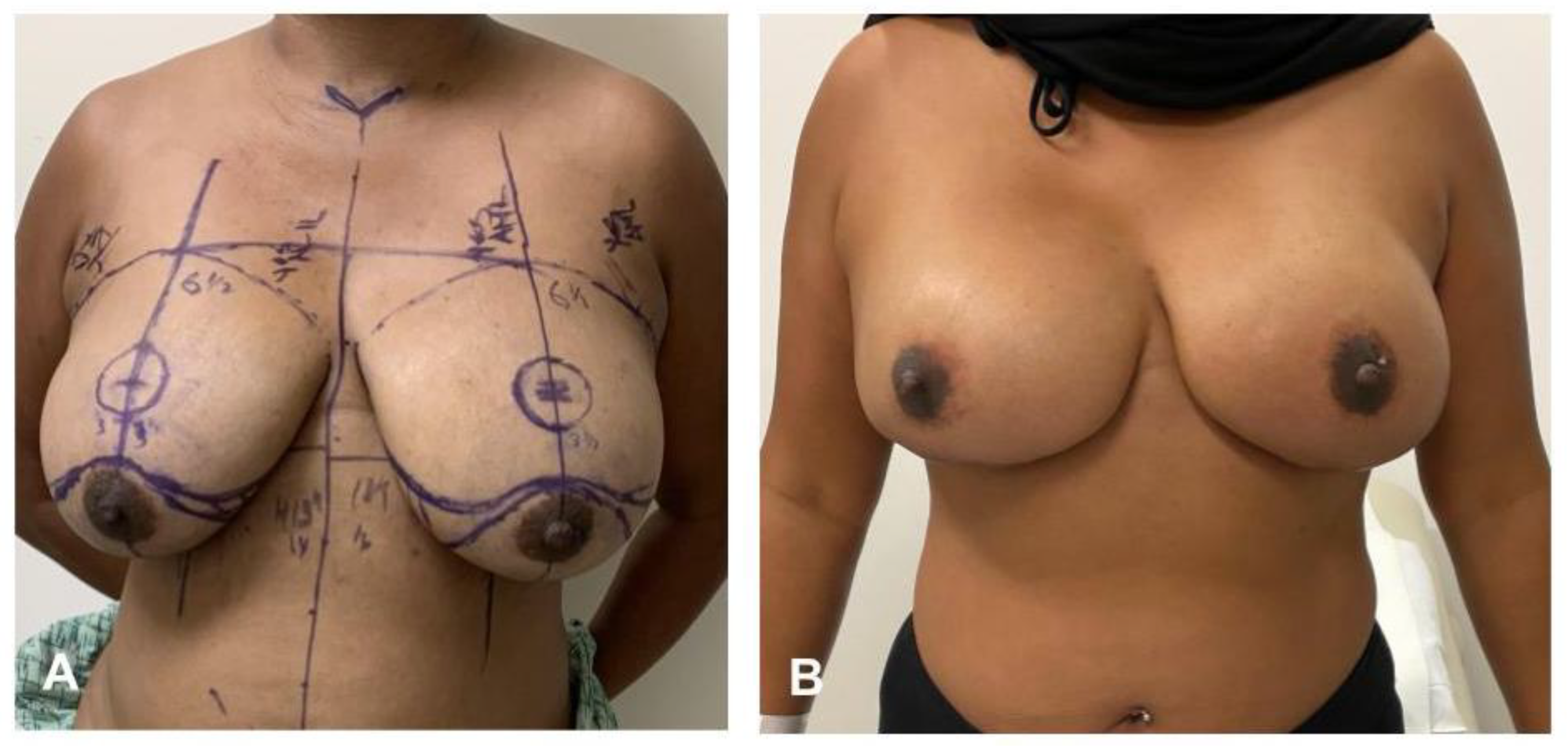
Pre- and post-operative images are shown in
Figure 2 and
Figure 3. The senior surgeon subjectively assessed aesthetic outcomes during follow-up visits. All outcomes were uniformly positive and described with satisfactory results based on clinical impression of symmetry, contour, and quality of scar healing. This was not rated on a standardized or validated scoring system due to the nature of retrospective data collection.
One patient has a small area of ischemia at the superior nipple–areolar complex with no other complications documented. There were no recorded cases of large flap necrosis, nipple loss, infection, wound dehiscence, hematoma, seroma, or need for reoperation during the follow-up period. While no complications were observed, the sample size was limited.
4. Discussion
Patients with large-volume ptotic breasts face significant physical and psychological challenges in the form of chronic pain, rashes, infection, and body image issues [
10], while redundant skin increases single-stage surgeries. These additionally come with an increased risk of tissue necrosis [
6], significant scarring, breast asymmetry, bleeding, and poor wound healing [
11]. Large and ptotic breasts also have higher rates of breast reconstruction after mastectomy compared to smaller nonptotic breasts [
12]. Historically, the Wise pattern has been employed in reduction mammoplasties to address skin redundancy while lifting the breast to restore the appropriate shape [
11]. However, inverted T mammoplasty patterns can result in unreliable skin flaps and carry a risk of T-junction necrosis with subsequent implant exposure [
11]. Additionally, inverted-T shape incisions and the weight of the mastectomy specimen are independent factors statistically associated with a higher risk of major ischemic complications [
5]. For patients with large-volume breasts who have undergone nipple-sparing mastectomies, there are additional complications of incision site tension and compromised blood supply to the nipple–alveolar complex (NAC) [
8,
11], making large-volume breasts and their surgical approach an area requiring further investigation.
This case series highlights eight total large-volume breasts that received the Carre Modification incision, with only one patient with a small area of superior ischemia at the NAC with adequate resolution. No reports of skin flap necrosis or nipple loss demonstrate the applicability and suitability of the procedure in this patient demographic. Previous technical changes to the inverted T shape have implemented horizontal or concealed incisions within the inframammary fold with positive outcomes similar to findings in this series. Inframammary fold incisions had significantly higher postoperative Breast-Q scores and higher surgeon-reported symmetry, contour, and scar appearance [
13]. The Boston modification demonstrated that larger breasts had lower rates of hematomas and scar hypertrophy [
14] while the Passot technique, from which this modification was derived, showed reduced operative time and visible scarring while preserving nipple viability [
7].
Positive aesthetic outcomes were documented in this case series by the surgeon, which aligns with similar published studies. Nipple-adjacent versus distal scars have been aesthetically compared with findings of proximal NAC scars to be the least aesthetically pleasing [
3], while those that were hidden were more highly rated [
2] compared to any transverse scars. Overall, postoperative patients reported satisfaction rates after immediate breast reconstruction and showed they would choose this option if presented to avoid [
15] scarring as much as possible.
When leaving subcutaneous fat, breast tissue is left behind due to the space between the breast and parenchyma. No study has shown that complete irradiated breast tissue has been left behind during these procedures. This technique does not influence the mastectomy plane and its ability to perform a total mastectomy.
Infarct IMF and the newly created flap are stitched superiorly. ADM was attached to the vascularized dermal flap with adherent adipose tissue and is sufficient to support the weight of large ptotic breasts.
This technique eliminates the need for a vertical scar, unlike traditional reduction mammoplasty techniques. Large-volume and ptotic breasts come with a multitude of complications regardless of incision type, yet variations to the Wise pattern are not recommended in this population. This case series hopes to add to the growing body of evidence of adjusted surgical approaches to large-volume breasts while offering an option that provides possibly both improved aesthetic outcomes and decreased complication rates.
This study was not compared against the Wise-pattern or other technical approaches. However, scarring has remained minimal, and the overall scar burden is decreased.
Limitations include the small sample size, a single institution, and a lack of long-term follow-up beyond one year post-operatively. There was no comparison against standardized Wise pattern outcomes or validation for scoring, and data remains empirical evidence, thus limiting and remaining preliminary in its recommendations. The authors recognize these limitations. Future direction of this work would benefit from standardized protocols pre- and post-operatively, including complications and aesthetics. Additional considerations include comparison with popular reconstructive approaches and long-term outcomes. Currently, a prospective trial is being developed with more robust numbers and standardized measures to further validate the superiority of this approach for single-stage direct-to-implant pre-pectoral large-volume breast reconstruction.
5. Conclusions
A refinement to a common direct-to-implant breast reconstruction technique has the potential to decrease wound tension, preserve vascular supply, and improve aesthetic outcomes in large-volume ptotic breasts.
Author Contributions
Conceptualization, methodology, and validation, A.L.C.; formal analysis, A.L.C. and K.L.V.; investigation, A.-P.S., K.L.V. and R.M.C.; data curation, K.L.V.; writing—original draft preparation, K.L.V. and A.-P.S.; writing—review and editing, K.L.V. and R.M.C.; visualization, K.L.V.; supervision, A.L.C.; project administration, A.L.C.; funding acquisition, A.L.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of City of Hope (Protocol# 21567, Reference# 220395) under Exempt status, for which consent is not required.
Informed Consent Statement
This study did not require informed consent.
Data Availability Statement
The original contributions presented in this study are included in the article. Further inquiries can be directed to the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Escandón, J.M.; Butterfield, J.A.; Christiano, J.G.; Gooch, J.C.; Olzinski, A.T.; Prieto, P.A.; Skinner, K.A.; Langstein, H.N.; Manrique, O.J. Wise Pattern versus Transverse Pattern Mastectomy in Two-Stage Implant-Based Breast Reconstruction: A Propensity Score–Matched Analysis. Plast. Reconstr. Surg. 2023, 152, 69S–80S. [Google Scholar] [CrossRef] [PubMed]
- Lotan, A.M.; Tongson, K.C.; Police, A.M.; Dec, W. Mastectomy Incision Design to Optimize Aesthetic Outcomes in Breast Reconstruction. Plast. Reconstr. Surg. Glob. Open 2020, 8, e3086. [Google Scholar] [CrossRef] [PubMed]
- Dunson, B.T.; Zaki, D.P.; Blondin, M.S.; Duet, M.L.; Steele, T.; Pestana, C.V.; Pestana, I.A. Crowdsourced Comparison of Aesthetic Outcomes of Traditional Transverse Versus Skin-Reducing Mastectomy Incision Patterns Following Implant-Based Breast Reconstruction. Cureus 2025, 17, e79924. [Google Scholar] [CrossRef] [PubMed]
- Ahn, S.J.; Woo, T.Y.; Lee, D.W.; Lew, D.H.; Song, S.Y. Nipple-areolar complex ischemia and necrosis in nipple-sparing mastectomy. Eur. J. Surg. Oncol. J. Eur. Soc. Surg. Oncol. Br. Assoc. Surg. Oncol. 2018, 44, 1170–1176. [Google Scholar] [CrossRef] [PubMed]
- Salibian, A.A.; Bekisz, J.M.; Frey, J.D.; Thanik, V.D.; Levine, J.P.; Karp, N.S.; Choi, M. Comparing Incision Choices in Immediate Microvascular Breast Reconstruction after Nipple-Sparing Mastectomy: Unique Considerations to Optimize Outcomes. Plast. Reconstr. Surg. 2021, 148, 1173–1185. [Google Scholar] [CrossRef] [PubMed]
- Antoniazzi, E.; De Grazia, A.; Dell’Antonia, F.; Pasquali, S.; Burelli, P.; Rizzetto, C.; Berna, G. Immediate prepectoral breast reconstruction in nipple-sparing mastectomy with Wise-pattern incision in large and ptotic breasts: Our experience and short-term results. J. Plast. Reconstr. Aesthetic Surg. JPRAS 2024, 91, 154–163. [Google Scholar] [CrossRef] [PubMed]
- Corban, J.; Shash, H.; Safran, T.; Sheppard-Jones, N.; Fouda-Neel, O. A systematic review of complications associated with direct implants vs. tissue expanders following Wise pattern skin-sparing mastectomy. J. Plast. Reconstr. Aesthetic Surg. JPRAS 2017, 70, 1191–1199. [Google Scholar] [CrossRef] [PubMed]
- Woo, S.H.; Lee, S.J.; Kim, E.K.; Han, H.H.; Eom, J.S. Safety of Augmenting Breast Volume in Direct-to-Implant Breast Reconstruction With Contralateral Breast Augmentation: Comparison With 2-Stage Reconstruction. Ann. Plast. Surg. 2023, 91, 693–697. [Google Scholar] [CrossRef] [PubMed]
- Brown, R.H.; Siy, R.; Khan, K.; Izaddoost, S. The Superomedial Pedicle Wise-Pattern Breast Reduction: Reproducible, Reliable, and Resilient. Semin. Plast. Surg. 2015, 29, 94–101. [Google Scholar] [CrossRef] [PubMed]
- Colizzi, L.; Lazzeri, D.; Agostini, T.; Giannotti, G.; Ghilli, M.; Gandini, D.; Pantaloni, M.; Roncella, M. Skin-reducing mastectomy: New refinements. J. Plast. Surg. Hand Surg. 2010, 44, 296–301. [Google Scholar] [CrossRef] [PubMed]
- Roy, P.G. Modified Lower Pole Autologous Dermal Sling for Implant Reconstruction in Women Undergoing Immediate Breast Reconstruction after Mastectomy. Int. J. Breast Cancer 2016, 2016, 9301061. [Google Scholar] [CrossRef] [PubMed]
- Thuman, J.; Freitas, A.M.; Schaeffer, C.; Campbell, C.A. Prepectoral Wise-Pattern Staged Implant-Based Breast Reconstruction for Obese or Ptotic Patients. Ann. Plast. Surg. 2019, 82, S404–S409. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Chun, Y.S.; Park, H.K.; Kim, S.E.; Kim, Y.W.; Cheon, Y.W. Inframammary Fold Incision Can Reduce Skin Flap Necrosis in Immediate Breast Reconstruction With Implant and Conjoined Fascial Flap. Ann. Plast. Surg. 2020, 85, 488–494. [Google Scholar] [CrossRef] [PubMed]
- Movassaghi, K.; Liao, E.C.; Ting, V.; Matros, E.; Morris, D.J.; Orgill, D.P.; Pribaz, J.J. Eliminating the vertical scar in breast reduction-Boston modification of the Robertson technique. Aesthet. Surg. J. 2006, 26, 687–696. [Google Scholar] [CrossRef] [PubMed]
- Saulis, A.S.; Mustoe, T.A.; Fine, N.A. A retrospective analysis of patient satisfaction with immediate postmastectomy breast reconstruction: Comparison of three common procedures. Plast. Reconstr. Surg. 2007, 119, 1669–1676. [Google Scholar] [CrossRef] [PubMed]
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).