Effect of Two Different Adhesion Modes of a Universal Resin Cement on the Retention of Glass Fiber Posts Cemented to Root Canal Dentine: An In Vitro Study
Abstract
1. Introduction
2. Materials and Methods
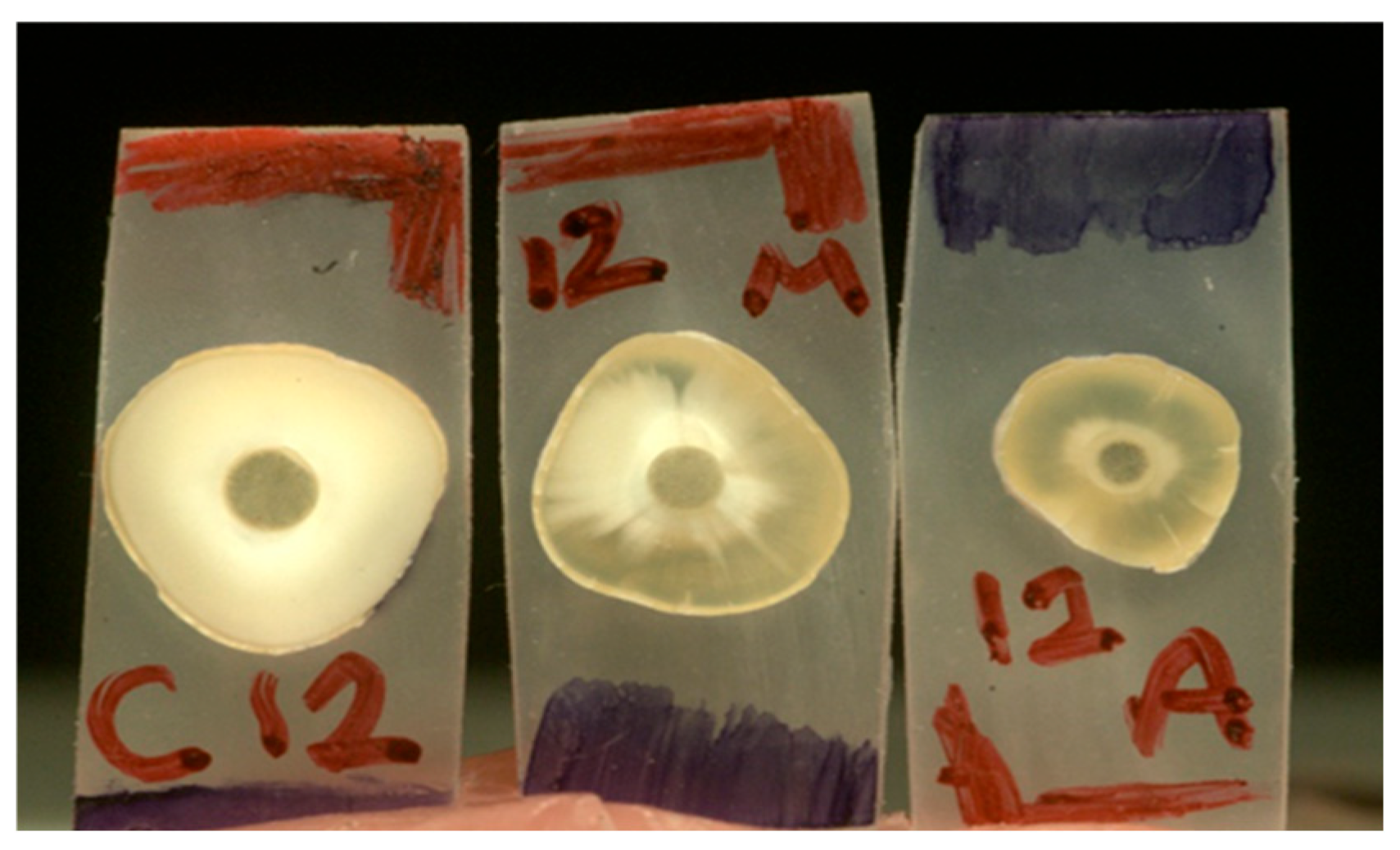
2.1. Specimen Preparation
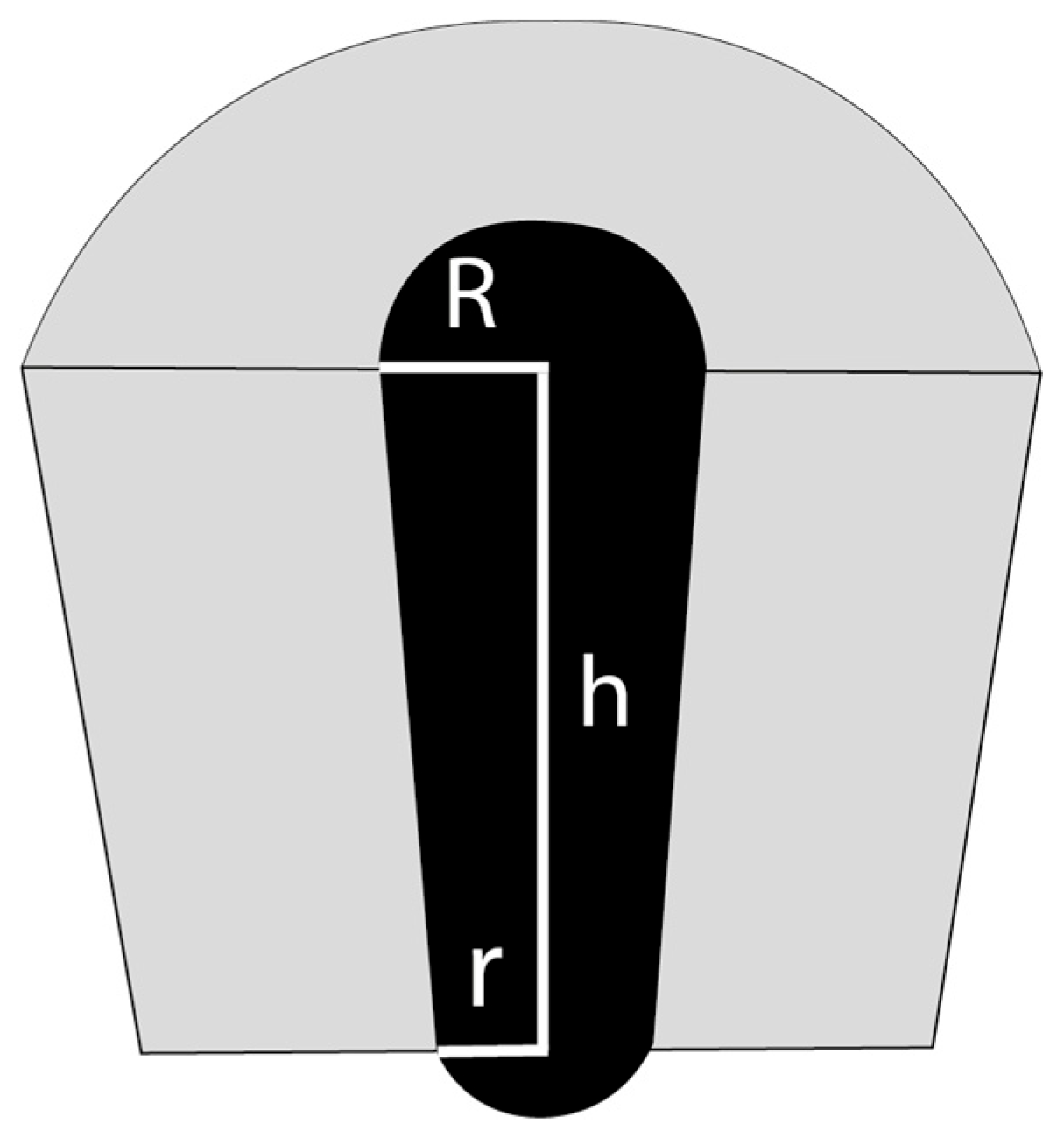
2.2. Bond Strength
2.3. Statistical Analysis
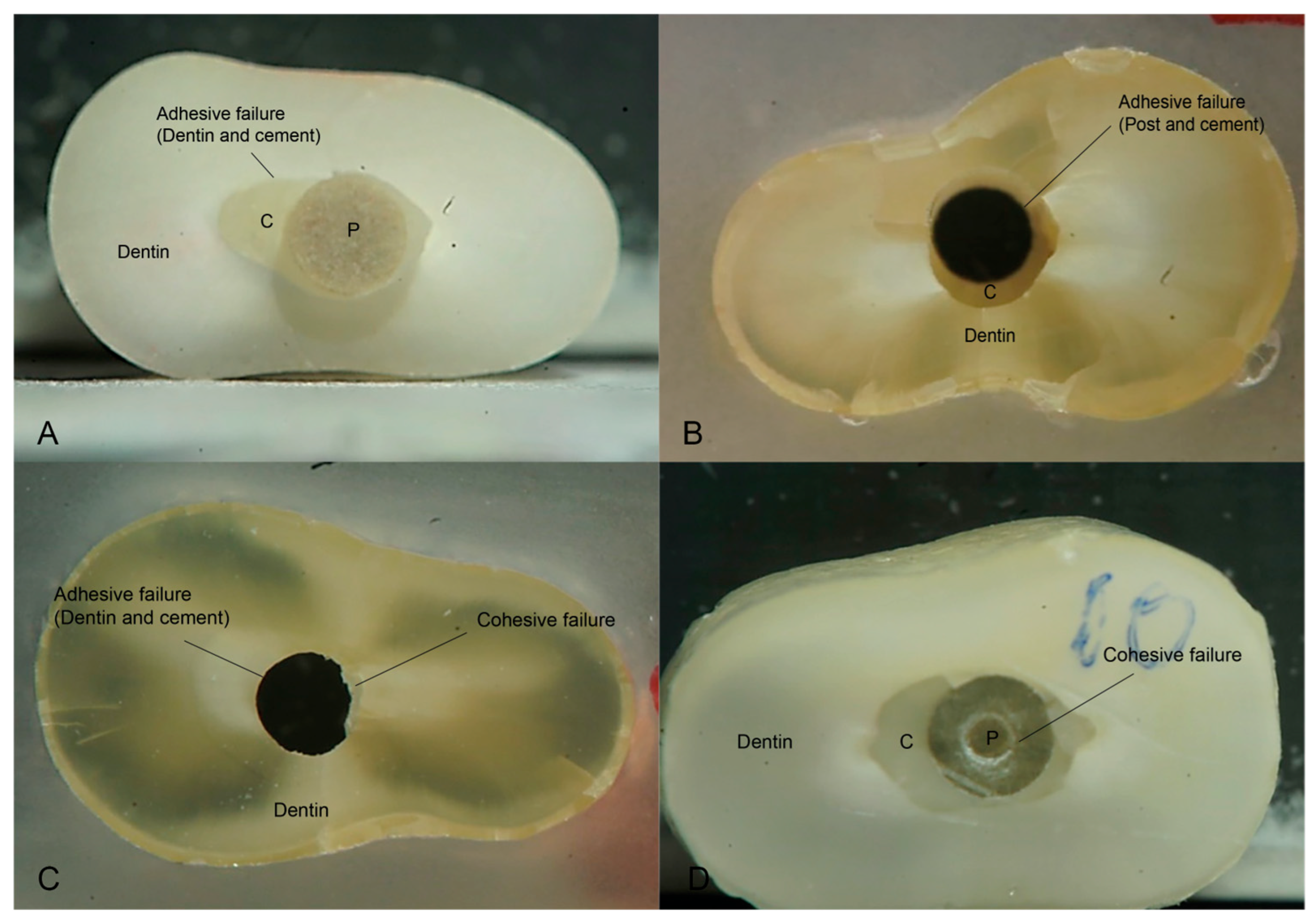
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Carvalho, M.A.; Lazari, P.C.; Gresnigt, M.; Del Bel Cury, A.A.; Magne, P. Current options concerning the endodontically-treated teeth restoration with the adhesive approach. Braz. Oral Res. 2018, 32, e74. [Google Scholar] [CrossRef]
- Wandscher, V.F.; Bergoli, C.D.; Limberger, I.F.; Ardenghi, T.M.; Valandro, L.F. Preliminary results of the survival and fracture load of roots restored with intracanal posts: Weakened vs nonweakened roots. Oper. Dent. 2014, 39, 541–555. [Google Scholar] [CrossRef] [PubMed]
- Alshabib, A.; Abid Althaqafi, K.; AlMoharib, H.S.; Mirah, M.; AlFawaz, Y.F.; Algamaiah, H. Dental Fiber-Post Systems: An In-Depth Review of Their Evolution, Current Practice and Future Directions. Bioengineering 2023, 10, 551. [Google Scholar] [CrossRef]
- Ferrari, M.; Vichi, A.; Mannocci, F.; Mason, P.N. Retrospective study of the clinical performance of fiber posts. Am. J. Dent. 2000, 13, 9b–13b. [Google Scholar]
- AlMadi, M.K.; Khabeer, A.; AlHilal, S.; AlShahrani, A.S.; Ali, S. Pull-out bond strength of fiber post luted with two types of resin luting cements using different light curing units. Niger. J. Clin. Pract. 2021, 24, 1841–1845. [Google Scholar] [CrossRef]
- Marchionatti, A.M.E.; Wandscher, V.F.; Rippe, M.P.; Kaizer, O.B.; Valandro, L.F. Clinical performance and failure modes of pulpless teeth restored with posts: A systematic review. Braz. Oral Res. 2017, 31, e64. [Google Scholar] [CrossRef] [PubMed]
- Freitas, T.L.; Vitti, R.P.; Miranda, M.E.; Brandt, W.C. Effect of Glass Fiber Post Adaptation on Push-Out Bond Strength to Root Dentin. Braz. Dent. J. 2019, 30, 350–355. [Google Scholar] [CrossRef] [PubMed]
- De Goes, M.F.; Giannini, M.; Foxton, R.M.; Nikaido, T.; Tagami, J. Microtensile bond strength between crown and root dentin and two adhesive systems. J. Prosthet. Dent. 2007, 97, 223–228. [Google Scholar] [CrossRef]
- Mjör, I.A.; Smith, M.R.; Ferrari, M.; Mannocci, F. The structure of dentine in the apical region of human teeth. Int. Endod. J. 2001, 34, 346–353. [Google Scholar] [CrossRef]
- Radovic, I.; Mazzitelli, C.; Chieffi, N.; Ferrari, M. Evaluation of the adhesion of fiber posts cemented using different adhesive approaches. Eur. J. Oral Sci. 2008, 116, 557–563. [Google Scholar] [CrossRef]
- Sarkis-Onofre, R.; Skupien, J.A.; Cenci, M.S.; Moraes, R.R.; Pereira-Cenci, T. The role of resin cement on bond strength of glass-fiber posts luted into root canals: A systematic review and meta-analysis of in vitro studies. Oper. Dent. 2014, 39, E31–E44. [Google Scholar] [CrossRef]
- Angnanon, W.; Thammajaruk, P.; Guazzato, M. Effective luting agents for glass-fiber posts: A network meta-analysis. Dent. Mater. 2023, 39, 1180–1189. [Google Scholar] [CrossRef] [PubMed]
- Bergoli, C.D.; Brondani, L.P.; Wandscher, V.F.; Pereira, G.; Cenci, M.S.; Pereira-Cenci, T.; Valandro, L.F. A Multicenter Randomized Double-blind Controlled Clinical Trial of Fiber Post Cementation Strategies. Oper. Dent. 2018, 43, 128–135. [Google Scholar] [CrossRef] [PubMed]
- Oskoee, S.S.; Bahari, M.; Kimyai, S.; Asgary, S.; Katebi, K. Push-out Bond Strength of Fiber Posts to Intraradicular Dentin Using Multimode Adhesive System. J. Endod. 2016, 42, 1794–1798. [Google Scholar] [CrossRef] [PubMed]
- Kosan, E.; Prates-Soares, A.; Blunck, U.; Neumann, K.; Bitter, K. Root canal pre-treatment and adhesive system affect bond strength durability of fiber posts ex vivo. Clin. Oral Investig. 2021, 25, 6419–6434. [Google Scholar] [CrossRef]
- Thanikachalam, Y.; Kadandale, S.; Ilango, S.; Parthasarathy, R.; Vishwanath, S.; Srinivasan, S. Comparative Evaluation of Retention of Fiber Posts in Different Dentin Regions Using Various Bonding Techniques: An In Vitro Study. Cureus 2023, 15, e33971. [Google Scholar] [CrossRef] [PubMed]
- Gwinnett, A.J. Quantitative contribution of resin infiltration/hybridization to dentin bonding. Am. J. Dent. 1993, 6, 7–9. [Google Scholar]
- Comba, A.; Baldi, A.; Juzikis, E.; Vergano, E.A.; Pasqualini, D.; Alovisi, M.; Berutti, E.; Scotti, N. Does Curing Delay Affect the Bond Strength of Fiber Post with Self-Adhesive Cements? Int. J. Prosthodont. 2023, 36, 595–602. [Google Scholar] [CrossRef]
- Bitter, K.; Paris, S.; Pfuertner, C.; Neumann, K.; Kielbassa, A.M. Morphological and bond strength evaluation of different resin cements to root dentin. Eur. J. Oral Sci. 2009, 117, 326–333. [Google Scholar] [CrossRef]
- Yumi Umeda Suzuki, T.; Gomes-Filho, J.E.; Fraga Briso, A.L.; Gonçalves Assunção, W.; Dos Santos, P.H. Influence of the depth of intraradicular dentin on the pushout bond strength of resin materials. J. Investig. Clin. Dent. 2019, 10, e12461. [Google Scholar] [CrossRef]
- Machry, R.V.; Fontana, P.E.; Bohrer, T.C.; Valandro, L.F.; Kaizer, O.B. Effect of Different Surface Treatments of Resin Relined Fiber Posts Cemented With Self-adhesive Resin Cement on Push-out and Microtensile Bond Strength Tests. Oper. Dent. 2020, 45, E185–E195. [Google Scholar] [CrossRef]
- Kitzmüller, K.; Graf, A.; Watts, D.; Schedle, A. Setting kinetics and shrinkage of self-adhesive resin cements depend on cure-mode and temperature. Dent. Mater. 2011, 27, 544–551. [Google Scholar] [CrossRef]
- Calixto, L.R.; Bandéca, M.C.; Clavijo, V.; Andrade, M.F.; Vaz, L.G.; Campos, E.A. Effect of resin cement system and root region on the push-out bond strength of a translucent fiber post. Oper. Dent. 2012, 37, 80–86. [Google Scholar] [CrossRef] [PubMed]
- Andrews, E.K.; Gedge, J.L.; Vandewalle, K.S. Bond Strength of a Novel Universal Resin Cement to Dentin with or without an Adhesive Bonding Agent: An In Vitro Study. J. Contemp. Dent. Pract. 2023, 24, 725–728. [Google Scholar] [CrossRef] [PubMed]
- Fokkinga, W.A.; Kreulen, C.M.; Vallittu, P.K.; Creugers, N.H. A structured analysis of in vitro failure loads and failure modes of fiber, metal, and ceramic post-and-core systems. Int. J. Prosthodont. 2004, 17, 476–482. [Google Scholar] [PubMed]
- Cheniski, D.A.; Freire, A.; Camargo, E.S.; da Costa, R.G.; de Souza, E.M.; Rached, R.N. Bond strength of prefabricated and CAD-CAM milled glass fiber post-and-cores luted with conventional, universal, and self-adhesive composite resin cement. J. Prosthet. Dent. 2024, 131, 251.e1–251.e7. [Google Scholar] [CrossRef]
| Surface Area [mm2] | |
|---|---|
| Coronal | 9.55 ± 0.81 |
| Middle | 7.22 ± 0.57 |
| Apical | 5.26 ± 1.14 |
| GP1—Self Adhesive | GP2—Adhesive | p-Value | |||
|---|---|---|---|---|---|
| Mean Bond Strength [Mpa] | SD [Mpa] | Mean Bond Strength [Mpa] | SD [Mpa] | ||
| Coronal | 13.04 | 2.62 | 17.65 | 4.68 | 0.014 |
| Middle | 16.29 | 5.35 | 20.07 | 6.79 | 0.184 |
| Apical | 20.47 | 7.58 | 23.78 | 9.77 | 0.409 |
| Failure Mode [%] | ||||
|---|---|---|---|---|
| Adhesive Dentine/Cement | Adhesive Post/Cement | Mixed | Cohesive | |
| Self-adhesive | 90 | 3.3 | 6.6 | 0 |
| Adhesive | 73.3 | 3.3 | 6.6 | 10 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
D’haese, R.; Vervack, V.; Hamid, I.; Vandeweghe, S. Effect of Two Different Adhesion Modes of a Universal Resin Cement on the Retention of Glass Fiber Posts Cemented to Root Canal Dentine: An In Vitro Study. Adhesives 2025, 1, 8. https://doi.org/10.3390/adhesives1020008
D’haese R, Vervack V, Hamid I, Vandeweghe S. Effect of Two Different Adhesion Modes of a Universal Resin Cement on the Retention of Glass Fiber Posts Cemented to Root Canal Dentine: An In Vitro Study. Adhesives. 2025; 1(2):8. https://doi.org/10.3390/adhesives1020008
Chicago/Turabian StyleD’haese, Rani, Valentin Vervack, Inas Hamid, and Stefan Vandeweghe. 2025. "Effect of Two Different Adhesion Modes of a Universal Resin Cement on the Retention of Glass Fiber Posts Cemented to Root Canal Dentine: An In Vitro Study" Adhesives 1, no. 2: 8. https://doi.org/10.3390/adhesives1020008
APA StyleD’haese, R., Vervack, V., Hamid, I., & Vandeweghe, S. (2025). Effect of Two Different Adhesion Modes of a Universal Resin Cement on the Retention of Glass Fiber Posts Cemented to Root Canal Dentine: An In Vitro Study. Adhesives, 1(2), 8. https://doi.org/10.3390/adhesives1020008






