Clinical Application of the EOS Imaging System—The Broader Horizon
Abstract
1. Introduction
2. Materials and Methods
2.1. Methodology
2.2. Amendment to Protocol
2.3. Search Strategy
2.4. Eligibility Criteria
2.5. Study Selection
2.6. Data Extraction
3. Results
3.1. Search and Screening
3.2. Adults
3.3. Adult Surgery
3.4. Pediatric
3.5. Pediatric Surgery
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Search Strings
| MEDLINE (PubMed) | Embase (Elsevier) | The Cochrane Library | Scopus | CINAHL Complete (EBSCO) | Academic Search Premier (EBSCO) | OpenGrey |
| ((((((((((((((((((((Biplanar x-ray) OR (Biplanar x ray)) OR (Biplanar xray)) OR (Biplanar radiograph)) OR (Biplanar radiography)) OR (Biplanar imaging)) OR (Biplane x-ray)) OR (Biplane x ray)) OR (Biplane radiograph)) OR (Biplane radiography)) OR (Biplane imaging)) OR (eos imaging)) OR (eos image)) OR (Eos images)) OR (eos radiography)) OR (Eos system)) OR (eos x-ray)) OR (eos x ray)) OR (slot scanner)) OR (slot scanners)) OR (slot scanning) | ‘biplanar x ray’ OR (biplanar AND x AND ray) OR ‘biplanar xray’ OR (biplanar AND xray) OR ‘biplanar radiograph’ OR (biplanar AND (‘radiograph’/exp OR radiograph)) OR ‘biplanar radiography’/exp OR ‘biplanar radiography’ OR (biplanar AND (‘radiography’/exp OR radiography)) OR ‘biplanar imaging’ OR (biplanar AND (‘imaging’/exp OR imaging)) OR ‘biplane x ray’ OR ((‘biplane’/exp OR biplane) AND x AND ray) OR ‘biplane xray’ OR ((‘biplane’/exp OR biplane) AND xray) OR ‘biplane radiograph’ OR ((‘biplane’/exp OR biplane) AND (‘radiograph’/exp OR radiograph)) OR ‘biplane radiography’ OR ((‘biplane’/exp OR biplane) AND (‘radiography’/exp OR radiography)) OR ‘biplane imaging’ OR ((‘biplane’/exp OR biplane) AND (‘imaging’/exp OR imaging)) OR ‘eos imaging’/exp OR ‘eos imaging’ OR ((‘eos’/exp OR eos) AND (‘imaging’/exp OR imaging)) OR ‘eos image’ OR ((‘eos’/exp OR eos) AND (‘image’/exp OR image)) OR ‘eos images’ OR ((‘eos’/exp OR eos) AND images) OR ‘eos radiography’ OR ((‘eos’/exp OR eos) AND (‘radiography’/exp OR radiography)) OR ‘eos system’/exp OR ‘eos system’ OR ((‘eos’/exp OR eos) AND system) OR ‘eos x ray’ OR ((‘eos’/exp OR eos) AND x AND ray) OR ‘eos xray’ OR ((‘eos’/exp OR eos) AND xray) OR ‘slot scanner’ OR (slot AND (‘scanner’/exp OR scanner)) OR ‘slot scanners’ OR (slot AND scanners) OR ‘slot scanning’ OR (slot AND scanning) | Biplanar x-ray OR Biplanar x ray OR Biplanar xray OR Biplanar radiograph OR Biplanar radiography OR Biplanar imaging OR Biplane x-ray OR Biplane x ray OR Biplane xray OR Biplane radiograph OR Biplane radiography OR Biplane imaging OR eos imaging OR eos image OR Eos images OR Eos system OR eos x-ray OR eos x ray OR eos xray OR slot scanner OR slot scanners OR slot scanning | (TITLE-ABS-KEY (biplanar W/3 x-ray) OR TITLE-ABS-KEY (biplanar W/3 x AND ray) OR TITLE-ABS-KEY (biplanar W/3 radiograph) OR TITLE-ABS-KEY (biplanar W/3 radiography) OR TITLE-ABS-KEY (biplanar W/3 imaging) OR TITLE-ABS-KEY (biplane W/3 x-ray) OR TITLE-ABS-KEY (biplane W/3 x AND ray) OR TITLE-ABS-KEY (biplane W/3 radiograph) OR TITLE-ABS-KEY (biplane W/3 radiography) OR TITLE-ABS-KEY (biplane W/3 imaging) OR TITLE-ABS-KEY (eos W/3 imaging) OR TITLE-ABS-KEY (eos W/3 image) OR TITLE-ABS-KEY (eos W/3 images) OR TITLE-ABS-KEY (eos W/3 radiography) OR TITLE-ABS-KEY (eos W/3 system) OR TITLE-ABS-KEY (eos W/3 x-ray) OR TITLE-ABS-KEY (eos W/3 x AND ray) OR TITLE-ABS-KEY (slot W/3 scanner) OR TITLE-ABS-KEY (slot W/3 scanners) OR TITLE-ABS-KEY (slot W/3 scanning)) | Biplanar x-ray OR Biplanar x ray OR Biplanar radiograph OR Biplanar radiography OR Biplanar imaging OR Biplane x-ray OR Biplane x ray OR Biplane xray OR Biplane radiograph OR Biplane radiography OR Biplane imaging OR eos imaging OR eos image OR Eos images OR eos radiography OR Eos system OR eos x-ray OR eos x ray OR slot scanner OR slot scanners OR slot scanning | Eos images OR eos radiography OR Eos system OR eos x-ray OR eos x ray OR slot scanner OR slot scanners OR slot scanning OR Biplanar x-ray OR Biplanar x ray OR Biplanar radiograph OR Biplanar radiography OR Biplanar imaging OR Biplane x-ray OR Biplane x ray OR Biplane radiograph OR Biplane radiography OR Biplane imaging OR eos imaging OR eos image OR eos images OR eos radiography OR eos system OR eos x-ray OR eos x ray OR slot scanner OR slot scanners OR slot scanning | (biplane AND x-ray) OR (biplane AND x ray) OR (biplane AND xray) OR (biplane AND imaging) OR (eos AND imaging) OR (eos AND image) OR (eos AND images) OR (eos AND system) |
Appendix B. Adult Imaging Using the EOS Imaging System
| Author, Year, Country | Title | Clinical Endpoints (Parameters) | Total n | Timeline | Study Type | |
| Center of mass analysis | ||||||
| Amabile, 2015, FR [45] | Alignment of centers of mass of body segments with the gravity line | Spinal/balance | 20 |  |  | |
| Head analysis | ||||||
| Berg, 2020, CH [46] | Experiences with a new biplanar low-dose X-ray device for imaging the facial skeleton: a feasibility study | Cephalometric angles/distances | 12 |  |  | |
| Kerbrat, 2021, FR [47] | Biplanar low-dose radiograph is suitable for cephalometric analysis in patients requiring 3D evaluation of the whole skeleton | Cephalometric angles/distances | 13 |  |  |  |
| Lower extremity analysis | ||||||
| Buck, 2012, CH [48] | Femoral and tibial torsion measurements with 3D models based on low-dose biplanar radiographs in comparison with standard CT measurements | Femoral; Tibial | 35 |  |  |  |
| Cebulski-Delebarre, 2016, FR [49] | Correlation between primary flat foot and lower extremity rotational misalignment in adults | Femoral; Knee; Leg length; Pelvic; Tibial | 54 |  |  | |
| Clément, 2014, CA [50] | Influence of biomechanical multi-joint models used in global optimisation to estimate healthy and osteoarthritis knee kinematics | Knee | 10 |  |  | |
| Clément, 2018, CA [51] | Comparison of soft tissue artifact and its effects on knee kinematics between non-obese and obese subjects performing a squatting activity recorded using an exoskeleton | Femoral; Knee; Tibial | 17 |  |  | |
| Dagneaux, 2020, FR [52] | Three-dimensional biometrics to correlate hindfoot and knee coronal alignments using modern weightbearing imaging | Foot/ankle; Knee | 59 |  |  | |
| Dufrénot, 2023, FR [53] | Three-dimensional biometrics using weight-bearing imaging shows relationship between knee and hindfoot axial alignment | Femoral; Foot/ankle; Tibial | 99 |  |  | |
| Dumas, 2004, CA [54] | Determination of personalized inertial parameters of lower limb by biplanar low-dose radiography | Femoral | 12 |  |  | |
| Dumas, 2005, CA [55] | Personalized body segment parameters from biplanar low-dose radiography | Femoral | 16 |  |  | |
| Guenoun, 2012, FR [56] | Reliability of a new method for lower-extremity measurements based on stereoradiographic three-dimensional reconstruction | Femoral; Leg length; Tibial | 25 |  |  |  |
| Hecker, 2021, CH [57] | The EOS 3D imaging system reliably measures posterior tibial slope | Tibial | 56 |  |  |  |
| Kümmerlin, 2022, GE [58] | Measuring knee joint laxity in three degrees-of-freedom in vivo using a robotics- and image-based technology | Knee | 4 |  |  | |
| Lo, 2024, TW [59] | Associations between femoral 3D curvature and sagittal imbalance of spine | Femoral; Foot/ankle; Knee; Pelvic; Spinal/balance | 105 |  |  | |
| Morin, 2016, CA [60] | Assessment of femur geometrical parameters using EOS™ imaging technology in patients with atypical femur fractures; preliminary results | Femoral | 16 |  |  | |
| Moon, 2020, KR [61] | The effect of knee joint rotation in the sagittal and axial plane on the measurement accuracy of coronal alignment of the lower limb | Femoral; Knee; Pelvic; Tibial | 90 |  |  | |
| Nam, 2014, US [62] | Evaluation of the 3-dimensional, weight-bearing orientation of the normal adult knee | Femoral; Knee; Pelvic; Tibial | 100 |  |  | |
| Serrurier, 2012, FR [63] | Robust femur condyle disambiguation on biplanar X-rays | Femoral | 30 |  |  | |
| Zeighami, 2020, CA [64] | A method for quantitative evaluation of a valgus knee orthosis using biplane X-ray images | Health outcomes; Knee | 1 |  |  | |
| Lower extremity analysis—imaging comparison | ||||||
| Cho, 2021, KR [65] | Evaluation of the reliability of lower extremity alignment measurements using EOS imaging system while standing in an even weight-bearing posture | Femoral; Knee; Pelvic; Tibial | 52 |   |  |  |
| Choi, 2022, KR [66] | Comparison of lower-limb alignment in patients with advanced knee osteoarthritis: EOS biplanar stereoradiography versus conventional scanography | Knee; Pelvic; Tibial | 52 |  |  |  |
| Cosentino, 2022, CH [67] | MRI signal and morphological alterations of the suprapatellar fat pad in asymptomatic subjects: are these normal variants? | Knee; Leg length | 110 |  |  | |
| Folinais, 2013, FR [68] | Measuring femoral and rotational alignment: EOS system versus computed tomography | Femoral; Image quality; Tibial | 30 |  |  |  |
| Mayr, 2021, GE [69] | Anteversion angle measurement in suspected torsional malalignment of the femur in 3-dimensional EOS vs computed tomography—a validation study | Femoral | 19 |  |  |  |
| Narahashi, 2024, BR [70] | Measurement of tibial slope using biplanar stereoradiography (EOS®) | Knee; Tibial | 30 |  |  | |
| Rosskopf, 2019, CH [71] | 3D hindfoot alignment measurements based on low-dose biplanar radiographs: a clinical feasibility study | Foot/ankle; Tibial | 50 |  |  | |
| Störmann, 2021, GE [72] | Comparison of medial distal tibial angle in EOS imaging and weightbearing X-ray | Foot/ankle; Tibial | 41 |  |  | |
| Wise, 2020, US [73] | Reliability of EOS compared to conventional radiographs for evaluation of lower extremity deformity in adult patients | Femoral; Knee; Leg length; Tibial | 10 |  |  |  |
| Yan, 2019, CN [74] | Femoral and tibial torsion measurements based on EOS imaging compared to 3D CT reconstruction measurements | Femoral; Tibial | 18 |  |  | |
| Lower extremity analysis—knee osteoarthritis | ||||||
| Huang, 2021, HK [75] | Exploring the relationship between pain intensity and knee moments in participants with medial knee osteoarthritis: a cross-sectional study | Knee | 47 |  |  | |
| Huang, 2021, HK [76] | Knee joint loadings are related to tibial torsional alignments in people with radiographic medial knee osteoarthritis | Knee; Tibial | 47 |  |  | |
| Koliogiannis, 2021, GE [77] | Is the EOS imaging system as accurate as conventional radiography in grading osteoarthritis of the knee? | Knee | 142 |  |  | |
| Zeighami, 2017, CA [78] | Tibio-femoral joint contact in healthy and osteoarthritic knees during quasi-static squat: a bi-planar X-ray analysis | Femoral parameters; Knee parameters; Tibial parameters | 19 |  |  | |
| Lower extremity analysis—leg length | ||||||
| Clavé, 2018, FR [79] | Reproducibility of length measurements of the lower limb by using EOS™ | Femoral; Knee; Leg length; Pelvic; Tibial | 112 |  |  |  |
| Guggenberger, 2014, CH [80] | Assessment of lower limb length and alignment by biplanar linear radiography: comparison with supine CT and upright full-length radiography | Foot/ankle; Knee; Leg length | 51 |  |  |  |
| Lazennec, 2016, FR [81] | Do patients’ perceptions of leg length correlate with standing 2- and 3-dimensional radiographic imaging? | Femoral; Knee; Leg length; Tibial | 70 |  |  | |
| Patient safety and radiation exposure | ||||||
| Ben Abdennebi, 2017, FR [82] | Comparative dose levels between CT-scanner and slot-scanning device (EOS system) in pregnant women pelvimetry | Radiation dose | 20 |  |  | |
| Boutry, 2013, FR [17] | Low-dose biplanar skeletal survey versus digital skeletal survey in multiple myeloma | Health outcomes; Radiation dose/Image quality | 56 |  |  | |
| Dietrich, 2013, CH [83] | Comparison of radiation dose, workflow, patient comfort and financial break-even of standard digital radiography and a novel biplanar low-dose X-ray system for upright full-length lower limb and whole spine radiography | Financials/Workflow; Health outcomes; Radiation dose | 445 |  |  | |
| Wood, 2021, US [84] | Incidental extraspinal imaging findings on adult EOS full body radiographs: prevalence and clinical importance | Incidental findings | 503 |  |  | |
| Pelvis analysis | ||||||
| Bordes, 2023, FR [85] | The influence of the sacral slope on pelvic kinematics and clinical manifestations in femoroacetabular impingement | Pelvic; Spinal/balance | 200 |  |  | |
| Buckland, 2017, US [86] | Sagittal pelvic orientation a comparison of two methods of measurement | Pelvic; Spinal/balance | 100 |  |  |  |
| Fritz, 2019, CH [87] | Acetabular coverage differs between standing and supine positions: model-based assessment of low-dose biplanar radiographs and comparison with CT | Pelvic | 50 |  |  |  |
| Gasparutto, 2023, CH [88] | Definition and reliability of 3D acetabular and global offset measurements from bi-plane X-rays | Pelvic | 28 |  |  | |
| Kim, 2019, FR [89] | Stand-to-sit kinematics of the pelvis is not always as expected: hip and spine pathologies can have an impact | Pelvic | 90 |  |  | |
| Mussmann, 2019, DK [90] | Radiographic signs of acetabular retroversion using a low-dose slot-scanning radiographic system (EOS®) | Pelvic; Radiation dose/Image quality | 34 |  |  |  |
| Rouissi, 2017, FR [91] | Intra and inter-observer reliability of determining degree of pelvic obliquity in neuromuscular scoliosis using the EOS-CHAIR® protocol | Pelvic; Spinal/balance | 36 |  |  | |
| Thelen, 2017, FR [92] | Normative 3D acetabular orientation measurements by the low-dose EOS imaging system in 102 asymptomatic subjects in standing position: analyses by side, gender, pelvic incidence and reproducibility | Pelvic | 102 |  |  | |
| Pelvis and lower extremity analysis | ||||||
| Bendaya, 2015, FR [93] | Healthy vs. osteoarthritic hips: a comparison of hip, pelvis and femoral parameters and relationships using the EOS® system | Femoral; Pelvic | 60 |  |  | |
| Canetti, 2020, FR [94] | Spinopelvic parameters in greater trochanteric pain syndrome: a retrospective case–control study | Pelvic | 86 |  |  | |
| Coulomb, 2023, FR [95] | Radiological signs of femoroacetabular impingement are linked to pelvic version in asymptomatic subjects | Pelvic; Spinal/balance | 118 |  |  | |
| Frasson, 2022, CA [96] | Do femoral version abnormalities play a role in hip function of patients with hip pain? | Femoral | 31 |  |  | |
| Hodel, 2022, CH [97] | The relationship between pelvic tilt, frontal, and axial leg alignment in healthy subjects | Foot/ankle; Knee; Pelvic | 30 |  |  | |
| Hodel, 2023, CH [98] | The relationship between frontal, axial leg alignment, and ankle joint line orientation-a radiographic analysis of healthy subjects | Femoral; Foot/ankle; Knee; Pelvic; Tibial | 30 |  |  |  |
| Huang, 2020, CN [99] | Reliability and concurrent validity of angle measurements in lower limb: EOS 3D goniometer versus 2D manual goniometer | Femoral; Knee; Pelvic; Tibial | 50 |  |  | |
| Pillet, 2014, FR [100] | A reference method for the evaluation of femoral head joint center location technique based on external markers | Pelvic | 17 |  |  | |
| Than, 2012, HU [101] | Geometrical values of the normal and arthritic hip and knee detected with the EOS imaging system | Femoral; Knee; Pelvic; Tibial | 197 | ? |  | |
| Vaynrub, 2021, US [102] | The ankle-pelvic angle (APA) and global lower extremity angle (GLA): summary measurements of pelvic and lower extremity compensation | Foot/ankle; Femoral; Pelvic; Spinal/balance | 518 |  |  | |
| Pelvis and lower extremity analysis—imaging comparison | ||||||
| Ferre, 2014, FR [103] | Evaluation of a method for the assessment of anterior acetabular coverage and hip joint space width | Femoral; Pelvic; Radiation dose/Image quality | 28 |  |  |  |
| Krug, 2014, GE [104] | Comparison of image quality using a X-ray stereotactical whole-body system and a direct flat-panel X-ray device in examinations of the pelvis and knee | Image quality | 114 |  |  | |
| Rosskopf, 2016, CH [105] | Assessment of two-dimensional (2D) and three-dimensional (3D) lower limb measurements in adults: comparison of micro-dose and low-dose biplanar radiographs | Radiation dose/Image quality | 100 |   |  |  |
| Sailhan, 2017, FR [106] | Differences in limb alignment and femoral mechanical-anatomical angles using two dimension versus three dimension radiographic imaging | Femoral; Knee; Tibial | 127 |  |  | |
| Pelvis and lower extremity analysis—spine | ||||||
| Katsumi, 2022, US [107] | The influence of knee osteoarthritis on spinopelvic alignment and global sagittal balance | Femoral; Knee; Pelvic; Spinal/balance; Tibial | 108 |  |  | |
| Kouyoumdjian, 2022, FR [108] | Hip-spine relationship between sagittal balance of the lumbo-pelvi-femoral complex and hip extension capacity: an EOS evaluation in a healthy caucasian population | Pelvic; Spinal/balance | 120 |  |  | |
| Lazennec, 2015, FR [109] | Measuring extension of the lumbar-pelvic-femoral complex with the EOS system | Femoral; Pelvic | 46 |  |  |  |
| Mekhael, 2021, LB [110] | Toward understanding the underlying mechanisms of pelvic tilt reserve in adult spinal deformity: the role of the 3D hip orientation | Pelvic | 227 |  |  | |
| Park, 2022, KR [111] | Knee extension is related to the posteriorly deviated gravity line to the pelvis in young adults: radiographic analysis using low-dose biplanar X-ray | Knee; Pelvic; Spinal/balance | 124 |  |  | |
| Shimizu, 2021, US [112] | Understanding sagittal compensation in adult spinal deformity patients: relationship between pelvic tilt and lower-extremity position | Femoral; Pelvic; Spinal/balance; Tibial | 200 |  |  | |
| Pelvis and lower extremity analysis—gait | ||||||
| Assi, 2023, LB [113] | ASD with high pelvic retroversion develop changes in their acetabular orientation during walking | Pelvic; Spinal/balance | 126 |  |  | |
| Bakouny, 2017, LB [114] | Roussouly’s sagittal spino-pelvic morphotypes as determinants of gait in asymptomatic adult subjects | Foot/ankle; Gait; Knee; Pelvic; Spinal/balance | 91 |  |  | |
| De Pieri, 2021, CH [115] | Subject-specific modeling of femoral torsion influences the prediction of hip loading during gait in asymptomatic adults | Pelvic | 37 |  |  | |
| Fu, 2023, CN [116] | Relationship between spinal imbalance and knee osteoarthritis by using full-body EOS | Knee; Pelvic; Spinal/balance | 213 |  |  | |
| Huang, 2023, CN [117] | The association between tibial torsion, knee flexion excursion and foot progression during gait in people with knee osteoarthritis: a cross-sectional study | Femoral; Knee; Tibial | 47 |  |  | |
| Ould-Slimane, 2021, FR [118] | Optoelectronic study of gait kinematics in sagittal spinopelvic imbalance | Gait | 35 |  |  | |
| Sangeux, 2014, AU [119] | Which method of hip joint centre localisation should be used in gait analysis? | Femoral | 17 |  |  | |
| Sauret, 2016, FR [120] | On the use of knee functional calibration to determine the medio-lateral axis of the femur in gait analysis: comparison with EOS biplanar radiographs as reference | Femoral; Foot/ankle; Knee; Tibial | 13 |  |  | |
| Südhoff, 2007, FR [121] | Comparing three attachment systems used to determine knee kinematics during gait | Knee | 18 |  |  | |
| van Drongelen, 2020, GE [122] | Determination of leg alignment in hip osteoarthritis patients with the EOS® system and the effect on external joint moments during gait | Femoral; Knee; Pelvic; Tibial | 36 |  |  | |
| Yared, 2023, LB [123] | Differences in kinematic changes from self-selected to fast speed gait in asymptomatic adults with radiological signs of femoro-acetabular impingement | Femoral; Pelvic | 130 |  |  | |
| Rib cage geometry and thoracic analysis | ||||||
| Attali, 2019, FR [124] | Compensation of respiratory-related postural perturbation is achieved by maintenance of head-to-pelvis alignment in healthy humans | Spinal/balance; Ribcage/lung | 48 |  |  | |
| Bertrand, 2008, FR [125] | Three-dimensional reconstruction of the rib cage from biplanar radiography | Ribcage/lung | 15 |  |  | |
| Bousigues, 2023, FR [126] | 3D reconstruction of the scapula from biplanar X-rays for pose estimation and morphological analysis | Shoulder | 18 |  |  |  |
| Vergari, 2022, FR [127] | Functional analysis of the human rib cage over the vital capacity range in standing position using biplanar X-ray imaging | Pelvic; Ribcage/lung; Spinal/balance | 58 |  |  | |
| Special topics in imaging | ||||||
| Herrou, 2022, FR [128] | Prevalence of enthesopathies in adults with x-linked hypophosphatemia: analysis of risk factors | Foot/ankle parameters; Pelvic parameters; Spinal parameters/balance | 114 |  |  | |
| Spinal and pelvis analysis | ||||||
| Fader, 2018, US [129] | The role of lumbar lordosis and pelvic sagittal balance in femoroacetabular impingement | Pelvic; Spinal/balance | 20 |  |  | |
| Ferenczi, 2020, FR [130] | Relationship between spinal-pelvic sagittal balance and pelvic-femoral injuries in professional soccer players | Leg length; Pelvic; Spinal/balance | 61 |  |  | |
| Hey, 2021, SG [131] | Pelvic and sacral morphology and their correlation with pelvic incidence, lumbar lordosis, and lumbar alignment changes between standing and sitting postures | Pelvic; Spinal/balance | 110 |  |  | |
| Spinal and posture analysis | ||||||
| Amabile, 2018, FR [132] | Invariance of head-pelvis alignment and compensatory mechanisms for asymptomatic adults older than 49 years | Pelvic; Spinal/balance | 110 |  |  | |
| Okamoto, 2018, JP [133] | Sagittal balance measures are more reproducible when measured in 3D vs in 2D using full-body EOS® images | Pelvic; Spinal/balance | 60 |  |  | |
| Park, 2023, US [134] | The posterior cranial vertical line: a novel radiographic marker for classifying global sagittal alignment | Knee; Pelvic; Health outcomes; Spinal/balance | 334 |  |  | |
| Upper extremity analysis | ||||||
| Cauchon, 2020, CA [135] | Morphologic and radiologic parameters correlating to shoulder function at diagnosis for patients with rotator cuff tear | Shoulder | 52 |  |  |  |
| Kaneko, 2016, JP [136] | Validation study of arm positions for evaluation of global spinal balance in EOS imaging | Spinal/balance | 34 |  |  | |
| Lagacé, 2012, CA [44] | Analysis of humeral head displacements from sequences of biplanar X-rays: repeatability study and preliminary results in healthy subjects | Shoulder | 9 |  |  | |
| Borotikar, 2019, FR [137] | Effects of gleno-humeral joint centre mislocation on gleno-humeral kinematics and kinetics | Shoulder | 11 |  |  | |
| Loisel, 2023, FR [138] | Three-dimensional reconstruction of the hand from biplanar X-rays: assessment of accuracy and reliability | Image quality | 6 |  |  |  |
| Ohl, 2010, FR [41] | Shoulder bony landmarks location using the EOS low-dose stereoradiography system: a reproducibility study | Shoulder | 22 |  |  | |
| Zhang, 2015, CA [42] | Investigation of 3D glenohumeral displacements from 3D reconstruction using biplane X-ray images: accuracy and reproducibility of the technique and preliminary analysis in rotator cuff tear patients | Shoulder | 45 |  |  | |
| Retrospective study: |  | |||||
| Prospective study. |  | |||||
| Cross-sectional, case-series, case-reports: |  | |||||
| Case–control, cohort, non-randomized controlled trials: |  | |||||
| Reliability/accuracy/agreement: |  | |||||
Appendix C. Adult Surgery Imaging Using the EOS System
| Author, Year, Country | Title | Clinical Endpoints (Parameters) | Total n | Timeline | Study Type | |
| Femoral shaft fractures | ||||||
| Knafo, 2016, FR [139] | Reproducibility of low-dose stereography measurements of femoral torsion after IM nailing of femoral shaft fractures and in intact femurs | Femoral | 45 |  |  | |
| Hip arthroplasty | ||||||
| Verdier, 2016, FR [140] | EOS-based cup navigation: randomised controlled trial in 78 total hip arthroplasties | Pelvic | 78 |  | RCT | |
| Billaud, 2015, FR [141] | Acetabular component navigation in lateral decubitus based on EOS imaging: a preliminary study of 13 cases | Pelvic | 10 |  |  | |
| Xie, 2023, CN [142] | A comparison of radiographic outcomes after total hip arthroplasty between the direct lateral approach and posterior lateral approach with EOS 2D/3D X-ray imaging system | Femoral; Pelvic | 321 |  |  |  |
| Demzik, 2016, US [143] | Inter-rater and intra-rater repeatability and reliability of EOS 3-dimensional imaging analysis software | Femoral; Pelvic | 25 |  |  | |
| Lazennec, 2012, FR [37] | THA Patients in standing and sitting positions: a prospective evaluation using the low-dose “full-body” EOS® imaging system | Femoral; Pelvic; Radiation dose | 150 |  |  | |
| Windsor, 2022, US [144] | Spinopelvic hypermobility corrects after staged bilateral total hip arthroplasty | Pelvic | 42 |  |  | |
| Hip arthroplasty—acetabular and femoral components | ||||||
| Loppini, 2017, IT [31] | Femur first surgical technique: a smart non-computer-based procedure to achieve the combined anteversion in primary total hip arthroplasty | Pelvic | 40 |  |  | |
| Morvan, 2016, FR [32] | Standing radiological analysis with a low-dose biplanar imaging system (EOS system) of the position of the components in total hip arthroplasty using an anterior approach | Femoral; Pelvic | 102 |  |  | |
| Tiberi, 2015, US [145] | What is the fate of total hip arthroplasty (THA) acetabular component orientation when evaluated in the standing position? | Leg length; Pelvic | 113 |  |  | |
| Hip arthroplasty—imaging comparison | ||||||
| Anderson, 2022, US [146] | Validating the use of 3D biplanar radiography versus CT when measuring femoral anteversion after total hip arthroplasty: a comparative study | Pelvic | 45 |  |  | |
| Auberger, 2021, FR [147] | Pelvic position, lying on a traction table, during THA by direct anterior approach. comparison with the standing position and influence on the acetabular cup anteversion | Pelvic | 58 |  |  | |
| Brenneis, 2021, GE [148] | Accuracy of preoperative templating in total hip arthroplasty with special focus on stem morphology: a randomized comparison between common digital and three-dimensional planning using biplanar radiographs | Pelvic | 51 |  | RCT |  |
| Buller, 2021, US [149] | EOS imaging is accurate and reproducible for preoperative total hip arthroplasty templating | Femoral; Pelvic | 43 |  |  | |
| Esposito, 2020, US [150] | Biplanar low-dose radiography is accurate for measuring combined anteversion after total hip arthroplasty | Femoral; Pelvic | 20 |  |  |  |
| Guenoun, 2014, FR [36] | Reliability of a new method for evaluating femoral stem positioning after total hip arthroplasty based on stereoradiographic 3D reconstruction | Femoral | 30 |  |  |  |
| Harold, 2020, US [151] | Are single plane intraoperative and biplanar postoperative radiographic measurements of acetabular cup position the same? | Pelvic | 48 |  |  |  |
| Lazenne, 2015, FR [152] | Offset and anteversion reconstruction after cemented and uncemented total hip arthroplasty: an evaluation with the low-dose EOS system comparing two- and three-dimensional imaging | Pelvic | 110 |  |  | |
| Lazennec, 2011, FR [153] | Pelvis and total hip arthroplasty acetabular component orientations in sitting and standing positions: measurements reproducibility with EOS imaging system versus conventional radiographies | Pelvic | 50 |  |  | |
| Ma, 2022, CN [154] | Assessing component orientation of total hip arthroplasty using the low-dose bi-planar radiographs | Pelvic | 44 |  |  |  |
| Mainard, 2017, FR [155] | Accuracy and reproducibility of preoperative three-dimensional planning for total hip arthroplasty using biplanar low-dose radiographs: a pilot study | Pelvic | 31 |  |  |  |
| Polkowsk, 2012, US [156] | Does standing affect acetabular component inclination and version after THA? | Pelvic | 46 |   |  | |
| Sun, 2023, US [157] | Validation of a novel method of measuring cup orientation using biplanar simultaneous radiographic images | Pelvic | 40 |  |  | |
| Tokunaga, 2018, JP [158] | Implant orientation measurement after THA using the EOS X-ray image acquisition system | Femoral; Pelvic | 90 |  |  | |
| Hip arthroplasty—pelvic positioning and orientation | ||||||
| Barbier, 2017, FR [159] | Changes In pelvic orientation after total hip arthroplasty: a prospective study with EOS™ | Pelvic | 40 |  |  | |
| Innmann, 2022, CA [160] | The accuracy in determining pelvic tilt from anteroposterior pelvic radiographs in patients awaiting hip arthroplasty | Pelvic | 100 |  |  |  |
| Loppini, 2022, IT [161] | Pelvic tilt and functional acetabular position after total hip arthroplasty: an EOS 2D/3D radiographic study | Pelvic | 45 |  |  | |
| Premkumar, 2021, US [162] | Variability of pelvic axial rotation in patients undergoing total hip arthroplasty | Pelvic | 156 |  |  | |
| Hip arthroplasty—planning | ||||||
| Barbier, 2014, FR [163] | The reliability of the anterior pelvic plane for computer navigated acetabular component placement during total hip arthroplasty: prospective study with the EOS imaging system | Pelvic | 44 |  |  | |
| Ben-Ari, 2023, US [164] | Calibration of magnification in two-dimensional low-dose full-body imaging for preoperative planning of total hip arthroplasty | Pelvic | 137 |  |  | |
| Fischer, 2020, JP [165] | Preoperative factors improving the prediction of the postoperative sagittal orientation of the pelvis in standing position after total hip arthroplasty | Health outcomes; Pelvic | 196 |  |  | |
| Huang, 2020, HK [166] | A novel method for accurate preoperative templating for total hip arthroplasty using a biplanar digital radiographic (EOS) system | Femoral | 41 |  |  | |
| Knafo, 2019, FR [167] | Value of 3D preoperative planning for primary total hip arthroplasty based on biplanar weightbearing radiographs | Femoral; Leg length | 33 |  |  |  |
| Pour, 2023, US [168] | Is it necessary to obtain lateral pelvic radiographs in flexed seated position for preoperative total hip arthroplasty planning? | Pelvic | 93 |  |  | |
| Sutphen, 2020, US [169] | Treatment of recurrent dislocation after total hip arthroplasty using advanced imaging and three-dimensional modeling techniques: a case series | Pelvic | 8 |  |  | |
| Hip arthroplasty—risk factors and safety | ||||||
| Bendaya, 2016, FR [170] | Good vs poor results after total hip arthroplasty: an analysis method using implant and anatomic parameters with the EOS imaging system | Health outcomes; Leg length; Pelvic | 35 |  |  | |
| Esposito, 2018, US [171] | Total hip arthroplasty patients with fixed spinopelvic alignment are at higher risk of hip dislocation | Pelvic; Spinal | 1000 |  |  | |
| Jang, 2022, US [172] | Abnormal spinopelvic mobility as a risk factor for acetabular placement error in total hip arthroplasty using optical computer-assisted surgical navigation system | Femoral; Pelvic | 338 |  |  | |
| Kim, 2022, JP [173] | Low pelvic incidence is a risk factor for intraoperative complications in minimally invasive anterolateral approach for total hip arthroplasty | Femoral, Health outcomes; Pelvic | 310 |  |  | |
| Kouyoumdjian, 2023, FR [174] | Influence of kinematics of the lumbopelvic complex in hip arthroplasty dislocation: from assessment to recommendations | Pelvic; Spinal/balance | 80 |  |  | |
| Lazennec, 2011, FR [175] | The EOS imaging system for understanding a patellofemoral disorder following THR | Femoral; Knee; Pelvic | 1 |  |  | |
| Lazennec, 2017, FR [176] | Acetabular and femoral anteversions in standing position are outside the proposed safe zone after total hip arthroplasty | Pelvic | 66 |  |  | |
| Perronne, 2021, FR [177] | How is quality of life after total hip replacement related to the reconstructed anatomy? A study with low-dose stereoradiography | Femoral; Health outcomes; Pelvic | 123 |   |  |  |
| Reina, 2020, FR [178] | The delta of correction: a novel, more reliable variable than limb-length discrepancy at predicting outcome after total hip arthroplasty | Health outcomes; Leg length | 121 |  |  |  |
| Sarpong, 2024, US [179] | Dislocation following anterior and posterior total hip arthroplasty in the setting of spinal deformity and stiffness: evolving trends using a high-risk protocol at a single tertiary center | Leg length; Pelvic; Spinal/balance | 367 |  |  |  |
| Hip arthroplasty—spine | ||||||
| Bassani, 2022, IT [180] | Simultaneous L5-S1 anterior lumbar interbody fusion and total hip arthroplasty through minimally invasive anterior approaches in hip-spine syndrome | Health outcomes; Pelvic; Spinal/balance; Financials/Workflow | 1 |  |  | |
| Bizdikian, 2023, LB [181] | Role of bilateral staged hip arthroplasty in hip-spine syndrome: a case report | Gait; Health outcomes; Pelvic; Spinal/balance | 1 |  |  | |
| Esposito, 2016, US [182] | Does degenerative lumbar spine disease influence femoroacetabular flexion in patients undergoing total hip arthroplasty? | Femoral; Pelvic; Spinal/balance | 242 |  |  | |
| Haffer, 2022, GE [183] | Acetabular cup position differs in spinopelvic mobility types: a prospective observational study of primary total hip arthroplasty patients | Pelvic; Spinal/balance | 197 |  |  | |
| Haffer, 2022, GE [184] | Total hip replacement influences spinopelvic mobility: a prospective observational study | Pelvic; Spinal/balance | 197 |  |  | |
| Vigdorchik, 2022, US [185] | Does low back pain improve following total hip arthroplasty? | Health outcomes; Pelvic | 500 |  |  | |
| Hip arthroplasty—alignment | ||||||
| Kobayashi, 2020, JP [34] | Association of femoral rotation with whole-body alignment in patients who underwent total hip arthroplasty | Health outcomes; Pelvic; Spinal/balance | 65 |  |  | |
| Haffer, 2021, GE [186] | Does obesity affect acetabular cup position, spinopelvic function and sagittal spinal alignment? A prospective investigation with standing and sitting assessment of primary hip arthroplasty patients | Femoral; Pelvic; Spinal/balance | 190 |   |  | |
| Haffer, 2022, GE [187] | Effect of coronal and sagittal spinal malalignment on spinopelvic mobility in patients undergoing total hip replacement: a prospective observational study | Pelvic; Spinal/balance | 197 |  |  |  |
| Shintaro, 2021, JP [188] | Prediction of pelvic mobility using whole-spinal and pelvic alignment in standing and sitting position in total hip arthroplasty patients | Pelvic; Spinal/balance | 78 |  |  | |
| Hip arthroplasty—leg alignment and length | ||||||
| Clavé, 2015, FR [189] | Comparison of the reliability of leg length and offset data generated by three hip replacement CAOS systems using EOS™ imaging | Leg length | 106 |  |  |  |
| van Drongelen, 2019, GE [190] | Are changes in radiological leg alignment and femoral parameters after total hip replacement responsible for joint loading during gait? | Femoral; Gait; Health Outcomes; Tibial | 37 |  |  | |
| Di Laura, 2021, UK [191] | Reconstruction of acetabular defects greater than Paprosky Type 3b: the importance of functional imaging | Health outcomes; Pelvic; Leg length | 25 |  |  |  |
| Gharanizadeh, 2023, IR [192] | Assessing leg length discrepancy is necessary before arthroplasty in patients with unilateral Crowe Type IV hip dislocation | Femoral; Knee; Leg length; Tibial | 61 |  |  | |
| Waibel, 2021, CH [193] | Symptomatic leg length discrepancy after total hip arthroplasty is associated with new onset of lower back pain | Health outcomes; Leg length | 79 |  |  | |
| Lazennec, 2018, FR [194] | Does patients’ perception of leg length after total hip arthroplasty correlate with anatomical leg length? | Femoral; Foot/ancle; Knee; Leg length; Pelvic | 101 |  |  | |
| Lecoanet, 2018, FR [195] | Leg length discrepancy after total hip arthroplasty: can leg length be satisfactorily controlled via anterior approach without a traction table? Evaluation in 56 patients with EOS 3D | Health outcomes; Leg length | 56 |  |  | |
| van Drongelen, 2022, GE [196] | Influence of implantation of a total hip endoprosthesis on the ipsilateral leg alignment: the effect of sex and dysplasia of the hip | Femoral; Knee; Leg length; Pelvic; Tibial | 27 |  |  | |
| Knee arthroplasty | ||||||
| Chalmers, 2022, US [197] | Characterizing the magnitude of and risk factors for functional limb lengthening in patients undergoing primary total knee arthroplasty | Knee; Leg length | 782 |  |  | |
| Nam, 2015, US [198] | Planned bone resections using an MRI-based custom cutting guide system versus 3-dimensional, weight-bearing images in total knee arthroplasty | Femoral; Knee; Tibial | 53 |  |  | |
| Man, 2024, HK [199] | Accuracy and outcome of a handheld accelerometer-based navigation device compared to conventional alignment method in total knee arthroplasty in a Chinese population | Femoral; Knee; Tibial | 123 |  |  | |
| Hau, 2020, UK [200] | Two-dimensional/three-dimensional EOS™ imaging is reliable and comparable to traditional X-ray imaging assessment of knee osteoarthritis aiding surgical management | Femoral; Foot/ankle; Knee; Pelvic; Tibial | 20 |  |  | |
| Hurry, 2023, CA [29] | A low-dose biplanar X-ray imager has RSA level precision in total knee arthroplasty | Knee | 15 |  |  | |
| Elkins, 2018, US [201] | Lower extremity geometry in morbid obesity-considerations for total knee arthroplasty | Health outcomes; Femoral; Knee; Pelvic; Tibial | 232 |  |  | |
| Bahadır, 2018, US [202] | Guidelines for instrumentation for total knee replacement based on frontal plane radiographs | Femoral; Foot/ancle; Knee; Tibial | 66 |  |  | |
| Finsterwald, 2021, AU [203] | Accuracy of one-dimensional templating on linear EOS radiography allows template-directed instrumentation in total knee arthroplasty | Femoral; Financials/Workflow; Knee; Tibial | 113 |  |  | |
| Ji, 2022, CN [204] | Pre-operative predictive factors of residual varus on the mechanical axis after Oxford unicompartmental knee arthroplasty | Femoral; Health outcomes; Knee; Pelvic; Tibial | 880 |  |  | |
| Vigdorchik, 2020, US [205] | Stiffness after total knee arthroplasty: is it a result of spinal deformity? | Health outcomes; Knee; Pelvic; Spinal/balance | 78 |  |  | |
| Liow, 2016, US [206] | Does 3-dimensional in vivo component rotation affect clinical outcomes in unicompartmental knee arthroplasty? | Femoral; Health outcomes; Knee; Tibial | 58 |  |  | |
| Schlatterer, 2009, MC [207] | Skeletal landmarks for TKR implantations: evaluation of their accuracy using EOS imaging acquisition system | Femoral; Knee | 7 | ? |  | |
| Knee arthroplasty—alignment | ||||||
| Meijer, 2017, NL [208] | Do CAS measurements correlate with EOS 3D alignment measurements in primary TKA? | Femoral; Knee; Tibial | 52 |  |  |  |
| Corbett, 2023, AU [209] | Comparison of CT and EOS in assessing coronal lower limb alignment when planning total knee arthroplasty | Knee; Pelvic; Tibial | 96 |  |  | |
| Nam, 2016, US [210] | The impact of imaging modality on the measurement of coronal plane alignment after total knee arthroplasty | Femoral; Knee; Tibial | 160 |  |  |  |
| Bar Ziv, 2022, IL [211] | Excessive sagittal slope of the tibia component during kinematic alignment-safety and functionality at a minimum 2-year follow-up | Femoral; Health outcomes; Knee; Pelvic; Tibial | 337 |  |  | |
| Bar Ziv, 2022, IL [212] | Minimum 2-year radiographic and clinical outcomes of unrestricted kinematic alignment total knee arthroplasty in patients with excessive varus of the tibia component | Femoral; Health outcomes; Knee; Pelvic; Tibial | 338 |  |  | |
| Kim, 2021, KR [213] | Effects of total knee arthroplasty on coronal and sagittal whole-body alignments: serial assessments using whole-body EOS | Femoral; Pelvic; Spinal/balance; Tibial | 101 |  |  |  |
| Meijer, 2014, NL [214] | Assessment of prosthesis alignment after revision total knee arthroplasty using EOS 2D and 3D imaging: a reliability study | Femoral; Knee: Tibial | 37 |  |  | |
| Tsai, 2016, US [215] | Three-dimensional imaging analysis of unicompartmental knee arthroplasty evaluated in standing position: component alignment and in vivo articular contact | Femoral; Knee; Tibial | 68 |  |  |  |
| Yoo, 2020, KR [216] | Pitfalls in assessing limb alignment affected by rotation and flexion of the knee after total knee arthroplasty: analysis using sagittal and coronal whole-body EOS radiography | Femoral; Knee; Tibial | 115 |  |  | |
| Shoulder arthroplasty | ||||||
| Linderman, 2022, US [217] | Return of scapulohumeral rhythm in patients after reverse shoulder arthroplasty: a midterm stereoradiographic imaging analysis | Shoulder | 10 |  |  | |
| Tibial osteotomy | ||||||
| Yoo, 2023, KR [218] | Changes in parameters after high tibial osteotomy: comparison of EOS system and computed tomographic analysis | Femoral; Knee; Tibial | 30 |  |  |  |
| Oh, 2023, KR [219] | Coronal and sagittal alignment of ankle joint is significantly affected by high tibial osteotomy | Femoral; Foot/angle; Knee; Tibial | 46 |  |  | |
| Retrospective study: |  | |||||
| Prospective study: |  | |||||
| Cross-sectional, case-series, case-reports: |  | |||||
| Case–control, cohort, non-randomized controlled trials: |  | |||||
| Reliability/accuracy/agreement: |  | |||||
| Randomized controlled trial. | RCT | |||||
Appendix D. Pediatric Imaging Using EOS Imaging System
| Author, Year, Country | Title | Clinical Endpoints (Parameters) | Total n | Timeline | Study Type | Pediatric/Adults | ||
| Center of mass analysis—fracture | ||||||||
| Sandoz, 2008, FR [220] | Subject-specific mass and 3D localisation of the mass centre of child body segments using biplanar X-rays | Spinal/balance | 12 |   |  |  |  | |
| Foot and ankle analysis | ||||||||
| Rampal, 2018, FR [221] | Assessing 3D paediatric foot morphology using low-dose biplanar radiography: parameter reproducibility and preliminary values | Foot/ankle | 10 |  |  |  |  | |
| Rungprai, 2014, US [222] | Validation and reproducibility of a biplanar imaging system versus conventional radiography of foot and ankle radiographic parameters | Femoral; Foot/ankle; Leg length; Tibial | 50 |  |  |  |  |  |
| Head and neck analysis—cerebral shunt status | ||||||||
| Ben-Sira, 2018, IL [11] | Use of EOS low-dose biplanar X-ray for shunt series in children with hydrocephalus: a preliminary study | Shunt | 9 |  |  |  | ||
| Monuszko, 2021, US [19] | Image quality of EOS low-dose radiography in comparison with conventional radiography for assessment of ventriculoperitoneal shunt integrity | Image quality/radiation dose; Shunt | 57 |  |  |  |  |  |
| Image quality | ||||||||
| Dubousset, 2005, FR [223] | A new imaging 2D and 3D for musculo-skeletal physiology and pathology with low radiation dose and standing position: the EOS system | Image quality/radiation dose | 45 |  |  |  | ||
| Welborn, 2020, US [224] | Image distortion in biplanar slot scanning: patient-specific factors | Image quality | 43 |  |  |  | ? | |
| Image quality—scoliosis | ||||||||
| Hui, 2016, HK [225] | Radiation dose of digital radiography (DR) versus micro-dose X-ray (EOS) on patients with adolescent idiopathic scoliosis: 2016 SOSORT- IRSSD “John Sevastic Award” winner in imaging research | Image quality/radiation dose | 131 |  |  |  |  | |
| Lower extremity analysis | ||||||||
| Brooks, 2021, US [226] | Reliability of low-dose biplanar radiography in assessing pediatric torsional pathology | Femoral; Tibial | 17 |  |  |  | ||
| Gaumétou, 2014, FR [227] | EOS analysis of lower extremity segmental torsion in children and young adults | Femoral; Tibial | 114 |  |  |  |  | |
| Ghanem, 2023, LB [228] | Towards a better understanding of knee angular deformities: discrepancies between clinical examination and 2D/3D assessments | Knee | 329 |  |  |  |  |  |
| Gheno, 2012, FR [229] | Three-dimensional measurements of the lower extremity in children and adolescents using a low-dose biplanar X-ray device | Femoral; Knee; Tibial | 27 |  |  |  |  | |
| Lerisson, 2018, FR [230] | Assessment of micro-dose biplanar radiography in lower limb measurements in children | Femoral; Leg length; Knee; Tibial; Image quality/radiation dose | 260 |  |  |  |  | |
| Meyrignac, 2014, FR [231] | Low-dose biplanar radiography can be used in children and adolescents to accurately assess femoral and tibial torsion and greatly reduce irradiation | Femoral parameters; Tibial parameters | 30 |  |  |  | ||
| Ries, 2023, US [232] | Interobserver reliability of biplanar radiography is unaffected by clinical factors relevant to individuals at risk of pathological lower limb torsion | Femoral; Tibial | 44 |  |  |  |  |  |
| Rosskopf, 2013, CH [233] | Femoral and tibial torsion measurement in children and adolescents: comparison of 3D models based on low-dose biplanar radiography and low-dose CT | Femoral; Tibial | 50 |  |  |  |  | |
| Rosskopf, 2017, CH [234] | Femoral and tibial torsion measurements in children and adolescents: comparison of MRI and 3D models based on low-dose biplanar radiographs | Femoral; Tibial | 60 |  |  |  |  | |
| Schlégl, 2022, HU [235] | Neck-shaft angle measurement in children: accuracy of the conventional radiography-based (2D) methods compared to 3D reconstructions | Femoral | 156 |  |  |  |  | |
| Westberry, 2019, US [236] | 3D modeling of lower extremities with biplanar radiographs: reliability of measures on subsequent examinations | Femoral; Knee; Leg length; Pelvic; Tibial | 53 |  |  |  |  | |
| Lower extremity analysis—bone lesions | ||||||||
| Yucekul, 2022, TR [237] | Prevalence of benign bone lesions of the lower extremity in the pediatric spinal disorders: a whole-body imaging study | Tumor | 1378 |  |  |  |  | |
| Lower extremity analysis—cerebral palsy | ||||||||
| Assi, 2007, FR [238] | Specific 3D reconstruction for children lower limbs using a low dose biplanar X-ray system. reproducibility of clinical parameters for cerebral palsy patients | Femoral; Knee; Pelvic; Tibial | 12 | ? |  |  |  |  |
| Assi, 2013, FR [239] | Three-dimensional reconstructions for asymptomatic and cerebral palsy children’s lower limbs using a biplanar X-ray system: a feasibility study | Femoral; Leg Length; Tibial | 10 |  |  |  | ||
| Lower extremity analysis—x-linked hypophosphatemia | ||||||||
| Bonnet-Lebrun, 2020, FR [240] | Quantitative analysis of lower limbs and pelvis deformities in children with x-linked hypophosphatemic rickets | Femoral; Pelvic; Tibial | 75 |  |  |  | ||
| Lower extremity analysis—scoliosis | ||||||||
| Burkus, 2019, HU [241] | Analysis of proximal femoral parameters in adolescent idiopathic scoliosis | Femoral; Spinal/balance | 670 |  |  |  |  | |
| Karam, 2020, LB [242] | Alterations of 3D acetabular and lower limb parameters in adolescent idiopathic scoliosis | Femoral; Knee; Leg length; Pelvic; Spinal/balance; Tibial | 360 |  |  |  | ||
| Márkus, 2018, HU [243] | The effect of coronal decompensation on the biomechanical parameters in lower limbs in adolescent idiopathic scoliosis | Femoral; Knee; Leg length; Pelvic; Spinal/balance; Tibial | 336 |  |  |  |  | |
| Lower extremity analysis—patellar dislocation | ||||||||
| Miao, 2023, CN [244] | Analysis of lower extremity alignment (LEA) in children with recurrent patellar dislocation by EOS system | Femoral; Knee; Tibial | 50 |  |  |  | ||
| Lower extremity analysis—clubfoot | ||||||||
| Rampal, 2020, FR [245] | Combined 3D analysis of lower-limb morphology and function in children with idiopathic equinovarus clubfoot: a preliminary study | Femoral; Foot/ankle; Gait; Pelvic; Tibial | 10 |  |  |  | ||
| Lower extremity analysis—gait | ||||||||
| Westberry, 2018, US [246] | Femoral anteversion assessment: comparison of physical examination, gait analysis, and EOS biplanar radiography | Femoral; Gait | 110 |  |  |  |  | |
| Lower extremity analysis—gait—cerebral palsy | ||||||||
| Assi, 2016, LB [247] | Validation of hip joint center localization methods during gait analysis using 3D EOS imaging in typically developing and cerebral palsy children | Pelvic | 28 |  |  |  | ||
| Bailly, 2021, FR [248] | 3-D lower extremity bone morphology in ambulant children with cerebral palsy and its relation to gait | Femoral; Gait; Knee; Leg length; Tibial | 523 |  |  |  | ||
| Bailly, 2022, FR [249] | Relationship between 3D lower limb bone morphology and 3D gait variables in children with uni and bilateral cerebral palsy | Femoral; Foot/ankle; Gait; Knee; Pelvic; Tibial | 121 |  |  |  | ||
| Lower extremity analysis—gait—x-linked hypophosphatemia | ||||||||
| Bonnet-Lebrun, 2023, FR [250] | Combined gait analysis and radiologic examination in children with x-linked hypophosphatemia | Gait; Femoral, Foot/ankle; Knee; Pelvic | 55 |   |  |  | ||
| Lower extremity analysis—leg length | ||||||||
| Chen, 2023, US [251] | Normative femoral and tibial lengths in a modern population of twenty-first-century U.S. children | Femoral; Leg length; Tibial | 700 |  |  |  | ||
| Jensen, 2017, DK [5] | Microdose acquisition in adolescent leg length discrepancy using a low-dose biplane imaging system | Femoral; Leg length; Tibial | 22 |  |  |  |  | |
| Rampal, 2018, FR [252] | Lower-limb lengths and angles in children older than six years: reliability and reference values by EOS(®) stereoradiography | Femoral; Tibial | ? |  |  |  |  | |
| Lower extremity analysis—leg length—scoliosis | ||||||||
| Sekiya, 2018, JP [253] | Evaluation of functional and structural leg length discrepancy in patients with adolescent idiopathic scoliosis using the EOS imaging system: a prospective comparative study | Leg length; Pelvic; Spinal/balance | 82 |  |  |  |  | |
| Pelvis and lower extremity analysis | ||||||||
| Khalifé, 2023, FR [254] | Femoral neck version in the spinopelvic and lower limb 3D alignment: a full-body EOS® study in 400 healthy subjects | Femoral; Foot/ankle; Knee; Pelvic; Spinal/balance | 400 |  |  |  |  | |
| Loppini, 2017, IT [255] | Analysis of the pelvic functional orientation in the sagittal plane: a radiographic study with EOS 2D/3D technology | Pelvic | 109 |  |  |  |  |  |
| Passmore, 2018, AU [256] | Defining the medial-lateral axis of the femur: medical imaging, conventional and functional calibration methods lead to differences in hip rotation kinematics for children with torsional deformities | Femoral; Gait; Knee | 20 |  |  |  | ||
| Prum, 2022, FR [257] | Can early golfing lead to acetabular and lower limb changes? A cross-sectional study | Femoral; Pelvic; Tibial; Pelvic | 35 |   |  |  |  | |
| Pytiak, 2016, US [258] | Analysis of spinal alignment and pelvic parameters on upright radiographs: implications for acetabular development | Pelvic; Spinal/balance | 99 |  |  |  |  | |
| Rampal, 2013, FR [259] | Three-dimensional morphologic study of the child’s hip: which parameters are reproducible? | Pelvic | 33 |  |  |  |  | |
| Schlégl, 2015, HU [260] | Three dimensional radiological imaging of normal lower-limb alignment in children | Femoral; Knee; Tibial | 523 |  |  |  |  | |
| Szuper, 2015, HU [261] | Three-dimensional quantitative analysis of the proximal femur and the pelvis in children and adolescents using an upright biplanar slot-scanning X-ray system | Femoral; Pelvic | 508 |  |  |  |  | |
| Pelvis and lower extremity analysis—cerebral palsy | ||||||||
| Massaad, 2016, LB [262] | Three-dimensional evaluation of skeletal deformities of the pelvis and lower limbs in ambulant children with cerebral palsy | Femoral; Pelvic; Tibial | 49 |  |  |  | ||
| Neirynck, 2019, BE [263] | The migration percentage measured on EOS® standing full-leg radiographs: equivalent and advantageous in ambulant children with cerebral palsy | Pelvic | 21 |  |  |  |  | |
| Thépaut, 2016, FR [264] | Measuring physiological and pathological femoral anteversion using a biplanar low-dose X-ray system: validity, reliability, and discriminative ability in cerebral palsy | Pelvic parameters | 38 |  |  |  | ||
| Pelvis and lower extremity analysis—dysplasia | ||||||||
| Powell, 2020, US [265] | Can EOS imaging substitute for conventional radiography in measurement of acetabular morphology in the young dysplastic hip? | Pelvic | 21 |  |  |  |  | |
| Pelvis and lower extremity analysis—leg length | ||||||||
| Park, 2022, KR [266] | The comparison of lower extremity length and angle between computed radiography-based teleoroentgenogram and EOS ® imaging system | Femoral; Knee; Leg length; Tibial | 101 |   |  |  |  |  |
| Pelvis and lower extremity analysis—impingement | ||||||||
| Schmitz, 2013, US [267] | Spectrum of radiographic femoroacetabular impingement morphology in adolescents and young adults: an EOS-based double-cohort study | Pelvic; Spinal/balance | 90 |  |  |  |  |  |
| Maturity | ||||||||
| Hughes, 2020, US [268] | The clavicle continues to grow during adolescence and early adulthood | Maturity | 57 |  |  |  |  |  |
| Nguyen, 2020, US [269] | Hand bone age radiography: comparison between slot-scanning and conventional techniques | Image quality/radiation dose; Maturity | 194 |  |  |  |  | |
| O’Sullivan, 2021, HU [270] | Femoral neck-shaft angle and bone age in 4- to 24-year-olds based on 1005 EOS three-dimensional reconstructions | Femoral; Maturity | 1005 |  |  |  |  | |
| Schlégl, 2017, HU [271] | Determination and correlation of lower limb anatomical parameters and bone age during skeletal growth (based on 1005 cases) | Femoral; Leg length; Maturity; Tibial | 1005 |  |  |  |  |  |
| Schlégl, 2022, HU [272] | Alternative methods for skeletal maturity estimation with the EOS scanner-experience from 934 patients | Maturity | 934 |  |  |  |  |  |
| Xie, 2023, CN [273] | Identification of adolescent menarche status using biplanar X-ray images: a deep learning-based method | Maturity | 259 |  |  |  |  | |
| Machine learning | ||||||||
| Vafadar, 2021, FR [274] | A novel dataset and deep learning-based approach for marker-less motion capture during gait | Gait | 31 |  |  |  |  | |
| Machine learning—leg length | ||||||||
| Tsai, 2021, US [275] | Anatomical landmark localization via convolutional neural networks for limb-length discrepancy measurements | Femoral; Leg length; Tibial | 359 |  |  |  |  | |
| Rib cage geometry and thoracic analysis | ||||||||
| Aubert, 2016, FR [276] | 3D reconstruction of rib cage geometry from biplanar radiographs using a statistical parametric model approach | Ribcage/lung; Spinal/balance | 79 |  |  |  |  | |
| Khalifé, 2022, FR [277] | The rib cage: a new element in the spinopelvic chain | Pelvic; Ribcage/lung; Spinal/balance; Thoracic | 256 |  |  |  |  | |
| Rib cage geometry and thoracic analysis—scoliosis | ||||||||
| Assi, 2021, LB [278] | A novel classification of 3D rib cage deformity in subjects with adolescent idiopathic scoliosis | Pelvic; Ribcage/lung; Spinal/balance | 271 |   |  |  | ||
| Bouloussa, 2019, FR [279] | Biplanar stereoradiography predicts pulmonary function tests in adolescent idiopathic scoliosis: a cross-sectional study | Spinal/balance; Ribcage/lung | 54 |  |  |  | ||
| Courvoisier, 2013, FR [280] | Evaluation of a three-dimensional reconstruction method of the rib cage of mild scoliotic patients | Spinal parameters/balance; Ribcage/lung parameters | 22 |  |  |  | ||
| Machino, 2020, JP [281] | Accuracy of rib cage parameters from 3-dimensional reconstruction images obtained using simultaneous biplanar radiographic scanning technique in adolescent idiopathic scoliosis: comparison with conventional computed tomography | Ribcage/lung | 28 |  |  |  |  | |
| Vergari, 2020, FR [282] | A novel method of anatomical landmark selection for rib cage 3D reconstruction from biplanar radiography | Ribcage/lung; Spinal/balance | 20 |  |  |  |  | |
| Yaszay, 2016, US [283] | The effects of the three-dimensional deformity of adolescent idiopathic scoliosis on pulmonary function | Spinal/balance; Ribcage/lung | 163 |  |  |  | ||
| Spinal and posture analysis—spine | ||||||||
| Clement, 2020, US [284] | What are normal radiographic spine and shoulder balance parameters among adolescent patients? | Spinal parameters/balance; Shoulder parameters | 117 |  |  |  | ||
| Retrospective study: |  | |||||||
| Prospective study: |  | |||||||
| Cross-sectional, case-series, case-reports: |  | |||||||
| Case–control, cohort, non-randomized controlled trials: |  | |||||||
| Reliability/accuracy/agreement: |  | |||||||
| Adult: |  | |||||||
| Pediatric: |  | |||||||
Appendix E. Pediatric Surgery Imaging Using EOS Imaging System
| Author, Year, Country | Title | Clinical Endpoints (Parameters) | Total n | Timeline | Study Type | Pediatric/Adults | ||
| Lower extremity analysis—fracture | ||||||||
| Boscher, 2022, FR [285] | Femoral shaft fractures treated by antegrade locked intramedullary nailing: EOS stereoradiographic imaging evaluation of rotational malalignment having a functional impact | Femoral; Health outcomes; Pelvic | 30 |  |  |  |  | |
| Orfeuvre, 2021, FR [286] | EOS stereographic assessment of femoral shaft malunion after intramedullary nailing: a prospective series of 48 patients at 9 months’ follow-up | Health outcomes; Femoral; Knee; Tibial | 48 |  |  |  |  | |
| Simon, 2018, FR [287] | Pediatric tibial shaft fractures treated by open reduction and stabilization with monolateral external fixation | Knee; Leg length; Maturity | 45 |  |  |  |  | |
| Lower extremity analysis—imaging comparison | ||||||||
| Chua, 2022, SG [288] | Accuracy of biplanar linear radiography versus conventional radiographs when used for lower limb and implant measurements | Femoral; Knee; Tibial | 43 |  |  |  |  | |
| Lower extremity analysis—leg length | ||||||||
| Lecoanet, 2020, FR [289] | Medium-term evaluation of leg lengthening by ISKD® intramedullary nail in 28 patients: should we still use this lengthening system? | Health outcomes; Leg length | 28 |  |  |  |  | |
| Pelvis and lower extremity analysis—Down’s syndrome | ||||||||
| Bakouny, 2020, LB [290] | Combining acetabular and femoral morphology improves our understanding of the Down syndrome hip | Femoral; Knee; Pelvic; Tibial | 82 |  |  |  |  | |
| Rib cage geometry and thoracic analysis—scoliosis | ||||||||
| Deng, 2022, HK [291] | Statistical changes of lung morphology in patients with adolescent idiopathic scoliosis after spinal fusion surgery: a prospective nonrandomized study based on low-dose biplanar X-ray imaging | Ribcage/lung; Spinal/balance | 25 |  |  |  |  | |
| Machino, 2021, JP [38] | Three-dimensional analysis of preoperative and postoperative rib cage parameters by simultaneous biplanar radiographic scanning technique in adolescent idiopathic scoliosis: minimum 2-year follow-up | Pelvic; Ribcage/lung Spinal/balance | 67 |  |  |  | ||
| Machino, 2021, JP [39] | Three-dimensional reconstruction image by biplanar stereoradiography reflects pulmonary functional states in adolescent idiopathic scoliosis | Health outcomes; Ribcage/lung; Spinal/balance | 67 |  |  |  | ||
| Machino, 2022, JP [40] | Factors affecting postoperative pulmonary function deterioration in adolescent idiopathic scoliosis: a prospective study using 3-dimensional image reconstruction by biplanar stereoradiography | Pelvic; Spinal/balance; Ribcage/lung | 67 |  |  |  | ||
| Pietton, 2022, FR [292] | Estimating pulmonary function after surgery for adolescent idiopathic scoliosis using biplanar radiographs of the chest with 3D reconstruction | Health outcomes; Ribcage/lung; Spinal/balance | 45 |  |  |  | ||
| Sabourin, 2010, FR [293] | Three-dimensional stereoradiographic modeling of rib cage before and after spinal growing rod procedures in early-onset scoliosis | Pelvic; Spinal/balance | 8 |  |  |  |  | |
| Spinal and posture analysis—shoulder | ||||||||
| Ha, 2021, US [294] | Can spinal deformity patients maintain proper arm positions while undergoing full-body X-ray? | Arm positioning | 370 |  |  |  |  | |
| Retrospective study: |  | |||||||
| Prospective study: |  | |||||||
| Cross-sectional, case-series, case-reports: |  | |||||||
| Case–control, cohort, non-randomized controlled trials: |  | |||||||
| Reliability/accuracy/agreement: |  | |||||||
| Adult: |  | |||||||
| Pediatric: |  | |||||||
References
- Illés, T.; Somoskeöy, S. The EOS™ imaging system and its uses in daily orthopaedic practice. Int. Orthop. 2012, 36, 1325–1331. [Google Scholar] [CrossRef] [PubMed]
- Escott, B.G.; Ravi, B.; Weathermon, A.C.; Acharya, J.; Gordon, C.L.; Babyn, P.S.; Kelley, S.P.; Narayanan, U.G. EOS low-dose radiography: A reliable and accurate upright assessment of lower-limb lengths. J. Bone Jt. Surg. Am. 2013, 95, e1831–e1837. [Google Scholar] [CrossRef] [PubMed]
- McKenna, C.; Wade, R.; Faria, R.; Yang, H.; Stirk, L.; Gummerson, N.; Sculpher, M.; Woolacott, N. EOS 2D/3D X-ray imaging system: A systematic review and economic evaluation. Health Technol. Assess. 2012, 16, 1–188. [Google Scholar] [CrossRef]
- Yvert, M.; Diallo, A.; Bessou, P.; Rehel, J.L.; Lhomme, E.; Chateil, J.F. Radiography of scoliosis: Comparative dose levels and image quality between a dynamic flat-panel detector and a slot-scanning device (EOS system). Diagn. Interv. Imaging 2015, 96, 1177–1188. [Google Scholar] [CrossRef]
- Jensen, J.; Mussmann, B.R.; Hjarbæk, J.; Al-Aubaidi, Z.; Pedersen, N.W.; Gerke, O.; Torfing, T. Microdose acquisition in adolescent leg length discrepancy using a low-dose biplane imaging system. Acta Radiol. 2017, 58, 1108–1114. [Google Scholar] [CrossRef] [PubMed]
- Girdler, S.; Cho, B.; Mikhail, C.M.; Cheung, Z.B.; Maza, N.; Cho, S.K.-W. Emerging Techniques in Diagnostic Imaging for Idiopathic Scoliosis in Children and Adolescents: A Review of the Literature. World Neurosurg. 2020, 136, 128–135. [Google Scholar] [CrossRef]
- Garg, B.; Mehta, N.; Bansal, T.; Malhotra, R. EOS® imaging: Concept and current applications in spinal disorders. J. Clin. Orthop. Trauma. 2020, 11, 786–793. [Google Scholar] [CrossRef]
- Wybier, M.; Bossard, P. Musculoskeletal imaging in progress: The EOS imaging system. Jt. Bone Spine 2013, 80, 238–243. [Google Scholar] [CrossRef] [PubMed]
- Delsole, E.M.; Mercuri, J.J. Utility of Upright Weight-bearing Imaging in Total Hip Arthroplasty. Semin. Musculoskelet. Radiol. 2019, 23, 603–608. [Google Scholar] [CrossRef]
- Hey, H.W.D.; Chan, C.X.; Wong, Y.M.; Sng, J.W.; Ong, H.Y.; Tan, C.S.; Liu, G.K.; Wong, H.K.; Quek, S.T. The Effectiveness of Full-body EOS Compared With Conventional Chest X-ray in Preoperative Evaluation of the Chest for Patients Undergoing Spine Operations: A Preliminary Study. Spine (Phila Pa 1976) 2018, 43, 1502–1511. [Google Scholar] [CrossRef]
- Ben-Sira, L.; Shiran, S.I.; Pratt, L.-T.; Precel, R.; Ovadia, D.; Constantini, S.; Roth, J. Use of EOS Low-Dose Biplanar X-Ray for Shunt Series in Children with Hydrocephalus: A Preliminary Study. World Neurosurg. 2018, 116, e273–e277. [Google Scholar] [CrossRef] [PubMed]
- Peters, M.D.J.; Godfrey, C.; McInerney, P.; Khalil, H.; Larsen, P.; Marnie, C.; Pollock, D.; Tricco, A.C.; Munn, Z. Best practice guidance and reporting items for the development of scoping review protocols. JBI Evid. Synth. 2022, 20, 953–968. [Google Scholar] [CrossRef] [PubMed]
- Aromataris, E.M. JBI Manual for Evidence Synthesis 2020. 2022. Available online: https://synthesismanual.jbi.global (accessed on 19 March 2025).
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Brage, K.; Mussmann, B.; Geijer, M.; Larsen, P.; Jensen, J. Clinical application of EOS imaging system: A scoping review protocol. JBI Evid. Synth. 2023, 21, 1009–1015. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Boutry, N.; Dutouquet, B.; Leleu, X.; Vieillard, M.H.; Duhamel, A.; Cotten, A. Low-dose biplanar skeletal survey versus digital skeletal survey in multiple myeloma. Eur. Radiol. 2013, 23, 2236–2245. [Google Scholar] [CrossRef]
- EOS Imaging, EOSedge. Available online: https://www.eos-imaging.com/our-expertise/imaging-solutions/eosedge (accessed on 19 March 2025).
- Monuszko, K.; Malinzak, M.; Yang, L.Z.; Niedzwiecki, D.; Fuchs, H.; Muh, C.R.; Gingrich, K.; Lark, R.; Thompson, E.M. Image quality of EOS low-dose radiography in comparison with conventional radiography for assessment of ventriculoperitoneal shunt integrity. J. Neurosurg. Pediatr. 2021, 27, 375–381. [Google Scholar] [CrossRef]
- Wade, R.; Yang, H.; McKenna, C.; Faria, R.; Gummerson, N.; Woolacott, N. A systematic review of the clinical effectiveness of EOS 2D/3D X-ray imaging system. Eur. Spine J. 2013, 22, 296–304. [Google Scholar] [CrossRef]
- Hamzian, N.; Roozmand, Z.; Abrisham, S.M.J.; Abdollahi-Dehkordi, S.; Afereydoon, S.; Ghorbani, M.; Deevband, M.R. Monte Carlo evaluation of effective dose and risk of exposure induced cancer death (REID) for common examinations in stereo radiography (EOS) imaging: Considering age and gender. J. Med. Imaging Radiat. Sci. 2022, 53, 283–290. [Google Scholar] [CrossRef]
- Hamzian, N.; Afereydoon, S.; Ghorbani, M.; Abrisham, S.M.J.; Roozmand, Z.; Abdollahi-Dehkordi, S.; Javan, M.S.; Deevband, M.R. Equivalent Dose and Risk of Exposure Induced Cancer Death of Different Organs due to Various Image Techniques of EOS Imaging System. J. Biomed. Phys. Eng. 2021, 11, 289–296. [Google Scholar] [CrossRef]
- Pacult, M.A.; Walker, C.T.; Godzik, J.; Turner, J.D.; Uribe, J.S. Emerging Technologies in Spinal Surgery: Ultra-Low Radiation Imaging Platforms. Oper. Neurosurg. 2021, 21 (Suppl. S1), S39–S45. [Google Scholar] [CrossRef] [PubMed]
- Chiron, P.; Demoulin, L.; Wytrykowski, K.; Cavaignac, E.; Reina, N.; Murgier, J. Radiation dose and magnification in pelvic X-ray: EOS™ imaging system versus plain radiographs. Orthop. Traumatol. Surg. Res. 2017, 103, 1155–1159. [Google Scholar] [CrossRef] [PubMed]
- Bragdon, C.H.W. Radiostereometric analysis (RSA) studies at Massachusetts general hospital. Psychol. Harv. Orthop. J. 2003, 5, 104–107. [Google Scholar]
- Lorenzen, N.D.; Stilling, M.; Jakobsen, S.S.; Gustafson, K.; Søballe, K.; Baad-Hansen, T. Marker-based or model-based RSA for evaluation of hip resurfacing arthroplasty? A clinical validation and 5-year follow-up. Arch. Orthop. Trauma Surg. 2013, 133, 1613–1621. [Google Scholar] [CrossRef] [PubMed]
- Jensen, J.; Tromborg, H.B.; Rasmussen, B.S.B.; Gerke, O.; Torfing, T.; Precht, H.; Graumann, O. The effect of forearm rotation on radiographic measurements of the wrist: An experimental study using radiostereometric analyses on cadavers. Eur. Radiol. Exp. 2021, 5, 15. [Google Scholar] [CrossRef]
- Valstar, E.R.; Gill, R.; Ryd, L.; Flivik, G.; Borlin, N.; Karrholm, J. Guidelines for standardization of radiostereometry (RSA) of implants. Acta Orthop. 2005, 76, 563–572. [Google Scholar] [CrossRef]
- Hurry, J.K.; Spurway, A.J.; Laende, E.K.; Rehan, S.; Wilson, J.L.A.; Dunbar, M.J.; El-Hawary, R. A low-dose biplanar X-ray imager has RSA level precision in total knee arthroplasty. Acta Orthop. 2023, 94, 555–559. [Google Scholar] [CrossRef]
- Hurry, J.K.; Rehan, S.; Spurway, A.J.; Laende, E.K.; Wilson, J.L.A.; Logan, K.J.; Dunbar, M.J.; El-Hawary, R. The reliability of radiostereometric analysis in determining physeal motion in slipped capital femoral epiphysis in standard uniplanar and low-dose EOS biplanar radiography: A phantom model study. J. Pediatr. Orthop. B 2018, 27, 496–502. [Google Scholar] [CrossRef] [PubMed]
- Loppini, M.; Longo, U.G.; Caldarella, E.; Rocca, A.D.; Denaro, V.; Grappiolo, G. Femur first surgical technique: A smart non-computer-based procedure to achieve the combined anteversion in primary total hip arthroplasty. BMC Musculoskelet. Disord. 2017, 18, 331. [Google Scholar] [CrossRef]
- Morvan, A.; Combourieu, B.; Pansard, E.; Marmorat, J.L.; Carlier, R.; Judet, T.; Moreau, S.; Lonjon, G. Standing radiological analysis with a low-dose biplanar imaging system (EOS system) of the position of the components in total hip arthroplasty using an anterior approach. Bone Jt. J. 2016, 98, 326–333. [Google Scholar] [CrossRef]
- Kobayashi, D.; Choe, H.; Kobayashi, N.; Watanabe, S.; Inaba, Y. Effects of changes in whole-body alignment on ipsilateral knee pain after total hip arthroplasty. J. Orthop. Sci. Off. J. Jpn. Orthop. Assoc. 2023, 28, 398–402. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, D.; Choe, H.; Kobayashi, N.; Tezuka, T.; Ike, H.; Inaba, Y. Association of Femoral Rotation With Whole-Body Alignment in Patients Who Underwent Total Hip Arthroplasty. Arthroplast. Today 2020, 6, 532–537. [Google Scholar] [CrossRef] [PubMed]
- Weng, W.; Wu, H.; Wu, M.; Zhu, Y.; Qiu, Y.; Wang, W. The effect of total hip arthroplasty on sagittal spinal-pelvic-leg alignment and low back pain in patients with severe hip osteoarthritis. Eur. Spine J. 2016, 25, 3608–3614. [Google Scholar] [CrossRef] [PubMed]
- Guenoun, B.; El Hajj, F.; Biau, D.; Anract, P.; Courpied, J.P. Reliability of a New Method for Evaluating Femoral Stem Positioning After Total Hip Arthroplasty Based on Stereoradiographic 3D Reconstruction. J. Arthroplast. 2015, 30, 141–144. [Google Scholar] [CrossRef] [PubMed]
- Lazennec, J.Y.; Brusson, A.; Rousseau, M.-A.; Standing, T.H.P.I.; Positions, S. “Full-Body” EOS® Imaging System. Semin. Arthroplast. JSES 2012, 23, 220–225. [Google Scholar] [CrossRef]
- Machino, M.; Kawakami, N.; Ohara, T.; Saito, T.; Tauchi, R.; Imagama, S. Three-Dimensional Analysis of Preoperative and Postoperative Rib Cage Parameters by Simultaneous Biplanar Radiographic Scanning Technique in Adolescent Idiopathic Scoliosis: Minimum 2-Year Follow-Up. Spine (Phila Pa 1976) 2021, 46, E105–E113. [Google Scholar] [CrossRef]
- Machino, M.; Kawakami, N.; Ohara, T.; Saito, T.; Tauchi, R.; Imagama, S. Three-dimensional reconstruction image by biplanar stereoradiography reflects pulmonary functional states inadolescent idiopathic scoliosis. J. Clin. Neurosci. 2021, 88, 178–184. [Google Scholar] [CrossRef]
- Machino, M.; Kawakami, N.; Ohara, T.; Saito, T.; Tauchi, R.; Imagama, S. Factors affecting postoperative pulmonary function deterioration in adolescent idiopathic scoliosis: A prospective study using 3-dimensional image reconstruction by biplanar stereoradiography. J. Clin. Neurosci. 2022, 98, 182–188. [Google Scholar] [CrossRef] [PubMed]
- Ohl, X.; Stanchina, C.; Billuart, F.; Skalli, W. Shoulder bony landmarks location using the EOS low-dose stereoradiography system: A reproducibility study. Surg. Radiol. Anat. 2010, 32, 153–158. [Google Scholar] [CrossRef]
- Zhang, C.; Skalli, W.; Lagacé, P.-Y.; Billuart, F.; Ohl, X.; Cresson, T.; Bureau, N.J.; Rouleau, D.M.; Roy, A.; Tétreault, P.; et al. Investigation of 3D glenohumeral displacements from 3D reconstruction using biplane X-ray images: Accuracy and reproducibility of the technique and preliminary analysis in rotator cuff tear patients. J. Electromyogr. Kinesiol. 2016, 29, 12–20. [Google Scholar] [CrossRef]
- Lempereur, M.; Leboeuf, F.; Brochard, S.; Rémy-Néris, O. Effects of glenohumeral joint centre mislocation on shoulder kinematics and kinetics. Comput. Methods Biomech. Biomed. Eng. 2014, 17, 130–131. [Google Scholar] [CrossRef] [PubMed]
- Lagacé, P.-Y.; Billuart, F.; Ohl, X.; Skalli, W.; Tétreault, P.; de Guise, J.; Hagemeister, N. Analysis of humeral head displacements from sequences of biplanar X-rays: Repeatability study and preliminary results in healthy subjects. Comput. Methods Biomech. Biomed. Eng. 2012, 15, 221–229. [Google Scholar] [CrossRef] [PubMed]
- Amabile, C.; Nérot, A.; Choisne, J.; Pillet, H.; Lafage, V.; Skalli, W. Alignment of centers of mass of body segments with the gravity line. Comput. Methods Biomech. Biomed. Eng. 2015, 18 (Suppl. S1), 1870–1871. [Google Scholar] [CrossRef] [PubMed]
- Berg, B.I.; Laville, A.; Courvoisier, D.S.; Rouch, P.; Schouman, T. Experiences with a new biplanar low-dose X-ray device for imaging the facial skeleton: A feasibility study. PLoS ONE 2020, 15, e0235032. [Google Scholar] [CrossRef] [PubMed]
- Kerbrat, A.; Rivals, I.; Dupuy, P.; Dot, G.; Berg, B.I.; Attali, V.; Schouman, T. Biplanar Low-Dose Radiograph Is Suitable for Cephalometric Analysis in Patients Requiring 3D Evaluation of the Whole Skeleton. J. Clin. Med. 2021, 10, 5477. [Google Scholar] [CrossRef] [PubMed]
- Buck, F.M.; Guggenberger, R.; Koch, P.P.; Pfirrmann, C.W. Femoral and tibial torsion measurements with 3D models based on low-dose biplanar radiographs in comparison with standard CT measurements. AJR Am. J. Roentgenol. 2012, 199, W607–W612. [Google Scholar] [CrossRef] [PubMed]
- Cebulski-Delebarre, A.; Boutry, N.; Szymanski, C.; Maynou, C.; Lefebvre, G.; Amzallag-Bellenger, E.; Cotten, A. Correlation between primary flat foot and lower extremity rotational misalignment in adults. Diagn. Interv. Imaging 2016, 97, 1151–1157. [Google Scholar] [CrossRef]
- Clément, J.; Hagemeister, N.; Dumas, R.; Kanhonou, M.; de Guise, J.A. Influence of biomechanical multi-joint models used in global optimisation to estimate healthy and osteoarthritis knee kinematics. Comput. Methods Biomech. Biomed. Eng. 2014, 17 (Suppl. S1), 76–77. [Google Scholar] [CrossRef]
- Clément, J.; de Guise, J.A.; Fuentes, A.; Hagemeister, N. Comparison of soft tissue artifact and its effects on knee kinematics between non-obese and obese subjects performing a squatting activity recorded using an exoskeleton. Gait Posture 2018, 61, 197–203. [Google Scholar] [CrossRef]
- Dagneaux, L.; Dufrenot, M.; Bernasconi, A.; Bedard, N.A.; de Cesar Netto, C.; Lintz, F. Three-Dimensional Biometrics to Correlate Hindfoot and Knee Coronal Alignments Using Modern Weightbearing Imaging. Foot Ankle Int. 2020, 41, 1411–1418. [Google Scholar] [CrossRef] [PubMed]
- Dufrénot, M.; Dagneaux, L.; Fernando, C.; Chabrand, P.; Ollivier, M.; Lintz, F. Three-dimensional biometrics using weight-bearing imaging shows relationship between knee and hindfoot axial alignment. Orthop. Traumatol. Surg. Res. 2023, 109, 103482. [Google Scholar] [CrossRef] [PubMed]
- Dumas, R.; Aissaoui, R.; Mitton, D.; Skalli, W.; de Guise, J.A. Determination of personalized inertial parameters of lower limb by biplanar low-dose radiography. Int. Congr. Ser. 2004, 1268, 19–24. [Google Scholar] [CrossRef]
- Dumas, R.; Aissaoui, R.; Mitton, D.; Skalli, W.; de Guise, J.A. Personalized body segment parameters from biplanar low-dose radiography. IEEE Trans. Biomed. Eng. 2005, 52, 1756–1763. [Google Scholar] [CrossRef] [PubMed]
- Guenoun, B.; Zadegan, F.; Aim, F.; Hannouche, D.; Nizard, R. Reliability of a new method for lower-extremity measurements based on stereoradiographic three-dimensional reconstruction. Orthop. Traumatol. Surg. Res. 2012, 98, 506–513. [Google Scholar] [CrossRef] [PubMed]
- Hecker, A.; Lerch, T.D.; Egli, R.J.; Liechti, E.F.; Klenke, F.M. The EOS 3D imaging system reliably measures posterior tibial slope. J. Orthop. Surg. Res. 2021, 16, 388. [Google Scholar] [CrossRef]
- Kümmerlin, J.; Fabro, H.K.; Pedersen, P.H.; Jensen, K.K.; Pedersen, D.; Andersen, M.S. Measuring Knee Joint Laxity in Three Degrees-of-Freedom In Vivo Using a Robotics- and Image-Based Technology. J. Biomech. Eng. 2022, 144, 084502. [Google Scholar] [CrossRef] [PubMed]
- Lo, C.H.; Fang, Y.H.D.; Wang, J.Y.; Yu, T.P.; Chuang, H.C.; Liu, Y.F.; Chang, C.J.; Lin, C.L. Associations between femoral 3D curvature and sagittal imbalance of spine. JOR Spine 2024, 7, e1305. [Google Scholar] [CrossRef]
- Morin, S.N.; Wall, M.; Belzile, E.L.; Godbout, B.; Moser, T.P.; Michou, L.; Ste-Marie, L.-G.; de Guise, J.A.; Rahme, E.; Brown, J.P. Assessment of femur geometrical parameters using EOS™ imaging technology in patients with atypical femur fractures; preliminary results. Bone 2016, 83, 184–189. [Google Scholar] [CrossRef]
- Moon, H.-S.; Choi, C.-H.; Jung, M.; Lee, D.-Y.; Kim, J.-H.; Kim, S.-H. The effect of knee joint rotation in the sagittal and axial plane on the measurement accuracy of coronal alignment of the lower limb. BMC Musculoskelet. Disord. 2020, 21, 470. [Google Scholar] [CrossRef]
- Nam, D.; Shah, R.R.; Nunley, R.M.; Barrack, R.L. Evaluation of the 3-dimensional, weight-bearing orientation of the normal adult knee. J. Arthroplast. 2014, 29, 906–911. [Google Scholar] [CrossRef] [PubMed]
- Serrurier, A.; Quijano, S.; Nizard, R.; Skalli, W. Robust femur condyle disambiguation on biplanar X-rays. Med. Eng. Phys. 2012, 34, 1433–1440. [Google Scholar] [CrossRef] [PubMed]
- Zeighami, A.; Dumas, R.; Bleau, J.; Lavoie, F.; Guise, J.; Aissaoui, R. A method for quantitative evaluation of a valgus knee orthosis using biplane x-ray images. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2020, 2020, 4815–4818. [Google Scholar] [PubMed]
- Cho, B.W.; Lee, T.H.; Kim, S.; Choi, C.H.; Jung, M.; Lee, K.Y.; Kim, S.H. Evaluation of the reliability of lower extremity alignment measurements using EOS imaging system while standing in an even weight-bearing posture. Sci. Rep. 2021, 11, 22039. [Google Scholar] [CrossRef]
- Choi, H.U.; Kim, D.H.; Lee, S.W.; Choi, B.C.; Bae, K.C. Comparison of Lower-Limb Alignment in Patients with Advanced Knee Osteoarthritis: EOS Biplanar Stereoradiography versus Conventional Scanography. Clin. Orthop. Surg. 2022, 14, 370–376. [Google Scholar] [CrossRef] [PubMed]
- Cosentino, A.; Richard, R.; Baron, M.; Demondion, X.; Favre, J.; Omoumi, P. MRI signal and morphological alterations of the suprapatellar fat pad in asymptomatic subjects: Are these normal variants? Skelet. Radiol. 2022, 51, 1995–2007. [Google Scholar] [CrossRef]
- Folinais, D.; Thelen, P.; Delin, C.; Radier, C.; Catonne, Y.; Lazennec, J.Y. Measuring femoral and rotational alignment: EOS system versus computed tomography. Orthop. Traumatol. Surg. Res. 2013, 99, 509–516. [Google Scholar] [CrossRef]
- Mayr, H.O.; Schmidt, J.-P.; Haasters, F.; Bernstein, A.; Schmal, H.; Prall, W.C. Anteversion Angle Measurement in Suspected Torsional Malalignment of the Femur in 3-Dimensional EOS vs Computed Tomography-A Validation Study. J. Arthroplast. 2021, 36, 379–386. [Google Scholar] [CrossRef]
- Narahashi, É.; Guimarães, J.B.; Filho, A.G.O.; Nico, M.A.C.; Silva, F.D. Measurement of tibial slope using biplanar stereoradiography (EOS®). Skelet. Radiol. 2024, 53, 1091–1101. [Google Scholar] [CrossRef]
- Rosskopf, A.B.; Sutter, R.; Pfirrmann, C.W.A.; Buck, F.M. 3D hindfoot alignment measurements based on low-dose biplanar radiographs: A clinical feasibility study. Skelet. Radiol. 2019, 48, 707–712. [Google Scholar] [CrossRef]
- Störmann, S.; Chraga-Urban, A.; Lüring, C.; Bouillon, B.; Gutteck, N.; Arbab, D. Comparison of medial distal tibial angle in EOS imaging and weightbearing X-ray. Foot Ankle Surg. 2021, 27, 855–859. [Google Scholar] [CrossRef]
- Wise, K.L.; Kelly, B.J.; Agel, J.; Marette, S.; Macalena, J.A. Reliability of EOS compared to conventional radiographs for evaluation of lower extremity deformity in adult patients. Skelet. Radiol. 2020, 49, 1423–1430. [Google Scholar] [CrossRef] [PubMed]
- Yan, W.; Xu, X.; Xu, Q.; Yan, W.; Sun, Z.; Jiang, Q.; Shi, D. Femoral and tibial torsion measurements based on EOS imaging compared to 3D CT reconstruction measurements. Ann. Transl. Med. 2019, 7, 460. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Chan, P.K.; Chiu, K.Y.; Yan, C.H.; Yeung, S.S.; Fu, S.N. Exploring the relationship between pain intensity and knee moments in participants with medial knee osteoarthritis: A cross-sectional study. BMC Musculoskelet. Disord. 2021, 22, 685. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Chan, P.K.; Chiu, K.Y.; Yan, C.H.; Yeung, D.S.S.; Lai, C.W.K.; Fu, S.N. Knee joint loadings are related to tibial torsional alignments in people with radiographic medial knee osteoarthritis. PLoS ONE 2021, 16, e0255008. [Google Scholar] [CrossRef] [PubMed]
- Koliogiannis, V.K.A.; Brandlhuber, M.; Messerschmidt, V.; Stahl, R.; Melcher, C.; Schinner, R.; Birkenmaier, C.; Ricke, J.; Baur-Melnyk, A. Is the EOS imaging system as accurate as conventional radiography in grading osteoarthritis of the knee? Eur. Radiol. 2021, 31, 3491–3497. [Google Scholar] [CrossRef]
- Zeighami, A.; Dumas, R.; Kanhonou, M.; Hagemeister, N.; Lavoie, F.; de Guise, J.A.; Aissaoui, R. Tibio-femoral joint contact in healthy and osteoarthritic knees during quasi-static squat: A bi-planar X-ray analysis. J. Biomech. 2017, 53, 178–184. [Google Scholar] [CrossRef]
- Clavé, A.; Maurer, D.G.; Nagra, N.S.; Fazilleau, F.; Lefèvre, C.; Stindel, E. Reproducibility of length measurements of the lower limb by using EOS™. Musculoskelet. Surg. 2018, 102, 165–171. [Google Scholar] [CrossRef] [PubMed]
- Guggenberger, R.; Pfirrmann, C.W.; Koch, P.P.; Buck, F.M. Assessment of lower limb length and alignment by biplanar linear radiography: Comparison with supine CT and upright full-length radiography. AJR Am. J. Roentgenol. 2014, 202, W161–W167. [Google Scholar] [CrossRef]
- Lazennec, J.Y.; Brusson, A.; Rousseau, M.A.; Robbins, C.B.; Pour, A.E. Do Patients’ Perceptions of Leg Length Correlate With Standing 2- and 3-Dimensional Radiographic Imaging? J. Arthroplast. 2016, 31, 2308–2313. [Google Scholar] [CrossRef] [PubMed]
- Abdennebi, A.B.; Aubry, S.; Ounalli, L.; Fayache, M.S.; Delabrousse, E.; Petegnief, Y. Comparative dose levels between CT-scanner and slot-scanning device (EOS system) in pregnant women pelvimetry. Phys. Med. 2017, 33, 77–86. [Google Scholar] [CrossRef]
- Dietrich, T.J.; Pfirrmann, C.W.; Schwab, A.; Pankalla, K.; Buck, F.M. Comparison of radiation dose, workflow, patient comfort and financial break-even of standard digital radiography and a novel biplanar low-dose X-ray system for upright full-length lower limb and whole spine radiography. Skelet. Radiol. 2013, 42, 959–967. [Google Scholar] [CrossRef]
- Wood, L.; Martin, C.; Polly, D.; Luchsinger, S.; Takahashi, T. Incidental extraspinal imaging findings on adult EOS full body radiographs: Prevalence and clinical importance. BMC Med. Imaging 2021, 21, 83. [Google Scholar] [CrossRef]
- Bordes, M.; Thaunat, M.; Maury, É.; Bonin, N.; May, O.; Tardy, N.; Martz, P.; Gedouin, J.-E.; Kouyoumdjian, P.; Krantz, N.; et al. The influence of the sacral slope on pelvic kinematics and clinical manifestations in femoroacetabular impingement. Orthop. Traumatol. Surg. Res. 2023, 109 (Suppl. S8), 103688. [Google Scholar] [CrossRef] [PubMed]
- Buckland, A.; DelSole, E.; George, S.; Vira, S.; Lafage, V.; Errico, T.; Vigdorchik, J. Sagittal Pelvic Orientation A Comparison of Two Methods of Measurement. Bull. Hosp. Jt. Dis. 2017, 75, 234–240. [Google Scholar]
- Fritz, B.; Agten, C.A.; Boldt, F.K.; Zingg, P.O.; Pfirrmann, C.W.A.; Sutter, R. Acetabular coverage differs between standing and supine positions: Model-based assessment of low-dose biplanar radiographs and comparison with CT. Eur. Radiol. 2019, 29, 5691–5699. [Google Scholar] [CrossRef] [PubMed]
- Gasparutto, X.; Besonhe, P.; DiGiovanni, P.L.; Armand, S.; Hannouche, D. Definition and reliability of 3D acetabular and global offset measurements from bi-plane X-rays. Sci. Rep. 2023, 13, 591. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Vergari, C.; Girinon, F.; Lazennec, J.Y.; Skalli, W. Stand-to-Sit Kinematics of the Pelvis Is Not Always as Expected: Hip and Spine Pathologies Can Have an Impact. J. Arthroplast. 2019, 34, 2118–2123. [Google Scholar] [CrossRef] [PubMed]
- Mussmann, B.; Jensen, C.; Bensen, A.S.; Torfing, T.; Ovesen, O.; Overgaard, S. Radiographic signs of acetabular retroversion using a low-dose slot-scanning radiographic system (EOS(®)). Radiography 2019, 25, e53–e57. [Google Scholar] [CrossRef] [PubMed]
- Rouissi, J.; Arvieu, R.; Dubory, A.; Vergari, C.; Bachy, M.; Vialle, R. Intra and inter-observer reliability of determining degree of pelvic obliquity in neuromuscular scoliosis using the EOS-CHAIR® protocol. Childs Nerv. Syst. 2017, 33, 337–341. [Google Scholar] [CrossRef]
- Thelen, T.; Thelen, P.; Demezon, H.; Aunoble, S.; Le Huec, J.C. Normative 3D acetabular orientation measurements by the low-dose EOS imaging system in 102 asymptomatic subjects in standing position: Analyses by side, gender, pelvic incidence and reproducibility. Orthop. Traumatol. Surg. Res. 2017, 103, 209–215. [Google Scholar] [CrossRef]
- Bendaya, S.; Lazennec, J.Y.; Anglin, C.; Allena, R.; Sellam, N.; Thoumie, P.; Skalli, W. Healthy vs. osteoarthritic hips: A comparison of hip, pelvis and femoral parameters and relationships using the EOS® system. Clin. Biomech. 2015, 30, 195–204. [Google Scholar] [CrossRef] [PubMed]
- Canetti, R.; de Saint Vincent, B.; Vieira, T.D.; Fière, V.; Thaunat, M. Spinopelvic parameters in greater trochanteric pain syndrome: A retrospective case-control study. Skelet. Radiol. 2020, 49, 773–778. [Google Scholar] [CrossRef] [PubMed]
- Coulomb, R.; Michaud, J.; Maury, E.; Bonin, N.; Krantz, N.; May, O.; Thaunat, M.; Bordes, M.; Tardy, N.; Martz, P.; et al. Radiological signs of femoroacetabular impingement are linked to pelvic version in asymptomatic subjects. Orthop. Traumatol. Surg. Res. 2023, 109, 103719. [Google Scholar] [CrossRef] [PubMed]
- Frasson, V.B.; Herzog, W.; Johnston, K.; Pauchard, Y.; Vaz, M.A.; Baroni, B.M. Do femoral version abnormalities play a role in hip function of patients with hip pain? Clin. Biomech. 2022, 97, 105708. [Google Scholar] [CrossRef] [PubMed]
- Hodel, S.; Flury, A.; Hoch, A.; Zingg, P.O.; Vlachopoulos, L.; Fucentese, S.F. The relationship between pelvic tilt, frontal, and axial leg alignment in healthy subjects. J. Orthop. Sci. 2022, 28, 1353–1358. [Google Scholar] [CrossRef] [PubMed]
- Hodel, S.; Cavalcanti, N.; Fucentese, S.; Vlachopoulos, L.; Viehöfer, A.; Wirth, S. The Relationship between Frontal, Axial Leg Alignment, and Ankle Joint Line Orientation-a Radiographic Analysis of Healthy Subjects. Orthop. Surg. 2022, 15, 79–84. [Google Scholar] [CrossRef]
- Huang, J.; Tian, F.; Zhang, Z.; Shi, W.; Lin, J.; Chen, L.; Yang, H. Reliability and concurrent validity of angle measurements in lower limb: EOS 3D goniometer versus 2D manual goniometer. J. Orthop. Translat. 2020, 24, 96–102. [Google Scholar] [CrossRef]
- Pillet, H.; Sangeux, M.; Hausselle, J.; El Rachkidi, R.; Skalli, W. A reference method for the evaluation of femoral head joint center location technique based on external markers. Gait Posture 2014, 39, 655–658. [Google Scholar] [CrossRef]
- Than, P.; Szuper, K.; Somoskeöy, S.; Warta, V.; Illés, T. Geometrical values of the normal and arthritic hip and knee detected with the EOS imaging system. Int. Orthop. 2012, 36, 1291–1297. [Google Scholar] [CrossRef]
- Vaynrub, M.; Tishelman, J.; Buckland, A.J.; Errico, T.J.; Protopsaltis, T.S. The Ankle-Pelvic Angle (APA) and Global Lower Extremity Angle (GLA): Summary Measurements of Pelvic and Lower Extremity Compensation. Int. J. Spine Surg. 2021, 15, 130–136. [Google Scholar] [CrossRef]
- Ferre, R.; Gibon, E.; Hamadouche, M.; Feydy, A.; Drapé, J.L. Evaluation of a method for the assessment of anterior acetabular coverage and hip joint space width. Skelet. Radiol. 2014, 43, 599–605. [Google Scholar] [CrossRef]
- Krug, K.B.; Weber, C.; Schwabe, H.; Sinzig, N.M.; Wein, B.; Müller, D.; Wegmann, K.; Peters, S.; Sendler, V.; Ewen, K.; et al. Comparison of image quality using a X-ray stereotactical whole-body system and a direct flat-panel X-ray device in examinations of the pelvis and knee. Rofo 2014, 186, 67–76. [Google Scholar] [CrossRef] [PubMed]
- Rosskopf, A.; Pfirrmann, C.; Buck, F.; Rosskopf, A.B.; Pfirrmann, C.W.A.; Buck, F.M. Assessment of two-dimensional (2D) and three-dimensional (3D) lower limb measurements in adults: Comparison of micro-dose and low-dose biplanar radiographs. Eur. Radiol. 2016, 26, 3054–3062. [Google Scholar] [CrossRef] [PubMed]
- Sailhan, F.; Jacob, L.; Hamadouche, M. Differences in limb alignment and femoral mechanical-anatomical angles using two dimension versus three dimension radiographic imaging. Int. Orthop. 2017, 41, 2009–2016. [Google Scholar] [CrossRef] [PubMed]
- Katsumi, R.; Mannen, E.M.; Bajaj, G.; Smith, J.R.; Mears, S.C.; Stambough, J.B.; Barnes, C.L. The Influence of Knee Osteoarthritis on Spinopelvic Alignment and Global Sagittal Balance. J. Knee Surg. 2022, 36, 917–924. [Google Scholar] [CrossRef] [PubMed]
- Kouyoumdjian, P.; Mansour, J.; Haignère, V.; Demattei, C.; Maury, E.; George, D.; Coulomb, R. Hip-Spine Relationship between Sagittal Balance of the Lumbo-Pelvi-Femoral Complex and Hip Extension Capacity: An EOS Evaluation in a Healthy Caucasian Population. Glob. Spine J. 2022, 14, 265–271. [Google Scholar] [CrossRef] [PubMed]
- Lazennec, J.; Brusson, A.; Folinais, D.; Zhang, A.; Pour, A.; Rousseau, M. Measuring extension of the lumbar-pelvic-femoral complex with the EOS system. Eur. J. Orthop. Surg. Traumatol. 2015, 25, 1061–1068. [Google Scholar] [CrossRef] [PubMed]
- Mekhael, M.; Kawkabani, G.; Saliby, R.M.; Skalli, W.; Saad, E.; Jaber, E.; Rachkidi, R.; Kharrat, K.; Kreichati, G.; Ghanem, I.; et al. Toward understanding the underlying mechanisms of pelvic tilt reserve in adult spinal deformity: The role of the 3D hip orientation. Eur. Spine J. 2021, 30, 2495–2503. [Google Scholar] [CrossRef] [PubMed]
- Park, J.Y.; Cho, B.W.; Kwon, H.M.; Park, K.K.; Lee, W.S. Knee Extension Is Related to the Posteriorly Deviated Gravity Line to the Pelvis in Young Adults: Radiographic Analysis Using Low-Dose Biplanar X-ray. Yonsei Med. J. 2022, 63, 933–940. [Google Scholar] [CrossRef]
- Shimizu, T.; Cerpa, M.; Lenke, L.G. Understanding sagittal compensation in adult spinal deformity patients: Relationship between pelvic tilt and lower-extremity position. J. Neurosurg. Spine 2021, 35, 616–623. [Google Scholar] [CrossRef] [PubMed]
- Assi, A.; Rebeyrat, G.; El Rachkidi, R.; Semaan, K.; Saad, E.; Mekhael, E.; Nassim, N.; Massaad, A.; Lafage, V.; Ghanem, I.; et al. ASD with high pelvic retroversion develop changes in their acetabular orientation during walking. Brain Spine 2023, 3, 101752. [Google Scholar] [CrossRef] [PubMed]
- Bakouny, Z.; Assi, A.; Massaad, A.; Saghbini, E.; Lafage, V.; Skalli, W.; Ghanem, I.; Kreichati, G. Roussouly’s sagittal spino-pelvic morphotypes as determinants of gait in asymptomatic adult subjects. Gait Posture 2017, 54, 27–33. [Google Scholar] [CrossRef]
- De Pieri, E.; Friesenbichler, B.; List, R.; Monn, S.; Casartelli, N.C.; Leunig, M.; Ferguson, S.J. Subject-Specific Modeling of Femoral Torsion Influences the Prediction of Hip Loading During Gait in Asymptomatic Adults. Front. Bioeng. Biotechnol. 2021, 9, 679360. [Google Scholar] [CrossRef] [PubMed]
- Fu, P.; Xu, W.; Xu, P.; Huang, J.; Guo, J.J. Relationship between spinal imbalance and knee osteoarthritis by using full-body EOS. BMC Musculoskelet. Disord. 2023, 24, 402. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Chan, P.K.; Chiu, K.Y.; Yan, C.H.; Yeung, S.S.; Lai, C.W.; Leung, A.K.; Fu, S.N. The association between tibial torsion, knee flexion excursion and foot progression during gait in people with knee osteoarthritis: A cross-sectional study. BMC Sports Sci. Med. Rehabil. 2023, 15, 110. [Google Scholar] [CrossRef]
- Ould-Slimane, M.; Bouyge, B.; Chastan, N.; Ferrand-Devouge, E.; Dujardin, F.; Bertucchi, W.; Michelin, P.; Gillibert, A.; Gauthé, R. Optoelectronic Study of Gait Kinematics in Sagittal Spinopelvic Imbalance. World Neurosurg. 2022, 158, e956–e963. [Google Scholar] [CrossRef]
- Sangeux, M.; Pillet, H.; Skalli, W. Which method of hip joint centre localisation should be used in gait analysis? Gait Posture 2014, 40, 20–25. [Google Scholar] [CrossRef] [PubMed]
- Sauret, C.; Pillet, H.; Skalli, W.; Sangeux, M. On the use of knee functional calibration to determine the medio-lateral axis of the femur in gait analysis: Comparison with EOS biplanar radiographs as reference. Gait Posture 2016, 50, 180–184. [Google Scholar] [CrossRef] [PubMed]
- Südhoff, I.; Van Driessche, S.; Laporte, S.; de Guise, J.A.; Skalli, W. Comparing three attachment systems used to determine knee kinematics during gait. Gait Posture 2007, 25, 533–543. [Google Scholar] [CrossRef]
- van Drongelen, S.; Kaldowski, H.; Fey, B.; Tarhan, T.; Assi, A.; Stief, F.; Meurer, A. Determination of Leg Alignment in Hip Osteoarthritis Patients with the EOS® System and the Effect on External Joint Moments during Gait. Appl. Sci. 2020, 10, 7777. [Google Scholar] [CrossRef]
- Yared, F.; Massaad, A.; Bakouny, Z.; Otayek, J.; Bizdikian, A.J.; Ghanimeh, J.; Labaki, C.; Ghanem, D.; Ghanem, I.; Skalli, W.; et al. Differences in Kinematic Changes From Self-Selected to Fast Speed Gait in Asymptomatic Adults With Radiological Signs of Femoro-Acetabular Impingement. Cureus 2023, 15, e43733. [Google Scholar] [CrossRef] [PubMed]
- Attali, V.; Clavel, L.; Rouch, P.; Rivals, I.; Rémy-Néris, S.; Skalli, W.; Sandoz, B.; Similowski, T. Compensation of Respiratory-Related Postural Perturbation Is Achieved by Maintenance of Head-to-Pelvis Alignment in Healthy Humans. Front. Physiol. 2019, 10, 441. [Google Scholar] [CrossRef]
- Bertrand, S.; Laporte, S.; Parent, S.; Skalli, W.; Mitton, D. Three-dimensional reconstruction of the rib cage from biplanar radiography. IRBM 2008, 29, 278–286. [Google Scholar] [CrossRef]
- Bousigues, S.; Gajny, L.; Abihssira, S.; Heidsieck, C.; Ohl, X.; Hagemeister, N.; Skalli, W. 3D reconstruction of the scapula from biplanar X-rays for pose estimation and morphological analysis. Med. Eng. Phys. 2023, 120, 104043. [Google Scholar] [CrossRef] [PubMed]
- Vergari, C.; Skalli, W.; Clavel, L.; Demuynck, M.; Valentin, R.; Sandoz, B.; Similowski, T.; Attali, V. Functional analysis of the human rib cage over the vital capacity range in standing position using biplanar X-ray imaging. Comput. Biol. Med. 2022, 144, 105343. [Google Scholar] [CrossRef] [PubMed]
- Herrou, J.; Picaud, A.S.; Lassalle, L.; Pacot, L.; Chaussain, C.; Merzoug, V.; Hervé, A.; Gadion, M.; Rothenbuhler, A.; Kamenický, P.; et al. Prevalence of Enthesopathies in Adults With X-linked Hypophosphatemia: Analysis of Risk Factors. J. Clin. Endocrinol. Metab. 2022, 107, e224–e235. [Google Scholar] [CrossRef]
- Fader, R.R.; Tao, M.A.; Gaudiani, M.A.; Turk, R.; Nwachukwu, B.U.; Esposito, C.I.; Ranawat, A.S. The role of lumbar lordosis and pelvic sagittal balance in femoroacetabular impingement. Bone Jt. J. 2018, 100, 1275–1279. [Google Scholar] [CrossRef] [PubMed]
- Ferenczi, A.; Moraux, A.; Gall, F.L.; Thevenon, A.; Wieczorek, V. Relationship Between Spinal-Pelvic Sagittal Balance and Pelvic-Femoral Injuries in Professional Soccer Players. Orthop. J. Sports Med. 2020, 8, 2325967119894962. [Google Scholar] [CrossRef]
- Hey, H.W.D.; Tan, J.H.; Ong, B.; Kumar, A.; Liu, G.; Wong, H.K. Pelvic and sacral morphology and their correlation with pelvic incidence, lumbar lordosis, and lumbar alignment changes between standing and sitting postures. Clin. Neurol. Neurosurg. 2021, 211, 107019. [Google Scholar] [CrossRef]
- Amabile, C.; Le Huec, J.C.; Skalli, W. Invariance of head-pelvis alignment and compensatory mechanisms for asymptomatic adults older than 49 years. Eur. Spine J. 2018, 27, 458–466. [Google Scholar] [CrossRef]
- Okamoto, M.; Jabour, F.; Sakai, K.; Hatsushikano, S.; Le Huec, J.C.; Hasegawa, K. Sagittal balance measures are more reproducible when measured in 3D vs in 2D using full-body EOS® images. Eur. Radiol. 2018, 28, 4570–4577. [Google Scholar] [CrossRef] [PubMed]
- Park, P.J.; Hassan, F.M.; Ferrer, X.E.; Morrissette, C.; Lee, N.J.; Cerpa, M.; Sardar, Z.M.; Kelly, M.P.; Bourret, S.; Hasegawa, K.; et al. The Posterior Cranial Vertical Line: A Novel Radiographic Marker for Classifying Global Sagittal Alignment. Neurospine 2023, 20, 790–797. [Google Scholar] [CrossRef] [PubMed]
- Cauchon, A.M.; Tétreault, P.; Bascans, C.; Skalli, W.; Hagemeister, N. Morphologic and radiologic parameters correlating to shoulder function at diagnosis for patients with rotator cuff tear. J. Shoulder Elb. Surg. 2020, 29, 2272–2281. [Google Scholar] [CrossRef] [PubMed]
- Kaneko, K.; Aota, Y.; Sekiya, T.; Yamada, K.; Saito, T. Validation study of arm positions for evaluation of global spinal balance in EOS imaging. Eur. J. Orthop. Surg. Traumatol. 2016, 26, 725–733. [Google Scholar] [CrossRef]
- Borotikar, B.; Lempereur, M.; Brochard, S.; Rémy-Néris, O.; Leboucher, J.; Leboeuf, F. Effects of gleno-humeral joint centre mislocation on gleno-humeral kinematics and kinetics. Comput. Methods Biomech. Biomed. Eng. 2019, 22, 764–771. [Google Scholar]
- Loisel, F.; Durand, S.; Goubier, J.N.; Bonnet, X.; Rouch, P.; Skalli, W. Three-dimensional reconstruction of the hand from biplanar X-rays: Assessment of accuracy and reliability. Orthop. Traumatol. Surg. Res. 2023, 109, 103403. [Google Scholar] [CrossRef]
- Knafo, J.; Thelen, T.; Verdier, D.; Creppy, L.; Tournier, C.; Fabre, T. Reproducibility of low-dose stereography measurements of femoral torsion after IM nailing of femoral shaft fractures and in intact femurs. Orthop. Traumatol. Surg. Res. 2016, 102, 595–599. [Google Scholar] [CrossRef] [PubMed]
- Verdier, N.; Billaud, A.; Masquefa, T.; Pallaro, J.; Fabre, T.; Tournier, C. EOS-based cup navigation: Randomised controlled trial in 78 total hip arthroplasties. Orthop. Traumatol. Surg. Res. 2016, 102, 417–421. [Google Scholar] [CrossRef]
- Billaud, A.; Verdier, N.; de Bartolo, R.; Lavoinne, N.; Chauveaux, D.; Fabre, T. Acetabular component navigation in lateral decubitus based on EOS imaging: A preliminary study of 13 cases. Orthop. Traumatol. Surg. Res. 2015, 101, 271–275. [Google Scholar] [CrossRef]
- Xie, R.; Huang, J.; Wu, Q.; Qian, Y.F.; Jiang, D.; Li, L.; Huang, L. A Comparison of Radiographic Outcomes after Total Hip Arthroplasty between the Direct Lateral Approach and Posterior Lateral Approach with EOS 2D/3D X-Ray Imaging System. Orthop. Surg. 2023, 15, 1312–1324. [Google Scholar] [CrossRef]
- Demzik, A.L.; Alvi, H.M.; Delagrammaticas, D.E.; Martell, J.M.; Beal, M.D.; Manning, D.W. Inter-Rater and Intra-Rater Repeatability and Reliability of EOS 3-Dimensional Imaging Analysis Software. J. Arthroplast. 2016, 31, 1091–1095. [Google Scholar] [CrossRef]
- Windsor, E.N.; Sculco, P.K.; Mayman, D.J.; Vigdorchik, J.M.; Jerabek, S.A. Spinopelvic Hypermobility Corrects After Staged Bilateral Total Hip Arthroplasty. Hss J. 2022, 18, 541–549. [Google Scholar] [CrossRef] [PubMed]
- Tiberi, J.V., III; Antoci, V.; Malchau, H.; Rubash, H.E.; Freiberg, A.A.; Kwon, Y.M. What is the Fate of Total Hip Arthroplasty (THA) Acetabular Component Orientation When Evaluated in the Standing Position? J. Arthroplast. 2015, 30, 1555–1560. [Google Scholar] [CrossRef] [PubMed]
- Anderson, C.G.; Brilliant, Z.R.; Jang, S.J.; Sokrab, R.; Mayman, D.J.; Vigdorchik, J.M.; Sculco, P.K.; Jerabek, S.A. Validating the use of 3D biplanar radiography versus CT when measuring femoral anteversion after total hip arthroplasty: A comparative study. Bone Jt. J. 2022, 104, 1196–1201. [Google Scholar] [CrossRef]
- Auberger, G.; Pansard, E.; Bouche, P.A.; Marmorat, J.L.; Judet, T.; Lonjon, G. Pelvic position, lying on a traction table, during THA by direct anterior approach. Comparison with the standing position and influence on the acetabular cup anteversion. Orthop. Traumatol. Surg. Res. 2021, 107, 103077. [Google Scholar] [CrossRef]
- Brenneis, M.; Braun, S.; van Drongelen, S.; Fey, B.; Tarhan, T.; Stief, F.; Meurer, A. Accuracy of Preoperative Templating in Total Hip Arthroplasty With Special Focus on Stem Morphology: A Randomized Comparison Between Common Digital and Three-Dimensional Planning Using Biplanar Radiographs. J. Arthroplast. 2021, 36, 1149–1155. [Google Scholar] [CrossRef] [PubMed]
- Buller, L.T.; McLawhorn, A.S.; Maratt, J.D.; Carroll, K.M.; Mayman, D.J. EOS Imaging is Accurate and Reproducible for Preoperative Total Hip Arthroplasty Templating. J. Arthroplast. 2021, 36, 1143–1148. [Google Scholar] [CrossRef]
- Esposito, C.I.; Miller, T.T.; Lipman, J.D.; Carroll, K.M.; Padgett, D.E.; Mayman, D.J.; Jerabek, S.A. Biplanar Low-Dose Radiography Is Accurate for Measuring Combined Anteversion After Total Hip Arthroplasty. Hss J. 2020, 16, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Harold, R.E.; Delagrammaticas, D.; Keller, T.; Butler, B.; Stover, M.D.; Manning, D.W. Are single plane intraoperative and biplanar postoperative radiographic measurements of acetabular cup position the same? Hip Int. 2020, 30, 530–535. [Google Scholar] [CrossRef] [PubMed]
- Lazennec, J.; Brusson, A.; Dominique, F.; Rousseau, M.-A.; Pour, A. Offset and anteversion reconstruction after cemented and uncemented total hip arthroplasty: An evaluation with the low-dose EOS system comparing two- and three-dimensional imaging. Int. Orthop. 2015, 39, 1259–1267. [Google Scholar] [CrossRef]
- Lazennec, J.Y.; Rousseau, M.A.; Rangel, A.; Gorin, M.; Belicourt, C.; Brusson, A.; Catonné, Y. Pelvis and total hip arthroplasty acetabular component orientations in sitting and standing positions: Measurements reproductibility with EOS imaging system versus conventional radiographies. Orthop. Traumatol. Surg. Res. 2011, 97, 373–380. [Google Scholar] [CrossRef]
- Ma, Z.; Tang, H.; Zhou, Y.; Wang, S.; Yang, D.; Guo, S. Assessing component orientation of total hip arthroplasty using the low-dose bi-planar radiographs. BMC Musculoskelet. Disord. 2022, 23, 886. [Google Scholar] [CrossRef] [PubMed]
- Mainard, D.; Barbier, O.; Knafo, Y.; Belleville, R.; Mainard-Simard, L.; Gross, J.B. Accuracy and reproducibility of preoperative three-dimensional planning for total hip arthroplasty using biplanar low-dose radiographs: A pilot study. Orthop. Traumatol. Surg. Res. 2017, 103, 531–536. [Google Scholar] [CrossRef] [PubMed]
- Polkowski, G.; Nunley, R.; Ruh, E.; Williams, B.; Barrack, R. Barrack, Does Standing Affect Acetabular Component Inclination and Version After THA? Clin. Orthop. Relat. Res. 2012, 470, 2988–2994. [Google Scholar] [CrossRef] [PubMed]
- Sun, D.C.; Murphy, W.S.; Amundson, A.J.; Lane, P.M.; Kowal, J.H.; Murphy, S.B. Validation of a Novel Method of Measuring Cup Orientation Using BiPlanar Simultaneous Radiographic Images. J. Arthroplast. 2023, 38, S252–S256. [Google Scholar] [CrossRef]
- Tokunaga, K.; Okamoto, M.; Watanabe, K. Implant Orientation Measurement After THA Using the EOS X-Ray Image Acquisition System. Adv. Exp. Med. Biol. 2018, 1093, 335–343. [Google Scholar]
- Barbier, O.; Skalli, W.; Mainard, D. Changes In Pelvic Orientation After Total Hip Arthroplasty: A Prospective Study With EOS™. Acta Orthop. Belg. 2017, 83, 360–366. [Google Scholar]
- Innmann, M.M.; McGoldrick, N.P.; Ratra, A.; Merle, C.; Grammatopoulos, G. The accuracy in determining pelvic tilt from anteroposterior pelvic radiographs in patients awaiting hip arthroplasty. J. Orthop. Res. 2022, 40, 854–861. [Google Scholar] [CrossRef] [PubMed]
- Loppini, M.; Pisano, A.; Ruggeri, R.; Della Rocca, A.; Grappiolo, G. Pelvic tilt and functional acetabular position after total hip arthroplasty: An EOS 2D/3D radiographic study. HIP Int. 2022, 33, 365–370. [Google Scholar] [CrossRef]
- Premkumar, A.; Almeida, B.; Ranawat, C.S.; Jerabek, S.A.; Esposito, C.I.; Mayman, D.J. Variability of pelvic axial rotation in patients undergoing total hip arthroplasty. HIP Int. 2021, 31, 215–222. [Google Scholar] [CrossRef]
- Barbier, O.; Skalli, W.; Mainard, L.; Mainard, D. The reliability of the anterior pelvic plane for computer navigated acetabular component placement during total hip arthroplasty: Prospective study with the EOS imaging system. Orthop. Traumatol. Surg. Res. 2014, 100 (Suppl. S6), S287–S291. [Google Scholar] [CrossRef] [PubMed]
- Ben-Ari, E.; Shichman, I.; Sissman, E.; Oakley, C.; Hepinstall, M.; Schwarzkopf, R. Calibration of magnification in two-dimensional low-dose full-body imaging for preoperative planning of total hip arthroplasty. Arch. Orthop. Trauma. Surg. 2023, 143, 6875–6881. [Google Scholar] [CrossRef] [PubMed]
- Fischer, M.C.M.; Tokunaga, K.; Okamoto, M.; Habor, J.; Radermacher, K. Preoperative factors improving the prediction of the postoperative sagittal orientation of the pelvis in standing position after total hip arthroplasty. Sci. Rep. 2020, 10, 15944. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.; Zhu, Y.; Ma, W.; Zhang, Z.; Shi, W.; Lin, J. A Novel Method for Accurate Preoperative Templating for Total Hip Arthroplasty Using a Biplanar Digital Radiographic (EOS) System. JBJS Open Access 2020, 5, e20.00078. [Google Scholar] [CrossRef]
- Knafo, Y.; Houfani, F.; Zaharia, B.; Egrise, F.; Clerc-Urmès, I.; Mainard, D. Value of 3D Preoperative Planning for Primary Total Hip Arthroplasty Based on Biplanar Weightbearing Radiographs. Biomed. Res. Int. 2019, 2019, 1932191. [Google Scholar] [CrossRef] [PubMed]
- Pour, A.E.; Green, J.H.; Christensen, T.H.; Muthusamy, N.; Schwarzkopf, R. Is It Necessary to Obtain Lateral Pelvic Radiographs in Flexed Seated Position for Preoperative Total Hip Arthro-plasty Planning? Arthroplast. Today 2023, 21, 101133. [Google Scholar] [CrossRef] [PubMed]
- Sutphen, S.A.; Lipman, J.D.; Jerabek, S.A.; Mayman, D.J.; Esposito, C.I. Treatment of Recurrent Dislocation after Total Hip Arthroplasty Using Advanced Imaging and Three-Dimensional Modeling Techniques: A Case Series. Hss J. 2020, 16 (Suppl. S2), 245–255. [Google Scholar] [CrossRef]
- Bendaya, S.; Anglin, C.; Lazennec, J.Y.; Allena, R.; Thoumie, P.; Skalli, W. Good vs Poor Results After Total Hip Arthroplasty: An Analysis Method Using Implant and Anatomic Parameters With the EOS Imaging System. J. Arthroplast. 2016, 31, 2043–2052. [Google Scholar] [CrossRef]
- Esposito, C.I.; Carroll, K.M.; Sculco, P.K.; Padgett, D.E.; Jerabek, S.A.; Mayman, D.J. Total Hip Arthroplasty Patients With Fixed Spinopelvic Alignment Are at Higher Risk of Hip Dislocation. J. Arthroplast. 2018, 33, 1449–1454. [Google Scholar] [CrossRef]
- Jang, S.J.; Vigdorchik, J.M.; Windsor, E.W.; Schwarzkopf, R.; Mayman, D.J.; Sculco, P.K. Abnormal spinopelvic mobility as a risk factor for acetabular placement error in total hip arthroplasty using optical computer-assisted surgical navigation system. Bone Jt. Open 2022, 3, 475–484. [Google Scholar] [CrossRef]
- Kim, Y.; Pour, A.E.; Lazennec, J.Y. Low pelvic incidence is a risk factor for intraoperative complications in minimally invasive anterolateral approach for total hip arthroplasty. Hip Int. 2022, 32, 304–311. [Google Scholar] [CrossRef] [PubMed]
- Kouyoumdjian, P.; Mansour, J.; Marouby, S.; Canovas, F.; Dagneaux, L.; Coulomb, R. Influence of kinematics of the lumbopelvic complex in hip arthroplasty dislocation: From assessment to recommendations. Arch. Orthop. Trauma. Surg. 2023, 143, 4773–4783. [Google Scholar] [CrossRef] [PubMed]
- Lazennec, J.Y.; Rangel, A.; Baudoin, A.; Skalli, W.; Catonne, Y.; Rousseau, M.A. The EOS imaging system for understanding a patellofemoral disorder following THR. Orthop. Traumatol. Surg. Res. 2011, 97, 98–101. [Google Scholar] [CrossRef] [PubMed]
- Lazennec, J.Y.; Thauront, F.; Robbins, C.B.; Pour, A.E. Acetabular and Femoral Anteversions in Standing Position are Outside the Proposed Safe Zone After Total Hip Arthroplasty. J. Arthroplast. 2017, 32, 3550–3556. [Google Scholar] [CrossRef] [PubMed]
- Perronne, L.; Haehnel, O.; Chevret, S.; Wybier, M.; Hannouche, D.; Nizard, R.; Bousson, V. How is quality of life after total hip replacement related to the reconstructed anatomy? A study with low-dose stereoradiography. Diagn. Interv. Imaging 2021, 102, 101–107. [Google Scholar] [CrossRef]
- Reina, N.; Hourtal, J.; Salib, C.G.; Gracia, G.; Cavaignac, E.; Chiron, P. The Delta of Correction: A novel, more reliable variable than limb-length discrepancy at predicting outcome after total hip arthroplasty. Hip Int. 2020, 30, 536–543. [Google Scholar] [CrossRef] [PubMed]
- Sarpong, N.O.; Rodriguez, S.; Kuyl, E.V.; Lyman, S.; Della Valle, A.G.; Vigdorchik, J.M.; Rodriguez, J.A. Dislocation Following Anterior and Posterior Total Hip Arthroplasty in the Setting of Spinal Deformity and Stiffness: Evolving Trends Using a High-Risk Protocol at a Single Tertiary Center. J. Arthroplast. 2024, 39, 1019–1024.e1. [Google Scholar] [CrossRef]
- Bassani, R.; Sirtori, P.; Morselli, C.; Cirullo, A.; Ciliberto, R.; Mangiavini, L.; Peretti, G.M. Simultaneous L5-S1 anterior lumbar interbody fusion and total hip arthroplasty through minimally invasive anterior approaches in hip-spine syndrome. J. Biol. Regul. Homeost. Agents 2022, 36, 239–245. [Google Scholar] [CrossRef]
- Bizdikian, A.J.; Assi, A.; Semaan, K.; Otayek, J.; Karam, M.; Massaad, A.; Jaber, E.; Ghanem, I.; El Rachkidi, R. Role of bilateral staged hip arthroplasty in Hip-spine syndrome: A case report. Medicine 2023, 102, e36296. [Google Scholar] [CrossRef]
- Esposito, C.I.; Miller, T.T.; Kim, H.J.; Barlow, B.T.; Wright, T.M.; Padgett, D.E.; Jerabek, S.A.; Mayman, D.J. Does Degenerative Lumbar Spine Disease Influence Femoroacetabular Flexion in Patients Undergoing Total Hip Arthroplasty? Clin. Orthop. Relat. Res. 2016, 474, 1788–1797. [Google Scholar] [CrossRef]
- Haffer, H.; Wang, Z.; Hu, Z.; Hipfl, C.; Pumberger, M. Acetabular cup position differs in spinopelvic mobility types: A prospective observational study of primary total hip arthroplasty patients. Arch. Orthop. Trauma. Surg. 2022, 142, 2979–2989. [Google Scholar] [CrossRef]
- Haffer, H.; Wang, Z.; Hu, Z.; Hipfl, C.; Perka, C.; Pumberger, M. Total Hip Replacement Influences Spinopelvic Mobility: A Prospective Observational Study. J. Arthroplast. 2022, 37, 316–324.e2. [Google Scholar] [CrossRef] [PubMed]
- Vigdorchik, J.M.; Shafi, K.A.; Kolin, D.A.; Buckland, A.J.; Carroll, K.M.; Jerabek, S.A. Does Low Back Pain Improve Following Total Hip Arthroplasty? J. Arthroplast. 2022, 37, S937–S940. [Google Scholar] [CrossRef] [PubMed]
- Haffer, H.; Wang, Z.; Hu, Z.; Becker, L.; Müllner, M.; Hipfl, C.; Pumberger, M.; Palmowski, Y. Does obesity affect acetabular cup position, spinopelvic function and sagittal spinal alignment? A prospective investigation with standing and sitting assessment of primary hip arthroplasty patients. J. Orthop. Surg. Res. 2021, 16, 640. [Google Scholar] [CrossRef]
- Haffer, H.; Wang, Z.; Hu, Z.; Muellner, M.; Hipfl, C.; Pumberger, M. Effect of Coronal and Sagittal Spinal Malalignment on Spinopelvic Mobility in Patients Undergoing Total Hip Replacement: A Prospective Observational Study. Clin. Spine Surg. 2022, 35, E510–E519. [Google Scholar] [CrossRef] [PubMed]
- Shintaro, W.; Hyonmin, C.; Naomi, K.; Hiroyuki, I.; Daigo, K.; Yutaka, I.; Watanabe, S.; Choe, H.; Kobayashi, N.; Ike, H.; et al. Prediction of pelvic mobility using whole-spinal and pelvic alignment in standing and sitting position in total hip arthroplasty patients. J. Orthop. Surg. 2021, 29, 10225536. [Google Scholar]
- Clavé, A.; Fazilleau, F.; Cheval, D.; Williams, T.; Lefèvre, C.; Stindel, E. Comparison of the reliability of leg length and offset data generated by three hip replacement CAOS systems using EOS™ imaging. Orthop. Traumatol. Surg. Res. 2015, 101, 647–653. [Google Scholar] [CrossRef] [PubMed]
- van Drongelen, S.; Kaldowski, H.; Tarhan, T.; Assi, A.; Meurer, A.; Stief, F. Are changes in radiological leg alignment and femoral parameters after total hip replacement responsible for joint loading during gait? BMC Musculoskelet. Disord. 2019, 20, 526. [Google Scholar] [CrossRef]
- Di Laura, A.; Henckel, J.; Gal, E.D.; Monem, M.; Moralidou, M.; Hart, A.J. Reconstruction of acetabular defects greater than Paprosky type 3B: The importance of functional imaging. BMC Musculoskelet. Disord. 2021, 22, 207. [Google Scholar] [CrossRef] [PubMed]
- Gharanizadeh, K.; Mahmoudi, M.; Shiva, F.; Ghazavi, M.; Abolghasemian, M. Assessing Leg Length Discrepancy Is Necessary Before Arthroplasty in Patients With Unilateral Crowe Type IV Hip Dislocation. Clin. Orthop. Relat. Res. 2023, 481, 1783–1789. [Google Scholar] [CrossRef]
- Waibel, F.W.A.; Berndt, K.; Jentzsch, T.; Farei-Campagna, J.; Rahm, S.; Dora, C.; Zingg, P.O. Symptomatic leg length discrepancy after total hip arthroplasty is associated with new onset of lower back pain. Orthop. Traumatol. Surg. Res. 2021, 107, 102761. [Google Scholar] [CrossRef] [PubMed]
- Lazennec, J.Y.; Folinais, D.; Florequin, C.; Pour, A.E. Does Patients’ Perception of Leg Length After Total Hip Arthroplasty Correlate With Anatomical Leg Length? J. Arthroplast. 2018, 33, 1562–1566. [Google Scholar] [CrossRef]
- Lecoanet, P.; Vargas, M.; Pallaro, J.; Thelen, T.; Ribes, C.; Fabre, T. Leg length discrepancy after total hip arthroplasty: Can leg length be satisfactorily controlled via anterior approach without a traction table? Evaluation in 56 patients with EOS 3D. Orthop. Traumatol. Surg. Res. 2018, 104, 1143–1148. [Google Scholar] [CrossRef] [PubMed]
- van Drongelen, S.; Fey, B.; Stief, F.; Meurer, A. Influence of implantation of a total hip endoprosthesis on the ipsilateral leg alignment: The effect of sex and dysplasia of the hip. Arch. Orthop. Trauma Surg 2022, 143, 3541–3549. [Google Scholar] [CrossRef] [PubMed]
- Chalmers, B.P.; LaGreca, M.; Addona, J.; Sculco, P.K.; Haas, S.B.; Mayman, D.J. Characterizing the Magnitude of and Risk Factors for Functional Limb Lengthening in Patients Undergoing Primary Total Knee Arthroplasty. Hss J. 2022, 18, 271–276. [Google Scholar] [CrossRef] [PubMed]
- Nam, D.; Williams, B.; Hirsh, J.; Johnson, S.R.; Nunley, R.M.; Barrack, R.L. Planned bone resections using an MRI-based custom cutting guide system versus 3-dimensional, weight-bearing images in total knee arthroplasty. J. Arthroplast. 2015, 30, 567–572. [Google Scholar] [CrossRef] [PubMed]
- Man, S.L.-C.; Chau, W.-W.; Zheng, X.; Ong, M.T.-Y.; Ho, K.K.-W. Accuracy and outcome of a handheld accelerometer-based navigation device compared to conventional alignment method in total knee arthroplasty in a Chinese population, Journal of Orthopaedics. Trauma. Rehabil. 2024, 31, 34–47. [Google Scholar] [CrossRef]
- Hau, M.Y.T.; Menon, D.K.; Chan, R.J.N.; Chung, K.Y.; Chau, W.W.; Ho, K.W. Two-dimensional/three-dimensional EOS™ imaging is reliable and comparable to traditional X-ray imaging assessment of knee osteoarthritis aiding surgical management. Knee 2020, 27, 970–979. [Google Scholar] [CrossRef]
- Elkins, J.M.; Simoens, K.J.; Callaghan, J.J. Lower Extremity Geometry in Morbid Obesity-Considerations for Total Knee Arthroplasty. J. Arthroplast. 2018, 33, 3304–3312. [Google Scholar] [CrossRef] [PubMed]
- Bahadır, T.; Werner, J.; Clair, A.J.; Walker, P.S. Guidelines for Instrumentation for Total Knee Replacement Based on Frontal Plane Radiographs. Bull. Hosp. Jt. Dis. 2018, 76, 238–245. [Google Scholar]
- Finsterwald, M.A.; Sobhi, S.; Isaac, S.; Scott, P.; Khan, R.J.K.; Fick, D.P. Accuracy of one-dimensional templating on linear EOS radiography allows template-directed instrumentation in total knee arthroplasty. J. Orthop. Surg. Res. 2021, 16, 664. [Google Scholar] [CrossRef] [PubMed]
- Ji, S.; Huang, Y.; Zhou, Y.; Wang, C.; Wang, X.; Ma, C.; Jiang, X. Pre-operative predictive factors of residual varus on the mechanical axis after Oxford unicompartmental knee arthroplasty. Front. Surg. 2022, 9, 1054351. [Google Scholar] [CrossRef]
- Vigdorchik, J.M.; Sharma, A.K.; Feder, O.I.; Buckland, A.J.; Mayman, D.J.; Carroll, K.M.; Sculco, P.K.; Long, W.J.; Jerabek, S.A. Stiffness After Total Knee Arthroplasty: Is It a Result of Spinal Deformity? J. Arthroplast. 2020, 35, S330–S335. [Google Scholar] [CrossRef] [PubMed]
- Liow, M.H.; Tsai, T.Y.; Dimitriou, D.; Li, G.; Kwon, Y.M. Does 3-Dimensional In Vivo Component Rotation Affect Clinical Outcomes in Unicompartmental Knee Arthroplasty? J. Arthroplast. 2016, 31, 2167–2172. [Google Scholar] [CrossRef] [PubMed]
- Schlatterer, B.; Suedhoff, I.; Bonnet, X.; Catonne, Y.; Maestro, M.; Skalli, W. Skeletal landmarks for TKR implantations: Evaluation of their accuracy using EOS imaging acquisition system. Orthop. Traumatol. Surg. Res. 2009, 95, 2–11. [Google Scholar] [CrossRef] [PubMed]
- Meijer, M.; Boerboom, A.; Bulstra, S.; Reininga, I.; Stevens, M.; Meijer, M.F.; Boerboom, A.L.; Bulstra, S.K.; Reininga, I.H.F. Do CAS measurements correlate with EOS 3D alignment measurements in primary TKA? Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 2894–2903. [Google Scholar] [CrossRef] [PubMed]
- Corbett, J.; Tai, J.; Salmon, L.; Roe, J. Comparison of CT and EOS in assessing coronal lower limb alignment when planning total knee arthroplasty. Knee 2023, 42, 400–408. [Google Scholar] [CrossRef]
- Nam, D.; Vajapey, S.; Nunley, R.M.; Barrack, R.L. The Impact of Imaging Modality on the Measurement of Coronal Plane Alignment After Total Knee Arthroplasty. J. Arthroplast. 2016, 31, 2314–2319. [Google Scholar] [CrossRef]
- Ziv, Y.B.; Livshits, G.; Lamykin, K.; Khatib, S.; Sira, Y.B.; Rabau, O.; Shohat, N.; Essa, A. Excessive Sagittal Slope of the Tibia Component during Kinematic Alignment-Safety and Functionality at a Minimum 2-Year Follow-Up. J. Pers. Med. 2022, 12, 1407. [Google Scholar]
- Ziv, Y.B.; Essa, A.; Lamykin, K.; Chacar, N.; Livshits, G.; Khatib, S.; Comaya, Y.; Shohat, N. Minimum 2-Year Radiographic and Clinical Outcomes of Unrestricted Kinematic Alignment Total Knee Arthroplasty in Patients with Excessive Varus of the Tibia Component. J. Pers. Med. 2022, 12, 1206. [Google Scholar]
- Kim, S.C.; Choi, H.G.; Kim, J.S.; Kim, T.W.; Lee, Y.S. Effects of Total Knee Arthroplasty on Coronal and Sagittal Whole-Body Alignments: Serial Assessments Using Whole-Body EOS. J. Clin. Med. 2021, 10, 3242. [Google Scholar] [CrossRef] [PubMed]
- Meijer, M.F.; Boerboom, A.L.; Stevens, M.; Bulstra, S.K.; Reininga, I.H. Assessment of prosthesis alignment after revision total knee arthroplasty using EOS 2D and 3D imaging: A reliability study. PLoS ONE 2014, 9, e104613. [Google Scholar] [CrossRef] [PubMed]
- Tsai, T.-Y.; Dimitriou, D.; Liow, M.H.L.; Rubash, H.E.; Li, G.; Kwon, Y.-M. Three-Dimensional Imaging Analysis of Unicompartmental Knee Arthroplasty Evaluated in Standing Position: Component Alignment and In Vivo Articular Contact. J. Arthroplast. 2016, 31, 1096–1101. [Google Scholar] [CrossRef] [PubMed]
- Yoo, H.J.; Kim, J.E.; Kim, S.C.; Kim, J.S.; Yang, H.J.; Kim, T.W.; Lee, Y.S. Pitfalls in assessing limb alignment affected by rotation and flexion of the knee after total knee arthroplasty: Analysis using sagittal and coronal whole-body EOS radiography. Knee 2020, 27, 1551–1559. [Google Scholar] [CrossRef] [PubMed]
- Linderman, S.E.; Hall, J.R.L.; Johnson, J.E.; Caceres, A.P.; Hettrich, C.M.; Anderson, D.D. Return of Scapulohumeral Rhythm in Patients After Reverse Shoulder Arthroplasty: A Midterm Stereoradiographic Imaging Analysis. Iowa Orthop. J. 2022, 42, 227–237. [Google Scholar]
- Yoo, H.-J.; Choi, J.-K.; Heo, Y.-M.; Moon, S.-J.; Oh, B.-H. Changes in Parameters after High Tibial Osteotomy: Comparison of EOS System and Computed Tomographic Analysis. J. Clin. Med. 2023, 12, 5638. [Google Scholar] [CrossRef]
- Oh, B.H.; Seo, K.D.; Heo, Y.M.; Kim, T.K.; Choi, J.K.; Song, J.H. Coronal and sagittal alignment of ankle joint is significantly affected by high tibial osteotomy. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 4878–4885. [Google Scholar] [CrossRef]
- Sandoz, B.; Laporte, S.; Skalli, W.; Mitton, D. Subject-specific mass and 3D localisation of the mass centre of child body segments using biplanar X-rays. Comput. Methods Biomech. Biomed. Eng. 2008, 11, 203–204. [Google Scholar] [CrossRef]
- Rampal, V.; Rohan, P.Y.; Saksik, R.; Wicart, P.; Skalli, W. Assessing 3D paediatric foot morphology using low-dose biplanar radiography: Parameter reproducibility and preliminary values. Orthop. Traumatol. Surg. Res. 2018, 104, 1083–1089. [Google Scholar] [CrossRef] [PubMed]
- Rungprai, C.; Goetz, J.E.; Arunakul, M.; Gao, Y.; Femino, J.E.; Amendola, A.; Phisitkul, P. Validation and reproducibility of a biplanar imaging system versus conventional radiography of foot and ankle radiographic parameters. Foot Ankle Int. 2014, 35, 1166–1175. [Google Scholar] [CrossRef]
- Dubousset, J.; Charpak, G.; Dorion, I.; Skalli, W.; Lavaste, F.; Deguise, J.; Kalifa, G.; Ferey, S. A new 2D and 3D imaging approach to musculoskeletal physiology and pathology with low-dose radiation and the standing position: The EOS system. Bull. Acad. Natl. Med. 2005, 189, 287–297, discussion 297. [Google Scholar] [PubMed]
- Welborn, M.C.; Bouton, D.; Baksh, N.; Degan, T.; Sienko, S. Image Distortion in Biplanar Slot Scanning: Patient-specific Factors. J. Pediatr. Orthop. 2020, 40, 468–473. [Google Scholar] [CrossRef] [PubMed]
- Hui, S.C.; Pialasse, J.P.; Wong, J.Y.; Lam, T.P.; Ng, B.K.; Cheng, J.C.; Chu, W.C. Radiation dose of digital radiography (DR) versus micro-dose x-ray (EOS) on patients with adolescent idiopathic scoliosis: 2016 SOSORT-IRSSD “John Sevastic Award” Winner in Imaging Research. Scoliosis Spinal Disord. 2016, 11, 46. [Google Scholar] [CrossRef] [PubMed]
- Brooks, J.T.; Bomar, J.D.; Jeffords, M.E.; Farnsworth, C.L.; Pennock, A.T.; Upasani, V.V. Reliability of Low-dose Biplanar Radiography in Assessing Pediatric Torsional Pathology. J. Pediatr. Orthop. 2021, 41, 33–39. [Google Scholar] [CrossRef]
- Gaumétou, E.; Quijano, S.; Ilharreborde, B.; Presedo, A.; Thoreux, P.; Mazda, K.; Skalli, W. EOS analysis of lower extremity segmental torsion in children and young adults. Orthop. Traumatol. Surg. Res. 2014, 100, 147–151. [Google Scholar] [CrossRef] [PubMed]
- Ghanem, D.; Ghoul, A.; Assi, A.; Ghanem, I. Towards a better understanding of knee angular deformities: Discrepancies between clinical examination and 2D/3D assessments. Arch. Orthop. Trauma. Surg. 2024, 144, 1005–1011. [Google Scholar] [CrossRef] [PubMed]
- Gheno, R.; Nectoux, E.; Herbaux, B.; Baldisserotto, M.; Glock, L.; Cotten, A.; Boutry, N. Three-dimensional measurements of the lower extremity in children and adolescents using a low-dose biplanar X-ray device. Eur. Radiol. 2012, 22, 765–771. [Google Scholar] [CrossRef]
- Lerisson, H.; Amzallag-Bellenger, É.; Cebulski-Delebarre, A.; Nectoux, E.; Desmulliez, G.; Duhamel, A.; Drumez, E.; Herbaux, B.; Boutry, N. Assessment of micro-dose biplanar radiography in lower limb measurements in children. Eur. Radiol. 2018, 28, 1778–1787. [Google Scholar] [CrossRef]
- Meyrignac, O.; Moreno, R.; Baunin, C.; Vial, J.; Accadbled, F.; Sommet, A.; De Gauzy, J.S.; Sans, N. Low-dose biplanar radiography can be used in children and adolescents to accurately assess femoral and tibial torsion and greatly reduce irradiation. Eur. Radiol. 2014, 25, 1752–1760. [Google Scholar] [CrossRef]
- Ries, A.J.; Duffy, E.A.; Schwartz, M.H.; Novacheck, T.F.; Chau, M.M. Interobserver reliability of biplanar radiography is unaffected by clinical factors relevant to individuals at risk of pathological lower limb torsion. Gait Posture 2023, 100, 126–131. [Google Scholar] [CrossRef] [PubMed]
- Rosskopf, A.B.; Ramseier, L.E.; Sutter, R.; Pfirrmann, C.W.; Buck, F.M. Femoral and tibial torsion measurement in children and adolescents: Comparison of 3D models based on low-dose biplanar radiography and low-dose CT. AJR Am. J. Roentgenol. 2014, 202, W285–W291. [Google Scholar] [CrossRef] [PubMed]
- Rosskopf, A.; Buck, F.; Pfirrmann, C.; Ramseier, L.; Rosskopf, A.B.; Buck, F.M.; Pfirrmann, C.W.A.; Ramseier, L.E. Femoral and tibial torsion measurements in children and adolescents: Comparison of MRI and 3D models based on low-dose biplanar radiographs. Skelet. Radiol. 2017, 46, 469–476. [Google Scholar] [CrossRef] [PubMed]
- Schlégl, Á.T.; Nyakas, V.; Kovács, D.; Maróti, P.; Józsa, G.; Than, P. Neck-shaft angle measurement in children: Accuracy of the conventional radiography-based (2D) methods compared to 3D reconstructions. Sci. Rep. 2022, 12, 16494. [Google Scholar]
- Westberry, D.E.; Carpenter, A.M. 3D Modeling of Lower Extremities With Biplanar Radiographs: Reliability of Measures on Subsequent Examinations. J. Pediatr. Orthop. 2019, 39, 521–526. [Google Scholar] [CrossRef] [PubMed]
- Yucekul, A.; Karaytug, K.; Bakircioglu, S.; Zulemyan, T.; Sirin, B.K.; Karaarslan, E.; Yilgor, C.; Alanay, A. Prevalence of benign bone lesions of the lower extremity in the pediatric spinal disorders: A whole-body imaging study. J. Pediatr. Orthop. B 2022, 31, 583–590. [Google Scholar] [CrossRef]
- Assi, A.; Presedo, A.; Baudoin, A.; Mitton, D.; Ghanem, I.; Skalli, W. Specific 3D reconstruction for children lower limbs using a low dose biplanar X-ray system. Reproducibility of clinical parameters for cerebral palsy patients. Comput. Methods Biomech. Biomed. Eng. 2007, 10, 27–28. [Google Scholar] [CrossRef]
- Assi, A.; Chaibi, Y.; Presedo, A.; Dubousset, J.; Ghanem, I.; Skalli, W. Three-dimensional reconstructions for asymptomatic and cerebral palsy children’s lower limbs using a biplanar X-ray system: A feasibility study. Eur. J. Radiol. 2013, 82, 2359–2364. [Google Scholar] [CrossRef]
- Bonnet-Lebrun, A.; Linglart, A.; De Tienda, M.; Ouchrif, Y.; Berkenou, J.; Assi, A.; Wicart, P.; Skalli, W. Quantitative analysis of lower limbs and pelvis deformities in children with X-linked hypophosphatemic rickets. Orthop. Traumatol. Surg. Res. 2022, 109, 103187. [Google Scholar] [CrossRef] [PubMed]
- Burkus, M.; Schlégl, Á.T.; József, K.; O’Sullivan, I.; Márkus, I.; Tunyogi-Csapó, M. Analysis of Proximal Femoral Parameters in Adolescent Idiopathic Scoliosis. Adv. Orthop. 2019, 2019, 3948595. [Google Scholar] [CrossRef]
- Karam, M.; Bizdikian, A.J.; Khalil, N.; Bakouny, Z.; Obeid, I.; Ghanimeh, J.; Labaki, C.; Mjaess, G.; Karam, A.; Skalli, W.; et al. Alterations of 3D acetabular and lower limb parameters in adolescent idiopathic scoliosis. Eur. Spine J. 2020, 29, 2010–2017. [Google Scholar] [CrossRef] [PubMed]
- Márkus, I.; Schlégl, Á.T.; Burkus, M.; József, K.; Niklai, B.; Than, P.; Tunyogi-Csapó, M. The effect of coronal decompensation on the biomechanical parameters in lower limbs in adolescent idiopathic scoliosis. Orthop. Traumatol. Surg. Res. 2018, 104, 609–616. [Google Scholar] [CrossRef] [PubMed]
- Miao, M.; Cai, H.; Zhang, L.; Cai, H. Analysis of lower extremity alignment (LEA) in children with recurrent patellar dislocation by EOS system. Front. Pediatr. 2023, 11, 1291739. [Google Scholar] [CrossRef] [PubMed]
- Rampal, V.; Rohan, P.Y.; Pillet, H.; Bonnet-Lebrun, A.; Fonseca, M.; Desailly, E.; Wicart, P.; Skalli, W. Combined 3D analysis of lower-limb morphology and function in children with idiopathic equinovarus clubfoot: A preliminary study. Orthop. Traumatol. Surg. Res. 2020, 106, 1333–1337. [Google Scholar] [CrossRef] [PubMed]
- Westberry, D.E.; Wack, L.I.; Davis, R.B.; Hardin, J.W. Femoral anteversion assessment: Comparison of physical examination, gait analysis, and EOS biplanar radiography. Gait Posture 2018, 62, 285–290. [Google Scholar] [CrossRef] [PubMed]
- Assi, A.; Sauret, C.; Massaad, A.; Bakouny, Z.; Pillet, H.; Skalli, W.; Ghanem, I. Validation of hip joint center localization methods during gait analysis using 3D EOS imaging in typically developing and cerebral palsy children. Gait Posture 2016, 48, 30–35. [Google Scholar] [CrossRef] [PubMed]
- Bailly, R.; Lempereur, M.; Pons, C.; Houx, L.; Thepaut, M.; Borotikar, B.; Gross, R.; Brochard, S. 3-D lower extremity bone morphology in ambulant children with cerebral palsy and its relation to gait. Ann. Phys. Rehabil. Med. 2021, 64, 101254. [Google Scholar] [CrossRef]
- Bailly, R.; Lempereur, M.; Thepaut, M.; Pons, C.; Houx, L.; Brochard, S. Relationship between 3D lower limb bone morphology and 3D gait variables in children with uni and bilateral Cerebral Palsy. Gait Posture 2022, 92, 51–59. [Google Scholar] [CrossRef] [PubMed]
- Bonnet-Lebrun, A.; Linglart, A.; De Tienda, M.; Khac, V.N.; Ouchrif, Y.; Berkenou, J.; Pillet, H.; Assi, A.; Wicart, P.; Skalli, W. Combined gait analysis and radiologic examination in children with X-linked hypophosphatemia. Clin. Biomech. 2023, 105, 105974. [Google Scholar] [CrossRef]
- Chen, C.; Milbrandt, T.A.; Babadi, E.; Duong, S.Q.; Larson, D.R.; Shaughnessy, W.J.; Stans, A.A.; Hull, N.C.; Peterson, H.A.; Larson, A.N. Normative Femoral and Tibial Lengths in a Modern Population of Twenty-First-Century U.S. Children. J. Bone Jt. Surg. Am. 2023, 105, 468–478. [Google Scholar] [CrossRef]
- Rampal, V.; Rohan, P.Y.; Assi, A.; Ghanem, I.; Rosello, O.; Simon, A.L.; Gaumetou, E.; Merzoug, V.; Skalli, W.; Wicart, P. Lower-limb lengths and angles in children older than six years: Reliability and reference values by EOS(®) stereoradiography. Orthop. Traumatol. Surg. Res. 2018, 104, 389–395. [Google Scholar] [CrossRef]
- Sekiya, T.; Aota, Y.; Yamada, K.; Kaneko, K.; Ide, M.; Saito, T. Evaluation of functional and structural leg length discrepancy in patients with adolescent idiopathic scoliosis using the EOS imaging system: A prospective comparative study. Scoliosis Spinal Disord. 2018, 13, 7. [Google Scholar] [CrossRef] [PubMed]
- Khalifé, M.; Vergari, C.; Rebeyrat, G.; Ferrero, E.; Guigui, P.; Assi, A.; Skalli, W. Femoral neck version in the spinopelvic and lower limb 3D alignment: A full-body EOS(®) study in 400 healthy subjects. Eur. Spine J. 2024, 33, 1807–1815. [Google Scholar] [CrossRef]
- Loppini, M.; Longo, U.G.; Ragucci, P.; Trenti, N.; Balzarini, L.; Grappiolo, G. Analysis of the Pelvic Functional Orientation in the Sagittal Plane: A Radiographic Study With EOS 2D/3D Technology. J. Arthroplast. 2017, 32, 1027–1032. [Google Scholar] [CrossRef]
- Passmore, E.; Graham, H.K.; Sangeux, M. Defining the medial-lateral axis of the femur: Medical imaging, conventional and functional calibration methods lead to differences in hip rotation kinematics for children with torsional deformities. J. Biomech. 2018, 69, 156–163. [Google Scholar] [CrossRef] [PubMed]
- Prum, G.; Sauret, C.; Bourgain, M.; Rouillon, O.; Rouch, P.; Thoreux, P. Can early golfing lead to acetabular and lower limb changes? A cross-sectional study. Int. J. Sports Sci. Coach. 2022, 18, 270–277. [Google Scholar] [CrossRef]
- Pytiak, A.; Bomar, J.D.; Peterson, J.B.; Schmitz, M.R.; Pennock, A.T.; Wenger, D.R.; Upasani, V.V. Analysis of spinal alignment and pelvic parameters on upright radiographs: Implications for acetabular development. J. Hip Preserv. Surg. 2016, 3, 208–214. [Google Scholar] [CrossRef]
- Rampal, V.; Hausselle, J.; Thoreux, P.; Wicart, P.; Skalli, W. Three-dimensional morphologic study of the child’s hip: Which parameters are reproducible? Clin. Orthop. Relat. Res. 2013, 471, 1343–1348. [Google Scholar] [CrossRef] [PubMed]
- Schlégl, Á.T.; Szuper, K.; Somoskeöy, S.; Than, P. Three dimensional radiological imaging of normal lower-limb alignment in children. Int. Orthop. 2015, 39, 2073–2080. [Google Scholar] [CrossRef]
- Szuper, K.; Schlégl, Á.; Vermes, C.; Somoskeöy, S.; Than, P.; Leidecker, E. Three-dimensional quantitative analysis of the proximal femur and the pelvis in children and adolescents using an upright biplanar slot-scanning X-ray system. Pediatr. Radiol. 2015, 45, 411–421. [Google Scholar] [CrossRef]
- Massaad, A.; Assi, A.; Bakouny, Z.; Sauret, C.; Khalil, N.; Skalli, W.; Ghanem, I. Three-dimensional evaluation of skeletal deformities of the pelvis and lower limbs in ambulant children with cerebral palsy. Gait Posture 2016, 49, 102–107. [Google Scholar] [CrossRef] [PubMed]
- Neirynck, J.; Proost, R.; Van Campenhout, A. The migration percentage measured on EOS® standing full-leg radiographs: Equivalent and advantageous in ambulant children with cerebral palsy. BMC Musculoskelet. Disord. 2019, 20, 366. [Google Scholar] [CrossRef]
- Thépaut, M.; Brochard, S.; Leboucher, J.; Lempereur, M.; Stindel, E.; Tissot, V.; Borotikar, B.; Borotikar, B.S. Measuring physiological and pathological femoral anteversion using a biplanar low-dose X-ray system: Validity, reliability, and discriminative ability in cerebral palsy. Skelet. Radiol. 2016, 45, 243–250. [Google Scholar] [CrossRef]
- Powell, J.; Gibly, R.F.; Faulk, L.W.; Carry, P.; Mayer, S.W.; Selberg, C.M. Can EOS Imaging Substitute for Conventional Radiography in Measurement of Acetabular Morphology in the Young Dysplastic Hip? J. Pediatr. Orthop. 2020, 40, 294–299. [Google Scholar] [CrossRef] [PubMed]
- Park, K.R.; Lee, J.H.; Kim, D.S.; Ryu, H.; Kim, J.; Yon, C.J.; Lee, S.W. The Comparison of Lower Extremity Length and Angle between Computed Radiography-Based Teleoroentgenogram and EOS(®) Imaging System. Diagnostics 2022, 12, 1052. [Google Scholar] [CrossRef] [PubMed]
- Schmitz, M.R.; Bittersohl, B.; Zaps, D.; Bomar, J.D.; Pennock, A.T.; Hosalkar, H.S. Spectrum of radiographic femoroacetabular impingement morphology in adolescents and young adults: An EOS-based double-cohort study. J. Bone Jt. Surg. Am. 2013, 95, e90. [Google Scholar] [CrossRef] [PubMed]
- Hughes, J.L.; Newton, P.O.; Bastrom, T.; Fabricant, P.D.; Pennock, A.T. The Clavicle Continues to Grow During Adolescence and Early Adulthood. Hss J. 2020, 16 (Suppl. S2), 372–377. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, J.C.; Guariento, A.; Nicholson, A.; Nguyen, M.K.; Gendler, L.; Ho-Fung, V.; Zhu, X.; Talwar, D.; Darge, K.; Flynn, J.M.; et al. Hand Bone Age Radiography: Comparison Between Slot-scanning and Conventional Techniques. J. Pediatr. Orthop. 2021, 41, e167–e173. [Google Scholar] [CrossRef]
- O’Sullivan, I.R.; Schégl, Á.T.; Varga, P.; Than, P.; Vermes, C. Femoral neck-shaft angle and bone age in 4- to 24-year-olds based on 1005 EOS three-dimensional reconstructions. J. Pediatr. Orthop. B 2021, 30, 337–345. [Google Scholar] [CrossRef]
- Schlégl, Á.T.; O’Sullivan, I.; Varga, P.; Than, P.; Vermes, C. Determination and correlation of lower limb anatomical parameters and bone age during skeletal growth (based on 1005 cases). J. Orthop. Res. 2017, 35, 1431–1441. [Google Scholar] [CrossRef] [PubMed]
- Schlégl, Á.T.; O’Sullivan, I.; Varga, P.; Than, P.; Vermes, C. Alternative methods for skeletal maturity estimation with the EOS scanner-Experience from 934 patients. PLoS ONE 2022, 17, e0267668. [Google Scholar] [CrossRef]
- Xie, L.; Ge, T.; Xiao, B.; Han, X.; Zhang, Q.; Xu, Z.; He, D.; Tian, W. Identification of Adolescent Menarche Status Using Biplanar X-ray Images: A Deep Learning-Based Method. Bioengineering 2023, 10, 769. [Google Scholar] [CrossRef] [PubMed]
- Vafadar, S.; Skalli, W.; Bonnet-Lebrun, A.; Khalifé, M.; Renaudin, M.; Hamza, A.; Gajny, L. A novel dataset and deep learning-based approach for marker-less motion capture during gait. Gait Posture 2021, 86, 70–76. [Google Scholar] [CrossRef] [PubMed]
- Tsai, A. Anatomical landmark localization via convolutional neural networks for limb-length discrepancy measurements. Pediatr. Radiol. 2021, 51, 1431–1447. [Google Scholar] [CrossRef]
- Aubert, B.; Vergari, C.; Ilharreborde, B.; Courvoisier, A.; Skalli, W. 3D reconstruction of rib cage geometry from biplanar radiographs using a statistical parametric model approach. Comput. Methods Biomech. Biomed. Eng. Imaging Vis. 2016, 4, 281–295. [Google Scholar] [CrossRef]
- Khalifé, M.; Vergari, C.; Ferrero, E.; Attali, V.; Heidsieck, C.; Assi, A.; Skalli, W. The rib cage: A new element in the spinopelvic chain. Eur. Spine J. 2022, 31, 1457–1467. [Google Scholar] [CrossRef]
- Assi, A.; Karam, M.; Skalli, W.; Vergari, C.; Vialle, R.; Pietton, R.; Bizdikian, A.J.; Kharrat, K.; Dubousset, J.; Ghanem, I. A Novel Classification of 3D Rib Cage Deformity in Subjects With Adolescent Idiopathic Scoliosis. Clin. Spine Surg. 2021, 34, 331–341. [Google Scholar] [CrossRef] [PubMed]
- Bouloussa, H.; Pietton, R.; Vergari, C.; Haen, T.X.; Skalli, W.; Vialle, R. Biplanar stereoradiography predicts pulmonary function tests in adolescent idiopathic scoliosis: A cross-sectional study. Eur. Spine J. 2019, 28, 1962–1969. [Google Scholar] [CrossRef] [PubMed]
- Courvoisier, A.; Ilharreborde, B.; Constantinou, B.; Aubert, B.; Vialle, R.; Skalli, W. Evaluation of a Three-Dimensional Reconstruction Method of the Rib Cage of Mild Scoliotic Patients. Spine Deform. 2013, 1, 321–327. [Google Scholar] [CrossRef] [PubMed]
- Machino, M.; Kawakami, N.; Ohara, T.; Saito, T.; Tauchi, R.; Imagama, S. Accuracy of rib cage parameters from 3-Dimensional reconstruction images obtained using simultaneous biplanar radiographic scanning technique in adolescent idiopathic scoliosis: Comparison with conventional computed tomography. J. Clin. Neurosci. 2020, 75, 94–98. [Google Scholar] [CrossRef]
- Vergari, C.; Aubert, B.; Lallemant-Dudek, P.; Haen, T.X.; Skalli, W. A novel method of anatomical landmark selection for rib cage 3D reconstruction from biplanar radiography. Comput. Methods Biomech. Biomed. Eng. Imaging Vis. 2020, 8, 15–23. [Google Scholar] [CrossRef]
- Yaszay, B.; Bastrom, T.; Bartley, C.; Parent, S.; Newton, P.; Bastrom, T.P.; Bartley, C.E.; Newton, P.O. The effects of the three-dimensional deformity of adolescent idiopathic scoliosis on pulmonary function. Eur. Spine J. 2017, 26, 1658–1664. [Google Scholar] [CrossRef] [PubMed]
- Clement, R.C.; Anari, J.; Bartley, C.E.; Bastrom, T.P.; Shah, R.; Talwar, D.; Upasani, V.V. What are normal radiographic spine and shoulder balance parameters among adolescent patients? Spine Deform. 2020, 8, 621–627. [Google Scholar] [CrossRef]
- Boscher, J.; Alain, A.; Vergnenegre, G.; Hummel, V.; Charissoux, J.L.; Marcheix, P.S. Femoral shaft fractures treated by antegrade locked intramedullary nailing: EOS stereoradiographic imaging evaluation of rotational malalignment having a functional impact. Orthop. Traumatol. Surg. Res. 2022, 108, 103235. [Google Scholar] [CrossRef]
- Orfeuvre, B.; Tonetti, J.; Kerschbaumer, G.; Barthelemy, R.; Moreau-Gaudry, A.; Boudissa, M. EOS stereographic assessment of femoral shaft malunion after intramedullary nailing. A prospective series of 48 patients at 9 months’ follow-up. Orthop. Traumatol. Surg. Res. 2021, 107, 102805. [Google Scholar] [CrossRef] [PubMed]
- Simon, A.L.; Apostolou, N.; Vidal, C.; Ferrero, E.; Mazda, K.; Ilharreborde, B. Paediatric tibial shaft fractures treated by open reduction and stabilization with monolateral external fixation. J. Child. Orthop. 2018, 12, 20–28. [Google Scholar] [CrossRef]
- Chua, C.X.K.; Tan, S.H.S.; Lim, A.K.S.; Hui, J.H. Accuracy of biplanar linear radiography versus conventional radiographs when used for lower limb and implant measurements. Arch. Orthop. Trauma. Surg. 2022, 142, 735–745. [Google Scholar] [CrossRef] [PubMed]
- Lecoanet, P.; Legallois, Y.; Ribes, C.; Lefevre, Y.; Cadennes, A.; Fabre, T. Medium-term evaluation of leg lengthening by ISKD® intramedullary nail in 28 patients: Should we still use this lengthening system? Orthop. Traumatol. Surg. Res. 2020, 106, 1433–1440. [Google Scholar] [CrossRef] [PubMed]
- Bakouny, Z.; Assi, A.; Yared, F.; Khalil, N.; Mansour, E.; Yaacoub, J.J.; Skalli, W.; Ghanem, I. Combining acetabular and femoral morphology improves our understanding of the down syndrome hip. Clin. Biomech. 2018, 58, 96–102. [Google Scholar] [CrossRef]
- Deng, M.; Chen, Q.; Deng, Q.; Shi, L.; Cheng, C.C.N.; Yeung, K.H.; Zhang, R.; Yu, W.P.F.; Lam, T.P.; Cheng, J.C.Y.; et al. Statistical changes of lung morphology in patients with adolescent idiopathic scoliosis after spinal fusion surgery-a prospective nonrandomized study based on low-dose biplanar X-ray imaging. Quant. Imaging Med. Surg. 2022, 12, 3325–3339. [Google Scholar] [CrossRef]
- Pietton, R.; Bouloussa, H.; Langlais, T.; Taytard, J.; Beydon, N.; Skalli, W.; Vergari, C.; Vialle, R. Estimating pulmonary function after surgery for adolescent idiopathic scoliosis using biplanar radiographs of the chest with 3D reconstruction. Bone Joint J. 2022, 104, 112–119. [Google Scholar] [CrossRef] [PubMed]
- Sabourin, M.; Jolivet, E.; Miladi, L.; Wicart, P.; Rampal, V.; Skalli, W. Three-dimensional stereoradiographic modeling of rib cage before and after spinal growing rod procedures in early-onset scoliosis. Clin. Biomech. 2010, 25, 284–291. [Google Scholar] [CrossRef] [PubMed]
- Ha, A.S.; Lee, N.; Blake, R.; Mathew, J.; Cerpa, M.; Lenke, L.G. Can spinal deformity patients maintain proper arm positions while undergoing full-body X-ray? Spine Deform. 2021, 9, 387–394. [Google Scholar] [CrossRef] [PubMed]
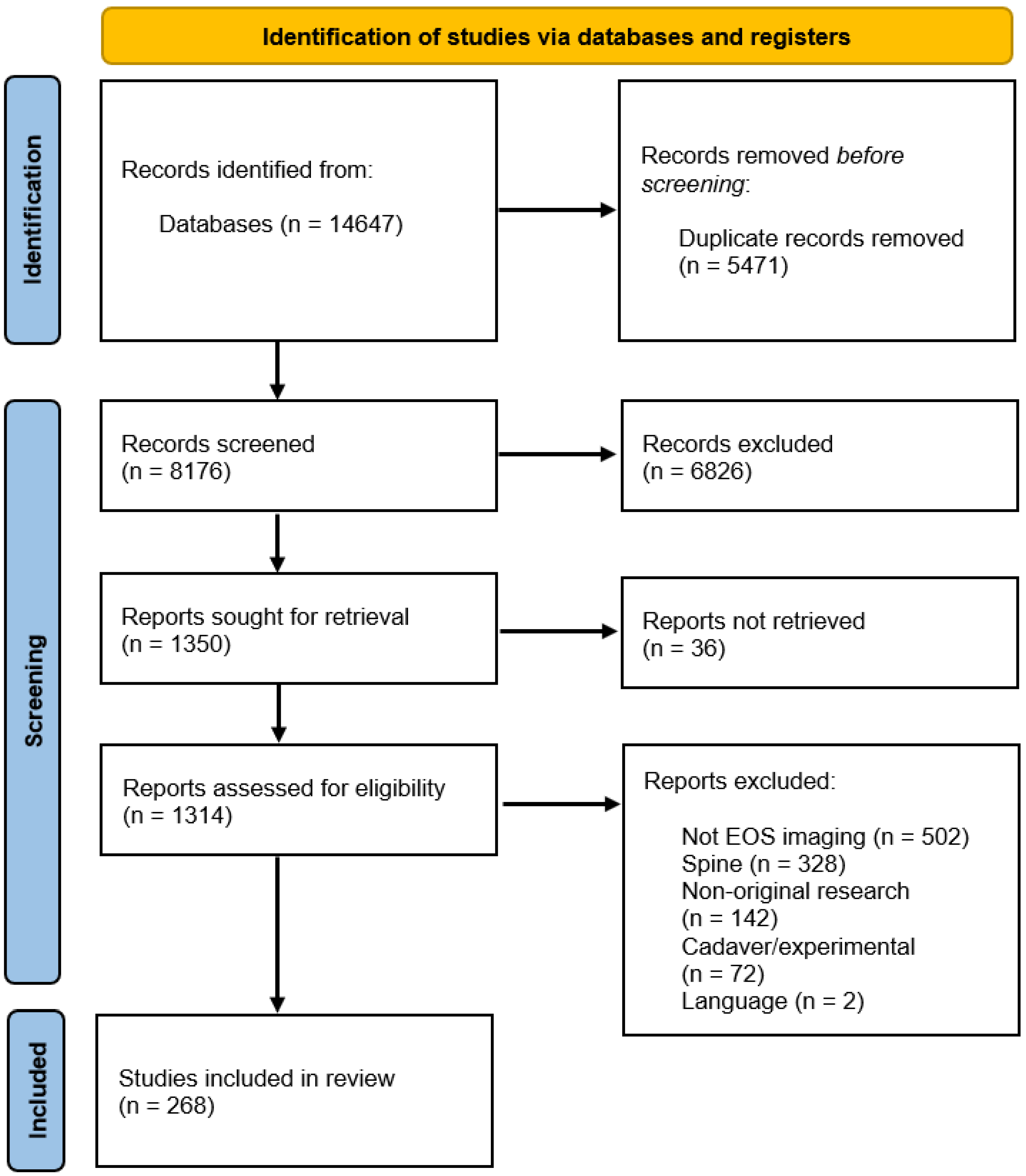
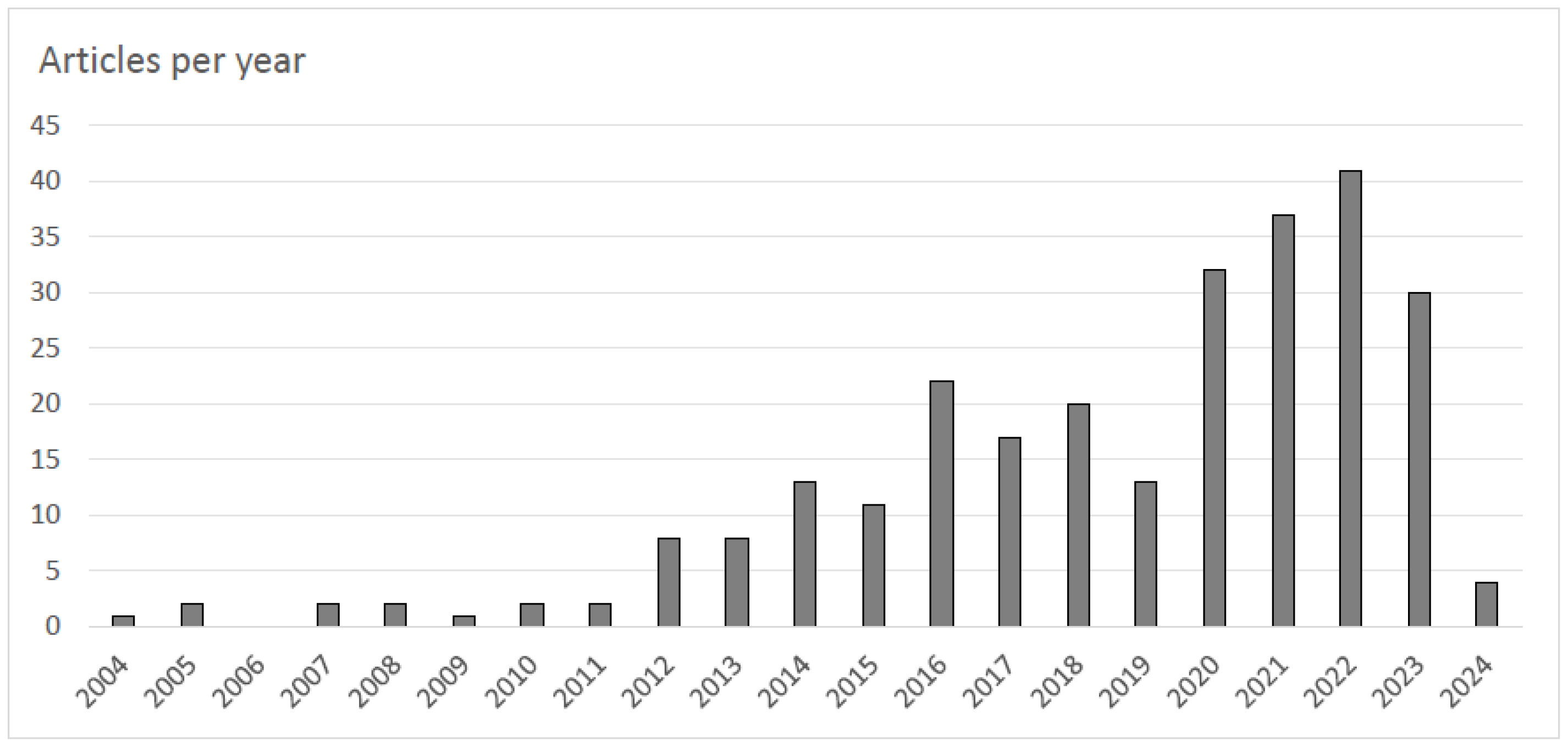
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Oman Medical Association. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brage, K.; Mussmann, B.; Pedersen, M.R.; Nissen, M.; Brage, O.; Mørup, S.D.; Geijer, M.; Larsen, P.; Jensen, J. Clinical Application of the EOS Imaging System—The Broader Horizon. J. Oman Med. Assoc. 2025, 2, 7. https://doi.org/10.3390/joma2010007
Brage K, Mussmann B, Pedersen MR, Nissen M, Brage O, Mørup SD, Geijer M, Larsen P, Jensen J. Clinical Application of the EOS Imaging System—The Broader Horizon. Journal of the Oman Medical Association. 2025; 2(1):7. https://doi.org/10.3390/joma2010007
Chicago/Turabian StyleBrage, Karen, Bo Mussmann, Malene Roland Pedersen, Marcus Nissen, Oliver Brage, Svea Deppe Mørup, Mats Geijer, Palle Larsen, and Janni Jensen. 2025. "Clinical Application of the EOS Imaging System—The Broader Horizon" Journal of the Oman Medical Association 2, no. 1: 7. https://doi.org/10.3390/joma2010007
APA StyleBrage, K., Mussmann, B., Pedersen, M. R., Nissen, M., Brage, O., Mørup, S. D., Geijer, M., Larsen, P., & Jensen, J. (2025). Clinical Application of the EOS Imaging System—The Broader Horizon. Journal of the Oman Medical Association, 2(1), 7. https://doi.org/10.3390/joma2010007






