Abstract
Background: Intestinal intussusception is defined as the invagination of one segment of the intestine into the lumen of an adjacent intestinal segment, resulting in the mechanical intestinal obstruction of multifactorial origin with a high risk of morbidity and mortality. It is a rare pathology in adults with a nonspecific clinical presentation. We present the case of a 26-year-old male patient who was admitted postoperatively after multiple extra institutional surgical interventions due to polytrauma secondary to a work-related accident that caused high-impact trauma by a solids mixer. However, he was referred to our institution due to suspected vascular trauma in the right femoral artery. During his hospital stay, he developed intolerance to oral intake associated with pain, abdominal distension, and persistent emetic episodes despite medical management. Consequently, an abdominal CT scan with double contrast was requested, revealing intestinal intussusception secondary to intestinal adhesions, which required new surgical management with a favorable resolution; Discussion: Intussusception in the adult population is rare and is primarily caused by an identifiable structural lesion. It is one of the most challenging pathologies in terms of diagnosis and management due to its nonspecific presentation. However, when postoperative symptoms indicating intestinal obstruction appear, a computed tomography scan is considered the imaging modality of choice for diagnosing intussusception in adults; Conclusions: The development of postoperative peritoneal adhesions is a common cause of intestinal obstruction that can lead to complications such as intestinal intussusception, requiring additional interventions. Therefore, it is vital to identify their presence to reduce morbidity and mortality.
1. Introduction
Intestinal intussusception is defined as the invagination of one segment of the intestine into the lumen of an adjacent intestinal segment. While it is a common cause of intestinal obstruction in the pediatric population, it is rare in adults, with an annual incidence of 2 cases per 100,000 people, representing up to 5% of all intussusceptions [1,2].
This pathology is commonly associated with an alteration in the intestinal wall. It is typically benign when involving the small intestine, including postoperative adhesions, and malignant when affecting the large intestine. Intussusception can be classified based on its anatomical location as colic, enteric, ileocecal, or ileocolic.
Symptoms are variable and nonspecific, including nausea, vomiting, abdominal pain, abdominal distension, constipation, and, in some cases, a palpable mass [3].
In recent years, the use of diagnostic imaging such as abdominal computed tomography (CT) has led to the increased detection of intestinal intussusception and is now more frequently used for preoperative diagnosis [1]. Regarding treatment, it varies without a universal consensus and can range from intestinal reduction to intestinal resection, depending on the individual context of each patient [2].
2. Case Report
We present the case of a 26-year-old male patient who was admitted to our institution postoperatively after multiple extra institutional surgical interventions for polytrauma secondary to a high-impact work-related accident involving a solids mixer. The patient was initially treated for closed thoracic trauma with hemopneumothorax, closed thoracostomy on the left side, unstable thorax due to a fracture of the 12th right rib with a thoracoabdominal hematoma, and fractures from the second to the ninth left ribs with laceration of the lingula and contusion of the upper segment of the lower lobe. He also had blunt abdominal trauma, prompting an exploratory laparotomy that revealed grade 4 splenic injuries and grade 2 hepatic injuries with 800cc of hemoperitoneum, leading to a splenectomy, peritoneal lavage, and drainage. Additionally, he sustained an open fracture of the right humerus, open fractures of the distal right tibia and fibula, a T-shaped acetabular fracture extending to the ilium, and a fracture of the inferior pole of the left scapula. Consequently, open fracture debridement and the lavage of the humerus were performed, along with the application of external fixators to the right humerus, tibia, and fibula. Due to suspected vascular trauma in the right femoral artery, he was referred to our institution.
A trauma assessment revealed fractures of the right transverse processes of L1, L3, and L4, which were deemed stable by spinal surgery, requiring no neurosurgical intervention. Thoracic surgery considered the rib fractures to be stable, with no need for surgical management, and removed the chest tube 14 days postoperatively without complications. Vascular surgery performed a CT angiogram of the thorax and abdomen, which showed no vascular injuries, and a CT angiogram of the extremities, which revealed the absence of flow in the distal third of the right peroneal artery but adequate flow in the posterior tibial artery, lateral plantar artery, and foot arch, with the right common femoral artery being patent. Since there was no ischemia in the limb, revascularization was not performed, and orthopedic management continued.
During his hospital stay, the patient experienced abdominal pain associated with multiple emetic episodes, abdominal distension, and intolerance to oral intake. Initially, these symptoms were considered to be of toxicological origin due to polypharmacy. However, given that it was the tenth postoperative day following laparotomy (splenectomy, lavage, and drainage of hemoperitoneum) and the persistence of symptoms, an abdominal CT scan with double contrast (Figure 1) was performed. This revealed a lack of contrast in medium progression, with a transition zone at the terminal ileum, showing an image of one intestinal loop within another, indicative of intestinal intussusception. Consequently, oral intake was suspended, and nasogastric decompression was performed for 24 h. A subsequent laparotomy (Figure 2) revealed adhesions at the level of the jejunum and ascending colon, an ileo–ileal intussusception 20 cm from the ileocecal valve with a length of 20 cm, caused by adhesions to the retroperitoneum and right pelvis, which was adequately reduced. There was also overdistension in three segments of the small intestine 20, 90, and 120 cm from the ileocecal valve, compromising the serosa, which required enterorrhaphy due to the high risk of perforation. Peritoneal lavage was performed due to turbid fluid, and areas of hypoperfused intestine were found, leading to the placement of a Viaflex bag for a second surgical procedure to evaluate the evolution of the enterorrhaphy and areas of hypoperfusion.
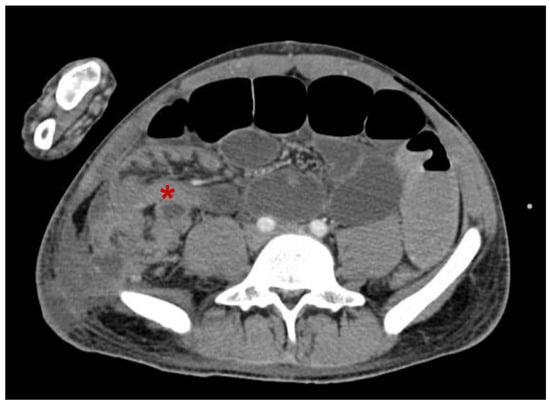
Figure 1.
Oral and IV contrast-enhanced abdominal computed tomography in the transverse section. absence of advance of the contrast medium, observing a transition zone at the level of the terminal ileum, with an image of an intestinal loop within an adjacent intestinal loop attributable to intestinal intussusception *. Source: Image taken by the authors.
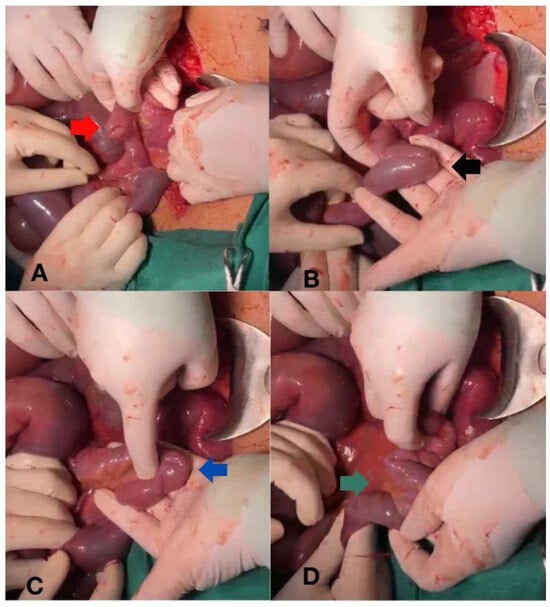
Figure 2.
Intestinal intussusception reduction sequence. (A) Identification of intestinal intussusception (red arrow). (B) Evidence of a band causing intestinal angulation, favoring the intussusception of 20 cm of the ileum (black arrow). (C) Intestinal band release and reduction in the intestinal intussusception (blue arrow). (D) Complete reduction in the intestinal intussusception (green arrow). Source: Image taken by the authors.
During the second surgical procedure, a systematic review of the intestine was conducted, revealing that the enterorrhaphy were in good condition with improved perfusion of the intestinal wall, with no evidence of other lesions. Therefore, the abdominal wall was closed. Postoperative intestinal transit was adequate without other gastrointestinal symptoms, and the patient was discharged from the service. Orthopedic management continued, and after the stabilization of the fractures and the control of infection, the patient was discharged from the hospital with favorable clinical progress.
3. Discussion
Intestinal intussusception is a rare form of intestinal obstruction in adults, where a segment of the intestine slides into the lumen of an adjacent intestinal segment. This condition is often caused by benign pathologies, which are more frequently found in the small intestine, such as leiomyomas, lipomas, Meckel’s diverticulum, and postoperative adhesions. However, it can also be caused by malignant pathologies, which are more commonly found in the large intestine, including primary tumors like adenocarcinomas, malignant polyps, carcinoids, leiomyosarcomas, and metastatic tumors [4,5,6].
Intestinal intussusception is classified according to its anatomical location into four types: colic, involving only the colon; enteric, involving only the small intestine; ileocecal, where the ileocecal valve acts as the reference point for the intussusception; and ileocolic, where the terminal ileum invaginates through the ileocecal valve into the colon [7].
For diagnosis, computed tomography (CT) is considered the method of choice over other imaging modalities, with sensitivity ranging from 68% to 100% and specificity from 57% to 71%. CT can reveal pathognomonic signs such as the telescoping of a segment of the gastrointestinal tract, a rounded mass with peripheral fat and edema, characterized by a “target sign” or sausage-shaped mass on longitudinal sections and a target-shaped mass on transverse sections, as shown in Figure 1 [1,2,8,9].
There is no universal consensus on the treatment of intestinal intussusception in adults. Management depends on the characteristics of the lesion, the associated pathology, its location, the degree of intussusception and obstruction, and the clinical condition of the patient. However, surgical intervention is reserved for cases where there is failure of reduction with endoscopic treatment, perforation, pneumoperitoneum, signs of peritonitis, sepsis or shock, or the presence of a pathological lesion [10,11,12].
Our patient presented with ileo–ileal intussusception secondary to intestinal adhesions from previous abdominal surgery. Intestinal reduction was performed with the release of the intestinal adhesions, resulting in favorable resolution without the recurrence of symptoms or complications.
4. Conclusions
The presence of postoperative intestinal adhesions is a common cause of intestinal obstruction that can lead to complications such as intestinal intussusception, which is rare in adults. Diagnosing this condition is challenging for surgeons due to its nonspecific signs and symptoms, with computed tomography (CT) being the most effective and accurate diagnostic method. Treatment should be individualized according to the clinical presentation and comorbidities of each patient.
Author Contributions
Conceptualization, C.V.J.G. and M.J.P.V.; methodology, M.J.P.V. and J.P.U.V.; validation C.V.J.G.; formal analysis, C.V.J.G. and M.J.P.V., investigation, C.V.J.G., M.J.P.V. and J.P.U.V., writing—original draft preparation, M.J.P.V. and J.P.U.V.; writing—review and editing, C.V.J.G., M.J.P.V. and J.P.U.V.; visualization, M.J.P.V.; supervision, C.V.J.G. and A.P.M.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Clinica de Marly S.A. Comité de Ética en Investigación-CEI, approved code: (CEISHCM) 003-2024.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patient(s) to publish this paper.
Data Availability Statement
The data presented in this study are available on request from the corresponding author due to identity protection measurements.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Aguirre, F.; Silva, Á.; Parra, P.; Salcedo, D.; López, P.; Acevedo, Y. Intussusception as cause of intestinal obstruction in the adult: A challenge for surgeons. Rev. Colomb. Cir. 2019, 34, 79–86. [Google Scholar] [CrossRef]
- Guillén, M.P.; Campillo, A.; Martín, J.G.; Torralba, J.A.; Mengual, M.; Cases, M.J.; Aguayo-Albasini, J.L. Adult intussusception—14 case reports and their outcomes. Rev. Esp. Enferm. Dig. 2010, 102, 32–36. [Google Scholar]
- Baldin, A.V.; De Rungs, B.D.R.; Ruiz, G.M.; Azcoitia, M.F. Intussusception in adults. Acta Med. 2014, 12, 137–140. [Google Scholar]
- Ludvigsson, J.F.; Nordenskjöld, A.; Murray, J.A.; Olén, O. A large nationwide population based case control study of the association between intussusception and later celiac disease. BMC Gastroenterol. 2013, 13, 89. [Google Scholar] [CrossRef] [PubMed]
- Erkan, N.; Haciyanli, M.; Yildirim, M.; Sayhan, H.; Vardar, E.; Polat, A.F. Intussusception in adults: An unusual and challenging condition for surgeons. Int. J. Colorectal Dis. 2005, 20, 452–456. [Google Scholar] [CrossRef] [PubMed]
- Shenoy, S.; Cassim, R. Metastatic melanoma to the gastrointestinal tract: Role of surgery as palliative treatment. West. Virginia Med. J. 2013, 109, 30–33. [Google Scholar]
- Azar, T.; Berger, D.L. Adult intussusception. Ann. Surg. 1997, 226, 134–138. [Google Scholar] [CrossRef] [PubMed]
- Gayer, G.; Zissin, R.; Apter, S.; Papa, M.; Hertz, M. Pictorial review: Adult intussusception a CT diagnosis. Br. J. Radiol. 2002, 75, 185–190. [Google Scholar] [CrossRef] [PubMed]
- Park, S.B.; Ha, H.K.; Kim, A.Y.; Lee, S.S.; Kim, H.J.; Park, B.J.; Jin, Y.H.; Park, S.H.; Kim, K.W. The diagnostic role of abdominal CT imaging findings in adults intussusception: Focused on the vascular compromise. Eur. J. Radiol. 2007, 62, 406–415. [Google Scholar] [CrossRef] [PubMed]
- Takeuchi, K.; Tsuzuki, Y.; Ando, T.; Sekihara, M.; Hara, T.; Kori, T.; Kuwano, H. The diagnosis and treatment of adult intussusception. J. Clin. Gastroenterol. 2003, 36, 18–21. [Google Scholar] [CrossRef] [PubMed]
- Ishibashi, Y.; Yamamoto, S.; Yamada, Y.; Fujita, S.; Akasu, T.; Moriya, Y. Laparoscopic resection for malignant lymphoma of the ileum causing ileocecal intussusception. Surg. Laparosc. Endosc. Percutan Tech. 2007, 17, 444–446. [Google Scholar] [CrossRef] [PubMed]
- Fisher, J.G.; Sparks, E.A.; Turner, C.G.; Klein, J.D.; Pennington, E.; Khan, F.A.; Zurakowski, D.; Durkin, E.T.; Fauza, D.O.; Modi, B.P. Operative indications in recurrent ileocolic intussusception. J. Pediatr. Surg. 2015, 50, 126–130. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).