A Healthcare Providers’ Survey for the Cognitive Rehabilitation of Multiple Sclerosis in France: From Research to Real Life
Abstract
:1. Backgrounds
1.1. Fundamental Background of Cognitive Rehabilitation in pwMSs
1.2. Proof of Concept
2. Methods
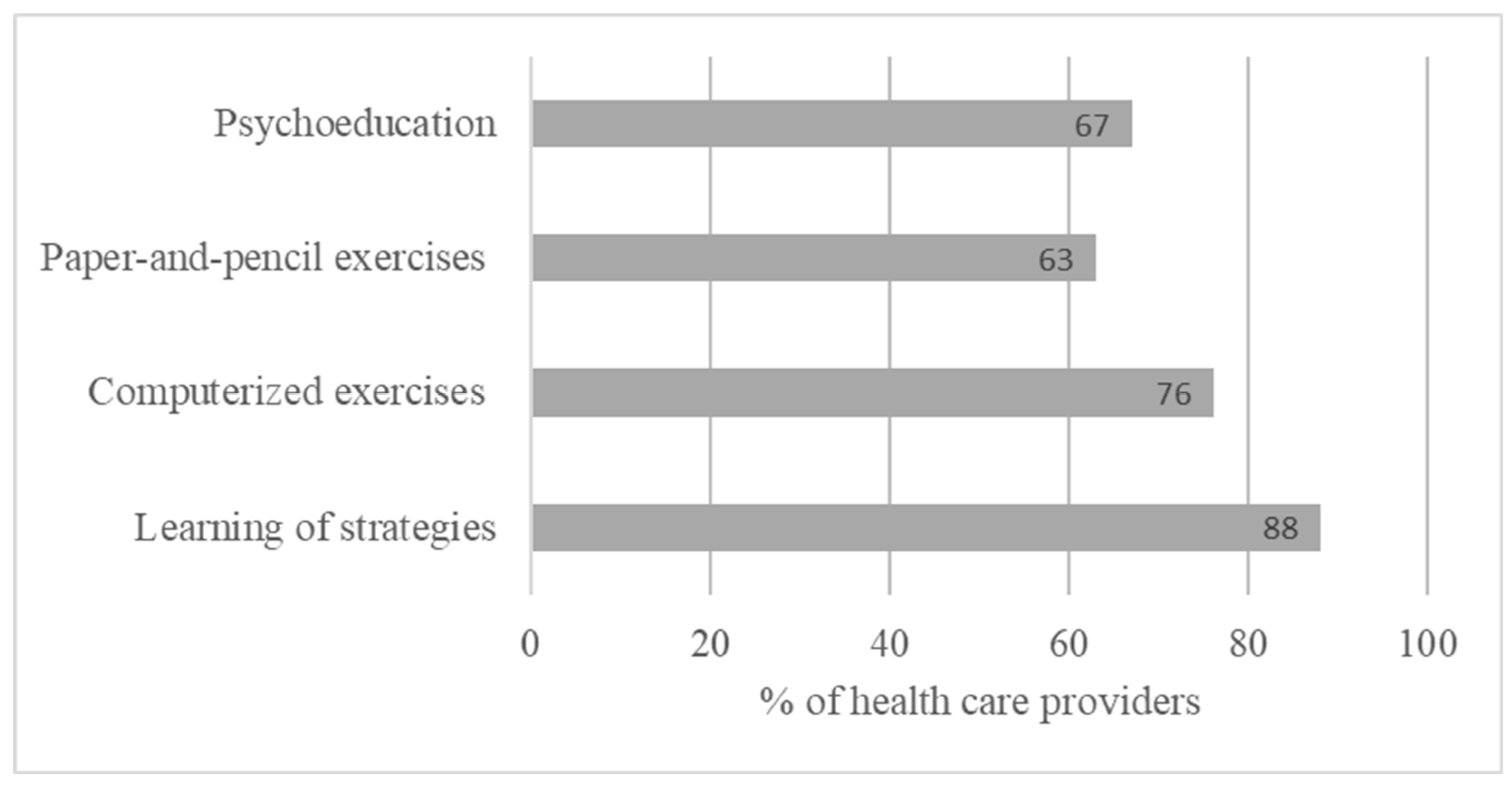
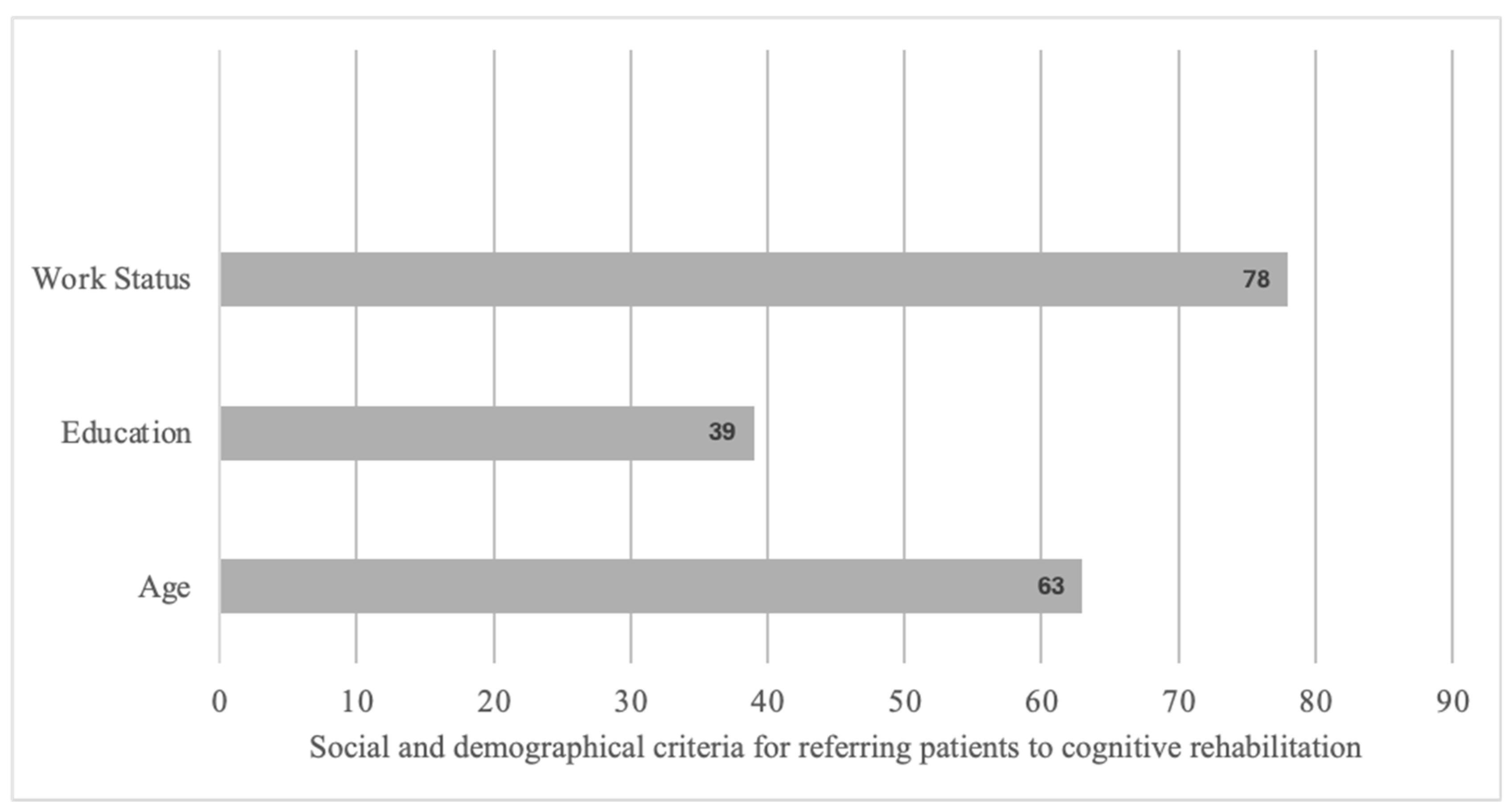
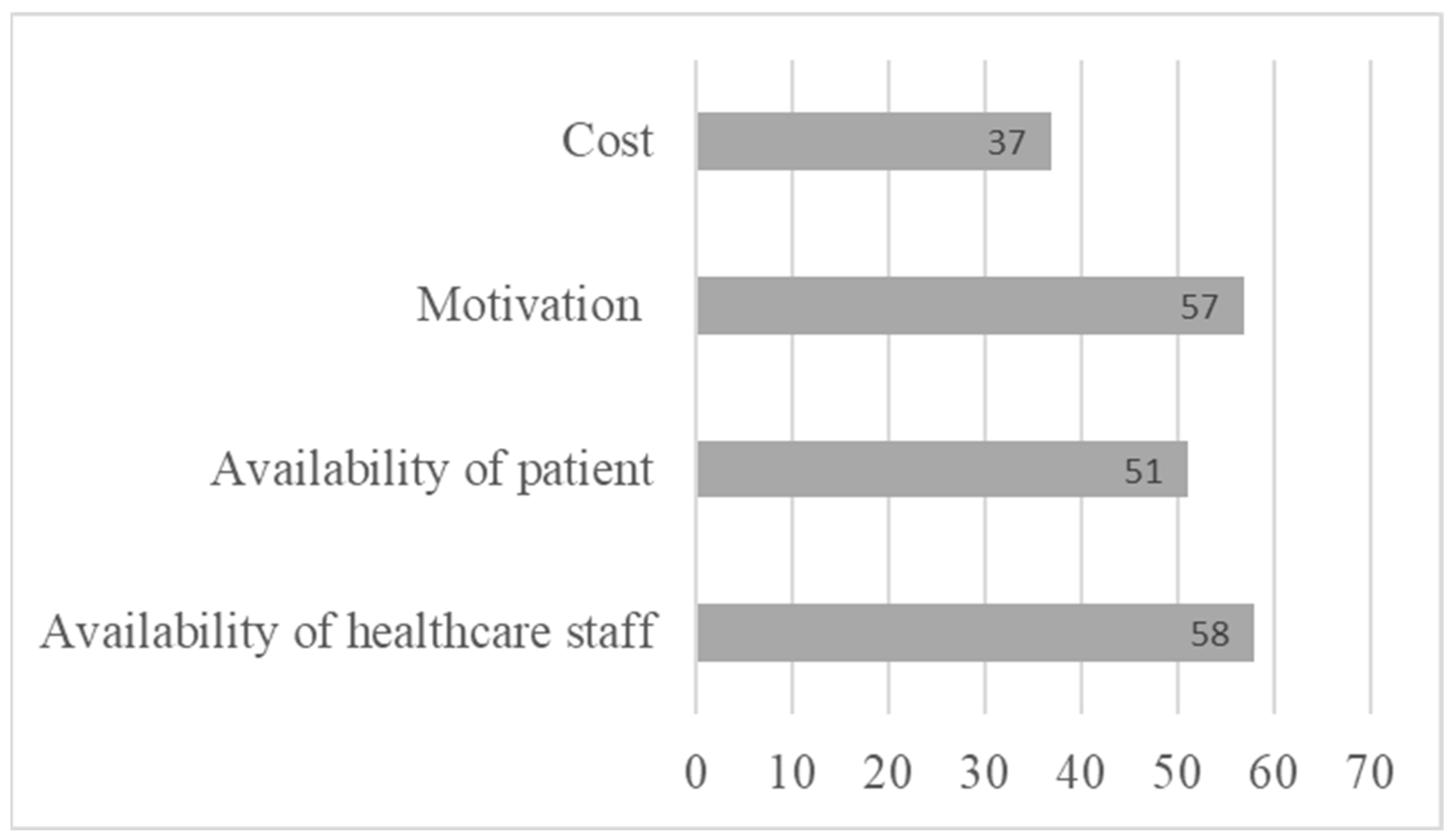
3. Results
4. Discussion
4.1. The Sooner the Better
4.2. Importance of Specific Tools and Their Accessibility
4.3. Importance of Assessing Intrinsic Motivation
4.4. Limitations
4.5. Perspectives for Cognitive Rehabilitation Among pwMSs
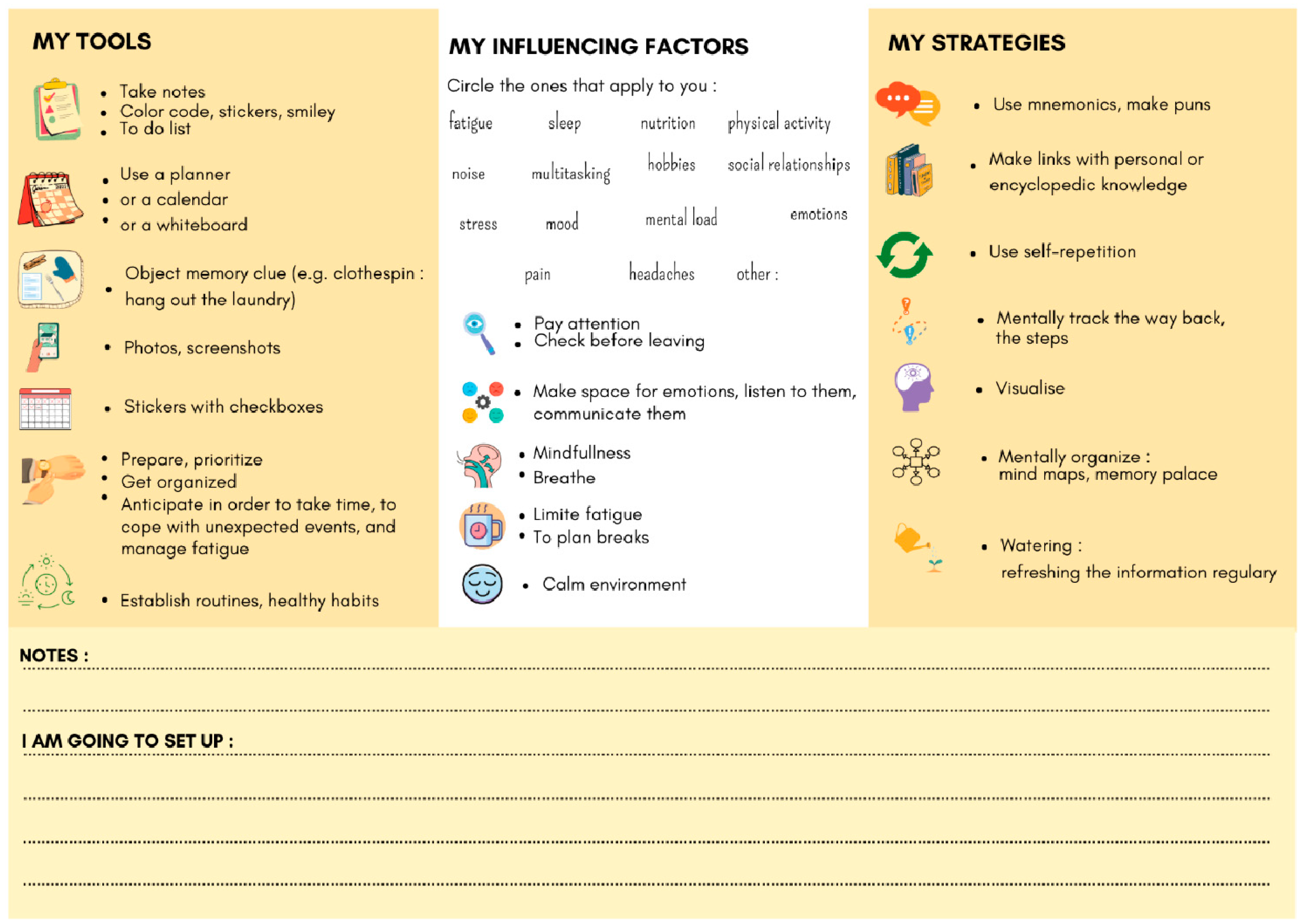
4.6. Guidelines for Cognitive Rehabilitation Among pwMSs Based on This Survey
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Brochet, B.; Ruet, A. Cognitive Impairment in Multiple Sclerosis with Regards to Disease Duration and Clinical Phenotypes. Front. Neurol. 2019, 10, 261. [Google Scholar] [CrossRef] [PubMed]
- Rao, S.M.; Leo, G.J.; Ellington, L.; Nauertz, T.; Bernardin, L.; Unverzagt, F. Cognitive dysfunction in multiple sclerosis. II. Impact on employment and social functioning. Neurology 1991, 41, 692–696. [Google Scholar] [CrossRef]
- Ruano, L.; Portaccio, E.; Goretti, B.; Niccolai, C.; Severo, M.; Patti, F.; Cilia, S.; Gallo, P.; Grossi, P.; Ghezzi, A.; et al. Age and disability drive cognitive impairment in multiple sclerosis across disease subtypes. Mult. Scler. J. 2017, 23, 1258–1267. [Google Scholar] [CrossRef] [PubMed]
- Labiano-Fontcuberta, A.; Mitchell, A.J.; Moreno-García, S.; Benito-León, J. Cognitive impairment in patients with multiple sclerosis predicts worse caregiver’s health-related quality of life. Mult. Scler. J. 2014, 20, 1769–1779. [Google Scholar] [CrossRef]
- Deloire, M.; Bonnet, M.; Salort, E.; Arimone, Y.; Boudineau, M.; Petry, K.; Brochet, B. How to detect cognitive dysfunction at early stages of multiple sclerosis? Mult. Scler. J. 2006, 12, 445–452. [Google Scholar] [CrossRef] [PubMed]
- Ruet, A.; Deloire, M.; Hamel, D.; Ouallet, J.-C.; Petry, K.; Brochet, B. Cognitive impairment, health-related quality of life and vocational status at early stages of multiple sclerosis: A 7-year longitudinal study. J. Neurol. 2013, 260, 776–784. [Google Scholar] [CrossRef]
- Miller, A.; Dishon, S. Health-related quality of life in multiple sclerosis: The impact of disability, gender and employment status. Qual. Life Res. 2006, 15, 259–271. [Google Scholar] [CrossRef]
- van der Hiele, K.; van Gorp, D.A.M.; Heerings, M.A.P.; van Lieshout, I.; Jongen, P.J.; Reneman, M.F.; van der Klink, J.J.L.; Vosman, F.; Middelkoop, H.A.M.; Visser, L.H.; et al. The MS@Work study: A 3-year prospective observational study on factors involved with work participation in patients with relapsing-remitting Multiple Sclerosis. BMC Neurol. 2015, 15, 134. [Google Scholar] [CrossRef]
- Krokavcova, M.; Nagyova, I.; Van Dijk, J.P.; Rosenberger, J.; Gavelova, M.; Middel, B.; Szilasiova, J.; Gdovinova, Z.; Groothoff, J.W. Self-rated health and employment status in patients with multiple sclerosis. Disabil. Rehabil. 2010, 32, 1742–1748. [Google Scholar] [CrossRef]
- Jongen, P.J.; Wesnes, K.; van Geel, B.; Pop, P.; Sanders, E.; Schrijver, H.; Visser, L.H.; Gilhuis, H.J.; Sinnige, L.G.; Brands, A.M.; et al. Relationship between working hours and power of attention, memory, fatigue, depression and self-efficacy one year after diagnosis of clinically isolated syndrome and relapsing remitting multiple sclerosis. PLoS ONE 2014, 9, e96444. [Google Scholar] [CrossRef]
- Langdon, D.W.; Amato, M.P.; Boringa, J.; Brochet, B.; Foley, F.; Fredrikson, S.; Hämäläinen, P.; Hartung, H.-P.; Krupp, L.; Penner, I.K.; et al. Recommendations for a Brief International Cognitive Assessment for Multiple Sclerosis (BICAMS). Mult. Scler. J. 2012, 18, 891–898. [Google Scholar] [CrossRef]
- Maubeuge, N.; Deloire, M.S.A.; Brochet, B.; Ehrlé, N.; Charré-Morin, J.; Saubusse, A.; Ruet, A. French validation of the Brief International Cognitive Assessment for Multiple Sclerosis. Rev. Neurol. 2021, 177, 73–79. [Google Scholar] [CrossRef] [PubMed]
- Jougleux, C.; Joly, H.; Brissard, H.; Lenne, B.; François, S.; Hamelin, F.; Derache, N.; Morin, J.; Reuter, F.; Colamarino, R.; et al. French consensus procedure for neuropsychological assessment in multiple sclerosis. Rev. Neurol. (Paris) 2025, 181, 58–66. [Google Scholar] [CrossRef]
- Benedict, R.H.B.; Amato, M.P.; DeLuca, J.; Geurts, J.J.G. Cognitive impairment in multiple sclerosis: Clinical management, MRI, and therapeutic avenues. Lancet Neurol. 2020, 19, 860–871. [Google Scholar] [CrossRef]
- Chiaravalloti, N.D.; DeLuca, J. Cognitive impairment in multiple sclerosis. Lancet Neurol. 2008, 7, 1139–1151. [Google Scholar] [CrossRef]
- Jakimovski, D.; Bittner, S.; Zivadinov, R.; Morrow, S.A.; Benedict, R.H.; Zipp, F.; Weinstock-Guttman, B. Multiple sclerosis. Lancet 2024, 403, 183–202. [Google Scholar] [CrossRef] [PubMed]
- Kobelt, G.; Thompson, A.; Berg, J.; Gannedahl, M.; Eriksson, J.; MSCOI Study Group; European Multiple Sclerosis Platform. New insights into the burden and costs of multiple sclerosis in Europe. Mult. Scler. J. 2017, 23, 1123–1136. [Google Scholar] [CrossRef]
- Meca-Lallana, V.; Gascón-Giménez, F.; Ginestal-López, R.C.; Higueras, Y.; Téllez-Lara, N.; Carreres-Polo, J.; Eichau-Madueño, S.; Romero-Imbroda, J.; Vidal-Jordana, Á.; Pérez-Miralles, F. Cognitive impairment in multiple sclerosis: Diagnosis and monitoring. Neurol. Sci. 2021, 42, 5183–5193. [Google Scholar] [CrossRef]
- Chen, M.H.; Chiaravalloti, N.D.; DeLuca, J. Neurological update: Cognitive rehabilitation in multiple sclerosis. J. Neurol. 2021, 268, 4908–4914. [Google Scholar] [CrossRef]
- Landmeyer, N.C.; Bürkner, P.-C.; Wiendl, H.; Ruck, T.; Hartung, H.-P.; Holling, H.; Meuth, S.G.; Johnen, A. Disease-modifying treatments and cognition in relapsing-remitting multiple sclerosis: A meta-analysis. Neurology 2020, 94, e2373–e2383. [Google Scholar] [CrossRef]
- Seron, X.; Linden, M.V.d. Traité de Neuropsychologie Clinique de L’adulte: Tome 2—Rééducation, 2nd ed.; DE BOECK SUP: Paris Louvain-la-Neuve (Belgique), France, 2016; 512p. [Google Scholar]
- Sumowski, J.F.; Leavitt, V.M. Cognitive reserve in multiple sclerosis. Mult. Scler. J. 2013, 19, 1122–1127. [Google Scholar] [CrossRef]
- Brissart, H.; Omorou, A.Y.; Forthoffer, N.; Berger, E.; Moreau, T.; De Seze, J.; Morele, E.; Debouverie, M. Memory improvement in multiple sclerosis after an extensive cognitive rehabilitation program in groups with a multicenter double-blind randomized trial. Clin. Rehabil. 2020, 34, 754–763. [Google Scholar] [CrossRef] [PubMed]
- Chiaravalloti, N.D.; Moore, N.B.; Weber, E.; DeLuca, J. The application of Strategy-based Training to Enhance Memory (STEM) in multiple sclerosis: A pilot RCT. Neuropsychol. Rehabil. 2021, 31, 231–254. [Google Scholar] [CrossRef] [PubMed]
- Chiaravalloti, N.D.; Weber, E.; Dobryakova, E.; Botticello, A.; Goverover, Y.; Moore, N.B.; DeLuca, J. Kessler Foundation Strategy-Based Training to Enhance Memory (KF-STEMTM): Study protocol for a single site double-blind randomized, clinical trial in Multiple Sclerosis. Contemp. Clin. Trials Commun. 2022, 30, 101026. [Google Scholar] [CrossRef]
- Blair, M.; Goveas, D.; Safi, A.; Marshall, C.; Rosehart, H.; Orenczuk, S.; Morrow, S.A. Does cognitive training improve attention/working memory in persons with MS? A pilot study using the Cogmed Working Memory Training program. Mult. Scler. Relat. Disord. 2021, 49, 102770. [Google Scholar] [CrossRef] [PubMed]
- Mattioli, F.; Flavia, M.; Stampatori, C.; Zanotti, D.; Parrinello, G.; Capra, R. Efficacy and specificity of intensive cognitive rehabilitation of attention and executive functions in multiple sclerosis. J. Neurol. Sci. 2010, 288, 101–105. [Google Scholar] [CrossRef]
- Vogt, A.; Kappos, L.; Calabrese, P.; Stöcklin, M.; Gschwind, L.; Opwis, K.; Penner, I.-K. Working memory training in patients with multiple sclerosis—comparison of two different training schedules. Restor. Neurol. Neurosci. 2009, 27, 225–235. [Google Scholar] [CrossRef]
- Brandstadter, R.; Fabian, M.; Leavitt, V.M.; Krieger, S.; Yeshokumar, A.; Katz Sand, I.; Klineova, S.; Riley, C.S.; Lewis, C.; Pelle, G.; et al. Word-finding difficulty is a prevalent disease-related deficit in early multiple sclerosis. Mult. Scler. J. 2020, 26, 1752–1764. [Google Scholar] [CrossRef]
- Joly, H.; Cohen, M.; Lebrun, C. Demonstration of a lexical access deficit in relapsing-remitting and secondary progressive forms of multiple sclerosis. Rev. Neurol. 2014, 170, 527–530. [Google Scholar] [CrossRef]
- Mäntynen, A.; Rosti-Otajärvi, E.; Koivisto, K.; Lilja, A.; Huhtala, H.; Hämäläinen, P. Neuropsychological rehabilitation does not improve cognitive performance but reduces perceived cognitive deficits in patients with multiple sclerosis: A randomised, controlled, multi-centre trial. Mult. Scler. J. 2014, 20, 99–107. [Google Scholar] [CrossRef]
- Brissart, H.; Leroy, M.; Morele, E.; Baumann, C.; Spitz, E.; Debouverie, M. Cognitive rehabilitation in multiple sclerosis. Neurocase 2013, 19, 553–565. [Google Scholar] [CrossRef] [PubMed]
- Brochet, B. Cognitive Rehabilitation in Multiple Sclerosis in the Period from 2013 and 2021: A Narrative Review. Brain Sci. 2021, 12, 55. [Google Scholar] [CrossRef]
- das Nair, R.; Ferguson, H.; Stark, D.L.; Lincoln, N.B. Memory Rehabilitation for people with multiple sclerosis. In Cochrane Collaboration; das Nair, R., Ed.; Cochrane Database of Systematic Reviews [Internet]; John Wiley & Sons, Ltd.: Chichester, UK, 2012. [Google Scholar]
- Lamargue, D.; Koubiyr, I.; Deloire, M.; Saubusse, A.; Charre-Morin, J.; Moroso, A.; Coupé, P.; Brochet, B.; Ruet, A. Effect of cognitive rehabilitation on neuropsychological and semiecological testing and on daily cognitive functioning in multiple sclerosis: The REACTIV randomized controlled study. J. Neurol. Sci. 2020, 415, 116929. [Google Scholar] [CrossRef] [PubMed]
- Munger, K.C.; Martinez, A.P.; Hyland, M.H. The impact of cognitive rehabilitation on quality of life in multiple sclerosis: A pilot study. Mult. Scler. J. Exp. Transl. Clin. 2021, 7, 20552173211040239. [Google Scholar] [CrossRef] [PubMed]
- Taylor, L.; Mhizha-Murira, J.; Law, G.; Evangelou, N.; Das Nair, R. Understanding who benefits most from cognitive rehabilitation for multiple sclerosis: A secondary data analysis. Mult. Scler. J. 2023, 29, 1482–1492. [Google Scholar] [CrossRef]
- Chiaravalloti, N.D.; Genova, H.M.; DeLuca, J. Cognitive Rehabilitation in Multiple Sclerosis: The Role of Plasticity. Front. Neurol. 2015, 6, 67. [Google Scholar] [CrossRef]
- Dobryakova, E.; Wylie, G.R.; DeLuca, J.; Chiaravalloti, N.D. A pilot study examining functional brain activity 6 months after memory retraining in MS: The MEMREHAB trial. Brain Imaging Behav. 2014, 8, 403–406. [Google Scholar] [CrossRef]
- Lampit, A.; Heine, J.; Finke, C.; Barnett, M.H.; Valenzuela, M.; Wolf, A.; Leung, I.H.K.; Hill, N.T.M. Computerized Cognitive Training in Multiple Sclerosis: A Systematic Review and Meta-analysis. Neurorehabilit. Neural. Repair. 2019, 33, 695–706. [Google Scholar] [CrossRef]
- Rosti-Otajärvi, E.M.; Hämäläinen, P.I. Neuropsychological rehabilitation for multiple sclerosis. Cochrane Database Syst. Rev. 2011, 2, CD009131. [Google Scholar] [CrossRef]
- Learmonth, Y.C.; Adamson, B.C.; Balto, J.M.; Chiu, C.-Y.; Molina-Guzman, I.M.; Finlayson, M.; Barstow, E.A.; Motl, R.W. Investigating the needs and wants of healthcare providers for promoting exercise in persons with multiple sclerosis: A qualitative study. Disabil. Rehabil. 2018, 40, 2172–2180. [Google Scholar] [CrossRef]
- Flavell, J.H. Metacognition and cognitive monitoring: A new area of cognitive–developmental inquiry. Am. Psychol. 1979, 34, 906–911. [Google Scholar] [CrossRef]
- Mazancieux, A.; Souchay, C.; Casez, O.; Moulin, C.J.A. Metacognition and self-awareness in Multiple Sclerosis. Cortex 2019, 111, 238–255. [Google Scholar] [CrossRef]
- Lebrun, C.; Blanc, F.; Brassat, D.; Zephir, H.; de Seze, J. CFSEP Cognitive function in radiologically isolated syndrome. Mult. Scler. 2010, 16, 919–925. [Google Scholar] [CrossRef] [PubMed]
- Anhoque, C.F.; Domingues, S.C.A.; Teixeira, A.L.; Domingues, R.B. Cognitive impairment in clinically isolated syndrome: A systematic review. Dement. Neuropsychol. 2010, 4, 86–90. [Google Scholar] [CrossRef]
- Brochet, B.; Clavelou, P.; Defer, G.; De Seze, J.; Louapre, C.; Magnin, E.; Ruet, A.; Thomas-Anterion, C.; Vermersch, P. Cognitive Impairment in Secondary Progressive Multiple Sclerosis: Effect of Disease Duration, Age, and Progressive Phenotype. Brain Sci. 2022, 12, 183. [Google Scholar] [CrossRef]
- Benedict, R.H.B.; Munschauer, F.; Linn, R.; Miller, C.; Murphy, E.; Foley, F.; Jacobs, L. Screening for multiple sclerosis cognitive impairment using a self-administered 15-item questionnaire. Mult. Scler. J. 2003, 9, 95–101. [Google Scholar] [CrossRef] [PubMed]
- Benedict, R.H.B.; Zivadinov, R. Predicting neuropsychological abnormalities in multiple sclerosis. J. Neurol. Sci. 2006, 245, 67–72. [Google Scholar] [CrossRef]
- Julian, L.; Merluzzi, N.M.; Mohr, D.C. The relationship among depression, subjective cognitive impairment, and neuropsychological performance in multiple sclerosis. Mult. Scler. J. 2007, 13, 81–86. [Google Scholar] [CrossRef]
- Maor, Y.; Olmer, L.; Mozes, B. The relation between objective and subjective impairment in cognitive function among multiple sclerosis patients-the role of depression. Mult. Scler. J. 2001, 7, 131–135. [Google Scholar]
- Jougleux-Vie, C.; Duhin, E.; Deken, V.; Outteryck, O.; Vermersch, P.; Zéphir, H. Does Fatigue Complaint Reflect Memory Impairment in Multiple Sclerosis? Mult. Scler. Int. 2014, 2014, 692468. [Google Scholar] [CrossRef]
- Carone, D.A.; Benedict, R.H.B.; Munschauer, F.E.; Fishman, I.; Weinstock-Guttman, B. Interpreting patient/informant discrepancies of reported cognitive symptoms in MS. J. Int. Neuropsychol. Soc. 2005, 11, 574–583. [Google Scholar] [CrossRef] [PubMed]
- Weld-Blundell, I.V.; Grech, L.; Learmonth, Y.C.; Marck, C.H. Lifestyle and complementary therapies in multiple sclerosis guidelines: Systematic review. Acta Neurol. Scand. 2022, 145, 379–392. [Google Scholar] [CrossRef]
- Aarts, J.; Saddal, S.R.D.; Bosmans, J.E.; de Groot, V.; de Jong, B.A.; Klein, M.; Ruitenberg, M.F.L.; Schaafsma, F.G.; Schippers, E.C.F.; Schoonheim, M.M.; et al. Don’t be late! Postponing cognitive decline and preventing early unemployment in people with multiple sclerosis: A study protocol. BMC Neurol. 2024, 24, 28. [Google Scholar] [CrossRef] [PubMed]
- Sumowski, J.F.; Benedict, R.; Enzinger, C.; Filippi, M.; Geurts, J.J.; Hamalainen, P.; Hulst, H.; Inglese, M.; Leavitt, V.M.; Rocca, M.A.; et al. Cognition in multiple sclerosis: State of the field and priorities for the future. Neurology 2018, 90, 278–288. [Google Scholar] [CrossRef]
- Schoonheim, M.M.; Meijer, K.A.; Geurts, J.J.G. Network collapse and cognitive impairment in multiple sclerosis. Front. Neurol. 2015, 6, 82. [Google Scholar] [CrossRef] [PubMed]
- Schoonheim, M.M.; Broeders, T.A.A.; Geurts, J.J.G. The network collapse in multiple sclerosis: An overview of novel concepts to address disease dynamics. Neuroimage Clin. 2022, 35, 103108. [Google Scholar] [CrossRef]
- Sumowski, J.F. Cognitive Reserve as a Useful Concept for Early Intervention Research in Multiple Sclerosis. Front. Neurol. 2015, 6, 176. [Google Scholar] [CrossRef]
- Brissart, H.; Leroy, M. ProCog-SEP: Programme de Remédiation Cognitive Chez les Personnes Atteintes de Sclérose En Plaques et en Réduire L’impact au Quotidien; Independently Published: Chicago, IL, USA, 2020; 168p. [Google Scholar]
- Brissart, H.; Morèle, E.; Perf, M.L.; Leininger, M. Manag’mind: Un Matériel Modulable Pour la Prise en Charge Cognitive de la Mémoire de Travail, 1st ed.; DE BOECK SUP: Paris Louvain-la-Neuve (Belgique), France, 2018; 136 p. [Google Scholar]
- Gaspari, M.; Zini, F.; Stecchi, S. Enhancing cognitive rehabilitation in multiple sclerosis with a disease-specific tool. Disabil. Rehabil. Assist. Technol. 2023, 18, 1–14. [Google Scholar] [CrossRef]
- Bove, R.; Rowles, W.; Zhao, C.; Anderson, A.; Friedman, S.; Langdon, D.; Alexander, A.; Sacco, S.; Henry, R.; Gazzaley, A.; et al. A novel in-home digital treatment to improve processing speed in people with multiple sclerosis: A pilot study. Mult. Scler. J. 2021, 27, 778–789. [Google Scholar] [CrossRef]
- De Luca, R.; Russo, M.; Gasparini, S.; Leonardi, S.; Foti Cuzzola, M.; Sciarrone, F.; Zichittella, C.; Sessa, E.; Maggio, M.G.; De Cola, M.C.; et al. Do people with multiple sclerosis benefit from PC-based neurorehabilitation? A pilot study. Appl. Neuropsychol. Adult 2021, 28, 427–435. [Google Scholar] [CrossRef]
- Harand, C.; Daniel, F.; Mondou, A.; Chevanne, D.; Creveuil, C.; Defer, G. Neuropsychological management of multiple sclerosis: Evaluation of a supervised and customized cognitive rehabilitation program for self-used at home (SEPIA): Protocol for a randomized controlled trial. Trials 2019, 20, 614. [Google Scholar] [CrossRef] [PubMed]
- Baetge, S.J.; Filser, M.; Renner, A.; Raithel, L.M.; Lau, S.; Pöttgen, J.; Penner, I.-K. Supporting brain health in multiple sclerosis: Exploring the potential of neuroeducation combined with practical mindfulness exercises in the management of neuropsychological symptoms. J. Neurol. 2023, 270, 3058–3071. [Google Scholar] [CrossRef] [PubMed]
- Manera, V.; Ben-Sadoun, G.; Aalbers, T.; Agopyan, H.; Askenazy, F.; Benoit, M.; Bensamoun, D.; Bourgeois, J.; Bredin, J.; Bremond, F.; et al. Recommendations for the Use of Serious Games in Neurodegenerative Disorders: 2016 Delphi Panel. Front. Psychol. 2017, 8, 1243. [Google Scholar] [CrossRef]
- Maggio, M.G.; Russo, M.; Cuzzola, M.F.; Destro, M.; La Rosa, G.; Molonia, F.; Bramanti, P.; Lombardo, G.; De Luca, R.; Calabrò, R.S. Virtual reality in multiple sclerosis rehabilitation: A review on cognitive and motor outcomes. J. Clin. Neurosci. 2019, 65, 106–111. [Google Scholar] [CrossRef] [PubMed]
- Ruet, A.; Brochet, B. Cognitive assessment in patients with multiple sclerosis: From neuropsychological batteries to ecological tools. Ann. Phys. Rehabil. Med. 2018, 63, 154–158. [Google Scholar] [CrossRef]
- Zyda, M. From visual simulation to virtual reality to games. Computer 2005, 38, 25–32. [Google Scholar] [CrossRef]
- Bove, R.M.; Rush, G.; Zhao, C.; Rowles, W.; Garcha, P.; Morrissey, J.; Schembri, A.; Alailima, T.; Langdon, D.; Possin, K.; et al. A Videogame-Based Digital Therapeutic to Improve Processing Speed in People with Multiple Sclerosis: A Feasibility Study. Neurol. Ther. 2019, 8, 135–145. [Google Scholar] [CrossRef]
- William, R. Miller Motivational Interviewing, Fourth Edition: Helping People Change and Grow, 4th ed.; The Guilford Press: New York, NY, USA, 2023; 338p. [Google Scholar]
- Arkowitz, H.; Miller, W.R.; Rollnick, S. Motivational Interviewing in the Treatment of Psychological Problems, 2nd ed.; The Guilford Press: New York, NY, USA, 2015; 400p. [Google Scholar]
- Easthall, C.; Song, F.; Bhattacharya, D. A meta-analysis of cognitive-based behaviour change techniques as interventions to improve medication adherence. BMJ Open 2013, 3, e002749. [Google Scholar] [CrossRef]
- Norcross, J.C.; Wampold, B.E. A new therapy for each patient: Evidence-based relationships and responsiveness. J. Clin. Psychol. 2018, 74, 1889–1906. [Google Scholar] [CrossRef]
- Haynes, R.B.; Devereaux, P.J.; Guyatt, G.H. Clinical expertise in the era of evidence-based medicine and patient choice. BMJ Evid. Based Med. 2002, 7, 36–38. [Google Scholar] [CrossRef]
- Hoffmann, T.; Bennett, S.; Del Mar, C. Evidence-Based Practice Across the Health Professions, 3rd ed.; Elsevier: Chatswood, NSW, Australia, 2017; 470p. [Google Scholar]
- Barbarulo, A.M.; Lus, G.; Signoriello, E.; Trojano, L.; Grossi, D.; Esposito, M.; Costabile, T.; Lanzillo, R.; Saccà, F.; Morra, V.B.; et al. Integrated Cognitive and Neuromotor Rehabilitation in Multiple Sclerosis: A Pragmatic Study. Front. Behav. Neurosci. 2018, 12. [Google Scholar] [CrossRef] [PubMed]
- On behalf of the CogEx Research Team; Feinstein, A.; Amato, M.P.; Brichetto, G.; Chataway, J.; Chiaravalloti, N.; Dalgas, U.; DeLuca, J.; Feys, P.; Filippi, M.; et al. Study protocol: Improving cognition in people with progressive multiple sclerosis: A multi-arm, randomized, blinded, sham-controlled trial of cognitive rehabilitation and aerobic exercise (COGEx). BMC Neurol. 2020, 20, 204. [Google Scholar] [CrossRef] [PubMed]
- Kalb, R.; Beier, M.; Benedict, R.H.; Charvet, L.; Costello, K.; Feinstein, A.; Gingold, J.; Goverover, Y.; Halper, J.; Harris, C.; et al. Recommendations for cognitive screening and management in multiple sclerosis care. Mult. Scler. J. 2018, 24, 1665–1680. [Google Scholar] [CrossRef] [PubMed]
- Wills, O.; Brischetto, D.; Zoszak, K.; Allogmanny, S.; McMahon, A.-T.; Haartsen, J.; Probst, Y. Establishing consensus on lifestyle recommendations and behaviour change strategies to promote brain health-focussed care for multiple sclerosis: A modified e-Delphi study. Mult. Scler. Relat. Disord. 2024, 92, 105949. [Google Scholar] [CrossRef]
- Wills, O.; Probst, Y. Towards new perspectives: A scoping review and meta-synthesis to redefine brain health for multiple sclerosis. Eur. J. Neurol. 2024, 31, e16210. [Google Scholar] [CrossRef]
- Bassetti, C.L.A.; Endres, M.; Sander, A.; Crean, M.; Subramaniam, S.; Carvalho, V.; Di Liberto, G.; Franco, O.H.; Pijnenburg, Y.; Leonardi, M.; et al. The European Academy of Neurology Brain Health Strategy: One brain, one life, one approach. Eur. J. Neurol. 2022, 29, 2559–2566. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brissart, H.; Joly, H.; Castro, C.; Lenne, B. A Healthcare Providers’ Survey for the Cognitive Rehabilitation of Multiple Sclerosis in France: From Research to Real Life. Sclerosis 2025, 3, 14. https://doi.org/10.3390/sclerosis3020014
Brissart H, Joly H, Castro C, Lenne B. A Healthcare Providers’ Survey for the Cognitive Rehabilitation of Multiple Sclerosis in France: From Research to Real Life. Sclerosis. 2025; 3(2):14. https://doi.org/10.3390/sclerosis3020014
Chicago/Turabian StyleBrissart, Hélène, Héloïse Joly, Clémentine Castro, and Bruno Lenne. 2025. "A Healthcare Providers’ Survey for the Cognitive Rehabilitation of Multiple Sclerosis in France: From Research to Real Life" Sclerosis 3, no. 2: 14. https://doi.org/10.3390/sclerosis3020014
APA StyleBrissart, H., Joly, H., Castro, C., & Lenne, B. (2025). A Healthcare Providers’ Survey for the Cognitive Rehabilitation of Multiple Sclerosis in France: From Research to Real Life. Sclerosis, 3(2), 14. https://doi.org/10.3390/sclerosis3020014





