Nose-to Brain Delivery of Resveratrol, a Non-Invasive Method for the Treatment of Cerebral Ischemia
Abstract
1. Introduction
2. Resveratrol’s Protective Effect in Cerebral Ischemia
3. Resveratrol Bioavailability
4. Resveratrol Delivery to the Brain
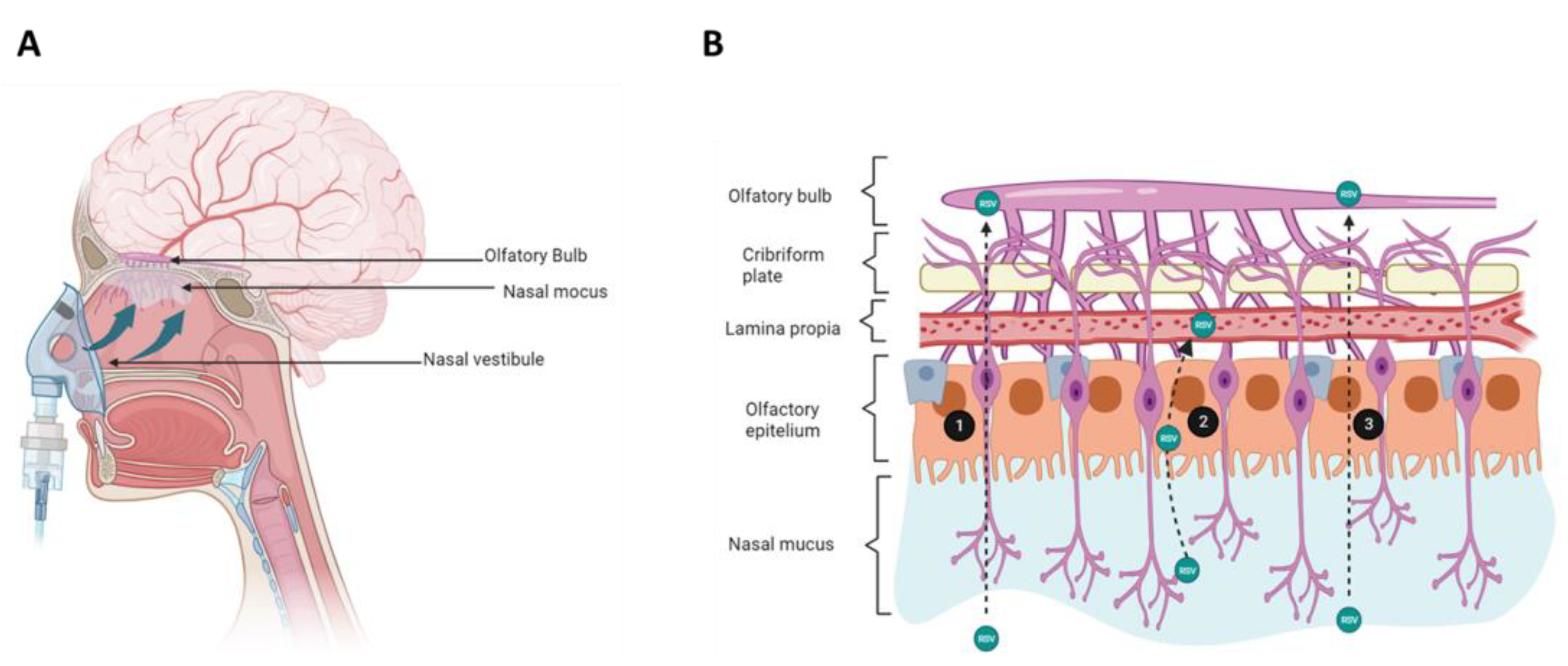
5. Nose Structure and Functions
6. The Intranasal Route of Administration
7. Formulations for the Release of Resveratrol to the Brain
7.1. Nose to Brain Delivery of Resveratrol Formulations
| Drug Delivery Nanosystem | Structural Characteristics | Drug Encapsulation Efficiency (%) | Spherical Shape (nm) | Observations | Reference |
|---|---|---|---|---|---|
| Vesicles | |||||
| NIOSOMES Formed by an aqueous core enclosed within a non-ionic surfactant bilayer. | Gelot 64 (SF) oleic or linoleic acids (ST) | Resveratrol 35 ± 2 | 299–402 | Ex vivo skin permeation experiments indicated that niosomes prepared with the ethanol injection are more effective. | [63] |
| Span 60 (SF) Dodecanol (ST) | Resveratrol 64 ± 8 | 168 ± 4 | Niosomes exhibited a small mean size, narrow size distribution, high entrapment efficiency, and good stability | [64] | |
| Maisine 35–1 (SF) Dodecanol (ST) | Resveratrol 53 ± 8 | 175 ± 13 | Niosomes exhibited a small mean size, narrow size distribution, high encapsulation efficiency and good stability | [64] | |
| Span 60 (SF) Cetyl alcoho (ST) | Resveratrol 81 ± 2 | 108 ± 3 | Nanoencapsulation of resveratrol using non-ionic surfactant and fatty alcohol dramatically improved its solubility and functionality | [65] | |
| LIPOSOMES Formed by phospholipids, which can include several other constituents like cholesterol to improve the stability of the bilayer. | OramixTM CG110 (SF) LauroglycolTM FCC (SF) Soybean phosphatidylcholine (ST) Oleico acid (ST) | Resveratrol >70 | 90 | Toxicity of the vesicular formulations evaluated in vitro, showed no alteration on cell viability after incubation with RSV loaded vesicles. | [66] |
| Soybean lecithin (ST) Oleico acid (ST) N-succinyl chitosan as protective shell of liposomes | Resveratrol and Quercetin 70 ± 5 | 82 ± 3 | The succinyl-chitosan shell increased physical stability of the vesicular system and release of the polyphenols to a greater extent at pH 7.0 (mimicking the intestinal environment). | [67] | |
| Tri-block polymer L64 D-α-tocopheryl polyethylene glycol 1000 succinate (SF) Phospholipon 90G (ST) | Resveratrol 95 | 86 ± 3 | Biocompatibility was demonstrated in an ex vivo model of hemolysis in human erythrocytes. Liposomes maintained the antioxidant properties of resveratrol. | [16] | |
| Emulsions | |||||
| SIMPLE EMULSIONS Formed by emulsifiers dispersed in oil, and water. | Soybean oil (OP) Soy lecithinas (SF) Labrasol (ST) | Resveratrol 92.5 ± 2.2 | 132 ± 9 | The improved oral bioavailability of resveratrol was attributable to the inhibition of intestinal glucuronidation by the presence of labrasol. | [68] |
| Labrafac (OP) Cremophor® 40 (SF) Hyaluronic acid (SF) | Resveratrol and curcumin N. A | 115.2 ± 0.2 | The mucoadhesive nanoemulsion was safe to nasal mucosa and increase amount of both polypehnols in the brain. | [69] | |
| Soybean phospholipiddipropylene glycol (OP) 2-hydroxypropyl-β-cyclodextrin (SF) Phosphatidyl choline 60 (SF) | Resveratrol N. A | 122 ± 08 | Nanoformulation presented good compatibility and skin permeation. | [70] | |
| Olive oil (OP) Polyethylenglycol Pluronic® P105 (SF) Cremophor® EL (SF) | Resveratrol N. A | 155 ± 33 | Perfluoropolyether was used as a nano emulsion tracer. Resveratrol-loaded nano emulsions was internalized by macrophages | [71] | |
| Capryol™ 90 (OP) Cremophor® EL (SF) Tween 20 (SF) | Resveratrol N. A | 41.3 ± 4 | The formulation increased oral bioavailability 3.2-fold compared to resveratrol alone. Anti-fatigue properties of resveratrol were improved. | [72] | |
| Labrafil (OP) Gelucire® 44–14 (SF) Labrasol (SF) | Resveratrol N. A | 21 ± 5 | Nanoemulsions significantly increased intestinal permeation across rat jejunum. | [73] | |
| Labrafil (OP) Miglyol® 812 (SF) Tween 80 (SF) | Resveratrol N. A | 103 ± 14 | Nanoemulsion significantly increased intestinal permeation across rat jejunum. | [73] | |
| Labrafil (OP) Labrasol (SF) Cremophor RH 40 (SF) | Resveratrol N. A | 26 ± 1 | Formulation components inhibited the UDP-glucuronosyltransferase and consequently increases the bioavailability of resveratrol. | [74] | |
| Miglyol® 812 (OP) orange oil (OP) Quinoa starch particles (SF) Octenyl succinic anhydride (SF) | Resveratrol 98 ± 2 | 50,000 | Appropriate resveratrol carrier system for use in oral formulations. | [75] | |
| Miglyol® 812 (OP) orange oil (OP) Quinoa starch particles (SF) Tween 20 (SF) | Resveratrol 63 ± 1 | 50,000 | Appropriate resveratrol carrier system for use in oral formulations. | [75] | |
| Olive oil (OP) Sodium lignin sulfonate (SF) Tween 80 (SF) PEG-400 (SF) | Resveratrol N. A | 119 ± 5 | Excellent biocompatibility, improved solubility, and showed antiradical efficiency compared to free trans-RSV | [76] | |
| MULTIPLE EMULSIONS Formed by multiple emulsions of water-in-oil-in-water. | Medium-chain Triacylglycerols (OP) Tween 80 (SF) For double layer nanoemulsions: chitosan, alginate or β-cyclodextrin | Resveratrol N. A | 27 ± 55 | The stability of resveratrol in the double-layer nanoemulsions complexed with chitosan or β-cyclodextrin was higher, compared with single-layer nanoemulsions. | [77] |
| Miglyol® 812 (OP) The inner aqueous phase: ethanol, RSV, and 0.1 M NaCl solution The external aqueous phase: carboxymethylcellulose, Tween 20, and 0.1 M NaCl. | Resveratrol 55 | 59,800 ± 0.002 | High encapsulation efficiency and slow storage release. | [78] | |
| Single-layer emulsion: lactoferrin Multilayer emulsion: lactoferrin/alginate lactoferrin/alginate/ε-poly-L-lysine | Resveratrol N. A | 249 | The antioxidant activity of resveratrol-loaded emulsion did not significantly change during storage, whereas it decreased in nonencapsulated resveratrol oil from the third week onwards. | [79] | |
| The single layer: ethanol/water RSV solution Miglyol 812 Polyglycerol polyricinoleate (ST) Multilayer emulsion: Tween 20 solution with and without sodium carboximethylcellulose as thickening agent. | Resveratrol 77.50 | 10,000–30,000 | The emulsion showed high encapsulation efficiency, good storage stability, shear-thinning behavior, and dominant elastic character. These double emulsions may be suitable for food applications. | [80] | |
| Particles | |||||
| LIPIDIC NANOPARTICLES Formed by a solid hydrophobic core stabilized by a hydrophilic layer of surfactant molecules or polymers. | Tristearin (OP) Chitosan (ST) Hydrogenated phosphatidylcholine (SF) | Resveratrol 67 | 6000 | The cream containing the chitosan-coated lipidic nano particles produced a significant enhancement in the in vivo permeation of resveratrol | [81] |
| Formulation | Components | Physical Characteristics | EE (%) PDI ZP (mV) | Observations | Reference |
|---|---|---|---|---|---|
| Vitamin E nanoemulsion | Vitamin E:sefsol (1:1) (ST) Tween 80 (SF) Transcutol P (co-SF) | Transparent and monophasic. Spherical globules (102 ± 1.46 nm). | N.D. 0.158 ± 0.02 −35 ± 0.02 | Histological studies showed decreased degenerative changes | [82] |
| F6SPION/W3 SPION-loaded with chitosan coated bilosomes | Cholesterol:sorbitan monosterate (Span 60) (1:1), sodium deoxycholate (10 mg), glycerin. Chitosan (0.1%). SPION (magnetite, Fe3O4, 10.3 mg/mL). Waffers: sodium alginate: poly vinyl pyrrolidone K-25 (1:2) + glycerol (10%). | Black spheres surrounded by a layer of less intense black color (chitosan coating layer). Porosity 88% (243 ± 1.87 nm). | 85 ± 1.08 0.14 ± 0.06 35 ± 2.05 | Resveratrol (20 mg/Kg/day, i.n.) improved induced memory and cognitive functions in mice with induced Alzheimer model with lipopolysaccharide. | [83] |
| Cubosomal in situ nasal gel | 4% w/v glicerol monooleate and 1.5% Lutrol F127. 12% w/v Poloxamer 407 (cubosomal gel, permeation enhancer) | Cubical in shape, uniform with smooth surface (161.5 ± 0.12 nm). | 83.08 ± 0.21 0.279 ± 0.15 −20.9 ± 0.11 | The formulation showed higher trans-nasal permeation and brain’s distribution compared to resveratrol solution. | [84] |
| Transferosomes capped with gold nanoparticles [gold (III) chloride HauCl4] | Soy lecithin (glycerophopholipids), ethanol (permeation enhancers), and Cremophor RH 40 (SF) in a ratio of 46.7:20:33.3 (w/w%). | Gold- nanoparticles (GNP), resveratrol-transferosomes-GNP, and resveratrol-nanoemulsion-GNP showed uniform spherical shape with size of 10.30 + 2.4, 94.93 + 5.6, and 20.36 + 4.3 nm | 69.53 ± 3.82 0.194 ± 0.08 −28.7 ± 4.7 | Transferosomes penetrated through nasal mucosal layers. Resveratrol-trans-GNP gel enhanced the spatial memory recovery in amnesic rats compared to i.n. pure resveratrol. | [85] |
| Nanoemulsion capped with gold nanoparticles [gold (III) chloride HAuCl4] | Capryol 90 (ST) Tween 20 (SF), and transcutol (co-SF) at a ratio of 30:60:10 v/v%. | 95.72 ± 5.34 0.26 ± 0.04 −18 ± 2.6 | |||
| Nonoestructured lipid carrier loaded in a situ gel | Cetyl palmitate (solid lipid), Capmul MCM (ST) 1:1 ratio. Acrysol (nonionic, solvent-free and hydrophobically modified ethylene). Poloxamer 188 (SF), Tween 80 (SF). Gellan gum 0.5% and xanthan gum 0.15% (in situ gel formulation) | 132 ± 11.9 nm | 74.05 ± 11.40 0.209 ± 0.005 −23 ± 3.79 | The scopolamine-induced amnesia was reduced with the optimized formulation. | [86] |
| Chitosan-coated lipid microparticles | Phosphatidylcholine (SF) 1.75%, w/v, Stearic acid (ST) Chitosan (bioadhesive excipient) | 68.5 ± 3.1 µm | N.D. N.D. −12.7 ± 2.1 | Resveratrol was found in the rat cerebrospinal fluid with no distribution in blood after nasal administration. | [87] |
| 76.3 ± 5.2 µm | 76.50% N.D. 24.0 ± 4.7 | ||||
| 84.5 ± 8.1 µm | 81.00% N.D. 44.6 ± 3.1 | ||||
| Ionic-sensitive in situ gel loaded with resveratrol nanosuspensions | 0.6% w/v gellan gum | Spherical shape in gellan gum matrix and dispersed uniformly without adhesions. | N.D. 0.234 −8.8 | The increase in the bioavailability of resveratrol in the brain showed in the pharmacokinetics studies suggested the direct nose-to brain delivery. | [88] |
| Nanosized transferosome based intranasal in situ gel | Transferosome Soya lecithin/PE (ratio 7:3) + (Cremophor RH 40 (SF) Gel: Poloxamer 407 (18%) and Carbopol 934 (0.4%) | Spherical shape (83.79 ± 2.54 nm) | 72.58 ± 4.51% N.D. N.D. | Resveratrol bioavailability was enhanced through the nasal route of administration. | [89] |
| Hyaluronic acid based lipidic nanoemulsion | Labrafac Lipophile/cremophor 40 10% (SF); hyaluronic acid 1.5% w/v | Spherical morphology and nanometer size (115 ± 0.15 nm). | N.D. 0.235 ± 0.01 −23.9 ±1.7 | The pharmacokinetic analysis showed that the intranasally administered mucoadhesive formula allowed the absorption of resveratrol and curcumin reaching the brain. | [69] |
7.1.1. Lipid Microparticles
7.1.2. Transferosomes
7.1.3. Bilosomes
7.1.4. Cubosomes
7.1.5. Nanoemulsions
7.1.6. Nanostructured Lipid Carriers (NLC)
7.1.7. Nanosuspensions
7.1.8. Cell Penetrating Peptides
8. Disadvantages of the Nanocarriers Systems
9. Future Directions
10. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Burns, J.; Yokota, T.; Ashihara, H.; Lean, M.E.J.; Crozier, A. Plant Foods and Herbal Sources of Resveratrol. J. Agric. Food Chem. 2002, 50, 3337–3340. [Google Scholar] [CrossRef] [PubMed]
- Thapa, S.B.; Pandey, R.P.; Il Park, Y.; Sohng, J.K. Biotechnological Advances in Resveratrol Production and Its Chemical Diversity. Molecules 2019, 24, 2571. [Google Scholar] [CrossRef]
- Donkor, E.S. Stroke in the 21st Century: A Snapshot of the Burden, Epidemiology, and Quality of Life. Stroke Res. Treat. 2018, 2018, 3238165. [Google Scholar] [CrossRef] [PubMed]
- Marko, M.; Posekany, A.; Szabo, S.; Scharer, S.; Kiechl, S.; Knoflach, M.; Serles, W.; Ferrari, J.; Lang, W.; Sommer, P.; et al. Trends of R-TPA (Recombinant Tissue-Type Plasminogen Activator) Treatment and Treatment-Influencing Factors in Acute Ischemic Stroke. Stroke 2020, 51, 1240–1247. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.; Tuo, Q.-Z.; Lei, P. Iron, Ferroptosis, and Ischemic Stroke. J. Neurochem. 2023, 165, 487–520. [Google Scholar] [CrossRef]
- Neves, D.; Salazar, I.L.; Almeida, R.D.; Silva, R.M. Molecular Mechanisms of Ischemia and Glutamate Excitotoxicity. Life Sci. 2023, 328, 121814. [Google Scholar] [CrossRef] [PubMed]
- Zhou, H.-Q.; Zhang, L.-M.; Li, X.; Huang, Z.-H. Crosstalk between Autophagy and Inflammation in Chronic Cerebral Ischaemia. Cell. Mol. Neurobiol. 2023, 43, 2557–2566. [Google Scholar] [CrossRef]
- Yousufuddin, M.; Young, N. Aging and Ischemic Stroke. Aging 2019, 11, 2542–2544. [Google Scholar] [CrossRef]
- Yang, A.C.; Stevens, M.Y.; Chen, M.B.; Lee, D.P.; Stähli, D.; Gate, D.; Contrepois, K.; Chen, W.; Iram, T.; Zhang, L.; et al. Physiological Blood-Brain Transport Is Impaired with Age by a Shift in Transcytosis. Nature 2020, 583, 425–430. [Google Scholar] [CrossRef]
- Do, T.M.; Dodacki, A.; Alata, W.; Calon, F.; Nicolic, S.; Scherrmann, J.-M.; Farinotti, R.; Bourasset, F. Age-Dependent Regulation of the Blood-Brain Barrier Influx/Efflux Equilibrium of Amyloid-β Peptide in a Mouse Model of Alzheimer’s Disease (3xTg-AD). J. Alzheimers. Dis. 2016, 49, 287–300. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; He, J.; Huang, Y.; Hu, Z. Resveratrol Has an Overall Neuroprotective Role in Ischemic Stroke: A Meta-Analysis in Rodents. Front. Pharmacol. 2021, 12, 795409. [Google Scholar] [CrossRef] [PubMed]
- Pineda-Ramírez, N.; Gutiérrez Aguilar, G.F.; Espinoza-Rojo, M.; Aguilera, P. Current Evidence for AMPK Activation Involvement on Resveratrol-Induced Neuroprotection in Cerebral Ischemia. Nutr. Neurosci. 2018, 21, 229–247. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Yu, Q.; Wu, M. Antioxidant and Neuroprotective Actions of Resveratrol in Cerebrovascular Diseases. Front. Pharmacol. 2022, 13, 948889. [Google Scholar] [CrossRef]
- Abdelsalam, S.A.; Renu, K.; Zahra, H.A.; Abdallah, B.M.; Ali, E.M.; Veeraraghavan, V.P.; Sivalingam, K.; Ronsard, L.; Ben Ammar, R.; Vidya, D.S.; et al. Polyphenols Mediate Neuroprotection in Cerebral Ischemic Stroke-An Update. Nutrients 2023, 15, 1107. [Google Scholar] [CrossRef] [PubMed]
- Ramírez-Garza, S.L.; Laveriano-Santos, E.P.; Marhuenda-Muñoz, M.; Storniolo, C.E.; Tresserra-Rimbau, A.; Vallverdú-Queralt, A.; Lamuela-Raventós, R.M. Health Effects of Resveratrol: Results from Human Intervention Trials. Nutrients 2018, 10, 1892. [Google Scholar] [CrossRef] [PubMed]
- Caddeo, C.; Pucci, L.; Gabriele, M.; Carbone, C.; Fernàndez-Busquets, X.; Valenti, D.; Pons, R.; Vassallo, A.; Fadda, A.M.; Manconi, M. Stability, Biocompatibility and Antioxidant Activity of PEG-Modified Liposomes Containing Resveratrol. Int. J. Pharm. 2018, 538, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Robinson, K.; Mock, C.; Liang, D. Pre-Formulation Studies of Resveratrol. Drug Dev. Ind. Pharm. 2015, 41, 1464–1469. [Google Scholar] [CrossRef] [PubMed]
- Walle, T.; Hsieh, F.; DeLegge, M.H.; Oatis, J.E.J.; Walle, U.K. High Absorption but Very Low Bioavailability of Oral Resveratrol in Humans. Drug Metab. Dispos. 2004, 32, 1377–1382. [Google Scholar] [CrossRef]
- Boocock, D.J.; Faust, G.E.S.; Patel, K.R.; Schinas, A.M.; Brown, V.A.; Ducharme, M.P.; Booth, T.D.; Crowell, J.A.; Perloff, M.; Gescher, A.J.; et al. Phase I Dose Escalation Pharmacokinetic Study in Healthy Volunteers of Resveratrol, a Potential Cancer Chemopreventive Agent. Cancer Epidemiol. Biomark. Prev. 2007, 16, 1246–1252. [Google Scholar] [CrossRef]
- Wang, Q.; Xu, J.; Rottinghaus, G.E.; Simonyi, A.; Lubahn, D.; Sun, G.Y.; Sun, A.Y. Resveratrol Protects against Global Cerebral Ischemic Injury in Gerbils. Brain Res. 2002, 958, 439–447. [Google Scholar] [CrossRef]
- Turner, R.S.; Thomas, R.G.; Craft, S.; Van Dyck, C.H.; Mintzer, J.; Reynolds, B.A.; Brewer, J.B.; Rissman, R.A.; Raman, R.; Aisen, P.S. A Randomized, Double-Blind, Placebo-Controlled Trial of Resveratrol for Alzheimer Disease. Neurology 2015, 85, 1383–1391. [Google Scholar] [CrossRef] [PubMed]
- Abbott, N.J.; Patabendige, A.A.K.; Dolman, D.E.M.; Yusof, S.R.; Begley, D.J. Structure and Function of the Blood-Brain Barrier. Neurobiol. Dis. 2010, 37, 13–25. [Google Scholar] [CrossRef] [PubMed]
- Azarmi, M.; Maleki, H.; Nikkam, N.; Malekinejad, H. Transcellular Brain Drug Delivery: A Review on Recent Advancements. Int. J. Pharm. 2020, 586, 119582. [Google Scholar] [CrossRef]
- Taylor, N.M.I.; Manolaridis, I.; Jackson, S.M.; Kowal, J.; Stahlberg, H.; Locher, K.P. Structure of the Human Multidrug Transporter ABCG2. Nature 2017, 546, 504–509. [Google Scholar] [CrossRef]
- Arvanitis, C.D.; Ferraro, G.B.; Jain, R.K. The Blood-Brain Barrier and Blood-Tumour Barrier in Brain Tumours and Metastases. Nat. Rev. Cancer 2020, 20, 26–41. [Google Scholar] [CrossRef]
- Begley, D.J. ABC Transporters and the Blood-Brain Barrier. Curr. Pharm. Des. 2004, 10, 1295–1312. [Google Scholar] [CrossRef]
- Engdahl, E.; van Schijndel, M.D.M.; Voulgaris, D.; Di Criscio, M.; Ramsbottom, K.A.; Rigden, D.J.; Herland, A.; Rüegg, J. Bisphenol A Inhibits the Transporter Function of the Blood-Brain Barrier by Directly Interacting with the ABC Transporter Breast Cancer Resistance Protein (BCRP). Int. J. Mol. Sci. 2021, 22, 5534. [Google Scholar] [CrossRef] [PubMed]
- Álvarez, A.I.; Vallejo, F.; Barrera, B.; Merino, G.; Prieto, J.G.; Tomás-Barberán, F.; Espín, J.C. Bioavailability of the Glucuronide and Sulfate Conjugates of Genistein and Daidzein in Breast Cancer Resistance Protein 1 Knockout Mice. Drug Metab. Dispos. 2011, 39, 2008–2012. [Google Scholar] [CrossRef] [PubMed]
- Duarte, A.C.; Rosado, T.; Costa, A.R.; Santos, J.; Gallardo, E.; Quintela, T.; Ishikawa, H.; Schwerk, C.; Schroten, H.; Gonçalves, I.; et al. The Bitter Taste Receptor TAS2R14 Regulates Resveratrol Transport across the Human Blood-Cerebrospinal Fluid Barrier. Biochem. Pharmacol. 2020, 177, 113953. [Google Scholar] [CrossRef]
- Halwachs, S.; Lakoma, C.; Schäfer, I.; Seibel, P.; Honscha, W. The Antiepileptic Drugs Phenobarbital and Carbamazepine Reduce Transport of Methotrexate in Rat Choroid Plexus by Down-Regulation of the Reduced Folate Carrier. Mol. Pharmacol. 2011, 80, 621–629. [Google Scholar] [CrossRef]
- Roberts, L.M.; Black, D.S.; Raman, C.; Woodford, K.; Zhou, M.; Haggerty, J.E.; Yan, A.T.; Cwirla, S.E.; Grindstaff, K.K. Subcellular Localization of Transporters along the Rat Blood-Brain Barrier and Blood-Cerebral-Spinal Fluid Barrier by in Vivo Biotinylation. Neuroscience 2008, 155, 423–438. [Google Scholar] [CrossRef]
- Grube, M.; Hagen, P.; Jedlitschky, G. Neurosteroid Transport in the Brain: Role of ABC and SLC Transporters. Front. Pharmacol. 2018, 9, 354. [Google Scholar] [CrossRef]
- Basseville, A.; Hall, M.D.; Chau, C.H.; Robey, R.W.; Gottesman, M.; Figg, W.D.; Bates, S.E. The ABCG2 Multidrug Transporter. In ABC Transporters—40 Years on; Springer: Berlin/Heidelberg, Germany, 2016; pp. 195–226. [Google Scholar]
- Cooray, H.C.; Blackmore, C.G.; Maskell, L.; Barrand, M.A. Localisation of Breast Cancer Resistance Protein in Microvessel Endothelium of Human Brain. Neuroreport 2002, 13, 2059–2063. [Google Scholar] [CrossRef]
- Sobiesk, J.; Munakomi, S. Anatomy, Head and Neck, Nasal Cavity; StatPearls Publishing: Treasure Island, FL, USA, 2020. [Google Scholar]
- Crowe, T.P.; Greenlee, M.H.W.; Kanthasamy, A.G.; Hsu, W.H. Mechanism of Intranasal Drug Delivery Directly to the Brain. Life Sci. 2018, 195, 44–52. [Google Scholar] [CrossRef] [PubMed]
- Graf, P.; Eccles, R.; Chen, S. Efficacy and Safety of Intranasal Xylometazoline and Ipratropium in Patients with Common Cold. Expert Opin. Pharmacother. 2009, 10, 889–908. [Google Scholar] [CrossRef] [PubMed]
- Wattanakumtornkul, S.; Pinto, A.B.; Williams, D.B. Intranasal Hormone Replacement Therapy. Menopause 2003, 10, 88–98. [Google Scholar] [CrossRef]
- Frey William, H.I. Neurologic Agents for Nasal Administration to the Brain. WO1991007947, 13 June 1991. [Google Scholar]
- Dhuria, S.V.; Hanson, L.R.; Frey, W.H. 2nd Intranasal Delivery to the Central Nervous System: Mechanisms and Experimental Considerations. J. Pharm. Sci. 2010, 99, 1654–1673. [Google Scholar] [CrossRef] [PubMed]
- Keller, L.-A.; Merkel, O.; Popp, A. Intranasal Drug Delivery: Opportunities and Toxicologic Challenges during Drug Development. Drug Deliv. Transl. Res. 2022, 12, 735–757. [Google Scholar] [CrossRef] [PubMed]
- Kapoor, M.; Cloyd, J.C.; Siegel, R.A. A Review of Intranasal Formulations for the Treatment of Seizure Emergencies. J. Control. release Off. J. Control. Release Soc. 2016, 237, 147–159. [Google Scholar] [CrossRef] [PubMed]
- Juel-Berg, N.; Darling, P.; Bolvig, J.; Foss-Skiftesvik, M.H.; Halken, S.; Winther, L.; Hansen, K.S.; Askjaer, N.; Heegaard, S.; Madsen, A.R.; et al. Intranasal Corticosteroids Compared with Oral Antihistamines in Allergic Rhinitis: A Systematic Review and Meta-Analysis. Am. J. Rhinol. Allergy 2017, 31, 19–28. [Google Scholar] [CrossRef] [PubMed]
- Ridolo, E.; Barone, A.; Nicoletta, F.; Paoletti, G.; Heffler, E.; Malvezzi, L.; Canonica, G.W. Intranasal Corticosteroid and Antihistamine Combinations in the Treatment of Allergic Rhinitis: The Role of the Novel Formulation Olopatadine/Mometasone Furoate. Expert Rev. Clin. Immunol. 2023, 19, 575–584. [Google Scholar] [CrossRef]
- Arora, P.; Sharma, S.; Garg, S. Permeability Issues in Nasal Drug Delivery. Drug Discov. Today 2002, 7, 967–975. [Google Scholar] [CrossRef]
- Oliveira, P.; Fortuna, A.; Alves, G.; Falcao, A. Drug-Metabolizing Enzymes and Efflux Transporters in Nasal Epithelium: Influence on the Bioavailability of Intranasally Administered Drugs. Curr. Drug Metab. 2016, 17, 628–647. [Google Scholar] [CrossRef] [PubMed]
- Mogollo, A.P. Importancia de La Vía Nasal Para La Administración de Opioides. Med. Paliativa 2015, 22, 33–45. [Google Scholar] [CrossRef]
- Ulusoy, S.; Muluk, N.B.; Karpischenko, S.; Passali, G.C.; Negm, H.; Passali, D.; Milkov, M.; Kopacheva-Barsova, G.; Konstantinidis, I.; Dilber, M. Mechanisms and Solutions for Nasal Drug Delivery—A Narrative Review. Eur. Rev. Med. Pharmacol. Sci. 2022, 26, 72–81. [Google Scholar] [PubMed]
- Pires, A.; Fortuna, A.; Alves, G.; Falcão, A. Intranasal Drug Delivery: How, Why and What For? J. Pharm. Pharm. Sci. 2009, 12, 288–311. [Google Scholar] [CrossRef] [PubMed]
- Machado, N.D.; Fernández, M.A.; Díaz, D.D. Recent Strategies in Resveratrol Delivery Systems. Chempluschem 2019, 84, 951–973. [Google Scholar] [CrossRef]
- Preeti; Sambhakar, S.; Malik, R.; Bhatia, S.; Al Harrasi, A.; Rani, C.; Saharan, R.; Kumar, S.; Geeta; Sehrawat, R. Nanoemulsion: An Emerging Novel Technology for Improving the Bioavailability of Drugs. Scientifica 2023, 2023, 6640103. [Google Scholar] [CrossRef]
- Shakeel, F.; Shafiq, S.; Haq, N.; Alanazi, F.K.; Alsarra, I.A. Nanoemulsions as Potential Vehicles for Transdermal and Dermal Delivery of Hydrophobic Compounds: An Overview. Expert Opin. Drug Deliv. 2012, 9, 953–974. [Google Scholar] [CrossRef]
- Robertson, I.; Wai Hau, T.; Sami, F.; Sajid Ali, M.; Badgujar, V.; Murtuja, S.; Saquib Hasnain, M.; Khan, A.; Majeed, S.; Tahir Ansari, M. The Science of Resveratrol, Formulation, Pharmacokinetic Barriers and Its Chemotherapeutic Potential. Int. J. Pharm. 2022, 618, 121605. [Google Scholar] [CrossRef]
- Johnsen, K.B.; Moos, T. Revisiting Nanoparticle Technology for Blood–Brain Barrier Transport: Unfolding at the Endothelial Gate Improves the Fate of Transferrin Receptor-Targeted Liposomes. J. Control. Release 2016, 222, 32–46. [Google Scholar] [CrossRef]
- Monsalve, Y.; Tosi, G.; Ruozi, B.; Belletti, D.; Vilella, A.; Zoli, M.; Vandelli, M.A.; Forni, F.; Lopez, B.L.; Sierra, L. PEG-g-Chitosan Nanoparticles Functionalized with the Monoclonal Antibody OX26 for Brain Drug Targeting. Nanomedicine 2015, 10, 1735–1750. [Google Scholar] [CrossRef]
- Vllasaliu, D.; Casettari, L.; Fowler, R.; Exposito-Harris, R.; Garnett, M.; Illum, L.; Stolnik, S. Absorption-Promoting Effects of Chitosan in Airway and Intestinal Cell Lines: A Comparative Study. Int. J. Pharm. 2012, 430, 151–160. [Google Scholar] [CrossRef]
- Peng, Y.; Chen, L.; Ye, S.; Kang, Y.; Liu, J.; Zeng, S.; Yu, L. Research and Development of Drug Delivery Systems Based on Drug Transporter and Nano-Formulation. Asian J. Pharm. Sci. 2020, 15, 220–236. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.; Minko, T. Nanotherapeutics for Nose-to-Brain Drug Delivery: An Approach to Bypass the Blood Brain Barrier. Pharmaceutics 2021, 13, 2049. [Google Scholar] [CrossRef]
- Sivadasan, D.; Sultan, M.H.; Alqahtani, S.S.; Javed, S. Cubosomes in Drug Delivery—A Comprehensive Review on Its Structural Components, Preparation Techniques and Therapeutic Applications. Biomedicines 2023, 11, 1114. [Google Scholar] [CrossRef]
- Waglewska, E.; Pucek-Kaczmarek, A.; Bazylińska, U. Novel Surface-Modified Bilosomes as Functional and Biocompatible Nanocarriers of Hybrid Compounds. Nanomaterials 2020, 10, 2472. [Google Scholar] [CrossRef]
- Mukherjee, S.; Ray, S.; Thakur, R.S. Solid Lipid Nanoparticles: A Modern Formulation Approach in Drug Delivery System. Indian J. Pharm. Sci. 2009, 71, 349–358. [Google Scholar] [CrossRef] [PubMed]
- Agrawal, M.; Saraf, S.; Saraf, S.; Dubey, S.K.; Puri, A.; Patel, R.J.; Ravichandiran, V.; Murty, U.S.; Alexander, A. Recent Strategies and Advances in the Fabrication of Nano Lipid Carriers and Their Application towards Brain Targeting. J. Control. Release 2020, 321, 372–415. [Google Scholar] [CrossRef]
- Pando, D.; Matos, M.; Gutiérrez, G.; Pazos, C. Formulation of Resveratrol Entrapped Niosomes for Topical Use. Colloids Surfaces B Biointerfaces 2015, 128, 398–404. [Google Scholar] [CrossRef]
- Pando, D.; Beltrán, M.; Gerone, I.; Matos, M.; Pazos, C. Resveratrol Entrapped Niosomes as Yoghurt Additive. Food Chem. 2015, 170, 281–287. [Google Scholar] [CrossRef]
- Vankayala, J.S.; Battula, S.N.; Kandasamy, R.; Mariya, G.A.; Franklin, M.E.E.; Pushpadass, H.A.; Naik, L.N. Surfactants and Fatty Alcohol Based Novel Nanovesicles for Resveratrol: Process Optimization, Characterization and Evaluation of Functional Properties in RAW 264.7 Macrophage Cells. J. Mol. Liq. 2018, 261, 387–396. [Google Scholar] [CrossRef]
- Caddeo, C.; Manconi, M.; Cardia, M.C.; Díez-Sales, O.; Fadda, A.M.; Sinico, C. Investigating the Interactions of Resveratrol with Phospholipid Vesicle Bilayer and the Skin: NMR Studies and Confocal Imaging. Int. J. Pharm. 2015, 484, 138–145. [Google Scholar] [CrossRef] [PubMed]
- Caddeo, C.; Pons, R.; Carbone, C.; Fernàndez-Busquets, X.; Cardia, M.C.; Maccioni, A.M.; Fadda, A.M.; Manconi, M. Physico-Chemical Characterization of Succinyl Chitosan-Stabilized Liposomes for the Oral Co-Delivery of Quercetin and Resveratrol. Carbohydr. Polym. 2017, 157, 1853–1861. [Google Scholar] [CrossRef]
- Zhou, J.; Zhou, M.; Yang, F.F.; Liu, C.Y.; Le Pan, R.; Chang, Q.; Liu, X.M.; Liao, Y.H. Involvement of the Inhibition of Intestinal Glucuronidation in Enhancing the Oral Bioavailability of Resveratrol by Labrasol Containing Nanoemulsions. Mol. Pharm. 2015, 12, 1084–1095. [Google Scholar] [CrossRef]
- Nasr, M. Development of an Optimized Hyaluronic Acid-Based Lipidic Nanoemulsion Co-Encapsulating Two Polyphenols for Nose to Brain Delivery. Drug Deliv. 2016, 23, 1444–1452. [Google Scholar] [CrossRef]
- Fang, Q.; Ma, C.; Xia, Q. Preparation and Evaluation of Trans-Resveratrol NanoSolve. Integr. Ferroelectr. 2016, 169, 7–14. [Google Scholar] [CrossRef]
- Herneisey, M.; Williams, J.; Mirtic, J.; Liu, L.; Potdar, S.; Bagia, C.; Cavanaugh, J.E.; Janjic, J.M. Development and Characterization of Resveratrol Nanoemulsions Carrying Dual-Imaging Agents. Ther. Deliv. 2016, 7, 795–808. [Google Scholar] [CrossRef]
- Yen, C.C.; Chang, C.W.; Hsu, M.C.; Wu, Y.T. Self-Nanoemulsifying Drug Delivery System for Resveratrol: Enhanced Oral Bioavailability and Reduced Physical Fatigue in Rats. Int. J. Mol. Sci. 2017, 18, 1853. [Google Scholar] [CrossRef]
- Mamadou, G.; Charrueau, C.; Dairou, J.; Limas Nzouzi, N.; Eto, B.; Ponchel, G. Increased Intestinal Permeation and Modulation of Presystemic Metabolism of Resveratrol Formulated into Self-Emulsifying Drug Delivery Systems. Int. J. Pharm. 2017, 521, 150–155. [Google Scholar] [CrossRef]
- Yang, F.F.; Zhou, J.; Hu, X.; Cong, Z.Q.; Liu, C.Y.; Le Pan, R.; Chang, Q.; Liu, X.M.; Liao, Y.H. Improving Oral Bioavailability of Resveratrol by a UDP-Glucuronosyltransferase Inhibitory Excipient-Based Self-Microemulsion. Eur. J. Pharm. Sci. 2018, 114, 303–309. [Google Scholar] [CrossRef] [PubMed]
- Matos, M.; Laca, A.; Rea, F.; Iglesias, O.; Rayner, M.; Gutiérrez, G. O/W Emulsions Stabilized by OSA-Modified Starch Granules versus Non-Ionic Surfactant: Stability, Rheological Behaviour and Resveratrol Encapsulation. J. Food Eng. 2018, 222, 207–217. [Google Scholar] [CrossRef]
- Dai, L.; Li, Y.; Kong, F.; Liu, K.; Si, C.; Ni, Y. Lignin-Based Nanoparticles Stabilized Pickering Emulsion for Stability Improvement and Thermal-Controlled Release of Trans-Resveratrol. ACS Sustain. Chem. Eng. 2019, 7, 13497–13504. [Google Scholar] [CrossRef]
- Choi, A.-J.; Jo, Y.; Cho, Y.-J.; Kim, T.-E.; Kim, C.-T. Preparation and Characterization of Resveratrol Nanoemulsions Stabilized by Self-Assembly and Complex Coacervation Consisting of Sodium Alginate, Chitosan, and β-Cyclodextrin. Food Eng. Prog. 2017, 21, 215–224. [Google Scholar] [CrossRef]
- Matos, M.; Gutiérrez, G.; Iglesias, O.; Coca, J.; Pazos, C. Enhancing Encapsulation Efficiency of Food-Grade Double Emulsions Containing Resveratrol or Vitamin B12 by Membrane Emulsification. J. Food Eng. 2015, 166, 212–220. [Google Scholar] [CrossRef]
- Acevedo-Fani, A.; Silva, H.D.; Soliva-Fortuny, R.; Martín-Belloso, O.; Vicente, A.A. Formation, Stability and Antioxidant Activity of Food-Grade Multilayer Emulsions Containing Resveratrol. Food Hydrocoll. 2017, 71, 207–215. [Google Scholar] [CrossRef]
- Matos, M.; Gutiérrez, G.; Martínez-Rey, L.; Iglesias, O.; Pazos, C. Encapsulation of Resveratrol Using Food-Grade Concentrated Double Emulsions: Emulsion Characterization and Rheological Behaviour. J. Food Eng. 2018, 226, 73–81. [Google Scholar] [CrossRef]
- Scalia, S.; Trotta, V.; Iannuccelli, V.; Bianchi, A. Enhancement of in Vivo Human Skin Penetration of Resveratrol by Chitosan-Coated Lipid Microparticles. Colloids Surfaces B Biointerfaces 2015, 135, 42–49. [Google Scholar] [CrossRef] [PubMed]
- Pangeni, R.; Sharma, S.; Mustafa, G.; Ali, J.; Baboota, S. Vitamin e Loaded Resveratrol Nanoemulsion for Brain Targeting for the Treatment of Parkinson’s Disease by Reducing Oxidative Stress. Nanotechnology 2014, 25, 485102. [Google Scholar] [CrossRef]
- Abbas, H.; Refai, H.; El Sayed, N.; Rashed, L.A.; Mousa, M.R.; Zewail, M. Superparamagnetic Iron Oxide Loaded Chitosan Coated Bilosomes for Magnetic Nose to Brain Targeting of Resveratrol. Int. J. Pharm. 2021, 610, 121244. [Google Scholar] [CrossRef]
- Ahirrao, M.; Shrotriya, S. In Vitro and in Vivo Evaluation of Cubosomal in Situ Nasal Gel Containing Resveratrol for Brain Targeting. Drug Dev. Ind. Pharm. 2017, 43, 1686–1693. [Google Scholar] [CrossRef] [PubMed]
- Salem, H.F.; Kharshoum, R.M.; Abou-Taleb, H.A.; Naguib, D.M. Brain Targeting of Resveratrol through Intranasal Lipid Vesicles Labelled with Gold Nanoparticles: In Vivo Evaluation and Bioaccumulation Investigation Using Computed Tomography and Histopathological Examination. J. Drug Target. 2019, 27, 1127–1134. [Google Scholar] [CrossRef]
- Rajput, A.; Bariya, A.; Allam, A.; Othman, S.; Butani, S.B. In Situ Nanostructured Hydrogel of Resveratrol for Brain Targeting: In Vitro-in Vivo Characterization. Drug Deliv. Transl. Res. 2018, 8, 1460–1470. [Google Scholar] [CrossRef]
- Trotta, V.; Pavan, B.; Ferraro, L.; Beggiato, S.; Traini, D.; Des Reis, L.G.; Scalia, S.; Dalpiaz, A. Brain Targeting of Resveratrol by Nasal Administration of Chitosan-Coated Lipid Microparticles. Eur. J. Pharm. Biopharm. 2018, 127, 250–259. [Google Scholar] [CrossRef]
- Hao, J.; Zhao, J.; Zhang, S.; Tong, T.; Zhuang, Q.; Jin, K.; Chen, W.; Tang, H. Fabrication of an Ionic-Sensitive in Situ Gel Loaded with Resveratrol Nanosuspensions Intended for Direct Nose-to-Brain Delivery. Colloids Surfaces B Biointerfaces 2016, 147, 376–386. [Google Scholar] [CrossRef]
- Salem, H.F.; Kharshoum, R.M.; Abou-Taleb, H.A.; Naguib, D.M. Nanosized Transferosome-Based Intranasal In Situ Gel for Brain Targeting of Resveratrol: Formulation, Optimization, In Vitro Evaluation, and In Vivo Pharmacokinetic Study. AAPS PharmSciTech 2019, 20, 181. [Google Scholar] [CrossRef]
- Kim, Y.; Hwang, S.; Khalmuratova, R.; Kang, S.; Lee, M.; Song, Y.; Park, J.W.; Yu, J.; Shin, H.W.; Lee, Y. α-Helical Cell-Penetrating Peptide-Mediated Nasal Delivery of Resveratrol for Inhibition of Epithelial-to-Mesenchymal Transition. J. Control. Release 2020, 317, 181–194. [Google Scholar] [CrossRef]

| Formulation (Resveratrol Concentration) | Cmax (ng/mL) | AUC0–24 | Tmax (h) | Reference |
|---|---|---|---|---|
| Brain | Brain | |||
| Cubosomal in situ nasal gel, i.n. (1.29 mg/kg) | 564.49 ± 2.24 | 3611.4 ± 17.3 ng/mL·h | ~2.4 | [84] |
| Resveratrol solution i.n. (1.29 mg/kg) | 133.7 ± 4.1 | 921.7 ± 63.5 ng/mL·h | ||
| Resveratrol solution oral (1.29 mg/kg) | 102.2 ± 9.8 | 656.5 ± 65.4 ng/mL·h | ||
| Lipid microparticles-resveratrol- Chitosan coated-plus, i.n. (0.2 mg) | 9700 ± 1900 | 554 ± 67 µg/mL/min−1 | 1 | [87] |
| Lipid microparticles-resveratrol- Chitosan coated, i.n. (0.2 mg) | 1300 ± 300 | 45 ± 5 µg/mL/min−1 | ||
| Lipid microparticles resveratrol suspension, i.n. (0.2 mg) | 790 ± 150 | 54 ± 13 µg/mL/min−1 | ||
| Ionic-sensitive in situ gel loaded with resveratrol nanosuspensions, i.n. (2 mg/kg) | 60.42 ± 35.14 | 362.54 ± 168.96 (h·ng/mL)/(h·g/g) | 0.3 | [88] |
| Ionic-sensitive in situ gel loaded with resveratrol nanosuspensions., i.v. (2 mg/kg) | 26.44 ± 8.71 | 125.88 ± 57.65 (h·ng/mL)/(h·g/g) | ||
| Nasal nanosized transferosome based intranasal in sito gel. (1 mg/mL) | N/A | 6.847 ± 0.997 µg·h/mL | 0.75 vs. 7.33 | [89] |
| Oral resveratrol suspension (1 mg/mL) | N/A | 0.459 ± 0.17 µg·h/mL | ||
| Hyaluronic acid based lipidic nanoemulsion (50 mg) | 1937.9 ± 221 | 1025.67 ± 18 ng/g | 1 | [69] |
| Resveratrol solution (50 mg) | 279.57 ± 43.4 | 7059.4 ± 326 ng/g | ||
| Vitamin E loaded resveratrol nanoemulsion, i.n. (150 mg/mL) | 3976.25 ± 118.62 | 36,453.43 ± 114.2 ng·h/mL | 1.5 | [82] |
| Resveratrol solution, i.n. (150 mg/mL) | 2792.76 ± 137.21 | 27,930.60 ± 104.38 ng·h/mL | ||
| Resveratrol solution, i.v. (150 mg/mL) | 1710.85 ± 64.92 | 13,235.20 ± 106.4 ng·h/mL |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alquisiras-Burgos, I.; González-Herrera, I.G.; Alcalá-Alcalá, S.; Aguilera, P. Nose-to Brain Delivery of Resveratrol, a Non-Invasive Method for the Treatment of Cerebral Ischemia. Drugs Drug Candidates 2024, 3, 102-125. https://doi.org/10.3390/ddc3010007
Alquisiras-Burgos I, González-Herrera IG, Alcalá-Alcalá S, Aguilera P. Nose-to Brain Delivery of Resveratrol, a Non-Invasive Method for the Treatment of Cerebral Ischemia. Drugs and Drug Candidates. 2024; 3(1):102-125. https://doi.org/10.3390/ddc3010007
Chicago/Turabian StyleAlquisiras-Burgos, Iván, Irma Gabriela González-Herrera, Sergio Alcalá-Alcalá, and Penélope Aguilera. 2024. "Nose-to Brain Delivery of Resveratrol, a Non-Invasive Method for the Treatment of Cerebral Ischemia" Drugs and Drug Candidates 3, no. 1: 102-125. https://doi.org/10.3390/ddc3010007
APA StyleAlquisiras-Burgos, I., González-Herrera, I. G., Alcalá-Alcalá, S., & Aguilera, P. (2024). Nose-to Brain Delivery of Resveratrol, a Non-Invasive Method for the Treatment of Cerebral Ischemia. Drugs and Drug Candidates, 3(1), 102-125. https://doi.org/10.3390/ddc3010007








