Using Virtual Reality During Chemotherapy to Support Emotional Regulation in Patients: Adding an Olfactory Reinforcement or Not?
Abstract
1. Introduction
1.1. Emotions and Olfaction
1.1.1. Olfaction, VR and the Sense of Presence
1.1.2. Olfaction and the Practice of Relaxation
1.1.3. Olfaction and Clinical Practice
1.2. From Interactivity to Olfactory Reinforcement
1.3. Emotional Distress
1.4. The Present Study
2. Materials and Methods
2.1. Sample
2.2. Materials
2.3. Apparatus
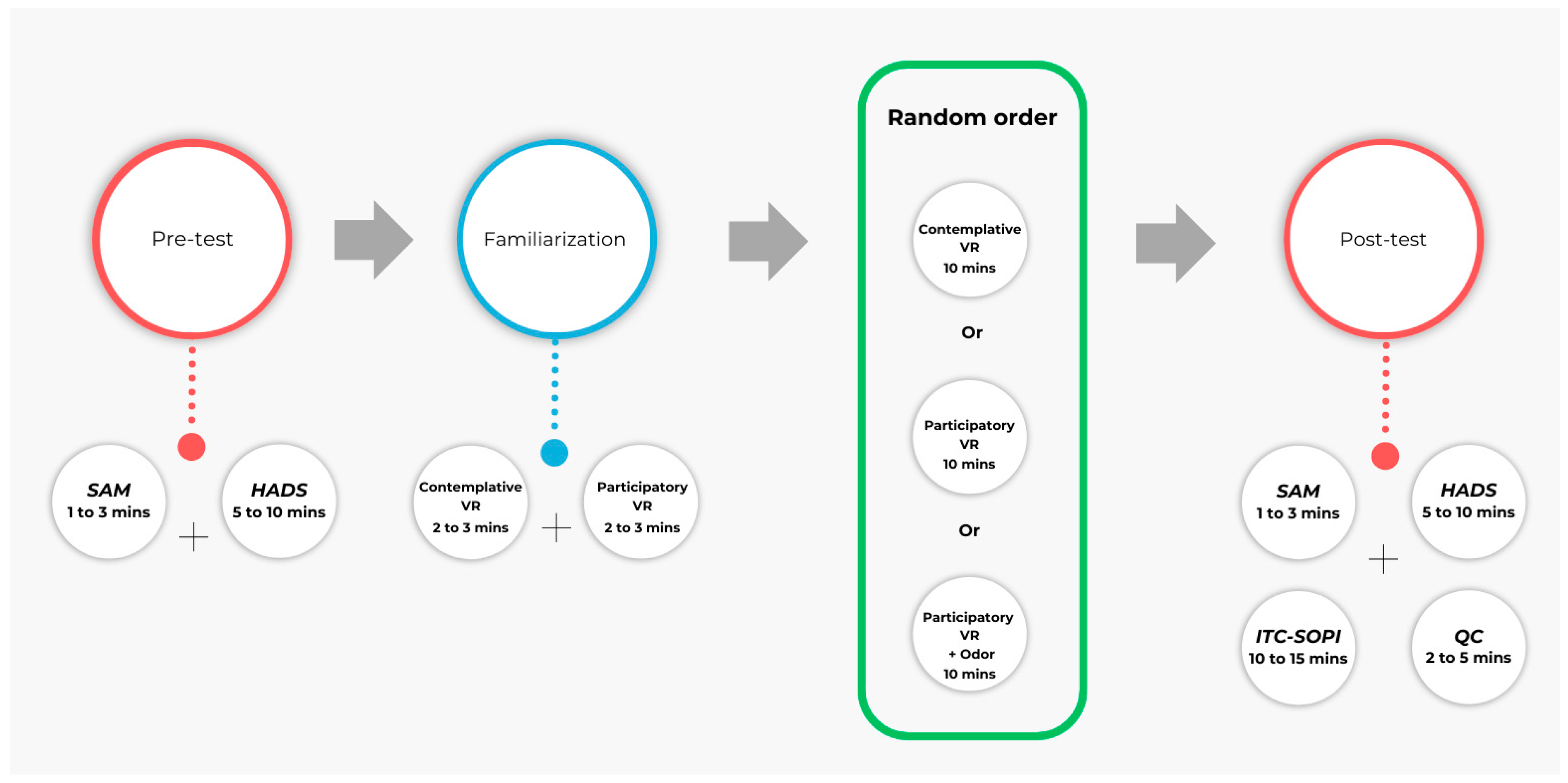
2.4. Procedure
3. Results
3.1. Anxiety
3.2. Depressive Mood
3.3. State of Mood
3.4. Sense of Presence
3.5. Cybersickness
3.6. Tendency to Immerse
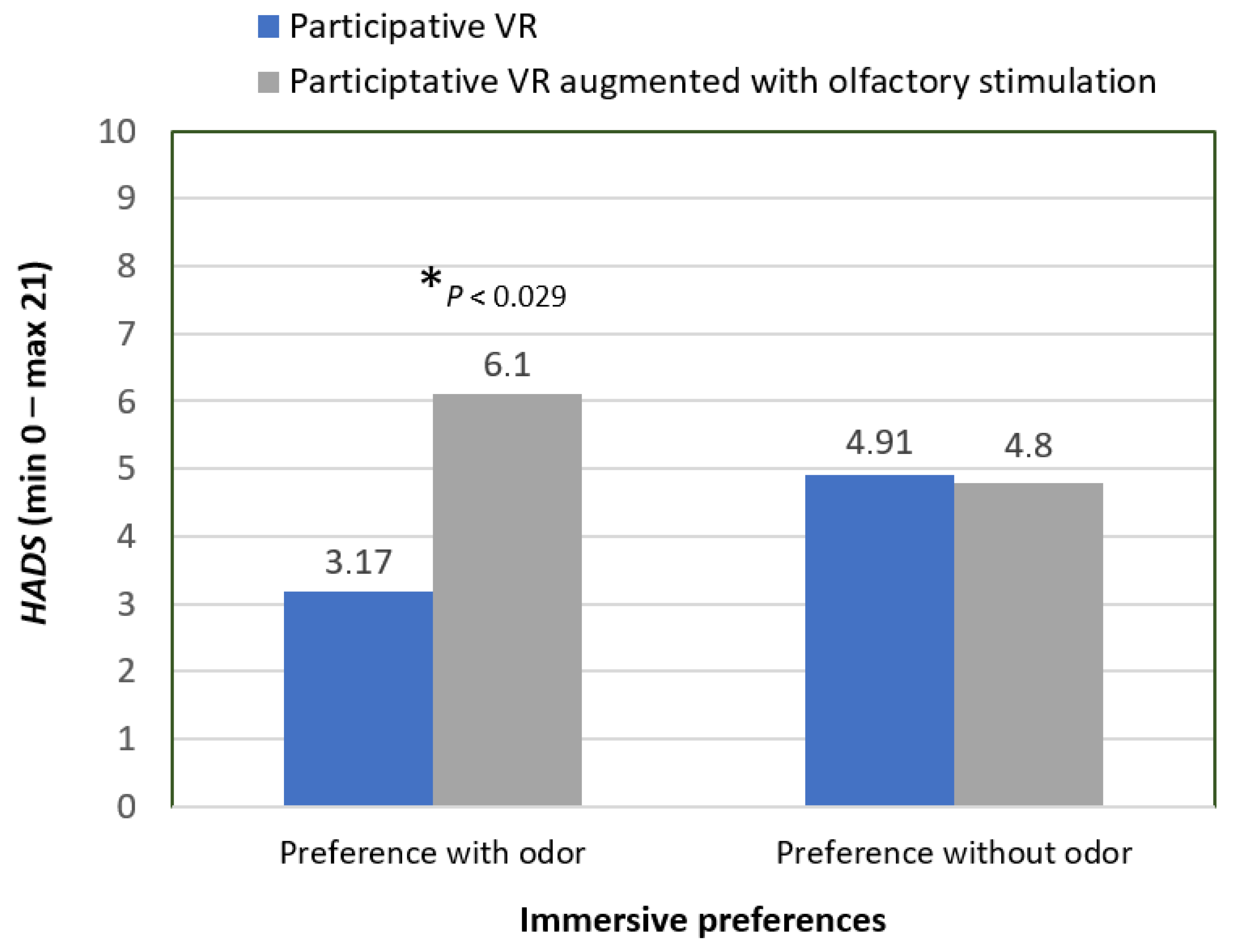
3.7. VR Benefits According to Immersive Preference
4. Discussion
Limitations and Perspectives
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| VR | Virtual reality |
| SD | Standard deviation |
References
- Buche, H.; Michel, A.; Blanc, N. Use of virtual reality in oncology: From the state of the art to an integrative model. Front. Virtual Real. 2022, 3, 894162. [Google Scholar] [CrossRef]
- Barfield, W.; Danas, E. Comments on the use of olfactory displays for virtual environments. Presence Teleoper. Virtual Environ. 1996, 5, 109–121. [Google Scholar] [CrossRef]
- Michel, A.; Brigaud, E.; Cousson-Gélie, F.; Vidal, J.; Blanc, N. La réalité virtuelle chez les femmes âgées suivies pour un cancer du sein: Intérêts et attentes. Gériatrie Psychol. Neuropsychiatr. Vieil. 2019, 17, 415–422. [Google Scholar] [CrossRef]
- Michel, A.; Vidal, J.; Brigaud, E.; Sokratous, K.; Blanc, N. Dessine-moi une réalité plus belle: La réalité virtuelle vue par les patients atteintes d’un cancer du sein. Psycho-Oncology 2019, 13, 69–78. [Google Scholar] [CrossRef]
- Ashley Verzwyvelt, L.; McNamara, A.; Xu, X.; Stubbins, R. Effects of virtual reality v. biophilic environments on pain and distress in oncology patients: A case-crossover pilot study. Sci. Rep. 2021, 11, 20196. [Google Scholar] [CrossRef] [PubMed]
- Wilson, K.; Scorsone, G. The use of virtual reality technologies to reduce anxiety and improve experience in chemotherapy patients during treatment. Front. Virtual Real. 2021, 2, 695449. [Google Scholar] [CrossRef]
- Kelleher, S.A.; Fisher, H.M.; Winger, J.G.; Miller, S.N.; Amaden, G.H.; Somers, T.J.; Colloca, L.; Uronis, H.E.; Keefe, F.J. Virtual reality for improving pain and pain-related symptoms in patients with advanced stage colorectal cancer: A pilot trial to test feasibility and acceptability. Palliat. Support. Care 2022, 20, 471–481. [Google Scholar] [CrossRef] [PubMed]
- Kaye, J.N. Symbolic Olfactory Display. Doctoral Dissertation, Massachusetts Institute of Technology, Cambridge, MA, USA, 2001. [Google Scholar]
- Tijou, A. Contribution à L’intégration et à L’évaluation du Retour Olfactif en Environnement Virtuel. Ph.D. Thesis, Université d’Angers, Angers, France, 2007. [Google Scholar]
- Soudry, Y.; Lemogne, C.; Malinvaud, D.; Consoli, S.M.; Bonfils, P. Olfactory system and emotion: Common substrates. Eur. Ann. Otorhinolaryngol. Head Neck Dis. 2011, 128, 18–23. [Google Scholar] [CrossRef]
- Amores, J.; Richer, R.; Zhao, N.; Maes, P.; Eskofier, B.M. Promoting relaxation using virtual reality, olfactory interfaces and wearable EEG. In Proceedings of the 2018 IEEE 15th International Conference on Wearable and Implantable Body Sensor Networks (BSN), Las Vegas, NV, USA, 4–7 March 2018; IEEE: New York, NY, USA, 2018; pp. 98–101. [Google Scholar] [CrossRef]
- Kontaris, I.; East, B.S.; Wilson, D.A. Behavioral and neurobiological convergence of odor, mood and emotion: A review. Front. Behav. Neurosci. 2020, 14, 35. [Google Scholar] [CrossRef]
- Sullivan, R.M.; Wilson, D.A.; Ravel, N.; Mouly, A.M. Olfactory memory networks: From emotional learning to social behaviors. Front. Behav. Neurosci. 2015, 9, 36. [Google Scholar] [CrossRef]
- Motomura, N.; Sakurai, A.; Yotsuya, Y. Reduction of mental stress with lavender odorant. Percept. Mot. Ski. 2001, 93, 713–718. [Google Scholar] [CrossRef] [PubMed]
- Lehrner, J.; Marwinski, G.; Lehr, S.; Johren, P.; Deecke, L. Ambient odors of orange and lavender reduce anxiety and improve mood in a dental office. Physiol. Behav. 2005, 86, 92–95. [Google Scholar] [CrossRef]
- Redd, W.H.; Manne, S.L.; Peters, B.; Jacobsen, P.B.; Schmidt, H. Fragrance administration to reduce anxiety during MR imaging. J. Magn. Reson. Imaging 1994, 4, 623–626. [Google Scholar] [CrossRef]
- Dinh, H.Q.; Walker, N.; Hodges, L.F.; Song, C.; Kobayashi, A. Evaluating the importance of multi-sensory input on memory and the sense of presence in virtual environments. In Proceedings of the Proceedings IEEE Virtual Reality (Cat. No. 99CB36316), Houston, TX, USA, 13–17 March 1999; IEEE: New York, NY, USA, 1999; pp. 222–228. [Google Scholar]
- Baus, O.; Bouchard, S. Exposure to an unpleasant odour increases the sense of presence in virtual reality. Virtual Real. 2017, 21, 59–74. [Google Scholar] [CrossRef]
- Baus, O.; Bouchard, S.; Nolet, K. Exposure to a pleasant odour may increase the sense of reality, but not the sense of presence or realism. Behav. Inf. Technol. 2019, 38, 1369–1378. [Google Scholar] [CrossRef]
- Pizzoli, S.F.M.; Monzani, D.; Mazzocco, K.; Maggioni, E.; Pravettoni, G. The power of odor persuasion: The incorporation of olfactory cues in virtual environments for personalized relaxation. Perspect. Psychol. Sci. 2022, 17, 652–661. [Google Scholar] [CrossRef]
- Risso, P.; Covarrubias Rodriguez, M.; Bordegoni, M.; Gallace, A. Development and testing of a small-size olfactometer for the perception of food and beverages in humans. Front. Digit. Humanit. 2018, 5, 7. [Google Scholar] [CrossRef]
- Rothbaum, B.O.; Rizzo, A.S.; Difede, J. Virtual reality exposure therapy for combat-related posttraumatic stress disorder. Ann. N. Y. Acad. Sci. 2010, 1208, 126–132. [Google Scholar] [CrossRef]
- Aiken, M.P.; Berry, M.J. Posttraumatic stress disorder: Possibilities for olfaction and virtual reality exposure therapy. Virtual Real. 2015, 19, 95–109. [Google Scholar] [CrossRef]
- Carlin, A.S.; Hoffman, H.G.; Weghorst, S. Virtual reality and tactile augmentation in the treatment of spider phobia: A case report. Behav. Res. Ther. 1997, 35, 153–158. [Google Scholar] [CrossRef]
- Hoffman, H.G.; Garcia-Palacios, A.; Carlin, A.; Furness Iii, T.A.; Botella-Arbona, C. Interfaces that heal: Coupling real and virtual objects to treat spider phobia. Int. J. Hum. Comput. Interact. 2003, 16, 283–300. [Google Scholar] [CrossRef]
- Baus, O.; Bouchard, S. The sense of olfaction: Its characteristics and its possible applications in virtual environments. J. CyberTher. Rehab. 2010, 3, 31–50. [Google Scholar]
- Freeman, D.; Reeve, S.; Robinson, A.; Ehlers, A.; Clark, D.; Spanlang, B.; Slater, M. Virtual reality in the assessment, understanding, and treatment of mental health disorders. Psychol. Med. 2017, 47, 2393–2400. [Google Scholar] [CrossRef]
- Bu, X.; Ng, P.H.; Xu, W.; Cheng, Q.; Chen, P.Q.; Cheng, A.S.; Liu, X. The effectiveness of virtual Reality–Based interventions in rehabilitation management of breast cancer survivors: Systematic review and meta-analysis. JMIR Serious Games 2022, 10, e31395. [Google Scholar] [CrossRef] [PubMed]
- Melillo, A.; Chirico, A.; De Pietro, G.; Gallo, L.; Caggianese, G.; Barone, D.; De Laurentiis, M.; Giordano, A. Virtual reality rehabilitation systems for cancer survivors: A narrative review of the literature. Cancers 2022, 14, 3163. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Wang, N.; Zhang, H.; Sun, X.; Wang, Y.; Zhang, Y. Effectiveness of Virtual Reality in Symptom Management of Cancer Patients: A Systematic Review and Meta-Analysis. J. Pain Symptom Manag. 2023, 65, e467–e482. [Google Scholar] [CrossRef]
- Buche, H.; Michel, A.; Blanc, N. When virtual reality supports patients’ emotional management in chemotherapy. Front. Virtual Real. 2023, 4, 1294482. [Google Scholar] [CrossRef]
- Pavlov, I.P. Conditioned Reflex: An Investigation of the Physiological Activity of the Cerebral Cortex; Dover Publications: New York, NY, USA, 1960. [Google Scholar]
- Wong, C.L.; Li, C.K.; Choi, K.C.; So, W.K.W.; Kwok, J.Y.Y.; Cheung, Y.T.; Chan, C.W.H. Effects of immersive virtual reality for managing anxiety, nausea and vomiting among paediatric cancer patients receiving their first chemotherapy: An exploratory randomised controlled trial. Eur. J. Oncol. Nurs. 2022, 61, 102233. [Google Scholar] [CrossRef]
- Henry, J.D.; Crawford, J.R. The short-form version of the Depression Anxiety Stress Scales (DASS-21): Construct validity and normative data in a large non-clinical sample. Br. J. Clin. Psychol. 2005, 44, 227–239. [Google Scholar] [CrossRef]
- O’Gara, G.; Murray, L.; Georgopoulou, S.; Anstiss, T.; Macquarrie, A.; Wheatstone, P.; Bellman, B.; Gilbert, P.; Steed, A.; Wiseman, T. SafeSpace: What is the feasibility and acceptability of a codesigned virtual reality intervention, incorporating compassionate mind training, to support people undergoing cancer treatment in a clinical setting? BMJ Open 2022, 12, e047626. [Google Scholar] [CrossRef]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef]
- Ando, M.M.; Leones, L.M.B.; Mendoza, M.J.L.; Ting, F.I.; Sacdalan, D.B. O15-4 Use of virtual reality for management of anxiety and depression among chemotherapy-naive Filipino breast cancer patients. Ann. Oncol. 2022, 33, S478. [Google Scholar] [CrossRef]
- Reynolds, L.M.; Cavadino, A.; Chin, S.; Little, Z.; Akroyd, A.; Tennant, G.; Dobson, R.; Broom, R.; Gautier, A. The benefits and acceptability of virtual reality interventions for women with metastatic breast cancer in their homes; a pilot randomised trial. BMC Cancer 2022, 22, 360. [Google Scholar] [CrossRef] [PubMed]
- Carline, J.; Carline, R. Nature Treks VR (Version 1.25). Greener Games. 2021. Available online: http://greenergames.net/ (accessed on 20 February 2017).
- Buche, H.; Michel, A.; Piccoli, C.; Blanc, N. Contemplating or Acting? Which Immersive Modes Should Be Favored in Virtual Reality During Physiotherapy for Breast Cancer Rehabilitation. Front. Psychol. 2021, 12, 631186. [Google Scholar] [CrossRef] [PubMed]
- Bradley, M.M.; Lang, P.J. Measuring emotion: The self-evaluation dummy and the semantic differential. J. Behav. Ther. Exp. Psychiatry 1994, 25, 49–59. [Google Scholar] [CrossRef]
- Independent Television Commission. Sens of Presence Inventory Administration and Scoring Instructions; Goldsmiths University: London, UK, 2000. [Google Scholar]
- Lessiter, J.; Freeman, J.; Keogh, E.; Davidoff, J. A cross-media presence questionnaire: The ITC-sense of presence inventory. Presence Teleoperators Virtual Environ. 2001, 10, 282–297. [Google Scholar] [CrossRef]
- Cyberpsychology Laboratory of UQO. Cyberpsychologie. 2002. Available online: https://w3.uqo.ca/cyberpsy/index.php/labs-team/ (accessed on 13 April 2025).
- Kennedy, R.S.; Lane, N.E.; Berbaum, K.S.; Lilienthal, M.G. Simulator Sickness Questionnaire: An enhanced method for quantifying simulator sickness. Int. J. Aviat. Psychol. 1993, 3, 203–220. [Google Scholar] [CrossRef]
- Spielberger, D.; Gorsuch, L.; Lushene, E. Manual for the State Trait Anxiety Inventory (From Y); Consulting Psychologists Press: Palo Alto, CA, USA, 1983. [Google Scholar]
- Dunbar, M.; Ford, G.; Hunt, K.; Der, G. A confirmatory factor analysis of the Hospital Anxiety and Depression scale: Comparing empirically and theoretically derived structures. Br. J. Clin. Psychol. 2000, 39, 79–94. [Google Scholar] [CrossRef]
- Festy, D. Ma Bible Des Huiles Essentielles; Éditions Leduc: Paris, France, 2018. [Google Scholar]
- Kawai, T.; Noro, K. Psychological effect of stereoscopic 3-D images with fragrances. Ergonomics 1996, 39, 1364–1369. [Google Scholar] [CrossRef]
- Burrai, F.; Ortu, S.; Marinucci, M.; De Marinis, M.G.; Piredda, M. Effectiveness of immersive virtual reality in people with cancer undergoing antiblastic therapy: A randomized controlled trial. Semin. Oncol. Nurs. 2023, 39, 151470. [Google Scholar] [CrossRef]
- Burrai, F.; Sguanci, M.; Petrucci, G.; De Marinis, M.G.; Piredda, M. Effectiveness of immersive virtual reality on anxiety, fatigue and pain in patients with cancer undergoing chemotherapy: A systematic review and meta-analysis. Eur. J. Oncol. Nurs. 2023, 64, 102340. [Google Scholar] [CrossRef]
- Yazdipour, A.B.; Saeedi, S.; Bostan, H.; Masoorian, H.; Sajjadi, H.; Ghazisaeedi, M. Opportunities and challenges of virtual reality-based interventions for patients with breast cancer: A systematic review. BMC Med. Inform. Decis. Mak. 2023, 23, 17. [Google Scholar] [CrossRef] [PubMed]
- Horesh, D.; Kohavi, S.; Shilony-Nalaboff, L.; Rudich, N.; Greenman, D.; Feuerstein, J.S.; Abbasi, M.R. Virtual Reality Combined with Artificial Intelligence (VR-AI) Reduces Hot Flashes and Improves Psychological Well-Being in Women with Breast and Ovarian Cancer: A Pilot Study. Healthcare 2022, 10, 2261. [Google Scholar] [CrossRef] [PubMed]
- Serrano, B.; Baños, R.M.; Botella, C. Virtual reality and stimulation of touch and smell for inducing relaxation: A randomized controlled trial. Comput. Hum. Behav. 2016, 55, 1–8. [Google Scholar] [CrossRef]
- Buche, H.; Michel, A.; Anders, R.; Blanc, N. The role of engagement in virtual reality to enhance emotional well-being in breast cancer patients: A mediation analysis. Cancers 2025, 17, 840. [Google Scholar] [CrossRef]
- Alvarado-Omenat, J.J.; Llamas-Ramos, R.; García-García, D.; Correyero-León, M.; Fonseca-Sánchez, E.; Llamas-Ramos, I. Effectiveness of virtual reality in cancer patients undergoing chemotherapy. Systematic review. Int. J. Cancer 2025, 156, 1419–1428. [Google Scholar] [CrossRef]
- Jeong, S.; Kim, E.J. Effect of depression and empowerment on medication adherence in patients with breast cancer: A descriptive survey. BMC Nurs. 2025, 24, 47. [Google Scholar] [CrossRef]
- Rasool, A.; Shahzad, M.I.; Aslam, H.; Chan, V.; Arshad, M.A. Emotion-Aware Embedding Fusion in Large Language Models (Flan-T5, Llama 2, DeepSeek-R1, and ChatGPT 4) for Intelligent Response Generation. AI 2025, 6, 56. [Google Scholar] [CrossRef]
| Variables | Participants | % |
|---|---|---|
| Age: Mean (SD *) | 53.06 (11.26) | |
| Marital status | ||
| Married/couple | N = 30 | 60 |
| Single/separated/divorced | N = 20 | 30 |
| Employed | ||
| Yes | N = 13 | 26 |
| No | N = 37 | 74 |
| Name of the Measure | Corresponding References | Number of Items | Targeted Measures |
|---|---|---|---|
| Self Assessment Manikin (SAM) | Bradeley et Lang (1994) [41] | 2 items | Mood state: Emotional valence, Emotional arousal |
| Hospital Anxiety Depression Scales (HADS) | Zigmond & Snaith, (1983) [36] | 14 items | Hospital Anxiety Depression |
| Independant Television Commission-Sense Of Presence Inventory (2000) (ITC-SOPI) [42] | Lessiter et al., (2001) [43], translated by Cyberpsychology from UQO (2006) | 28 items | Sens of presence: The spatial presence, Engagement |
| Questionnaire on Cybersickness (QC) | Laboratory of Cyberpsychology at UQO (2002) [44], French translation of the Simulator Sickness Questionnaire (Kennedy et al., 1993) [45] | 16 items | Symptoms which may be caused by VR: Oculomotor, Nausea |
| Tendency of Immersion French version (ITQ) | Laboratory of Cyberpsychology at UQO (2002) [44] | 18 items | Tendency to immerse in distraction |
| Immersive preference | 1 standardized qualitative question | Preference for interactive and sensory modalities |
| Measures | Immersion Condition | Before | After | Difference | p Value |
|---|---|---|---|---|---|
| Mean (SD) | Mean (SD *) | ||||
| Emotional valence | Contemplative VR | 6.16 (1.84) | 7.28 (1.78) | 1.12 | 0.002 |
| Participative VR | 6.32 (1.99) | 7.9 (1.49) | 1.58 | <0.001 | |
| Participative VR with odor | 6.26 (1.98) | 7.84 (1.60) | 1.58 | <0.001 | |
| Arousal | Contemplative VR | 3.84 (2.03) | 2.38 (1.76) | −1.46 | <0.001 |
| Participative VR | 3.14 (2.29) | 2.50 (1.88) | −0.64 | 0.11 | |
| Participative VR with odor | 3.04 (1.78) | 2.28 (1.64) | −0.76 | 0.007 | |
| Anxiety | Contemplative VR | 7.70 (3.97) | 5.44 (4.14) | −2.26 | <0.001 |
| Participative VR | 6.88 (3.70) | 4.56 (3.55) | −2.32 | <0.001 | |
| Participative VR with odor | 7.48 (3.92) | 4.74 (3.59) | −2.74 | <0.001 | |
| Depressive mood | Contemplative VR | 5.04 (3.65) | 4.10 (3.54) | −0.94 | 0.066 |
| Participative VR | 4.42 (3.57) | 3.34 (2.83) | −1.08 | 0.014 | |
| Participative VR with odor | 5.48 (3.32) | 3.52 (2.80) | −1.96 | <0.001 |
| Contemplative VR | Participative VR | Participative VR Augmented with Olfactory Stimulation | |
|---|---|---|---|
| Mean (SD) | Mean (SD *) | Mean (SD) | |
| Spatial presence | 3.48 (0.65) | 4.05 (0.57) | 4.13 (0.52) |
| Engagement | 3.87 (0.59) | 4.14 (0.50) | 4.20 (0.44) |
| Contemplative VR | Participative VR | Participative VR Augmented with Olfactory Stimulation | |
|---|---|---|---|
| Mean (SD) | Mean (SD *) | Mean (SD) | |
| Total cybersickness | 1.04 (1.78) | 1.16 (1.84) | 1.46 (2.3) |
| Oculo-motor | 0.6 (1.25) | 0.52 (1.20) | 0.66 (1.65) |
| Nausea | 0.42 (0.86) | 0.62 (0.97) | 0.8 (1.14) |
| Patients | Norms | |
|---|---|---|
| Mean (SD *) | Mean (SD) | |
| Total | 81.6 (16.9) | 64.11 (13.11) |
| Focus | 25.3 (4.86) | 24.81 (7.54) |
| Engagement | 23.2 (6.28) | 15.33 (8.67) |
| Emotions | 18.2 (5.29) | 14.25 (6.70) |
| Games | 10.5 (529) | 6.56 (4.95) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Buche, H.; Michel, A.; Blanc, N. Using Virtual Reality During Chemotherapy to Support Emotional Regulation in Patients: Adding an Olfactory Reinforcement or Not? Virtual Worlds 2025, 4, 16. https://doi.org/10.3390/virtualworlds4020016
Buche H, Michel A, Blanc N. Using Virtual Reality During Chemotherapy to Support Emotional Regulation in Patients: Adding an Olfactory Reinforcement or Not? Virtual Worlds. 2025; 4(2):16. https://doi.org/10.3390/virtualworlds4020016
Chicago/Turabian StyleBuche, Hélène, Aude Michel, and Nathalie Blanc. 2025. "Using Virtual Reality During Chemotherapy to Support Emotional Regulation in Patients: Adding an Olfactory Reinforcement or Not?" Virtual Worlds 4, no. 2: 16. https://doi.org/10.3390/virtualworlds4020016
APA StyleBuche, H., Michel, A., & Blanc, N. (2025). Using Virtual Reality During Chemotherapy to Support Emotional Regulation in Patients: Adding an Olfactory Reinforcement or Not? Virtual Worlds, 4(2), 16. https://doi.org/10.3390/virtualworlds4020016







