Abstract
Because psychedelics have been found to increase psychological traits like openness, mental flexibility, and interpersonal perceptiveness, some researchers believe that psychedelics could help individuals cope with the psychological effects of discrimination. However, it is still unclear whether psychedelic use can help manage the internalized stigma that deters formal mental health treatment. This study investigates the impact of six measures of psychedelic use (MDMA, psilocybin, DMT, ayahuasca, peyote/mescaline, and LSD) on psychological distress (Kessler Psychological Distress Scale) and internalized stigma. The study used data from the National Survey of Drug Use and Health (NSDUH) from 2008 to 2019, with a sample size of 458,372 participants. Ordinary least square regression models were conducted using Stata 18. Gender analysis found that among men, ayahuasca use was linked to reduced stigma perception associated with higher distress. For women, DMT use was linked to reduced stigma perceptions when experiencing higher distress. However, results find that individuals who have used MDMA and psilocybin reported heightened perceptions of stigma associated with increased psychological distress. Among women, MDMA and psilocybin use was associated with a higher perception of stigma when they experienced distress. These findings suggest that, overall, psychedelics may not reduce the impact of distress on the perception of stigma, especially for women.
1. Introduction
Because psychedelics have been linked to mental health improvements [1,2,3], which are often explained through changes in psychological dispositions, including improved communication, emotion processing, self-regulation, openness, and interpersonal perceptiveness [4,5,6,7,8,9,10], some researchers have postulated that psychedelics may help manage the psychological effects of discrimination that can exacerbate mental health issues. Indeed, some research has found that psychedelics can help manage the consequences of perceived racial discrimination, whereby past experiences of discrimination were less distressing among psychedelic users [11,12,13].
However, it is yet to be determined whether psychedelics can help people manage the internalized stigma attached to mental illness that hinders help-seeking behavior [14]. While public stigma refers to discrimination that can result in the loss of resources [15,16], self-stigma refers to the internalization of discrimination that disempowers and reduces self-mastery, increases psychological distress, and leads to more negative coping strategies, including drinking, smoking, substance use, and avoidance of formal treatment [14,17,18,19,20,21]. If psychedelics can positively impact internalized perceptions of discrimination [22,23,24,25,26,27,28,29], psychedelics may help diminish the harmful psychological consequences of the stigma attached to mental illness in several ways. First, psychedelic use may help people reconceptualize their internalized negative beliefs, which may enable them to disregard or diminish the impact of stigma, thereby feeling less distressed. Second, those who have used psychedelics and are less threatened by the stigma attached to their mental illness may then be more likely to engage positively with their social world or access resources, further offsetting the negative consequences of the stigma that drives harmful behaviors.
However, it is also worth considering that the stigma attached to mental illness may have such detrimental effects on a person’s health and well-being that psychedelics might not counteract it; rather, the stigma attached to mental illness may lead some people to self-medicate with psychedelics. Ample evidence finds that stigma remains a significant barrier to mental health care, as it encourages individuals to remain silent about their problems, avoid seeking formal treatment, and often drives people to negative behaviors [14,15,16,19,30,31] More specifically, those who perceive more stigma are also more likely to use negative coping strategies to deal with their mental health issues, including seeking illicit substances [19,32]. Given the growing collective knowledge of effects on health, it is equally possible that instead of psychedelics managing stigma, discrimination leads to higher perceptions of the stigma attached to mental illness, higher levels of psychological distress, and in turn, drives people into harmful behaviors including self-medicating with psychedelics. Moreover, psychedelics are “mind-manifesting”, enlarging a person’s personal experience [33]. More specifically, while psychedelics can moderate perceptions of a person’s lived reality, providing clarity that could lead to different personal behaviors, psychedelics cannot erase past or ongoing experiences of discrimination. Thus, even if perceptions are changed, the real-world consequences of discrimination remain prevalent and would likely continue to lead to psychological deterioration, which would drive different perceptions and behaviors across groups who experience different types and levels of discrimination.
Real-world discrimination’s impact on creating negative perceptions is important considering the increased discrimination faced by women in multiple contexts, such as lower economic power, increased domestic labor, higher levels of gender-based violence [34,35,36,37], and increased stigma and discrimination in the field of medicine [38,39,40]. The theory of minorities’ diminished psychedelic returns (MDPR) suggests that structural inequalities can negatively impact the effectiveness of psychedelics on health, behaviors, and internalized beliefs [41,42,43,44]. It argues that cultural and structural inequalities can hinder access to resources and expose individuals to trauma or stress, resulting in diminished outcomes. Additionally, individuals with compromised conditions may lack the necessary factors for optimal health outcomes associated with psychedelic use or may have conditions that discourage positive use [43,44,45,46]. Systemic inequality may also lead marginalized psychedelic users to perceive more stigma, particularly during times of heightened distress, due to increased discrimination [47]. Given the increased gender-based discrimination in their everyday lives, MDPR suggests that women are less likely than men to have a decrease in perceived stigma associated with using psychedelics [40].
This paper explores the relationship between psychedelics, stigma perceptions, distress, and gender using data from the National Survey of Drug Use and Health (NSDUH) from 2008 to 2019, with a sample size of 458,372 participants. Ordinary least square regression models were conducted using Stata 18. The study aims to determine whether psychedelic use is linked to reduced perception of stigma for those who may be experiencing heightened levels of psychological distress or if stigma leads to more distress, potentially driving psychedelic use through self-medication. Overall, results only found minor evidence that psychedelic use is associated with a reduction in perceptions of stigma: among men, ayahuasca was linked to reduced stigma perception, while among women, DMT was associated with reduced stigma perceptions when they experienced higher distress. Rather, this study observed a notable negative correlation between stigma and psychedelic substance use. Among the total population, those using MDMA and psilocybin reported heightened perceptions of stigma associated with increased distress. Among women, MDMA and psilocybin users reported higher stigma associated with higher distress. These findings underscore the negative impact of stigma on distress and psychedelic use and gender-based disparities in the impact of psychedelics on stigma perception, with potential implications for negative treatment-seeking behaviors in mental health.
2. Data and Methods
This study analyzed pooled data from the National Survey of Drug Use and Health (NSDUH) conducted from 2008 to 2019 (n = 458,372). The NSDUH is an annual nationwide survey that measures substance use and mental health issues in the United States. The data was weighted to accurately represent the population. Descriptive statistics for the variables were obtained from publicly available data files on the NSDUH home page. Since this study used anonymous, publicly available data, no ethics approval or consent was required.
2.1. Study Replications
This study replicates previous research on psychedelic use and health outcomes using the NSDUH [3,10,46,48,49,50]. Where it differs is it explores previously unknown relationships between psychedelics, stigma, and gender. The study closely adheres to the statistical procedure used in over a dozen other papers analyzing psychedelics and outcomes using the NSDUH, including similar dependent, independent, and sociodemographic control variables.
2.2. Key Dependent Variable: Stigma
This study used seven variables from the NSDHU to create a continuous measure of the stigma attached to mental illness. First, the NSDUH asked participants if they had needed formal mental health treatment in the past year and if they missed it. Among those who missed treatment, participants were then provided five binary measures that indicated possible reasons for missing treatment: (1) “fear of neighbors’ negative opinion”, (2) “fear of negative effect on job”, (3) “confidentiality concerns”, (4) “fear of being committed/forced to use meds”, and (5) “didn’t want others to find out”. Participants were then provided a sixth variable that asked them to identify the most important reason for not seeking treatment from a list of options. This sixth variable was coded as a binary variable for stigma if a participant indicated any of the following options caused them to miss treatment: “afraid of diagnosis”, “others were unsupportive”, “ashamed or embarrassed, afraid, or sign of weakness”, “too stubborn/prideful”, “unmotivated, depressed, confused, angry, unworthy”, “concerned with treatment from the court system”, and “concerned with future insurability”. The six variables were added to create the continuous measure of stigma which ranges 0 to 6 [51,52,53,54,55]. Because “0” indicates that a person did not miss treatment, the analysis then included “missed treatment” (yes vs. no) as a control variable for all regression analyses.
2.3. Key Independent Variables: Gender, Psychological Distress, and Psychedelic Use
First, gender is a binary variable (women versus men). Next, Respondents utilized the Kessler Psychological Distress Scale (K6) [56,57] to indicate their level of distress in the past month, which ranges from 0–24 and is a reliable and valid measure of psychological distress in various mental health disorders [58,59]. The analysis measures drug use by asking respondents if they have ever used MDMA, DMT, ayahuasca, psilocybin, LSD, mescaline, or peyote. DMT, ayahuasca, psilocybin, LSD, mescaline, and peyote are classic psychedelics [60,61]. One exception is MDMA, which produces psychedelic effects by flooding the brain with serotonin and has been associated with positive mental health outcomes [3,29,62,63,64,65]. Consistent with previous research [48,66], the six classic psychedelics were used to create a dummy variable indicating any lifetime classic psychedelic use (LCPU) (yes vs. no). The NSDUH includes questions on DMT use, both lifetime use and use of DMT, AMT, or 5-MeO-DIPT. The second question was not included, as AMT and 5-MeO-DIPT are not considered classic psychedelics. Additionally, I followed a recommendation run analysis with both the combined LCPU variables and each individual drug use measure to account for potential socioeconomic and cultural differences in drug use [67,68,69,70,71]. Mescaline and peyote are grouped together as they share similar origins and social contexts [72,73].
2.4. Socioeconomic, Demographic, and Drug Use Control Variables
Continuous sociodemographic control variables include age, household income, and educational attainment. Marital status includes married, widowed, divorced/separated, and single (never married). Race/ethnicity includes non-Hispanic African American, non-Hispanic Native American/Alaska Native, non-Hispanic Native Hawaiian/Pacific Islander, non-Hispanic Asian, non-Hispanic more than one race, Hispanic, and non-Hispanic white (reference). Religiosity variables include religious attendance and religious salience [74]. The analysis controls for survey year, lifetime use of other drugs (cocaine, marijuana, PCP, inhalants, other stimulants, sedatives, pain relievers, and tobacco), age of first alcohol use, and self-reported risky behavior.
2.5. Analytic Strategy
In order to analyze the study’s questions, the analysis first reported the descriptive statistics (Table 1). Then, it computed the mean for each variable related to psychedelic use and used a post-estimation LINCOM command to determine the statistical difference between the two subpopulations [75]. The statistical mean difference was calculated for all key outcome variables for those for women minus (−) men (Table 2). Then, for testing the empirical predictions, a series of analyses were conducted using ordinary least square regression models (Supplemental Tables S1–S3). The first models investigated the impact of MDMA and LCPU on stigma. The next model adds psychological distress. Model 3 included the interaction between LCPU and psychological distress. Model 4 examines the effects of all six psychedelic variables on stigma. Model 5 then adds psychological distress to this analysis. The subsequent models (6–11) test the interaction between each psychedelic variable and psychological distress on stigma. Lastly, using an intersectional approach, the analysis runs individual models by gender to compare meaningful profiles [76]. Statistical difference of coefficients is assessed using post-estimation SUEST commands, allowing for generalized Hausman specification tests [77]. The analysis incorporates NSDUH weights and complex study design in STATA 17, using pooled data from 2008–2019. Multiple comparison control was not performed, as it is not required based on the study’s characteristics [78].

Table 1.
Descriptive Statistics for Dependent, Independent, and Control Variables (2008–2019) (weighted).

Table 2.
Mean Difference of Dependent, Independent, and Control Variables by Gender (Weighted).
3. Results
3.1. Descriptive Statistics
Mean differences of outcome variables by psychedelic use (Table 2) show women perceive higher levels of stigma, have higher levels of distress, and are less likely to use MDMA, psilocybin, DMT, peyote/mescaline, and LSD (p < 0.001). There was no gender difference in ayahuasca use. Additionally, compared to men, women also had lower family income, more education, and were less likely to use any drug except for sedatives and tranquilizers (p < 0.001). Women also had higher religious scores and were less likely to be married or single but more likely to be widowed and divorced (p < 0.001).
3.2. Do Psychedelic Users Perceive Less Stigma?
Regression analysis reveals that among the total population (Supplemental Table S1), only MDMA was associated with lower perceptions of stigma, but only when controlling for psychological distress (Model 5, b = −0.0104, p < 0.05) (Figure 1). No other psychedelics were independently associated with stigma. The gender analysis found that among men (Supplemental Table S2), DMT was independently associated with more stigma regardless of controlling for distress (Model 5, b = 0.173, p < 0.1), but at 0.1 level, this relationship is not that significant. Additionally, for men, peyote/mescaline was associated with less stigma (Model 4, b = −0.00689, p < 0.05), which lost significance when the model included psychological distress (Figure 2). Among women (Supplemental Table S3), mainline effects in the regression analysis showed that MDMA (Model 2, b = −0.0152, p < 0.05) was associated with less stigma, but only when controlling for distress. On the other hand, DMT was also associated with less stigma among women (Model 4, b = −0.068, p < 0.05), which lost significance when controlling for psychological distress (Figure 3). Results only found minor evidence that psychedelic use is independently associated with less stigma, and contrary to the predictions, there were more instances where women users perceived less stigma.
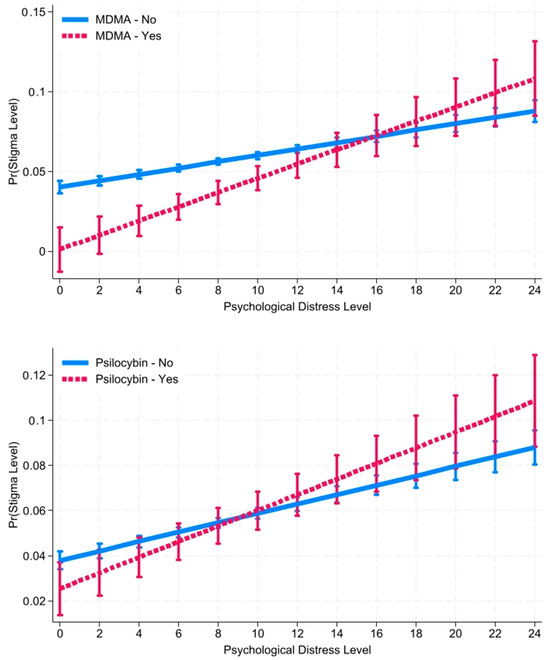
Figure 1.
Predicted Margins of MDMA and Psilocybin* Level of Psychological Distress in the Past Month on Level of Perceived Stigma for the Total Population with 95% CIs. Source: National Survey of Health and Social Behaviors, 2008–2019. Note: Based on Model 6 and 7, Supplemental Table S1, multinomial OLS regression model predicting level of perceived Stigma for the Total Population.
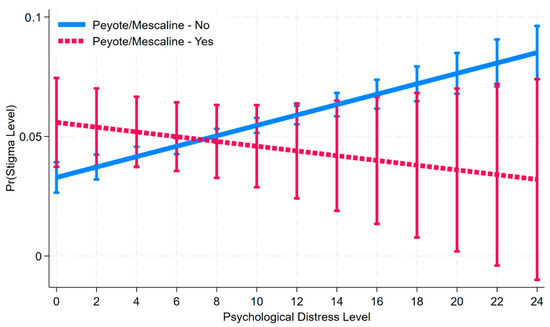
Figure 2.
Predicted Margins of Peyote/Mescaline * Level of Psychological Distress in the Past Month on Level of Perceived Stigma Among Men with 95% CIs. Source: National Survey of Health and Social Behaviors, 2008–2019. Note: Based on Model 10, Supplemental Table S2, multinomial OLS regression model predicting level of perceived Stigma Among Men.
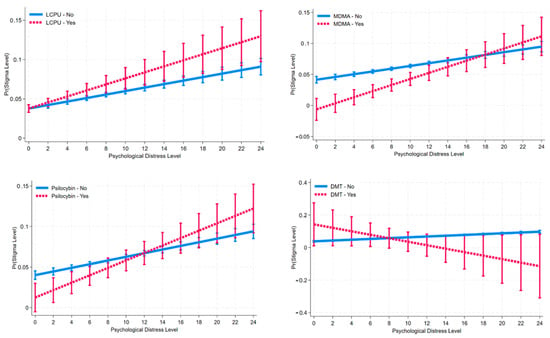
Figure 3.
Predicted Margins of LCPU, MDMA, Psilocybin, DMT * Level of Psychological Distress in the Past Month on Level of Perceived Stigma Among Women with 95% CIs. Source: National Survey of Health and Social Behaviors, 2008–2019. Note: Based on Models 3, 6, 7 and 8, Supplemental Table S3, multinomial OLS regression model predicting level of perceived Stigma Among Women.
3.3. Does Psychedelic Use Moderate Distress on Stigma?
Among men who have used peyote/mescaline (Model 10, b = −0.00317, p < 0.01), high levels of distress were associated with less stigma. Similarly, among women and men who have used DMT (Model 8, b = −0.0132, p < 0.05), high levels of distress were associated with less stigma.
However, among the total population (Supplemental Table S1), interaction terms revealed that among MDMA (Model 6, b = 0.00247, p < 0.01) and psilocybin users (Model 7, b = 0.00138, p < 0.05), as levels of distress increased, so did their perceptions of stigma. Among men (Supplemental Table S2), MDMA users perceived more stigma as distress increased (Model 6, b = 0.00211, p < 0.1), but only at the 0.1 level. Among women (Supplemental Table S3), both MDMA (Model 6, b = 0.00268, p < 0.01) and psilocybin users (Model 7, b = 0.00233, p < 0.01) were associated with higher levels of stigma as distress increased.
Overall, the analysis provides little support for the prediction that psychedelic use is associated with reduced perceptions of stigma as distress increases. There were only two instances that supported the hypotheses: peyote/mescaline for men and DMT for women. Moreover, there was some evidence of the diminished psychedelics returns hypothesis concerning gender; there were more instances where psychedelics were associated with more stigma as distress increased for women compared to men.
4. Discussion
This study examines the relationship between psychedelics, stigma, distress, and gender. Previous research suggests that psychedelics may have positive effects on health and well-being. Some theories propose that psychedelics can change perceptions and help individuals cope with the psychological effects of discrimination. If psychedelics can help manage internalized stigma, they could be a valuable tool in promoting positive treatment outcomes. Results indicated that only a few substances were independently associated with lower perceived stigma. Among women, MDMA was associated with less internalized stigma. However, as women experienced more distress, LCPU, MDMA, and psilocybin users perceived more stigma, while DMT users perceived less. Among men, peyote/mescaline use was linked to less stigma and appeared to moderate perceptions of stigma as distress increased. Overall, results indicate there were more instances in which psychedelic use was associated with higher perceptions of stigma than lower perceptions, suggesting psychedelics may provide little stigma management among the general population.
Moreover, results revealed gender disparity in the relationship between psychedelics and perception of stigma, which adds to the growing evidence that the benefits of psychedelics on health outcomes appear to be diminished among marginalized subpopulations, including by race, socioeconomic status, employment status, educational level, marital status, and religious participation [2,42,43,44,45,79]. The perception of increased stigma among women who use MDMA and psilocybin when they are distressed may be partially explained by a combination of stigmas and negative coping mechanisms. Women not only face more discrimination, but they also experience higher levels of stigma associated with drug use. A meta-analysis using mixed methods revealed that women who used drugs such as marijuana, heroin, cocaine, amphetamines, and alcohol were more likely to be stigmatized [80]. This analysis also found that women’s drug use was often negatively perceived, leading to expectations of promiscuity and stereotypes related to womanhood, which directly affected their treatment in healthcare settings and increased the risk of gender-based violence. In contrast, there is evidence suggesting that substance use among men is often socially celebrated. For example, men who drink, smoke, or use illicit drugs, including opioids and marijuana, may be seen as exhibiting positive masculinity [81,82]. Consequently, women who are distressed and stigmatized in medical contexts may turn to substances that are themselves highly stigmatized as a form of self-medication. When comparing their experiences to those of men, it is evident that men are more likely to receive positive messages about psychedelics and may be more inclined to openly discuss their experiences with these drugs.
Unfortunately, the study found that psychedelic users perceived more stigma as they became more distressed, particularly with drugs like MDMA and psilocybin. This suggests that stigma may hinder the potential therapeutic benefits of psychedelics. Moreover, individuals may be using psychedelics as a form of self-medication due to fear of stigma associated with mental illness. This raises concerns about the potential consequences for those with mental illnesses that may have adverse reactions to psychedelics [83,84]. Research suggests that psychedelic use may be harmful for individuals with schizophrenia or bipolar syndrome [85,86]. Stigma not only drives individuals toward self-medication but also puts those with a personal or family history at risk. Women may be particularly affected by these patterns. Policymakers and healthcare advocates should approach this issue with caution to avoid unintended negative consequences.
The study only found two instances in which psychedelic use was linked to better stigma management: DMT for women and peyote/mescaline for men, even though these drugs are chemically identical. It is important to note that this study is a population study, which means that it is capturing social differences and differences in use, which are likely to explain these gendered differences; there may be other factors influencing the results, as expected within our theoretical framework. On the other hand, most psychedelic health research is conducted in clinical settings, allowing for careful control. In these settings, participants receive comprehensive psychological counseling before being administered the drugs. The counseling aims to identify sources of stress, establish a positive relationship with counselors, and create a safe and trusting environment [5]. Since these population studies capture cultural differences in drug use, we should also anticipate that in carefully controlled settings similar to clinics, all chemically identical drugs should produce a relationship with stigma, even if this particular study did not find it. Therefore, the small but significant positive relationship in which psychedelic diminish the impact of distress on stigma, DMT for women and peyote/mescaline for men, suggests there may be potential to reduce negative perceptions of discrimination. Future research should focus on understanding these specific relationships within the general population and answer why this gender specific substance seeming provided positive results.
5. Limitations and Future Directions
This study has limitations, including the exclusion of certain influential factors like personality traits, peak experiences, and dosage. Additionally, there may be unmeasured variables influencing the relationship between stigma, psychedelics, and distress. Future research should use longitudinal data, consider the timing of psychedelic use, and employ comprehensive measures of public and personal stigma. The General Social Survey’s mental health modules and the “Why Try Stigma Scale” are potential tools for further exploration [87,88].
Additionally, this study does not consider the cultural factors that can impact the stigma surrounding mental illness and psychedelic use. While this study is the first to analyze the statistical connection between psychedelics and the stigma attached to mental illness, there may be other variables, such as cultural and economic conditions, that could further explain these findings or reveal additional differences within subcultures. It is important to acknowledge that the quality of stigma varies greatly depending on factors like poverty, types of traumas, and race/ethnicity [82,89]. Despite the growing acceptance of psychedelics, stigma remains prevalent, as seen in the ongoing stigma surrounding marijuana use. Furthermore, the stigma associated with drug use is not evenly distributed across different social statuses, including gender, age, marital status, or history of sexual trauma. Therefore, it is crucial to examine how cultural patterns related to race/ethnicity and mental health stigma may also influence various patterns of self-medication involving psychedelics.
Most importantly, this study cannot establish causal relationships. Clinical use of psychedelics is for health benefits, while naturalistic use may vary. The paper applies a modified theory of cultural set and setting to show how cultural differences affect drug effectiveness and behaviors. It aims to demonstrate broader epidemiological patterns. Future research can explore the implications of stigma findings on treatment seeking. Psychedelics marginally reduce stigma perceptions, potentially improving health seeking. However, users also experience higher levels of stigma, suggesting less formal treatment utilization, which needs to be explored.
Despite its limitations, this study provides valuable insights into the relationship between psychedelics and health, considering the sociocultural conditions surrounding their use. Recreational psychedelic use among college students increased from 5% to 9% between 2019 and 2021 [90], and over seven million individuals used hallucinogens in 2020 [91]. With the increasing availability of psychedelics, naturalistic use will surpass clinical treatment, particularly in regions with limited mental health resources and stigma. Incorporating a modified theory of cultural set and setting can help understand how individuals facing discrimination and limited access to healthcare may resort to negative coping strategies involving psychedelics. Stigma affects behaviors, and society plays a significant role in the effectiveness of psychedelics, highlighting that they are not a cure-all for health outcomes. The idea of psychedelic exceptionalism, prioritizing drug law reforms based on health benefits, needs reevaluation as it neglects systemic inequality [92].
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/psychoactives3020019/s1, Table S1: Weighted Multivariate Ordinary Least Square Regression Predicting the Level of Perceived Stigma Among the Total Population; Table S2: Weighted Multivariate Ordinary Least Square Regression Predicting the Level of Perceived Stigma Among Men; Table S3: Weighted Multivariate Ordinary Least Square Regression Predicting the Level of Perceived Stigma Among Women.
Funding
This research received no external funding.
Institutional Review Board Statement
Since this study used anonymous, publicly available data, no ethics approval or consent was required per the IRB of The UNiersity of the Incarnate Word.
Informed Consent Statement
Not Applicable.
Data Availability Statement
The National Survey of Drug Use and Health (NSDUH) is public-use data and is available on their home page: https://www.datafiles.samhsa.gov/dataset/nsduh-2002-2019-ds0001-nsduh-2002-2019-ds0001.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Luoma, J.B.; Chwyl, C.; Bathje, G.J.; Davis, A.K.; Lancelotta, R. A Meta-Analysis of Placebo-Controlled Trials of Psychedelic-Assisted Therapy. J. Psychoact. Drugs 2020, 52, 289–299. [Google Scholar] [CrossRef] [PubMed]
- Jones, G.M.; Nock, M.K. Race and Ethnicity Moderate the Associations between Lifetime Psychedelic Use (MDMA and Psilocybin) and Psychological Distress and Suicidality. Sci. Rep. 2022, 37, 61–69. [Google Scholar] [CrossRef] [PubMed]
- Jones, G.M.; Nock, M.K. MDMA/Ecstasy Use and Psilocybin Use Are Associated with Lowered Odds of Psychological Distress and Suicidal Thoughts in a Sample of US Adults. J. Psychopharmacol. 2022, 36, 46–56. [Google Scholar] [CrossRef] [PubMed]
- Maclean, K.A.; Johnson, M.W.; Griffiths, R.R. Mystical experiences occasioned by the hallucinogen psilocybin lead to increases in the personality domain of openness. J. Psychoph. 2011, 25, 1453–1461. [Google Scholar] [CrossRef]
- Griffiths, R.R.; Richards, W.A.; McCann, U.; Jesse, R. Psilocybin Can Occasion Mystical-Type Experiences Having Substantial and Sustained Personal Meaning and Spiritual Significance. Psychopharmacology 2006, 187, 268–283. [Google Scholar] [CrossRef] [PubMed]
- Mans, K.; Kettner, H.; Erritzoe, D.; Haijen, E.C.H.M.; Kaelen, M.; Carhart-Harris, R.L. Sustained, Multifaceted Improvements in Mental Well-Being Following Psychedelic Experiences in a Prospective Opportunity Sample. Front. Psychiatry 2021, 12, 647909. [Google Scholar] [CrossRef] [PubMed]
- Payne, J.E.; Chambers, R.; Liknaitzky, P. Combining Psychedelic and Mindfulness Interventions: Synergies to Inform Clinical Practice. In ACS Pharmacology and Translational Science; American Chemical Society: Washington, DC, USA, 2021; pp. 416–423. [Google Scholar] [CrossRef]
- Søndergaard, A.; Madsen, M.K.; Ozenne, B.; Armand, S.; Knudsen, G.M.; Fisher, P.M.D.; Stenbæk, D.S. Lasting Increases in Trait Mindfulness after Psilocybin Correlate Positively with the Mystical-Type Experience in Healthy Individuals. Front. Psychol. 2022, 13, 948729. [Google Scholar] [CrossRef] [PubMed]
- dos Santos, R.G.; Bouso, J.C.; Alcázar-Córcoles, M.Á.; Hallak, J.E.C. Efficacy, Tolerability, and Safety of Serotonergic Psychedelics for the Management of Mood, Anxiety, and Substance-Use Disorders: A Systematic Review of Systematic Reviews. In Expert Review of Clinical Pharmacology; Taylor and Francis Ltd.: Oxfordshire, UK, 2018; pp. 889–902. [Google Scholar] [CrossRef]
- Hendricks, P.S.; Thorne, C.B.; Clark, C.B.; Coombs, D.W.; Johnson, M.W. Classic Psychedelic Use Is Associated with Reduced Psychological Distress and Suicidality in the United States Adult Population. J. Psychopharmacol. 2015, 29, 280–288. [Google Scholar] [CrossRef] [PubMed]
- Ching, T.H.W.; Davis, A.K.; Xin, Y.; Williams, M.T. Effects of Psychedelic Use on Racial Trauma Symptoms and Ethnic Identity among Asians in North America. J. Psychoact. Drugs 2023, 55, 19–29. [Google Scholar] [CrossRef]
- Williams, D.R. Stress and the Mental Health of Populations of Color: Advancing Our Understanding of Race-Related Stressors. J. Health Soc. Behav. 2018, 59, 466–485. [Google Scholar] [CrossRef]
- Williams, D.Z. Examining the Relationship between Race-Related Stressors and Post-Traumatic Stress Disorder among African American; Washington State University, College of Education: Washington, DC, USA, 2007. [Google Scholar]
- Goffman, E. Stigma: Notes on the Management of Spoiled Identity; Simon & Schuster, Inc.: New York, NY, USA, 1963. [Google Scholar]
- Link, B.G.; Phelan, J.C. Conceptualizing Stigma. Annu. Rev. Sociol. 2001, 27, 363–385. [Google Scholar] [CrossRef]
- Link, B.G.; Phelan, J.C. Labeling and Stigma. In Handbook of the Sociology of Mental Health; Aneshensel, C.S., Phelan, J.C., Bierman, A., Eds.; Springer: Dordrecht, The Netherlands, 2013; pp. 525–541. [Google Scholar] [CrossRef]
- Levy, B.R.; Pilver, C.E. Residual Stigma: Psychological Distress among the Formerly Overweight. Soc. Sci. Med. 2012, 75, 297–299. [Google Scholar] [CrossRef] [PubMed]
- Corrigan, P.W.; Watson, A.C. The Paradox of Self-Stigma and Mental Illness. Clin. Psychol. Sci. Pract. 2002, 9, 35–53. [Google Scholar] [CrossRef]
- Pescosolido, B.A.; Martin, J.K. The Stigma Complex. Annu. Rev. Sociol. 2015, 41, 87–116. [Google Scholar] [CrossRef] [PubMed]
- Pescosolido, B.A.; Halpern-Manners, A.; Luo, L.; Perry, B. Trends in Public Stigma of Mental Illness in the US, 1996–2018. JAMA Netw. Open 2021, 4, e2140202. [Google Scholar] [CrossRef] [PubMed]
- Pescosolido, B.A. The Public Stigma of Mental Illness: What Do We Think; What Do We Know; What Can We Prove? J. Health Soc. Behav. 2013, 54, 1–21. [Google Scholar] [CrossRef] [PubMed]
- Williams, M.T.; Cabral, V.; Faber, S. Psychedelics and Racial Justice. Int. J. Ment. Health Addict. 2023, 1–17. [Google Scholar] [CrossRef]
- Thrul, J.; Garcia-Romeu, A. Whitewashing Psychedelics: Racial Equity in the Emerging Field of Psychedelic-Assisted Mental Health Research and Treatment. In Drugs: Education, Prevention and Policy; Taylor and Francis Ltd.: Oxfordshire, UK, 2021; pp. 211–214. [Google Scholar] [CrossRef]
- Neitzke-Spruill, L. Race as a Component of Set and Setting: How Experiences of Race Can Influence Psychedelic Experiences. J. Psychedelic Stud. 2019, 4, 51–60. [Google Scholar] [CrossRef]
- Korman, B.A. Could Classic Psychedelics Influence Immigrants’ Acculturation Process? A Narrative Review Contemplating How. Drug Sci. Policy Law 2023, 9, 20503245231191400. [Google Scholar] [CrossRef]
- Carlin, S. MDMA Therapy Training for Communities of Color. MAPS Bull. Res. 2020, 30, 12–18. [Google Scholar]
- Williams, M.T. Race-Based Trauma: The Challenge and Promise of MDMA-Assisted Psychotherapy; 2016. Available online: https://www.researchgate.net/publication/300920255 (accessed on 1 February 2024).
- Michaels, T.I.; Purdon, J.; Collins, A.; Williams, M.T. Inclusion of People of Color in Psychedelic-Assisted Psychotherapy: A Review of the Literature. BMC Psychiatry 2018, 18, 245. [Google Scholar] [CrossRef] [PubMed]
- Williams, M.T.; Reed, S.; Aggarwal, R. Culturally Informed Research Design Issues in a Study for MDMA-Assisted Psychotherapy for Posttraumatic Stress Disorder. J. Psychedelic Stud. 2019, 4, 40–50. [Google Scholar] [CrossRef]
- Link, B.G.; Cullen, F.T.; Struening, E.; Shrout, P.E.; Dohrenwend, P.B. A Modified Labeling Theory Approach to Mental Disorders: An Empirical Assessment Published. Am. Sociol Rev. 1989, 54, 400–423. [Google Scholar] [CrossRef]
- Borenstein, J. Stigma, Prejudice and Discrimination Against People with Mental Illness; American Psychiatric Assocation: Washington, DC, USA, 2020; Available online: https://www.psychiatry.org/patients-families/stigma-and-discrimination (accessed on 1 February 2024).
- Pescosolido, B.A.; Medina, T.R.; Martin, J.K.; Long, J.S. The “Backbone” of Stigma: Identifying the Global Core of Public Prejudice Associated with Mental Illness. Am. J. Public Health 2013, 103, 853–860. [Google Scholar] [CrossRef] [PubMed]
- Noorani, T. Containment Matters: Set and Setting in Contemporary Psychedelic Psychiatry. Philos. Psychiatry Psychol. 2021, 28, 201–216. [Google Scholar] [CrossRef]
- Doering, L.; Thébaud, S. The Effects of Gendered Occupational Roles on Men’s and Women’s Workplace Authority: Evidence from Microfinance. Am. Sociol Rev. 2017, 82, 542–567. [Google Scholar] [CrossRef]
- Harder, B.M.; Sumerau, J.E. Understanding Gender as a Fundamental Cause of Health: Simultaneous Linear Relationships between Gender, Mental Health, and Physical Health over Time. Sociol. Spectr. 2018, 38, 387–405. [Google Scholar] [CrossRef]
- Hochschild, A.; Machung, A. The Second Shift: Working Families and the Revolution at Home, 3rd ed.; Penguin Books Ltd.: London, UK, 2012. [Google Scholar]
- WHO. Global, Regional, and National Prevalence Estimates for Intimate Partner Violence against Women and Global and Regional Prevalence Estimates for Non-Partner Sexual Violence against Women; WHO: Geneva, Switzerland, 2018. [Google Scholar]
- Naaman, E.; Gelfand Saar, L.; Naftali Ben-Haim, L.; Barak, Y.; Bar, N.; Labardini, C.; Soudry, S. Examination of Inattentive Gender Bias in Medicine: Patients’ Form of Addressing Male and Female Physicians. Cogent. Soc. Sci. 2022, 8, 2136605. [Google Scholar] [CrossRef]
- Monzani, D.; Vergani, L.; Pizzoli, S.F.M.; Marton, G.; Mazzocco, K.; Bailo, L.; Messori, C.; Pancani, L.; Cattelan, M.; Pravettoni, G. Sexism Interacts with Patient–Physician Gender Concordance in Influencing Patient Control Preferences: Findings from a Vignette Experimental Design. Appl. Psychol. Health Well Being 2020, 12, 471–492. [Google Scholar] [CrossRef]
- Champagne-Langabeer, T.; Hedges, A.L. Physician Gender as a Source of Implicit Bias Affecting Clinical Decision-Making Processes: A Scoping Review. BMC Med. Educ. 2021, 21, 171. [Google Scholar] [CrossRef]
- Hartogsohn, I. Set and Setting, Psychedelics and the Placebo Response: An Extra-Pharmacological Perspective on Psychopharmacology. J. Psychopharmacol. 2016, 30, 1259–1267. [Google Scholar] [CrossRef]
- Viña, S.M. Minorities’ Diminished Psychedelic Returns: Cardio-Metabolic Health. Drug Sci. Policy Law 2024, 10, 1–13. [Google Scholar] [CrossRef]
- Viña, S.M.; Stephens, A.L. Minorities’ Diminished Psychedelic Returns. Drug Sci. Policy Law 2023, 9, 1–19. [Google Scholar] [CrossRef]
- Viña, S.M.; Stephens, A.L. Psychedelics and Workplace Harm. Front. Psychiatry 2023, 14, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Viña, S.M. Diminished Psychedelic Returns on Distress: Marital Status and Household Size. PLoS ONE 2024, 19, 1–23. [Google Scholar] [CrossRef]
- Viña, S. The Harmful Relationship Between Classic Psychedelic Use and Religion on Mental Health. In Proceedings of the American Sociological Association 117th Annual Meeting: Bureaucracies of Displacement, Los Angeles, CA, USA, 5–9 August 2022. [Google Scholar]
- Quinn, D.M.; Williams, M.K.; Weisz, B.M. From Discrimination to Internalized Mental Illness Stigma: The Mediating Roles of Anticipated Discrimination and Anticipated Stigma. Psychiatr. Rehabil. J. 2015, 38, 103–108. [Google Scholar] [CrossRef] [PubMed]
- Simonsson, O.; Sexton, J.D.; Hendricks, P.S. Associations between Lifetime Classic Psychedelic Use and Markers of Physical Health. J. Psychopharmacol. 2021, 35, 447–452. [Google Scholar] [CrossRef] [PubMed]
- Simonsson, O.; Hendricks, P.S.; Carhart-Harris, R.; Kettner, H.; Osika, W. Association between Lifetime Classic Psychedelic Use and Hypertension in the Past Year. Hypertension 2021, 77, 1510–1516. [Google Scholar] [CrossRef] [PubMed]
- Hendricks, P.S.; Crawford, M.S.; Cropsey, K.L.; Copes, H.; Sweat, N.W.; Walsh, Z.; Pavela, G. The Relationships of Classic Psychedelic Use with Criminal Behavior in the United States Adult Population. J. Psychopharmacol. 2018, 32, 37–48. [Google Scholar] [CrossRef]
- Choi, N.G.; DiNitto, D.M.; Marti, C.N. Treatment Use, Perceived Need, and Barriers to Seeking Treatment for Substance Abuse and Mental Health Problems among Older Adults Compared to Younger Adults. Drug Alcohol. Depend 2014, 145, 113–120. [Google Scholar] [CrossRef]
- Mason, M.J.; Keyser-Marcus, L.; Snipes, D.; Benotsch, E.; Sood, B. Perceived Mental Health Treatment Need and Substance Use Correlates among Young Adults. Psychiatr. Serv. 2013, 64, 871–877. [Google Scholar] [CrossRef] [PubMed]
- Rosner, B.; Neicun, J.; Yang, J.C.; Roman-Urrestarazu, A. Substance Use among Sexual Minorities in the US—Linked to Inequalities and Unmet Need for Mental Health Treatment? Results from the National Survey on Drug Use and Health (NSDUH). J. Psychiatr. Res. 2021, 135, 107–118. [Google Scholar] [CrossRef] [PubMed]
- Salameh, T.; Hall, L.; Crawford, T.; Hall, M. Perceived Barriers to Mental Health and Substance Use Treatment among US Childbearing-Aged Women: NSDUH 2008–2014. Women Health 2021, 61, 1007–1015. [Google Scholar] [CrossRef] [PubMed]
- Townsend, L.; Gearing, R.E.; Polyanskaya, O. Influence of Health Beliefs and Stigma on Choosing Internet Support Groups over Formal Mental Health Services. Psychiatr. Serv. 2012, 63, 370–376. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.C.; Green, J.G.; Gruber, M.J.; Sampson, N.A.; Bromet, E.; Cuitan, M.; Furukawa, T.A.; Oye, G.; Hinkov, H.; Hu, C.Y.; et al. Screening for Serious Mental Illness in the General Population with the K6 Screening Scale: Results from the WHO World Mental Health (WMH) Survey Initiative. Int. J. Methods Psychiatr. Res. 2010, 19 (Suppl. S1), 4–22. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.C.; Andrews, G.; Colpe, L.J.; Hiripi, E.; Mroczek, D.K.; Normand, S.L.T.; Walters, E.E.; Zaslavsky, A.M. Short Screening Scales to Monitor Population Prevalences and Trends in Non-Specific Psychological Distress. Psychol. Med. 2002, 32, 959–976. [Google Scholar] [CrossRef] [PubMed]
- Cotton, S.M.; Menssink, J.; Filia, K.; Rickwood, D.; Hickie, I.B.; Hamilton, M.; Hetrick, S.; Parker, A.; Herrman, H.; McGorry, P.D.; et al. The Psychometric Characteristics of the Kessler Psychological Distress Scale (K6) in Help-Seeking Youth: What Do You Miss When Using It as an Outcome Measure? Psychiatry Res. 2021, 305, 114182. [Google Scholar] [CrossRef] [PubMed]
- Umucu, E.; Fortuna, K.; Jung, H.; Bialunska, A.; Lee, B.; Mangadu, T.; Storm, M.; Ergun, G.; Mozer, D.A.; Brooks, J. A National Study to Assess Validity and Psychometrics of the Short Kessler Psychological Distress Scale (K6). Rehabil. Couns Bull. 2022, 65, 140–149. [Google Scholar] [CrossRef]
- Ly, C.; Greb, A.C.; Cameron, L.P.; Wong, J.M.; Barragan, E.V.; Wilson, P.C.; Burbach, K.F.; Soltanzadeh Zarandi, S.; Sood, A.; Paddy, M.R.; et al. Psychedelics Promote Structural and Functional Neural Plasticity. Cell Rep. 2018, 23, 3170–3182. [Google Scholar] [CrossRef]
- NIDA. MDMA (Ecstasy/Molly) Drug Facts. NIDA. MDMA (Ecstasy/Molly) DrugFacts. National Institute on Drug Abuse Website. Available online: https://nida.nih.gov/publications/drugfacts/mmdma-ecstasymolly (accessed on 15 October 2023).
- Mitchell, J.M.; Bogenschutz, M.; Lilienstein, A.; Harrison, C.; Kleiman, S.; Parker-Guilbert, K.; Ot’alora, G.M.; Garas, W.; Paleos, C.; Gorman, I.; et al. MDMA-Assisted Therapy for Severe PTSD: A Randomized, Double-Blind, Placebo-Controlled Phase 3 Study. Nat. Med. 2021, 27, 1025–1033. [Google Scholar] [CrossRef]
- Brewerton, T.D.; Wang, J.B.; Lafrance, A.; Pamplin, C.; Mithoefer, M.; Yazar-Klosinki, B.; Emerson, A.; Doblin, R. MDMA-Assisted Therapy Significantly Reduces Eating Disorder Symptoms in a Randomized Placebo-Controlled Trial of Adults with Severe PTSD. J. Psychiatr. Res. 2022, 149, 128–135. [Google Scholar] [CrossRef] [PubMed]
- Mithoefer, M.C.; Feduccia, A.A.; Jerome, L.; Mithoefer, A.; Wagner, M.; Walsh, Z.; Hamilton, S.; Yazar-Klosinski, B.; Emerson, A.; Doblin, R. MDMA-Assisted Psychotherapy for Treatment of PTSD: Study Design and Rationale for Phase 3 Trials Based on Pooled Analysis of Six Phase 2 Randomized Controlled Trials. Psychopharmacology 2019, 236, 2735–2745. [Google Scholar] [CrossRef] [PubMed]
- Ching, T.H.W.; Williams, M.T.; Wang, J.B.; Jerome, L.; Yazar-Klosinski, B.; Emerson, A.; Doblin, R. MDMA-Assisted Therapy for Posttraumatic Stress Disorder: A Pooled Analysis of Ethnoracial Differences in Efficacy and Safety from Two Phase 2 Open-Label Lead-in Trials and a Phase 3 Randomized, Blinded Placebo-Controlled Trial. J. Psychopharmacol. 2022, 36, 974–986. [Google Scholar] [CrossRef] [PubMed]
- Simonsson, O.; Osika, W.; Carhart-Harris, R.; Hendricks, P.S. Associations between Lifetime Classic Psychedelic Use and Cardiometabolic Diseases. Sci. Rep. 2021, 11, 10–14. [Google Scholar] [CrossRef] [PubMed]
- Clemens, K.J.; McGregor, I.S.; Hunt, G.E.; Cornish, J.L. MDMA, Methamphetamine and Their Combination: Possible Lessons for Party Drug Users from Recent Preclinical Research. Drug Alcohol Rev. 2007, 26, 9–15. [Google Scholar] [CrossRef] [PubMed]
- Rigg, K.K. Motivations for Using MDMA (Ecstasy/Molly) among African Americans: Implications for Prevention and Harm-Reduction Programs. J. Psychoact. Drugs 2017, 49, 192–200. [Google Scholar] [CrossRef] [PubMed]
- Palamar, J.J.; Keyes, K.M. Trends in Drug Use among Electronic Dance Music Party Attendees in New York City, 2016–2019. Drug Alcohol Depend. 2020, 209, 107889. [Google Scholar] [CrossRef] [PubMed]
- Johnstad, P.G. Who Is the Typical Psychedelics User? Methodological Challenges for Research in Psychedelics Use and Its Consequences. Nord. Stud. Alcohol Drugs 2021, 38, 35–49. [Google Scholar] [CrossRef] [PubMed]
- Viña, S.M. Socioeconomic Status and Minorities’ Diminished Psychedelic Return on Distress. J. Race Ethn. Health Disparities 2024. Accepted (Forthcoming). [Google Scholar]
- Jones, P.N. The Native American Church, Peyote, and Health: Expanding Consciousness for Healing Purposes. Contemp. Justice Rev. 2007, 10, 411–425. [Google Scholar] [CrossRef]
- Halpern, J.H.; Sherwood, A.R.; Hudson, J.I.; Yurgelun-Todd, D.; Pope, H.G. Psychological and Cognitive Effects of Long-Term Peyote Use among Native Americans. Biol. Psychiatry 2005, 58, 624–631. [Google Scholar] [CrossRef] [PubMed]
- Viña, S.M. Religion, Psychedelics, Risky Behavior, and Violence. J. Psychoact. Drugs 2024, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Long, J.S.; Freese, J. Regression Models for Categorical Dependent Variables Using Stata, 3rd ed.; Stata Press: College Station, TX, USA, 2014. [Google Scholar]
- Long, J.S. Group Comparisons in Logit and Probit Using Predicted Probabilities; Indiana University Bloomington: Bloomington, Indiana, 2009; Available online: http://www.indiana.edu/~jslsoc/files_research/groupdif/groupwithprobabilities/groups-with-prob-2009-06-25.pdf (accessed on 1 February 2024).
- Oberfichtner, M.; Tauchmann, H. Stacked Linear Regression Analysis to Facilitate Testing of Hypotheses across OLS Regressions. Stata J. Promot. Commun. Stat. Stata 2021, 21, 411–429. [Google Scholar] [CrossRef]
- Armstrong, R.A. When to Use the Bonferroni Correction. Ophthalmic Physiol. Opt. 2014, 34, 502–508. [Google Scholar] [CrossRef] [PubMed]
- Jones, G.M. Race and Ethnicity Moderate the Associations between Lifetime Psychedelic Use (MDMA/Ecstasy and Psilocybin) and Major Depressive Episodes. J. Psychopharmacol. 2023, 37, 61–69. [Google Scholar] [CrossRef] [PubMed]
- Meyers, S.A.; Earnshaw, V.A.; D’Ambrosio, B.; Courchesne, N.; Werb, D.; Smith, L.R. The Intersection of Gender and Drug Use-Related Stigma: A Mixed Methods Systematic Review and Synthesis of the Literature. Drug Alcohol Depend. 2021, 223, 108706. [Google Scholar] [CrossRef] [PubMed]
- Newhart, M.; Dolphin, W. The Medicalization of Marijuana: Legitimacy, Stigma, and the Patient Experience; Routledge: New York, NY, USA, 2019. [Google Scholar]
- Back, S.E.; Payne, R.L.; Wahlquist, A.H.; Carter, R.E.; Stroud, Z.; Haynes, L.; Hillhouse, M.; Brady, K.T.; Ling, W. Comparative Profiles of Men and Women with Opioid Dependence: Results from a National Multisite Effectiveness Trial. Am. J. Drug Alcohol Abus. 2011, 37, 313–323. [Google Scholar] [CrossRef] [PubMed]
- Cormier, Z. No Link Found between Psychedelics and Psychosis. Nature 2015. [Google Scholar] [CrossRef]
- Lenzenweger, M.F. Schizotypy, Schizotypic Psychopathology and Schizophrenia. World Psychiatry 2018, 17, 25–26. [Google Scholar] [CrossRef]
- Barber, G.; Nemeroff, C.B.; Siegel, S. A Case of Prolonged Mania, Psychosis, and Severe Depression After Psilocybin Use: Implications of Increased Psychedelic Drug Availability. Am. J. Psychiatry 2022, 179, 892–896. [Google Scholar] [CrossRef]
- Morton, E.; Sakai, K.; Ashtari, A.; Pleet, M.; Michalak, E.E.; Woolley, J. Risks and Benefits of Psilocybin Use in People with Bipolar Disorder: An International Web-Based Survey on Experiences of ‘Magic Mushroom’ Consumption. J. Psychopharmacol. 2023, 37, 49–60. [Google Scholar] [CrossRef] [PubMed]
- Pescosolido, B.A.; Martin, J.K.; Link, B.G.; Kikuzawa, S.; Burgos, G.; Swingle, R.; Phelan, J. Americans’ Views of Mental Health and Illness at Century’s End: Continuity and Change; Indiana University: Bloomington, IN, USA, 2006. [Google Scholar]
- Corrigan, P.W.; Nieweglowski, K.; Sayer, J. Self-Stigma and the Mediating Impact of the “Why Try” Effect on Depression. J. Community Psychol. 2019, 47, 698–705. [Google Scholar] [CrossRef] [PubMed]
- McGuffey, C.S. “Saving Masculinity”: Gender Reaffirmation, Sexuality, Race, and Parental Responses to Male Child Sexual Abuse. Soc. Probl. 2008, 55, 216–237. [Google Scholar] [CrossRef]
- NIH. National Survey on Drug Use and Health (NSDUH); NIH: Washington, DC, USA, 2021. [Google Scholar]
- SAMHSA Substance Abuse and Mental Health Service Administration. Key Substance Use and Mental Health Indicators in the United States: Results from the 2020 National Survey on Drug Use and Health. 2021. Available online: https://jslsoc.sitehost.iu.edu/files_research/groupdif/groupwithprobabilities/groups-with-prob-2009-05-28.pdf (accessed on 1 June 2023).
- Marlan, D. The Myth of Psychedelic Exceptionalism. Harvard Law: Bill of Health. Available online: https://blog.petrieflom.law.harvard.edu/2021/03/24/psychedelic-exceptionalism-drug-policy/ (accessed on 1 June 2023).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).