Abstract
Background: Undergraduate research is vital for developing critical thinking and academic identity in medical students, yet traditional models often fail to overcome institutional and personal barriers. Peer-led approaches may offer more accessible, supportive environments that promote deeper engagement and leadership in research. Methods: This study evaluated medical students’ experiences in a peer-led research initiative from 2022 to 2024. Students were then invited to complete a qualitative questionnaire reflecting on their perceptions towards research, development in research skills, confidence, and academic identity. Results: Code saturation was achieved after 9 responses (N = 15). Participants reported intrinsic interest, peer encouragement, and opportunities to publish as motivating factors. The peer-led model made research feel more approachable, fostering technical growth and academic confidence. Peer mentorship and a gradual learning structure were especially valued. While challenges such as workload and team dynamics emerged, students reported growth in resilience and self-reflection. Conclusions: Peer-led research initiatives can effectively support academic identity formation by integrating motivation, support, and skill development. Despite obstacles, students gained competence and confidence.
1. Introduction
Evidence-based medicine underpins safe, effective clinical practice [1]. To contribute meaningfully, future doctors need to engage in research from early stages of their career, acquiring skills in data analysis, literature review, and scientific writing, all of which are critical for clinical reasoning and academic success [2,3,4,5]. Beyond skill acquisition, early research involvement promotes confidence, shapes academic identity, and encourages long-term scholarly engagement [2,3,4,6,7,8].
Yet, traditional research opportunities are often misaligned with student needs, being limited in number, inflexible and with inconsistent mentorship [2,6,8,9,10,11,12]. Students are motivated by aspirations for career progression, academic curiosity, and contribution to evidence-based practice [2,4,5,6,9,10,11,12]. Research experience enhances critical thinking, improves postgraduate competitiveness, and builds publication records [2,4,5,6,9]. However, systemic barriers such as including limited formal training, lack of supervised projects, and rigid curricula impede participation. On a personal level, time constraints, lack of confidence, and limited access to mentorship also hinder early research involvement [2,4,5,6,10,11,12]. Peer-led models in medical education may provide the solution by creating collaborative, low-pressure environments where students can explore research. They offer informal mentorship, demystify academic practices, and support skill-building. These models foster autonomy, belonging, and sustained interest in research [13,14]. Existing initiatives demonstrate this potential; Patel et al. [15] describe the A.S.P.I.R.E. programme, offering peer mentoring, journal clubs, and flexible project dashboards. The National Medical Research Association’s Peer-Led Research Teaching Series combined peer and faculty input to improve research literacy among junior doctors [15]. Academic libraries have also facilitated experiential learning through peer-assisted research services [16]. Similarly, inclusive peer-support structures in higher education broaden student engagement [13,17]. However, these programmes mostly enhance literacy rather than enabling students to lead and publish research. There’s a significant gap in literature on student-led, publication-oriented projects, especially in-depth insights, limiting our understanding of how such experiences contribute to research identity and sustained engagement.
This project aims to address this gap by exploring medical students’ perceptions of a peer-led research initiative, to assess its effectiveness as an accessible and supportive model for developing research skills, confidence, and emerging academic identity.
2. Materials and Methods
Between 2022 and 2024, an annual open call each April invited all University of Malta medical students to participate in peer-led summer research projects, focusing on narrative or systematic reviews. This timing aligned with prior survey findings showing that students preferred to conduct elective research during July–September due to fewer academic demands [18].
Academic collaborators were recruited beforehand to mentor students, ensuring methodological rigour. Participants attended a May orientation session to familiarize themselves with the programme and a peer-led June workshop on research methodology and academic writing. From July to September, students conducted research with flexible, on-demand virtual mentorship via Messenger and WhatsApp.
Students were involved in all review stages, i.e., literature search, screening, data extraction, synthesis, and writing, except topic selection, which was decided with mentors. Manuscripts were drafted collaboratively, reviewed by mentors, then submitted for publication in a peer-reviewed journal or as an abstract as part of conference proceedings. Students participated in journal/conference submissions to gain experience with peer review, journal guidelines, and academic dissemination.
Evaluation of the peer-led initiative followed a qualitative questionnaire (Supplementary Material S1) designed to explore students’ experiences and insights, as it is difficult to capture these aspects quantitatively [19,20,21]. The questionnaire drew on literature in undergraduate research, peer-assisted learning, and prior work on factors shaping research engagement [2,3,6,7,8,18,22,23,24,25,26,27,28]. Open-ended questions encouraged in-depth reflection [29]. To reduce social desirability, recall, and confirmation bias, as well as the Hawthorne effect, a written questionnaire replaced interviews [30]. The questionnaire was distributed in January 2025 through a closed Facebook group, and responses were analysed using grounded theory. Open coding identified concepts, and axial coding formed broader themes. Data collection continued until coding saturation, usually 6–12 participants in homogenous groups [31,32], which ensured sufficient information power [33]. Saturation was defined as the point where no new codes or themes emerged [31,33].
Analysis followed a constructivist lens, examining how students interpreted their experiences, developed research identities, and built confidence guided using grounded theory [34,35]. Thematic interconnections and pattern recognition were explored to obtain deeper insights and develop conceptual logic models on how peer-led research may contribute to the formation of participant’s academic identity [36,37,38,39].
Reflexivity was maintained to ensure transparency and analytic rigour [40]. Ethical approval was obtained by the University of Malta Faculty Research and Ethics Committee (MED-2025-00065).
3. Results
Over three years, 15 students participated in a peer-led research initiative, producing five publications and six conference presentations [41,42,43,44,45,46,47,48,49,50,51]. The participating students were all Maltese, with the majority being clinical medical students. Open coding of nine participant responses yielded 102 codes, grouped into 23 axial codes and eight overarching themes (Table 1). The full list of open codes is provided in Supplementary Material S1. Participants were primarily motivated by intrinsic interest, peer influence, and the opportunity to publish. One student stated, “I was very intrigued to join the programme; I was not very informed, and peer support motivated me to venture into it.” Another shared, “Being student-led made it much less overwhelming to start learning all about research.”

Table 1.
Themes, axials coding, and open codes reflecting medical students’ experiences in peer-led research.
Motivation, support, and identity formation were noted to be interlinked across participant responses (Table 2). Students highlighted the programme’s clear structure and gradual progression. One participant noted, “This opportunity provided a structured approach,” while others identified learning outcomes such as “methodology of research, time management, teamwork” and “the steps and practical skills on how a ‘lit’ review is carried out.” Another described the experience as “more hands-on than I expected, but that was good.” Patterns of learning and development were identified through thematic analysis (Table 3). The programme impacted participants’ confidence and self-perception. One participant stated, “Not as daunting as I thought, now seems more manageable,” while another commented, “It made me more comfortable and competent in taking part in research initiatives.” Mentorship was described as consistently available throughout the programme. One participant noted, “Mentorship was always available at every stage, making me more comfortable at everything I found difficult.” Others mentioned that while faculty involvement varied, peer mentorship was active and supportive: “Lecturers weren’t that involved in my case—but the involvement by students was quite effective.” Participants reported barriers including workload, time constraints, and unclear expectations. Team-related challenges included uneven contribution: “Other members not doing their work on time […] more strict deadlines would help.” Some students described learning experiences even in the absence of clear outcomes: “It was a learning moment […] identifying a pattern even when there was no concrete evidence.”

Table 2.
Interrelationships Between Themes and Their Influence on Medical Students’ Research Engagement and Future Aspirations.

Table 3.
Thematic patterns identified from participant reflections on a peer-led research programme.
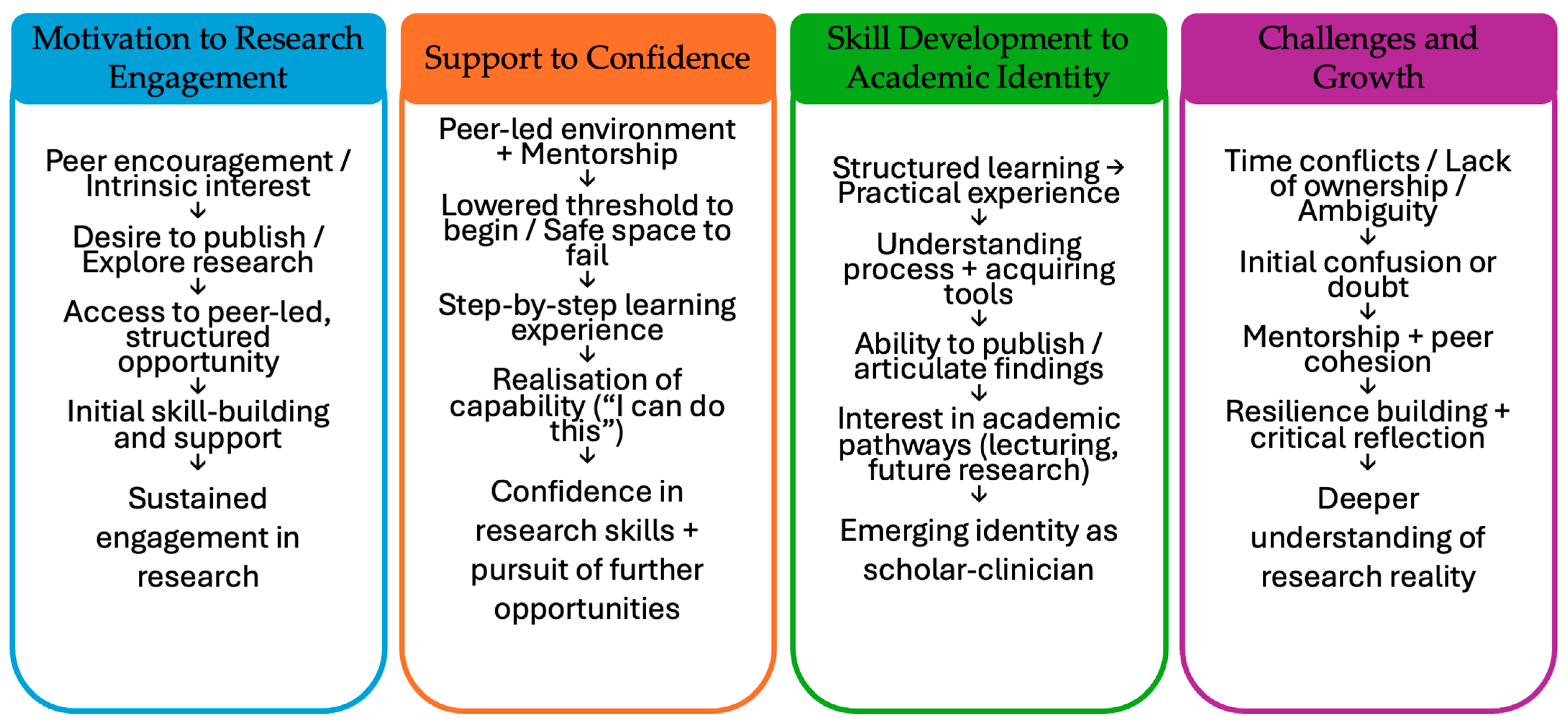
A logic model was developed to visualise proposed pathways between peer-led engagement and academic identity formation (Figure 1). Thematic analysis identified four developmental pathways: (1) Motivation to Research Engagement via peer support; (2) Support to Confidence through guided practice; (3) Skill Development to Academic Identity; and (4) Challenges and Growth.
Figure 1.
Logic model illustrating hypothesising causal pathways through which the peer-led research programme influenced the formation of academic identity.
Thematic and axial coding were conducted through a constructivist lens. Participant responses were analysed iteratively to identify consistent patterns while maintaining analytic rigor.
4. Discussion
This study contributes to a growing body of literature highlighting the potential of peer-led research initiatives to foster early engagement, build academic identity, and scaffold research competencies among undergraduate students, shaping students’ research journeys and identity trajectories.
4.1. Motivation and Peer Influence
Participants were primarily driven by a blend of intrinsic curiosity and peer influence. This supports existing research that emphasises the powerful role of social context in shaping academic engagement [14,15]. The majority of students entered the programme with limited prior exposure to research but were encouraged by peers who had already navigated this unfamiliar terrain. The student-led structure was particularly effective in lowering psychological barriers, as it allowed for a more relatable and less hierarchical introduction to research practices.
This sense of social validation and shared purpose highlights the unique dynamics of horizontal mentorship models, which contrast with more traditional, faculty-driven structures that can feel exclusionary or intimidating [52]. As reflected in international studies [16,17], peer networks not only motivate entry but also provide ongoing reinforcement, creating a sense of mutual accountability and belonging.
4.2. Structured Learning and Skill Development
A clear, scaffolded progression was a defining feature of the programme and a critical enabler of learning. Students described gaining essential research skills through a gradual, experiential process. Rather than relying solely on theoretical instruction, the programme integrated active, hands-on engagement with real research projects, which was both empowering and educational. This approach reflects pedagogical principles of constructive alignment, where learning outcomes, activities, and assessments are coherently integrated [53]. As prior literature suggests, scaffolded opportunities for authentic practice are essential in fostering not only technical competence but also confidence and autonomy [4,5].
4.3. Confidence and Identity Formation
One of the most transformative outcomes was the shift in students’ academic self-concept. Many began the programme with apprehensions about their ability to contribute meaningfully to research. However, through repeated, supported exposure to research tasks, students reported significant increases in confidence and self-efficacy. This evolution reflects a redefinition of self, from passive learner to active contributor, marking a key milestone in academic identity formation. These findings align with conceptual frameworks that link early engagement and success in scholarly tasks to longer-term academic persistence and achievement [14,15]. Confidence, in this context, is not simply a byproduct of skill acquisition but a dynamic and cumulative construct shaped by meaningful participation, feedback, and reflection. As students increasingly saw themselves as capable and legitimate researchers, they also expressed heightened aspirations for future academic and professional development.
4.4. Role of Mentorship
Mentorship emerged as a foundational pillar of the programme. The consistent presence of peer mentors created a supportive environment conducive to risk-taking and growth. Peer mentorship offered not only technical guidance but also emotional reassurance, helping to normalise struggles and demystify academic norms. This model aligns with contemporary understandings of distributed mentorship, where non-hierarchical, reciprocal relationships enhance learning and belonging [16,17]. By offering accessible, culturally proximate role models, peer mentorship bridged gaps in understanding and confidence that traditional structures may overlook. Importantly, the programme’s emphasis on near-peer support illustrates how mentoring relationships themselves can be sites of identity development.
4.5. Navigating Challenges and Building Resilience
Despite overall positive outcomes, students faced a number of challenges, including time constraints, uneven group dynamics, and ambiguous expectations. Notably, these obstacles were not experienced as failures but as opportunities for reflection and adaptive learning. Participants often reframed difficulties as formative moments that built resilience and problem-solving capacity. This aligns with literature emphasising the pedagogical value of struggle, particularly when students are supported in reframing and learning from setbacks [4,5]. The capacity to persist through ambiguity and challenge is increasingly recognised as central to research readiness. Moreover, the students’ reflective stance evidenced in their ability to articulate lessons learned from adversity indicates a mature, metacognitive engagement with the research process.
4.6. Conceptual Contributions
A key contribution of this study is the development of a conceptual model linking four developmental pathways (Figure 1). This model is grounded in constructivist theories of learning and identity, which suggest that individuals become part of academic communities not through transmission of knowledge alone but through meaningful participation in practice [54]. The pathways identified in this study offer a practical and theoretical framework for designing future programmes that seek to democratise access to research and support underrepresented students in navigating the transition from learner to scholar.
These findings suggest several significant long-term outcomes of such peer-led research initiatives. Primarily, by fostering initial engagement and making research more approachable, these programs likely lead to sustained involvement in research beyond the immediate program duration. The observed increase in student confidence and shift in self-perception from apprehension to competence also strongly suggest continued engagement and a greater willingness to pursue further research opportunities. Furthermore, the structured learning and skill development, coupled with publication opportunities, cultivate an interest in academic pathways, contributing to the formation of an emerging scholar-clinician identity. Even when facing challenges, students demonstrated enhanced resilience and critical reflection, essential qualities for navigating the complexities of long-term academic and clinical careers. The immediate academic output (publications and presentations) further underscores the program’s effectiveness in generating tangible contributions, setting a precedent for continued scholarly input and accelerating the development of future clinician-academics.
4.7. Limitations and Future Directions
This study is subject to several limitations. The small sample size and specific target population may limit the generalisability of findings. Participants who opted into the programme and the subsequent evaluation may have had pre-existing interest or motivation towards research, introducing potential selection bias. Additionally, as the initiative was conducted within a single institution and cultural context, the findings may not be directly transferable to other medical education settings. The use of a written qualitative questionnaire, while reducing interviewer bias, may have constrained depth of responses compared to interviews. Finally, self-reported reflections may be influenced by recall and social desirability biases.
Future research could focus on longitudinal studies to track the long-term academic and professional trajectories of students who participate in such programs, providing more robust evidence of their impact on career progression and sustained scholarly engagement. Additionally, exploring the optimal integration of peer-led models within diverse medical curricula and investigating the specific mechanisms through which peer mentorship fosters resilience and mitigates challenges would offer valuable insights for curriculum refinement.
5. Conclusions
The findings of this study point to the potential of peer-led research models to transform how undergraduate medical students access and experience research. By shifting away from traditional, top-down approaches, this model positions students not merely as passive recipients of knowledge but as active participants in scholarly work from the outset of their training. Peer-led research programmes create an environment where students can explore research meaningfully and sustainably, on their own terms. This approach offers a scalable, low-resource strategy to embed research engagement into medical curricula without overburdening faculty or institutional infrastructure. It holds promise for widening participation, especially among students who may not see themselves reflected in conventional academic pathways. Moreover, its emphasis on publication and dissemination introduces students to the full research cycle early in their career, potentially accelerating the development of future clinician-academics. The implications are far-reaching: Institutions that invest in peer-led initiatives stand to cultivate not only research skills, but also a culture of collaboration, curiosity, and academic confidence. As pressures mount for medical education to produce graduates who are research-literate and reflective practitioners, models like this provide a compelling, learner-centered framework that aligns with both educational and professional priorities.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ime4020022/s1, Document S1: Qualitative questionnaire and full list of open codes.
Author Contributions
Conceptualization A.C., methodology A.C. and S.C., data-curation A.C., formal analysis A.C., writing-original draft preparation A.C., writing—review and editing A.C. and S.C., supervision S.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki. Ethical review was obtained by the University of Malta Faculty Research and Ethics Committee (MED-2025-00065).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data cannot be provided to maintain participant’s anonymity.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Connor, L.; Dean, J.; McNett, M.; Tydings, D.M.; Shrout, A.; Gorsuch, P.F.; Hole, A.; Moore, L.; Brown, R.; Melnyk, B.M.; et al. Evidence-based practice improves patient outcomes and healthcare system return on investment: Findings from a scoping review. Worldviews Evid. Based Nurs. 2023, 20, 6–15. [Google Scholar] [CrossRef] [PubMed]
- Naing, C.; Wai, V.N.; Durham, J.; Whittaker, M.A.; Win, N.N.; Aung, K.; Mak, J.W. A systematic review and meta-analysis of medical students’ perspectives on the engagement in research. Medicine 2015, 94, e1089. [Google Scholar] [CrossRef]
- Sobczuk, P.; Dziedziak, J.; Bierezowicz, N.; Kiziak, M.; Znajdek, Z.; Puchalska, L.; Mirowska-Guzel, D.; Cudnoch-Jędrzejewska, A. Are medical students interested in research?–students’ attitudes towards research. Ann. Med. 2022, 54, 1538–1547. [Google Scholar] [CrossRef]
- Mokhtari, B.; Badalzadeh, R.; Ghaffarifar, S. The next generation of physician-researchers: Undergraduate medical students’ and residents’ attitudes, challenges, and approaches towards addressing them. BMC Med. Educ. 2024, 24, 1313. [Google Scholar] [CrossRef] [PubMed]
- Bhuiya, T.; Makaryus, A.N. The Importance of Engaging in Scientific Research during Medical Training. Int. J. Angiol. Off. Publ. Int. Coll. Angiol. 2023, 32, 153–157. [Google Scholar] [CrossRef]
- Mass-Hernández, L.M.; Acevedo-Aguilar, L.M.; Lozada-Martínez, I.D.; Osorio-Agudelo, L.S.; Maya-Betancourth, J.G.E.M.; Paz-Echeverry, O.A.; Paz-Echeverry, M.J.; Castillo-Pastuzan, H.S.; Rojas-Pimentel, J.C.; Rahman, S. Undergraduate research in medicine: A summary of the evidence on problems, solutions and outcomes. Ann. Med. Surg. 2022, 74, 103280. [Google Scholar] [CrossRef] [PubMed]
- Stone, C.; Dogbey, G.Y.; Klenzak, S.; Van Fossen, K.; Tan, B.; Brannan, G.D. Contemporary global perspectives of medical students on research during undergraduate medical education: A systematic literature review. Med. Educ. Online 2018, 23, 15370. [Google Scholar] [CrossRef]
- Burgoyne, L.N.; O’Flynn, S.; Boylan, G.B. Undergraduate medical research: The student perspective. Med. Educ. Online 2010, 15, 5212. [Google Scholar] [CrossRef]
- Cuschieri, A.; Cuschieri, S. Analysing the impact of an elective research experience on medical students’ research perceptions. Med. Sci. Educ. 2023, 33, 157–164. [Google Scholar] [CrossRef]
- Mydin, F.; Rahman, R.S.; Mohammad, W.M. Research collaboration: Enhancing the research skills and self-confidence of early career academics. Asian J. Univ. Educ. 2021, 17, 142–153. [Google Scholar] [CrossRef]
- Kumar, J.; Memon, A.; Kumar, A.; Kumari, R.; Kumar, B.; Fareed, S. Barriers experienced by medical students in conducting research at undergraduate level. Cureus 2019, 11, e4452. [Google Scholar] [CrossRef] [PubMed]
- Alduraibi, K.M.; Aldosari, M.; Alharbi, A.D.; Alkhudairy, A.I.; Almutairi, M.N.; Almosa, M.S.; Alanazi, N.S. Challenges and Barriers to Medical Research Among Medical Students in Saudi Arabia. Cureus 2024, 16, e59505. [Google Scholar] [CrossRef]
- Abusamak, M.; AlQato, S.; Alrfooh, H.H.; Altheeb, R.; Bazbaz, L.; Suleiman, R.; Almansi, A.; Karajeh, A.; Alkhalaileh, A.; Al-Amer, R. Knowledge, attitudes, practices and barriers of medical research among undergraduate medical students in Jordan: A cross-sectional survey. BMC Med. Educ. 2024, 24, 23. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Liao, A.W.; Goh, S.H.; Wu, X.V.; Yoong, S.Q. Effectiveness of peer teaching in health professions education: A systematic review and meta-analysis. Nurse Educ. Today 2022, 118, 105499. [Google Scholar] [CrossRef]
- Mulkalwar, A.; Krishnani, O.; Rao, S.; Tripathi, R. A.S.P.I.R.E: A student led initiative to foster a facilitative environment for undergraduate medical research. Perspect. Clin. Res. 2022, 13, 65–69. [Google Scholar] [CrossRef]
- Bali, P.; Bakshi, S.S.; Haji, S.; Donnelly, L.M.; Rubinger, L. The Research Teaching Series: A peer-led and faculty-supported research skills curriculum for foundation year doctors. J. Adv. Med. Educ. Prof. 2023, 11, 132–140. [Google Scholar]
- Graewingholt, M.; Cornforth, J.; Parramore, S. Better together: Experiential learning in peer-led research services. Ref. Serv. Rev. 2023, 51, 151–170. [Google Scholar] [CrossRef]
- Chilvers, L. The Peer-to-Peer Model: A UK Institution’s Approach to Broadening and Embedding the Provision of Peer Learning and Support. J. Peer Learn. 2025, 16, 1–15. [Google Scholar] [CrossRef]
- Cuschieri, A.; Cuschieri, S. Medical students’ perceptions on research: Results from a small European island state. Med. Sci. Educ. 2021, 31, 1991–1999. [Google Scholar] [CrossRef]
- Cristancho, S.M.; Goldszmidt, M.; Lingard, L.; Watling, C. Qualitative research essentials for medical education. Singapore Med. J. 2018, 59, 622–627. [Google Scholar] [CrossRef]
- Finn, G.M.; Dueñas, A.N.; Kehoe, A.; Brown, M.E. A novice’s guide to qualitative health professions education research. Clin. Exp. Dermatol. 2022, 47, 2090–2095. [Google Scholar] [CrossRef] [PubMed]
- Lim, W.M. What is qualitative research? An overview and guidelines. Australas. Mark J. 2024, 33, 199–229. [Google Scholar] [CrossRef]
- Nakao, H.; Nomura, O.; Nagata, C.; Ishiguro, A. Peer Learning Has Double Effects in Clinical Research Education: A Qualitative Study. Int. J. Pediatr. 2024, 2024, 5513079. [Google Scholar] [CrossRef]
- Avonts, M.; Bombeke, K.; Michels, N.R.; Vanderveken, O.M.; De Winter, B.Y. How can peer teaching influence the development of medical students? A descriptive, longitudinal interview study. BMC Med. Educ. 2023, 23, 861. [Google Scholar] [CrossRef]
- Jawhari, A.A.; Safhi, M.A.; Magadmi, M.M.; Alobaidi, R.H.; Alghamdi, K.M.; Basyouni, R.N. Effect of peer-assisted learning on enhancing clinical research skills among medical students: Students’ and tutors’ perceptions. Adv. Med. Educ. Pract. 2021, 12, 685–696. [Google Scholar] [CrossRef] [PubMed]
- Brierley, C.; Ellis, L.; Reid, E.R. Peer-assisted learning in medical education: A systematic review and meta-analysis. Med. Educ. 2022, 56, 365–373. [Google Scholar] [CrossRef]
- Morris, T.J.; Collins, S.; Hart, J. Informal peer-assisted learning amongst medical students: A qualitative perspective. Clin. Teach. 2024, 21, e13721. [Google Scholar] [CrossRef]
- Cuschieri, A.; Sant, D.; Vella, S.L.; Demanuele, R.; Schembri, R.; Cuschieri, S. Allied health professional students’ perceptions on research: A multi-disciplinary mixed-methods study. Med. Sci. Educ. 2023, 33, 129–138. [Google Scholar] [CrossRef]
- Cuschieri, S.; Cuschieri, A. “An Introduction to Health Research: From Idea to Publication”—Designing and Implementing a Virtual Hands-On Research Course for Healthcare Students. J. Med. Educ. Res. 2024, 4, 19–32. [Google Scholar] [CrossRef]
- Birks, M.; Mills, J. Grounded theory: A practical guide. In The SAGE Encyclopedia of Qualitative Research Methods; Given, L.M., Ed.; SAGE Publications, Inc.: Thousand Oaks, CA, USA, 2008; pp. 375–377. [Google Scholar] [CrossRef]
- Mackieson, P.; Shlonsky, A.; Connolly, M. Increasing rigor and reducing bias in qualitative research: A document analysis of parliamentary debates using applied thematic analysis. Qual. Soc. Work 2019, 18, 965–980. [Google Scholar] [CrossRef]
- Guest, G.; Bunce, A.; Johnson, L. How Many Interviews Are Enough?: An Experiment with Data Saturation and Variability. Field Methods 2006, 18, 59–82. [Google Scholar] [CrossRef]
- Hennink, M.M.; Kaiser, B.N.; Marconi, V.C. Code Saturation Versus Meaning Saturation: How Many Interviews Are Enough? Qual. Health Res. 2017, 27, 591–608. [Google Scholar] [CrossRef] [PubMed]
- Braun, V.; Clarke, V. One size fits all? What counts as quality practice in (reflexive) thematic analysis? Qual. Res. Psychol. 2021, 18, 328–352. [Google Scholar] [CrossRef]
- Mogashoa, T. Applicability of constructivist theory in qualitative educational research. Am. Int. J. Contemp. Res. 2014, 4, 51–59. [Google Scholar]
- Foley, G.; Timonen, V. Using grounded theory method to capture and analyze health care experiences. Health Serv. Res. 2015, 50, 1195–1210. [Google Scholar] [CrossRef] [PubMed]
- Naeem, M.; Ozuem, W.; Howell, K.; Ranfagni, S. A step-by-step process of thematic analysis to develop a conceptual model in qualitative research. Int. J. Qual. Methods 2023, 22, 16094069231205789. [Google Scholar] [CrossRef]
- Attard Cortis, P.; Muir, F. Twelve tips for using Pattern Matching in data analysis for qualitative medical education research. Med. Teach. 2022, 44, 1209–1213. [Google Scholar] [CrossRef]
- Mills, T.; Lawton, R.; Sheard, L. Advancing complexity science in healthcare research: The logic of logic models. BMC Med. Res. Methodol. 2019, 19, 55. [Google Scholar] [CrossRef]
- George, A.Z. Research Frameworks: Critical Components for Reporting Qualitative Health Care Research. J. Patient Cent. Res. Rev. 2024, 11, 4–7. [Google Scholar] [CrossRef]
- Cuschieri, A.; Pisani, R.; Agius, S. CSF shunts as conduits for metastasis: Is there a discrepancy between retrograde and antegrade spread? Egypt. J. Neurosurg. 2025, 40, 37. [Google Scholar] [CrossRef]
- Zerafa, J.; Shaw, C.; Cushieri, A. Neurobiology of handedness. Impulse Prem. Undergrad. Neurosci. J. 2024, 21, 1–15. [Google Scholar]
- Cuschieri, A.; Pisani, R.; Agius, S. From Trauma to Tumor: Exploring Post-Traumatic Brain Injury Glioblastoma Patient Characteristics. World Neurosurg. 2024, 184, 175–181. [Google Scholar] [CrossRef]
- Cuschieri, A.; Borg, M.; Levinskaia, E.; Zammit, C. LITT for biopsy-proven radiation necrosis: A qualitative systematic review. J. Clin. Neurosci. 2023, 116, 69–78. [Google Scholar] [CrossRef]
- Cuschieri, A.; Zammit, C. Closed loop deep brain stimulation: A systematic scoping review. Clin. Neurol. Neurosurg. 2022, 223, 107516. [Google Scholar] [CrossRef] [PubMed]
- Cuschieri, A.; Pace, G.; Darzaweh, R. Primary isolated third ventricle glioblastoma multiforme: Systematic review. Brain Spine. 2024, 4 (Suppl. 3), 103724. [Google Scholar] [CrossRef]
- Cuschieri, A.; Agius, D. Deep Brain Stimulation of the Nucleus Basalis of Meynert for Lewy-Body Dementias: A systematic review of randomised control trials. In Proceedings of the Poster Presentation, National Dementia Conference 2024, Melbourne, Australia, 12–13 June 2024. [Google Scholar]
- Pisani, R.; Cuschieri, A.; Agius, S. Antegrade and retrograde metastasis along CSF shunts: A dual systematic review. In Proceedings of the ePoster Presentation, Evolution of Surgery, Scalpel Undergraduate Surgical Conference 2023, Manchester, UK, 4 November 2023. [Google Scholar]
- Cuschieri, A.; Caruana, A.; Shaw, C.; German, E.; Pace, G.; Attard-Montalto, G.; Zerafa, J.; Farrugia, M.; Pisani, R.; Agius, S. CSF ascites: A comprehensive systematic review. In Proceedings of the Evolution of Surgery, Scalpel Undergraduate Surgical Conference 2023, Manchester, UK, 4 November 2023. [Google Scholar]
- Borg, N.; Cuschieri, A.; Zammit, C. Current paradigms and uses of adaptive neuromodulation. In Proceedings of the 9th Lublin International Medical Congress, Neurology and Neurosurgery Section, LIMC2022, Lublin, Poland, 17–19 November 2022; Student’s Scientific Society of the Medical University of Lublin: Lublin, Poland, 2022. Available online: https://ppm.umlub.pl/info/book/UML39b4ba643ef340ba988200a73f851b55/ (accessed on 18 May 2025).
- Cuschieri, A.; Borg, M.; Levinskaia, E. 10 years of Laser Interstitial Thermal Therapy for biopsy proven Radiation Necrosis: Where do we stand? The future of our scalpel. In Proceedings of the ePoster Presentation, Evolution of Surgery, Scalpel Undergraduate Surgical Conference 2022, Manchester, UK, 12 November 2022. [Google Scholar]
- Olmos-Vega, F.M.; Stalmeijer, R.E.; Varpio, L.; Kahlke, R. A practical guide to reflexivity in qualitative research: AMEE Guide No. 149. Med. Teach. 2023, 45, 241–251. [Google Scholar] [CrossRef]
- Zheng, D.X. The need for horizontal mentorship networks to facilitate medical students’ engagement in research. Acad. Med. 2022, 97, 167–169. [Google Scholar] [CrossRef]
- Jervis, L.M.; Jervis, L. What is the constructivism in constructive alignment? Biosci. Educ. 2005, 6, 1–4. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Academic Society for International Medical Education. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).