Abstract
Early involvement and exposure to evidence-based research during medical school have been shown to play a formative role in students’ holistic development as future physicians. While there are medical schools encouraging research initiatives, few programs implement 4-year longitudinal research in the curriculum. Here, the authors categorized graduates as pre-LRP or post-LRP and utilized PubMed’s Advanced Search Builder to identify each graduate’s publications with a time frame that began from 1 year to 7 years post-graduation. The data were then analyzed to identify any significant changes between these two cohorts. A total of 1022 medical school graduates from an ACGME-accredited U.S. medical school were included in this study. The average rate of publications annually was 0.47 + 1.43 (pre-LRP) and 0.57 + 1.40 (post-LRP). Additionally, the average probability of at least one publication in a given year was 22% (95% CI: 0.21–0.23) pre-LRP and 27% (95% CI: 0.25–0.28) post-LRP. Lastly, the average probability of at least one first-author publication in a given year was 12.2% (95% CI: 0.12–0.13) pre-LRP and 15% (95% CI: 0.14–0.16) post-LRP. Overall, participation in a mentored longitudinal research program during medical school demonstrated a positive trend in the number and rate of publications. The implementation of a mentored longitudinal research program can contribute to increased research productivity in physicians’ early careers, leading to the development of important research skills, the fostering of commitment in scholarly work, and a deeper understanding of evidence-based medicine.
1. Introduction
In 2004, the University of Pittsburgh School of Medicine (UPSOM) implemented a novel, mandatory research curriculum for medical students titled the longitudinal research project (LRP). Under faculty mentorship, first-year medical students construct an individualized scholarly research project that must be completed prior to graduation. Students in the program engage in first- and second-year coursework focused on formulating research questions, participate in weekly journal clubs and discussions, collaborate on scholarly projects under mentorship, have the chance to participate in funded summer research opportunities, and conclude with presentations of written scholarly products [1]. Institutional support, faculty engagement, and mentorship are highlighted as critical pillars contributing to the program’s success [2]. Several medical schools in the United States have implemented similar types of longitudinal programs that facilitate continuous research training for their medical students [3,4,5,6,7,8,9]. Stanford University School of Medicine and Duke University School of Medicine have incorporated scholarly concentration (SC) programs and Longitudinal Integrated Clerkship Programs (LICPs) into their medical curriculum, respectively [10]. Many of these programs emphasize different areas of focus which require medical students to be involved in experiences and activities throughout the entirety of their medical education. There has been an observed increase in the spectrum of research components within medical school curricula, encompassing both mandatory and non-mandatory elements, across international programs [11,12]. The identified literature primarily aimed to describe these initiatives, evaluate their impact on students, and assess research outputs, yet it highlighted limited information on longitudinal research outcomes. Furthermore, a retrospective, self-reported survey administered to recent University of Alabama at Birmingham School of Medicine (UAB SOM) graduates delved into the impact of elective versus mandatory research experiences, identifying a positive association between medical school research activities and subsequent engagement in research [13]. Collectively, these studies underscore the multifaceted nature of research training initiatives during medical school, emphasizing the need for comprehensive assessments of their longitudinal impacts on research outcomes. Previous observations and studies have indicated that universities that implement these programs within their curriculum often see an enhancement in the medical student’s educational experience. These findings have been supported by the literature that has not only observed an increase in academic outcomes but clinical readiness as well [14,15,16,17,18,19,20].
However, very few MD programs specifically require longitudinal research for all 4 years of medical education. We focused on UPSOM’s curriculum because of its distinctiveness in several key areas. Firstly, the Scientific Reasoning and Medicine curriculum guides students systematically from theoretical knowledge to practical application, specifically preparing them for scholarly projects, which sets it apart from other medical education models. Secondly, UPSOM integrates mandatory didactic sessions and practical training in scientific writing, emphasizing effective communication skills crucial in the medical field. Lastly, UPSOM’s formal mentoring and team-building programs for faculty mentors foster a supportive environment, enhancing student–mentor relationships and promoting collaborative research. The goal of this formative research experience was to equip medical students with the skills necessary to conduct and evaluate research methodology while promoting the practice of evidence-based medicine. This study evaluated the long-term implications of the LRP by analyzing postgraduate research productivity following the implementation of this unique research curriculum.
2. Materials and Methods
This retrospective study analyzed publicly available publication data from 2007 to 2020 on UPSOM graduates before and after LRP implementation in 2004. Data collection included graduation year, residency program, medical specialty, MD or MD/PhD status, and postgraduate publication data for UPSOM classes of 2006–2012. Graduation cohorts were categorized relative to LRP status. Pre-LRP classes included the class of 2006 and 2007, and post-LRP graduates included 2008–2012. Each graduate’s respective publicly available publication(s) were identified via PubMed’s Advanced Search Builder with a publication time frame that began at least one year post-graduation to seven years post-graduation to exclude publications initiated while in medical school.
The results were set to be sorted by Publication Date, and All Results were saved as a PubMed Excel export, listing each publication’s PubMed Identifier (PMID), Title, Authors, Citations, First Author, Journal/Books, Publication Year, Create Date, and DOI. The UPSOM match list was used to confirm graduate residency affiliation and specialty for each publication extracted from PubMed. If further specification was needed, “Dr. First name Last name University of Pittsburgh School of Medicine” was inputted into Google’s search engine. Any additional information used to identify the graduates’ publications was limited to the publicly available information provided by the graduate’s current institution’s site, LinkedIn, and Doximity. The Science/SCI Journal Impact Factor database was utilized to identify journal impact factors corresponding to the publication year. We analyzed the cross-sectional time series cohort using t-tests with unequal variance, multivariate logistic regression, and multivariate Poisson models using STATA 16 statistical software with significance set to 0.05.
3. Results
A total of 1022 medical school graduates met the inclusion criteria. Of these, 278 graduated prior to 2008 (pre-LRP), while 744 graduated in 2008 or later (post-LRP). The average rate of publications annually was 0.54 + 1.41 for the overall cohort, 0.47 + 1.43 for pre-LRP, and 0.57 + 1.40 for post-LRP (publications per year averaged across the 8-year study period for each medical school graduate). Figure 1 details the average number of publications over postgraduate status for the pre-LRP and post-LRP groups. According to the multivariate linear mixed-effects results, the post-LRP medical school graduates exhibited a greater average annual publication rate than the pre-LRP medical student graduates (β = 0.10, 95% CI: 0.03–0.17, p = 0.008) (Table 1).
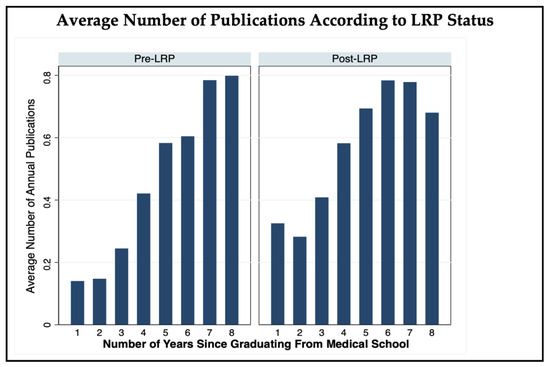
Figure 1.
The average number of publications in a given year across experience (number of years since graduating from medical school) and LRP status (pre-LRP versus post-LRP). Pre-LRP was defined as 2006 and 2007 medical school graduates, while post-LRP consisted of 2008–2012 graduates. Results were derived based on multivariate Poisson regression models.

Table 1.
Multivariate predictors of postgraduate publication rates for overall, first author, and odds of publishing at least one overall or first-author manuscript per year among medical school graduates’ manuscripts.
When considering the proportion of graduates who published at least one manuscript, the overall probability of having at least one publication in a given year was 25% for the overall cohort across the 8-year period. According to mixed-effects multinomial logistic regression results, the probability of having at least one publication was 2.9 times greater for the post-LRP graduates than the pre-LRP graduates (OR: 2.88, 95% CI: 2.15–3.86, p < 0.001) (Table 1). However, compared to the pre-LRP graduates, the post-LRP graduates revealed a slower increase in the probability of publishing at least one manuscript each year as postgraduate experience increased (Figure 2, Table 1). After adjusting for these predictors, we estimate an average pre-LRP probability of 22% (95% CI: 0.21–0.23) and post-LRP probability of 27% (95% CI: 0.25–0.28) of having at least one publication across a given year.
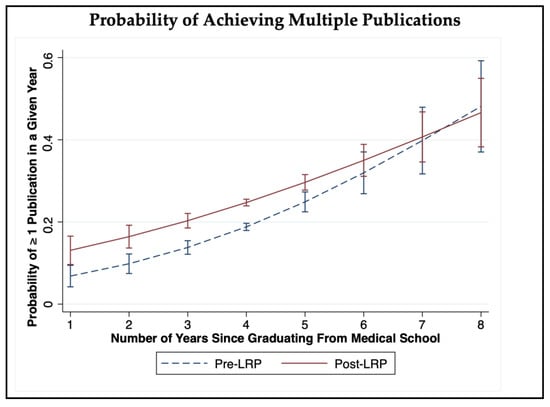
Figure 2.
The probability of authorship per year based on experience (number of years since graduating from medical school) and LRP status (pre-LRP versus post-LRP). Medical school graduates from 2006 and 2007 were classified as pre-LRP, while those from 2008 to 2012 were considered post-LRP. Results were obtained through multivariate Poisson regression models.
The average rate of first-author publications was 0.23 + 0.48 for the overall cohort, 0.22 + 0.54 for pre-LRP, and 0.24 + 0.45 for post-LRP (first-author publications per year averaged across the 8 years of postgraduate experience). Figure 3 illustrates the average number of first-author publications over postgraduate status for the pre-LRP and post-LRP groups. According to the multivariate linear mixed-effects results, the post-LRP medical school graduates exhibited a greater average first-author publication rate than the pre-LRP medical student graduates (β = 0.13, 95% CI: 0.05–0.22, p = 0.001). However, compared to the pre-LRP graduates, the post-LRP graduates revealed a slower increase in first-author publications as postgraduate experience increased (Table 1). After adjusting for these predictors, we estimate an average of 23% (95% CI: 0.19–0.27) for pre-LRP graduates and 23% (95%CI: 0.21–0.26) for post-LRP graduates when considering first-author publication rates across all 8 years of postgraduate experience.
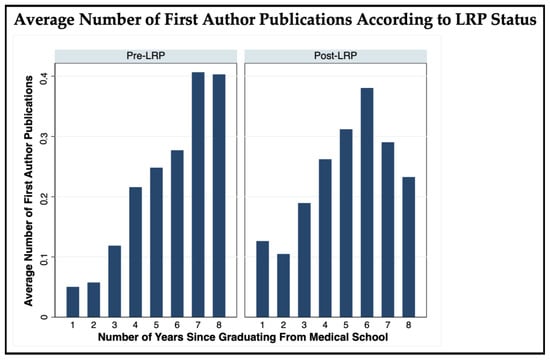
Figure 3.
The average number of first-author publications per year based on experience (number of years since graduating from medical school) and LRP status (pre-LRP versus post-LRP). Medical school graduates from 2006 and 2007 were considered pre-LRP, while those from 2008 to 2012 were classified as post-LRP.
Lastly, the overall probability of having at least one first-author publication each year was 14.2% for the overall cohort across all 8 years of postgraduate experience. According to the mixed-effects multinomial logistic regression results, the probability of having at least one first-author publication was roughly three times greater for the post-LRP graduates than the pre-LRP graduates (OR: 3.08, 95% CI: 2.38–4.00, p < 0.001) (Table 1). Compared to the pre-LRP graduates, the post-LRP graduates revealed a slower increase in the probability of publishing at least one first-author manuscript in a given year as postgraduate experience increased (Figure 4, Table 1). After adjusting for these predictors, we estimate an average pre-LRP probability of 12.2% (95% CI: 0.12–0.13) and post-LRP probability of 15% (95% CI: 0.14–0.16) of having at least one first-author publication in a given year.
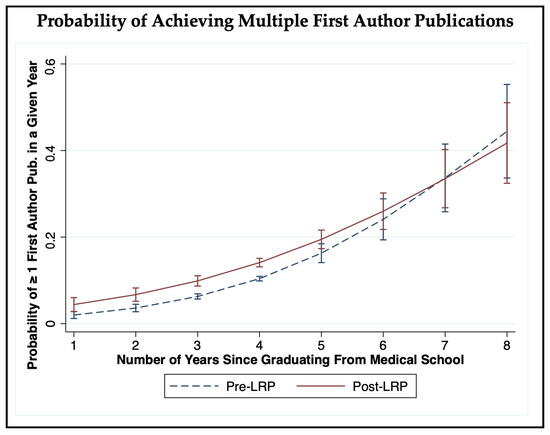
Figure 4.
The probability of first-author publications per year based on experience (number of years since graduating from medical school) and LRP status (pre-LRP versus post-LRP). Medical school graduates from 2006 and 2007 were classified as pre-LRP, while those from 2008 to 2012 were considered post-LRP. Results were obtained through multivariate Poisson regression models.
4. Discussion
Following graduation, physicians who took part in the LRP were more likely to publish and publish more frequently. To our knowledge, there is currently no research in the literature that reports long-term postgraduate productivity following a mandatory research program in the medical school curriculum. As discussed in the results, there are various interesting trends, such as the slower rise in first-author publications post-LRP while there being a greater probability of publishing as the first author over the longitudinal analysis. While the primary focus of this study was to quantify the impact on academic productivity, it is important to recognize that it is only one aspect of the overall impact research can have on the development of physicians. The data suggest that physicians that underwent the LRP remained involved in research beyond their time in medical school, which can be directly translated to an improvement in the quality of the physician’s healthcare performance [21]. The published literature has reported medical student perspectives of this required program, which was found to be meaningful and valuable in gaining skills related to critical thinking, leadership, and scientific communication [22].
A point of consideration is the level of quality that comes with the increased quantity of publications. While the likelihood of publishing and number of publications increased, the aggregate impact factor value did not change. This suggests that the increase in publications did not diminish the level of impact of these manuscripts after the implementation of this program.
The medical school curriculum often revolves around the pathophysiology and clinical skills required to meet the needs of future patients. While these are fundamental aspects of medical education, there is a lesser nationwide emphasis on providing a longitudinal curriculum that fosters research skills that may ultimately impact the career of a physician and their respective field [23]. This study suggests that implementing a mandatory LRP within a medical school’s curriculum may increase meaningful research productivity and the progression of clinical science for young physicians beyond the curriculum.
While our study primarily focused on the impact of the LRP, we recognize that various other factors were not considered, which serves as a limitation of this study. Our analysis relied on publicly available datasets, which limited variables that may influence productivity such as marital status, extracurricular activities, or family responsibilities, which can play a dynamic role in a medical graduate’s scholarly involvement. Future research regarding this unique program may provide additional insights by identifying and controlling for these variables to gain further insights into the impact of the LRP. Additionally, the graduate cohorts between pre-LRP and post-LRP were not equal as there were limitations in obtaining earlier classes’ data. This inequality of data also serves as a limitation.
5. Conclusions
Medical school graduates who partook in a mandatory, longitudinal research program in a medical school curriculum published more and more frequently in their early careers compared to earlier graduates prior to this program. The results from this study encourage the implementation of such a research program for medical schools looking to support and increase early-career research productivity for their graduates.
Author Contributions
Conceptualization, H.O., S.C., J.O., B.N., S.T. and J.R.F.; methodology, H.O., S.C., J.O., B.N., S.T. and J.R.F.; software, S.C.; validation, H.O., S.C., J.O., B.N., S.T. and J.R.F.; writing—original draft preparation, H.O., S.C., J.O., B.N., S.T. and J.R.F.; writing—review and editing, H.O., S.C., J.O., B.N., S.T. and J.R.F. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable as this study analyzed only publicly available data.
Informed Consent Statement
Not applicable as this study analyzed only publicly available data.
Data Availability Statement
Data available upon reasonable request.
Acknowledgments
This research was presented at the 2022 American Medical Association (AMA) Research Challenge conference.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Boninger, M.; Troen, P.; Green, E.; Borkan, J.; Lance-Jones, C.; Humphrey, A.; Gruppuso, P.; Kant, P.; McGee, J.; Willochell, M.; et al. Implementation of a Longitudinal Mentored Scholarly Project: An Approach at Two Medical Schools. Acad. Med. 2010, 85, 429–437. [Google Scholar] [CrossRef]
- Schor, N.F.; Troen, P.; Kanter, S.L.; Levine, A.S. The Scholarly Project Initiative: Introducing Scholarship in Medicine through a Longitudinal, Mentored Curricular Program. Acad. Med. 2005, 80, 824–831. [Google Scholar] [CrossRef] [PubMed]
- Holloway, R.; Nesbit, K.; Bordley, D.; Noyes, K. Teaching and evaluating first and second year medical students’ practice of evidence-based medicine. Med. Educ. 2004, 38, 868–878. [Google Scholar] [CrossRef] [PubMed]
- Silverman, H.; Cohen, T.M.; Fridsma, D. The evolution of a novel biomedical informatics curriculum for medical students. Acad. Med. 2012, 87, 84–90. [Google Scholar] [CrossRef] [PubMed]
- van Alfen-van der Velden, J.A.E.M.; Verbeek, A.L.M.; Morava, E.; Ruijs, A.J.E.M.; Draaisma, J.M.T. Integration of three different medical research projects for medical students in a Department of Pediatrics. Med. Sci. Educ. 2013, 23, 648–655. [Google Scholar] [CrossRef]
- Mitchell, K.D.; Krane, N.K. Training medical students in research: The DeBakey scholars program at Tulane University School of Medicine. Med. Sci. Educ. 2013, 23, 385–390. [Google Scholar] [CrossRef]
- LaConte, L.; Johnson, T.A.; Vari, R.C.; Friedlander, M.J. Research immersion at the virginia tech carilion school of medicine—An integrated curriculum producing scientist physicians for the future of healthcare. Med. Sci. Educ. 2013, 23, 122–134. [Google Scholar] [CrossRef]
- Brousseau, D.C.; Harder, D.R. Integration of the medical college of wisconsin physician scientist pathway and summer research programs to increase medical student research skills. Med. Sci. Educ. 2013, 23, 84–87. [Google Scholar] [CrossRef]
- Green, E.P.M.; Borkan, J.M.; Pross, S.H.; Adler, S.R.; Nothnagle, M.; Parsonnet, J.; Gruppuso, P.A. Encouraging Scholarship: Medical School Programs to Promote Student Inquiry Beyond the Traditional Medical Curriculum. Acad. Med. 2010, 85, 409–418. [Google Scholar] [CrossRef]
- Latessa, R.A.; Swendiman, R.A.; Parlier, A.B.; Galvin, S.L.; Hirsh, D.A. Perceptions of Learning Affordances in Longitudinal Integrated Clerkships: A Dual-Institution, Mixed-Methods Study. Acad. Med. 2017, 92, 1313–1319. [Google Scholar] [CrossRef]
- Murray, H.; Payandeh, J.; Walker, M. Scoping Review: Research Training during Medical School. Med. Sci. Educ. 2022, 32, 1553–1561. [Google Scholar] [CrossRef] [PubMed]
- Radville, L.; Aldous, A.; Arnold, J.; Hall, A.K. Outcomes from an elective medical student Research Scholarly Concentration program. J. Investig. Med. 2019, 67, 1018–1023. [Google Scholar] [CrossRef] [PubMed]
- Weaver, A.N.; McCaw, T.R.; Fifolt, M.; Hites, L.; Lorenz, R.G. Impact of elective versus required medical school research experiences on career outcomes. J. Investig. Med. 2017, 65, 942–948. [Google Scholar] [CrossRef] [PubMed]
- Hallan, D.R.; Mikhail, D.; Lu, K.; Henry, A.; Chiang, K.; Patterson, M.; Sakya, S.M. Residency Specialty and National Resident Matching Program Outcomes as Predictors of Academic vs Non-Academic Position as an Attending Physician. Cureus 2020, 12, e9548. [Google Scholar] [CrossRef] [PubMed]
- National Resident Matching Program. Charting Outcomes in the Match: Senior Students of U.S. MD Medical Schools. July 2020. Available online: https://www.nrmp.org/wp-content/uploads/2021/08/Charting-Outcomes-in-the-Match-2020_MD-Senior_final.pdf (accessed on 23 January 2024).
- Glinton, K.E.; Potocki, L.; Dhar, S.U. An innovative medical school curriculum to enhance exposure to genetics and genomics: Updates and outcomes. Genet. Med. 2022, 24, 722–728. [Google Scholar] [CrossRef]
- Bajaj, S.S.; Wang, H.; Williams, K.M.; Pickering, J.M.; Heiler, J.C.; Manjunatha, K.; Sanchez, M.; O’Donnell, C.T.; Boyd, J.H. Career Research Productivity Correlates with Medical School Ranking among Cardiothoracic Surgeons. J. Surg. Res. 2021, 264, 99–106. [Google Scholar] [CrossRef]
- Zhu, H.; Huang, A.; Zhou, K.; Bhatnagar, A.; Sorensen, R.; Cordova, K.; Calderara, G.A.; Dasari, N.; Kirby, R.P.; Kim, S.J. Demographic and applicant-specific predictors of medical school research productivity in a national cohort of dermatology residents. Clin. Dermatol. 2023, 41, 291–295. [Google Scholar] [CrossRef]
- Bard, J.T.; Yeluru, H.; Karpov, M.V.; Mu, D. Evaluating the Impact of a Medical School Student-Run Research Organization on Scholarly Activity. Cureus 2023, 15, e43067. [Google Scholar] [CrossRef] [PubMed]
- Cain, L.; Kramer, G.; Ferguson, M. The Medical Student Summer Research Program at the University of Texas Medical Branch at Galveston: Building research foundations. Med. Educ. Online 2019, 24, 1581523. [Google Scholar] [CrossRef]
- Carberry, C.; McCombe, G.; Tobin, H.; Stokes, D.; Last, J.; Bury, G.; Cullen, W. Curriculum initiatives to enhance research skills acquisition by medical students: A scoping review. BMC Med. Educ. 2021, 21, 312. [Google Scholar] [CrossRef]
- Boaz, A.; Hanney, S.; Jones, T.; Soper, B. Does the engagement of clinicians and organisations in research improve healthcare performance: A three-stage review. BMJ Open 2015, 5, e009415. [Google Scholar] [CrossRef] [PubMed]
- Nikiforova, T.; Carter, A.; Chang, J.C.; DeFranco, D.B.; Veldkamp, P.J.; Levine, A.S. Impact of A Required, Longitudinal Scholarly Project in Medical School: A Content Analysis of Medical Students’ Reflections. Med. Sci. Educ. 2021, 31, 1385–1392. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).