Abstract
This study aims to investigate nursing interns’ training experiences in emergency departments (EDs) in Saudi Arabia and explore the factors influencing their experiences. A descriptive research design was employed utilizing a survey distributed to nursing interns who completed their ED rotation within the last three months. The data were analyzed using SPSS version 27, and principal component analysis (PCA) was conducted to identify the challenges encountered by the interns. This study analyzed the responses of 126 nursing internship students in various regions of Saudi Arabia to assess their training experiences in emergency departments. The principal component analysis revealed two significant factors: (1) “Emergency Department Training and Skill Development”, which focused on challenges faced during training, and (2) “Integrated Emergency Department Training and Competence Development”, which provided a holistic view of nursing internship students’ experiences and preparedness for their careers. The results indicated moderately below-average challenges and a moderately positive overall training experience. The findings suggest a need to address these challenges to improve the training experience and better prepare nursing internship students for careers in emergency departments. This study recommends enhancing the nursing curricula alignment with practical training objectives, focusing on technical and interpersonal skills development. A supportive learning environment in emergency departments is crucial, including effective communication and collaboration. Diverse clinical experiences and reflection on training can guide students in exploring potential career paths in emergency departments or other specialized nursing areas.
1. Introduction
Nursing education plays a pivotal role in equipping healthcare professionals with the necessary skills and knowledge to provide high-quality care and address the multifaceted needs of patients [1]. Nursing internships, in particular, serve as an indispensable component of nursing education, offering students invaluable opportunities to gain hands-on experience in real-world clinical environments [2,3]. The practical exposure during internships enables nursing students to apply theoretical knowledge acquired in the classroom, develop clinical competencies, and enhance critical thinking and decision-making skills [1]. The internship period is essential for nursing students as it bridges the gap between theoretical knowledge and clinical practice, enabling them to become well-rounded professionals [4].
Internships provide a supportive learning environment where students can gain experience in various aspects of patient care, including assessment, intervention planning, and evaluation, under the supervision of experienced healthcare professionals [5,6]. Additionally, internships foster the development of essential soft skills such as communication, teamwork, and time management, which are crucial for successful nursing practice [7].
Nursing interns frequently face numerous challenges during their internships, which can adversely affect their learning experiences and professional growth [1,8]. These challenges may include adapting to the fast-paced and demanding clinical environment, managing emotional stress, navigating complex interpersonal relationships with patients and colleagues, and overcoming knowledge gaps or skill deficiencies [9]. Understanding and addressing these challenges is of utmost importance to ensure successful nursing internship programs and ultimately enhance the overall quality of healthcare delivery [10]. Strategies to support nursing interns during their clinical placements may include providing targeted training and orientation programs, assigning dedicated mentors or preceptors, integrating stress management and resilience-building techniques into the curriculum, and encouraging reflection and feedback to promote continuous learning and improvement [11].
In Saudi Arabia, the healthcare system has been experiencing rapid expansion, driven by factors such as a growing population and increased demand for healthcare services [12]. As a result, there is an escalating need for well-prepared and competent nursing professionals, particularly in emergency departments (EDs), which often serve as the initial point of contact for patients requiring urgent care [13]. Nursing interns in EDs are expected to function in a highly dynamic and unpredictable environment, catering to diverse patient populations and managing a broad spectrum of medical conditions [14].
However, research on the challenges encountered by nursing interns in Saudi Arabia, especially in EDs, remains limited. A few studies have sought to understand the experiences of nursing interns in general [15,16], yet there is no consensus on the identification and quantification of factors influencing their internship experiences. This knowledge gap is even more pronounced when examining the difficulties faced by student interns in EDs, where the intricacies of a multicultural workforce and the unique demands of the emergency setting have not been extensively investigated [14].
In light of these research gaps, this study aims to investigate the nursing intern’ training experiences in emergency departments (EDs) in Saudi Arabia and explore the factors influencing their experiences. By examining the experiences of nursing interns in this context, the study seeks to contribute to a better understanding of the issues they encounter and provide insights that can inform the development of strategies to support their learning and professional growth.
2. Materials and Methods
A descriptive study was carried out using a survey distributed to nursing interns in 19 Saudi Arabian cities. The study’s sample was purposive, with inclusion criteria requiring that student interns had completed their emergency department rotation within the last three months. The survey was developed by the researchers through a systematic approach, which included a literature review, translation, and validation. Relevant studies on the challenges faced by nursing internship students were identified, revealing existing knowledge on this subject. Specific keywords such as “challenges”, “nursing intern”, “clinical education”, “internship program”, “emergency”, “experience”, and “Saudi Arabia” helped locate relevant studies from the Saudi Digital Library. The search involved the following databases: CINAHL, PubMed, ScienceDirect, and Wiley. Initially, 615 studies were identified; however, after reviewing the abstracts, 587 studies were excluded because their purposes did not focus on the challenges faced by interns in emergency departments (EDs). Among the remaining 28 studies, 13 conducted in Middle Eastern countries, specifically Saudi Arabia, were included in the review to extract items for developing a new scale [1,17,18,19,20,21,22,23,24,25,26,27,28]. A total of 70 items indicating challenges faced by student interns were identified from these relevant studies.
The identified items were subsequently translated into Arabic, as no existing related questionnaires were available in Arabic. Seven experts from academia and the emergency department staff reviewed the items by rating each one on a scale of 1 to 10 in terms of relevance (1 = not relevant at all and 10 = very relevant) and clarity (1 = not clear at all and 10 = very clear). The data were analyzed using SPSS to calculate the mean for each item in terms of both clarity and relevance. Consequently, the means for clarity ranged between 4.28 and 9.56, while for relevance, the means ranged from 2.7 to 9.4. Based on these results, all items with a relevance score below 7 were removed, and all items with a clarity score below 7 were modified for improved readability. This process led to the elimination of unrelated and similar items, ultimately reducing the total number of items to 43. A 5-level Likert scale was employed, with 1 denoting strong disagreement and 5 indicating strong agreement.
The survey was distributed to nursing interns across various regions in Saudi Arabia after obtaining ethical approval from IRB-HAP-02T-067, number 767, dated 23 December 2022. The survey was distributed to participants by sending invitations to the nurse managers at the identified hospitals. These nurse managers facilitated the delivery of the survey link to the participants via email.
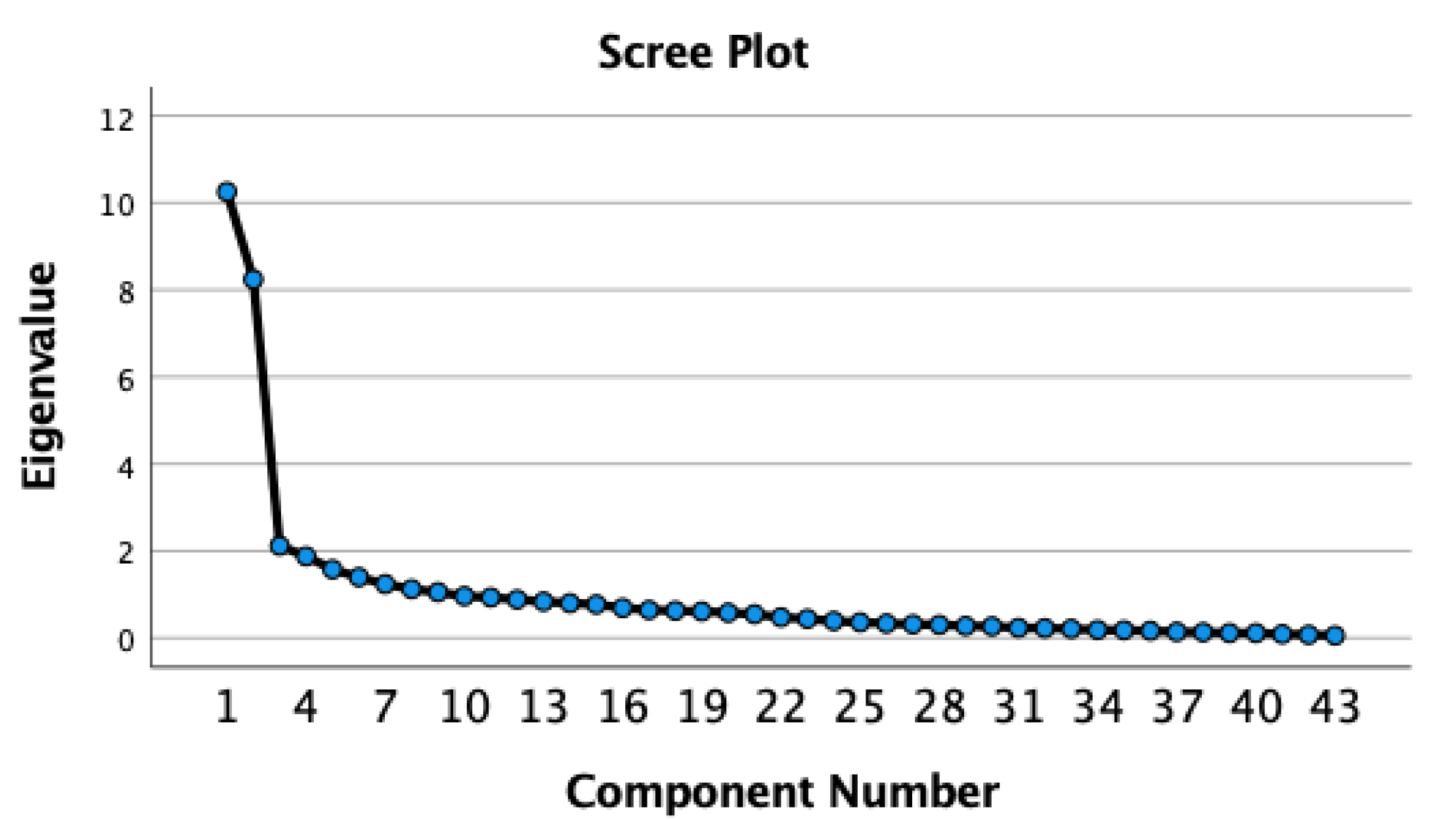
The data were entered into an online survey and analyzed using SPSS version 27. Missing values, outliers, and normality were examined by checking the skewness and kurtosis of each item, which is essential for the PCA to extract the factor and remove the redundant items. To guarantee an adequate sample size for conducting the PCA, KMO and Bartlett’s tests were employed, in addition to requiring a participant count of over 100 [29]. The method for determining the number of factors involved three criteria: (1) eigenvalues, (2) a scree plot, and (3) Horn’s parallel analysis. Orthogonal varimax rotation was then applied for easy interpretation of the newly generated items [29,30,31]. Redundant items were removed based on cross-loading differences exceeding 0.30 between the primary and secondary loadings. The final step in the PCA was the interpretation [29].
3. Results
Among the 126 responses from internship students in some regions of the Kingdom of Saudi Arabia, most of the responses were from females, with (60.3%). The responses were taken from 16 regions of the Kingdom of Saudi Arabia, and the majority was from the Riyadh region, with (18.3%). Participants reported their understanding of the hospital’s policies during the internship, with (80.2%). Most of the participants trained for one month in the emergency department during the internship (48.4%).
The KMO value of 0.812 indicated sufficient information for factor analysis, and Bartlett’s test of sphericity result, p < 0.001, suggested that the data were suitable for PCA. The participant count in this study was 126, which, while falling short of the recommended 300 cases suggested by Tabachnick’s rule of thumb, met the threshold of 100 or greater, as suggested by Hair et al. It is important to note that there is a lack of agreement in the literature regarding sample size requirements for factor analysis, with recommendations ranging from 100 to 1000 or more cases [30]. In this context, our sample size can be considered within the acceptable range, although larger sample sizes could provide more robust results. The PCA was sufficient for this sample, and three factors were identified based on eigenvalues greater than 1, explaining 56.63% of the total variance: the scree plot (Figure 1), which displayed three factors above the elbow, and Horn’s parallel analysis (Table 1), which indicated that three significant factors were identified (Factors 1–3), as their initial eigenvalues were greater than their corresponding parallel analysis values. Factors 4–9 were rejected due to lower initial eigenvalues than their respective parallel analysis values. Consequently, three factors were extracted from the data. Out of 43 items, 15 were deleted due to no loading or cross-loading on multiple factors. After four iterations, 28 items remained without cross-loading, as shown in Table 2.
Figure 1.
Scree plot.

Table 1.
Horn’s parallel analysis.

Table 2.
Nursing interns’ perceptions of emergency department training: principal component analysis of survey items.
Factor 1, titled “Emergency Department Training and Skill Development”, focuses on challenges facing nursing internship students during emergency department training. This training enables individuals to handle various cases, manage fatalities, attend to car accident victims, understand safety measures, acquire new abilities, provide emergency care, and operate medical equipment. This factor consists of 15 items with loadings ranging from 0.76 to 0.57, explaining 27.84% of the variance. The major challenges include technical and procedural challenges, communication and decision-making challenges, and personal well-being and safety challenges. A total mean score of 2.86 out of 5 indicates that nursing students face moderately below-average challenges during their emergency department training, such as medical staff cooperation, managing patient emotions, role clarity, and skill development. The score suggests a need to address these challenges to improve the training experience and better prepare students for careers in emergency departments.
Factor 2, titled “Integrated Emergency Department Training and Competence Development”, encompasses support from medical staff, alignment with nursing program objectives, effective communication, skill development, hands-on experience, professionalism, and career aspirations. This factor offers a holistic perspective on nursing students’ training experiences and their preparedness for careers in emergency departments. Thirteen items were loaded on this factor, with loadings ranging from 0.77 to 0.54, explaining 23.31% of the variance. Notable items with loadings above 0.70 include medical staff cooperation, dealing with various patient emotions, and clearly defined responsibilities during training. A mean score of 3.70 out of 5 indicates a moderately positive emergency department training experience for nursing students, covering support, communication, skill development, and career aspirations. However, there is room for improvement in preparing students for careers in emergency departments.
The third factor initially had few items explaining 5.48% of the variance, and after removing redundant and cross-loaded items, no additional items were loaded on it. As a result, only two factors were retained and extracted from the data: (1) “Emergency Department Training and Skill Development” and (2) “Integrated Emergency Department Training and Competence Development”. These two factors provide a comprehensive understanding of the nursing interns’ training experiences in emergency departments.
Table 3 presents the results for two factors related to emergency department training for nursing students, including the mean scores, standard deviation (SD), number of items, and Cronbach’s alpha. Factor 1, “Challenges of Emergency Department Training and Skill Development”, has a mean of 2.86, indicating moderately below-average challenges faced, an SD of 0.71, 15 items, and a Cronbach’s alpha of 0.909, showing high internal consistency. Factor 2, “Comprehensive Emergency Department Training Experiences”, has a mean of 3.70, indicating a moderately positive overall experience, an SD of 0.73, 13 items, and a Cronbach’s alpha of 0.900, also demonstrating high internal consistency.

Table 3.
Factors affecting internship in the emergency department.
4. Discussion
This study aimed to explore the factors affecting nursing internship experiences in emergency departments (EDs) within the Kingdom of Saudi Arabia. A total of 126 responses were collected, and principal component analysis (PCA) identified two factors influencing the internship experience, accounting for 56.63% of the total variance. The results revealed two significant factors: (1) “Emergency Department Training and Skill Development”, which focused on challenges encountered during training, and (2) “Integrated Emergency Department Training and Competence Development”, which offered a comprehensive view of nursing students’ experiences and preparedness for their careers. The findings suggest that nursing interns face challenges related to emergency training proficiency, communication, and the overall difficulties of working in EDs. Furthermore, the results emphasize the importance of aligning training programs with clinical practice demands and the potential influence of ED experiences on interns’ career aspirations [30,31,32]. By addressing these challenges and aligning training with educational goals, the nursing internship experience can be enhanced, promoting positive career aspirations and facilitating a smoother transition into professional practice [1,17,32].
The study’s findings have several implications for nursing education, practice, and further research. Challenges faced by nursing internship students, such as technical and procedural difficulties, communication and decision-making issues, and personal well-being and safety concerns, highlight the need for nursing education programs to focus more on preparing students for the complexities of emergency care. Future research could investigate the most effective teaching strategies and simulation experiences to enhance nursing students’ preparedness for emergency situations [33,34,35]. Additionally, educators might consider incorporating more hands-on experiences and interprofessional collaboration opportunities for students to develop skills in rapid decision-making and diverse case management [36,37].
As this study demonstrated that communication is a significant barrier for nursing interns in EDs, it is suggested that communication skills training should be a priority in nursing curricula [20]. This could include developing students’ competency in medical terminology, effective communication with patients and families, and interprofessional collaboration [38]. The impact of targeted communication interventions on nursing students’ experiences and outcomes in clinical settings could be explored in further research. Moreover, providing support for students with language barriers, such as offering language courses or translation tools, may help alleviate communication challenges and enhance their overall clinical experiences [33,39].
Finally, the findings emphasize the importance of offering adequate support for nursing interns in EDs. This support may include assigning dedicated trainers or mentors, providing stress management resources, and fostering a supportive learning environment [1,33,40]. It is essential for nursing training programs to align with the actual demands and realities of working in emergency departments, facilitating a smoother transition to professional practice [1,6,34]. Further research could investigate the long-term effects of improved training alignment on nursing interns’ career trajectories and job satisfaction, as well as the potential impact on patient outcomes in emergency care settings.
5. Recommendations
- Enhance the integration and alignment of nursing curricula with practical training objectives:
- Ensure that the Bachelor of Nursing program objectives are closely aligned with the skills and knowledge required in emergency department settings;
- Provide opportunities for internship students to acquire technical skills, such as operating medical equipment, by incorporating hands-on training and simulation experiences within the curriculum.
- Strengthen the development of interpersonal and professional skills:
- Integrate emotional intelligence training and support for handling various patient emotions within nursing education programs;
- Emphasize the importance of professionalism, communication, and leadership skills in the curriculum and provide targeted training to enhance these competencies.
- Foster a supportive learning environment during clinical training:
- Encourage medical staff to actively cooperate with and support nursing internship students during their training in emergency departments;
- Promote effective communication between nursing internship students and medical staff, including addressing potential language barriers and fostering a culture of collaboration and respect.
- Facilitate opportunities for diverse clinical experiences and career exploration:
- Provide nursing internship students with opportunities to gain experience in various emergency departments, allowing them to become familiar with different settings and patient populations;
- Encourage nursing internship students to reflect on their training experiences to identify areas of interest and consider potential career paths in emergency departments or other specialized areas of nursing.
6. Limitations
The main limitation of this study is the small sample size, which may affect the validity of the new questionnaire. Future research for confirmatory factor analysis (CFA) with larger samples is needed to confirm our findings and develop a more reliable instrument.
7. Conclusions
In conclusion, this study illuminates the factors influencing nursing interns’ experiences in emergency departments (EDs) within the Kingdom of Saudi Arabia. The findings reveal challenges related to emergency training proficiency, communication, and general training struggles, emphasizing the need for targeted interventions to enhance nursing education and practice in ED settings. By improving emergency care preparedness, addressing communication challenges, and ensuring proper alignment between training programs and clinical practice, nursing interns can experience a more positive and supportive learning environment. Consequently, this may foster positive career aspirations and facilitate a smoother transition to professional practice. Further research is encouraged to explore effective teaching strategies, interventions targeting communication skills, and the long-term effects of improved training alignment on nursing interns’ career trajectories, job satisfaction, and patient outcomes in emergency care settings. As the tool is new, we plan to continue evaluating it by conducting a confirmatory factor analysis (CFA) to ensure its consistent validity and reliability.
Author Contributions
Conceptualization, M.M.A. and A.A.T. (Abeer Adel Turkistani); methodology, R.M.A. (Reem Mutlaq Alotaibi); software, A.A.T. (Abeer Adel Turkistani) and A.A.T. (Abdulellah Al Thobaity); validation, Z.S.A.; formal analysis, M.H.A. and A.A.T. (Abdulellah Al Thobaity); investigation, R.M.A. (Rawan Maqbool Alkhaldi); resources, L.S.A.; data curation, A.A.T.; writing—original draft preparation, R.M.A. (Rawan Maqbool Alkhaldi) and A.A.T. (Abeer Adel Turkistani); writing—review and editing, A.A.T. (Abdulellah Al Thobaity); visualization, R.M.A. (Rawan Maqbool Alkhaldi); supervision, A.A.T. (Abdulellah Al Thobaity); project administration, A.A.T. (Abdulellah Al Thobaity). All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board (or Ethics Committee) of Taif; IRB registration number with KACST, KSA: HAP-02-T-067, approval number: 767, and date: 23 December 2022.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data is unavailable due to privacy or ethical restrictions.
Acknowledgments
The investigators are grateful to the Deanship of Scientific Research at Taif University for financially supporting this project. We also extend our heartfelt thanks to all participants who generously contributed their time to this research. Our appreciation goes to Joud Saad Almalki for her invaluable assistance and unwavering support in refining the instrument prior to distribution among the participants.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Ahmadi, S.; Abdi, A.; Nazarianpirdosti, M.; Rajati, F.; Rahmati, M.; Abdi, A. Challenges of clinical nursing training through internship approach: A qualitative study. J. Multidiscip. Healthc. 2020, 13, 891–900. [Google Scholar] [CrossRef] [PubMed]
- Duchscher, J.B. A process of becoming: The stages of new nursing graduate professional role transition. J. Contin. Educ. Nurs. 2008, 39, 441–450, quiz 451–442, 480. [Google Scholar] [CrossRef] [PubMed]
- Mousa, A.; Menssey, R.F.M.; Kamel, N.M.F. Relationship between perceived stress, emotional intelligence and hope among intern nursing students. IOSR J. Nurs. Health Sci. 2017, 6, 75–83. [Google Scholar] [CrossRef]
- Vae, K.J.U.; Engström, M.; Mårtensson, G.; Löfmark, A. Nursing students’ and preceptors’ experience of assessment during clinical practice: A multilevel repeated-interview study of student–preceptor dyads. Nurse Educ. Pract. 2018, 30, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Levett-Jones, T.; Lathlean, J.; Higgins, I.; McMillan, M. Staff–student relationships and their impact on nursing students’ belongingness and learning. J. Adv. Nurs. 2009, 65, 316–324. [Google Scholar] [CrossRef] [PubMed]
- Killam, L.A.; Heerschap, C. Challenges to student learning in the clinical setting: A qualitative descriptive study. Nurse Educ. Today 2013, 33, 684–691. [Google Scholar] [CrossRef]
- Morphet, J.; Hood, K.; Cant, R.; Baulch, J.; Gilbee, A.; Sandry, K. Teaching teamwork: An evaluation of an interprofessional training ward placement for health care students. Adv. Med. Educ. Pract. 2014, 5, 197–204. [Google Scholar]
- Duchscher, J.E.B. Transition shock: The initial stage of role adaptation for newly graduated registered nurses. J. Adv. Nurs. 2009, 65, 1103–1113. [Google Scholar] [CrossRef]
- Sharif, F.; Masoumi, S. A qualitative study of nursing student experiences of clinical practice. BMC Nurs. 2005, 4, 6. [Google Scholar] [CrossRef]
- Rush, K.L.; Adamack, M.; Gordon, J.; Lilly, M.; Janke, R. Best practices of formal new graduate nurse transition programs: An integrative review. Int. J. Nurs. Stud. 2013, 50, 345–356. [Google Scholar] [CrossRef]
- Thomas, L.J.; Asselin, M. Promoting resilience among nursing students in clinical education. Nurse Educ. Pract. 2018, 28, 231–234. [Google Scholar] [CrossRef] [PubMed]
- Rahman, R. The Privatization of Health Care System in Saudi Arabia. Health Serv. Insights 2020, 13, 1178632920934497. [Google Scholar] [CrossRef] [PubMed]
- Al-Dossary, R.N.; Kitsantas, P.; Maddox, P. Residency programs and clinical leadership skills among new Saudi graduate nurses. J. Prof. Nurs. 2016, 32, 152–158. [Google Scholar] [CrossRef] [PubMed]
- Alboliteeh, M.; Magarey, J.; Wiechula, R. The profile of Saudi nursing workforce: A cross-sectional study. Nurs. Res. Pract. 2017, 2017, 1710686. [Google Scholar] [CrossRef] [PubMed]
- Almalki, M.; FitzGerald, G.; Clark, M. The nursing profession in Saudi Arabia: An overview. Int. Nurs. Rev. 2011, 58, 304–311. [Google Scholar] [CrossRef]
- Albejaidi, F.M. Healthcare system in Saudi Arabia: An analysis of structure, total quality management and future challenges. J. Altern. Perspect. Soc. Sci. 2010, 2, 794–818. [Google Scholar]
- Al Najjar, H.; Rawas, H. Factors affecting the clinical practice of nursing interns at tertiary hospital Jeddah in Saudi Arabia. Int. J. Stud. Nurs. 2018, 3, 45. [Google Scholar] [CrossRef]
- Al-Momani, M.M. Difficulties encountered by final-year male nursing students in their internship programmes. Malays. J. Med. Sci. MJMS 2017, 24, 30. [Google Scholar] [CrossRef]
- Alamri, A.A.; Sami, R.N. Alhamidi Exploring the Barriers and Challenges Saudi Arabian Nursing Students Encounter during their Internship Program: A Qualitative Study. Saudi J. Nurs. Health Care 2022, 5, 64–70. [Google Scholar] [CrossRef]
- Alharbi, A.R.; Alhosis, K.F. The challenges and difficulties of the nursing interns during their clinical internship in Qassim Region, Saudi Arabia. Saudi J. Health Sci. 2019, 8, 6. [Google Scholar]
- Alsadaan, N.; Jones, L.K.; Kimpton, A.; DaCosta, C. Challenges Facing the Nursing Profession in Saudi Arabia: An Integrative Review. Nurs. Rep. 2021, 11, 395–403. [Google Scholar] [CrossRef]
- Althaqafi, S.S.; Alhatimi, H.A.; Almalki, A.M.; Alyamani, O.M.; Banakhar, M.A. Nursing students’ clinical practice experience during the internship year at different hospitals: A qualitative study. Am. J. Nurs. Sci. 2019, 8, 255–262. [Google Scholar] [CrossRef]
- AlThiga, H.; Mohidin, S.; Park, Y.S.; Tekian, A. Preparing for practice: Nursing intern and faculty perceptions on clinical experiences. Med. Teach. 2017, 39, S55–S62. [Google Scholar] [CrossRef]
- Wambui, W.M.; Githui, S.N. Nurse Interns’ Satisfaction with the Clinical Learning Environment: A Cross-Sectional Study. Int. J. Adv. Res. 2019, 7, 164–169. [Google Scholar] [CrossRef]
- Baraz, S.; Memarian, R.; Vanaki, Z. Learning challenges of nursing students in clinical environments: A qualitative study in Iran. J. Educ. Health Promot. 2015, 4, 52. [Google Scholar]
- Kalyani, M.N.; Jamshidi, N.; Molazem, Z.; Torabizadeh, C.; Sharif, F. How do nursing students experience the clinical learning environment and respond to their experiences? A qualitative study. BMJ Open 2019, 9, e028052. [Google Scholar] [CrossRef]
- Elbilgahy, A.A.; Eltaib, F.A.; Lawend, J.A. Challenges facing clinical nurse educators and nursing students in Egyptian and Saudi clinical learning environment: A comparative study. Int. J. Afr. Nurs. Sci. 2020, 13, 100240. [Google Scholar] [CrossRef]
- Bano, N.; Al Najjar, H. Experiences of nursing interns with the application of knowledge and skills in drug administration: A qualitative study. Saudi J. Health Sci. 2020, 9, 227. [Google Scholar]
- Williams, B.; Onsman, A.; Brown, T. Exploratory factor analysis: A five-step guide for novices. Australas. J. Paramed. 2010, 8, 1–13. [Google Scholar] [CrossRef]
- Hair, J.F. Multivariate Data Analysis; Kennesaw State University: Kennesaw, GA, USA, 2009. [Google Scholar]
- Pett, M.A.; Lackey, N.R.; Sullivan, J.J. Making Sense of Factor Analysis: The Use of Factor Analysis for Instrument Development in Health Care Research; SAGE: Newbury Park, CA, USA, 2003. [Google Scholar]
- Bahari, G.; Alharbi, F.; Alharbi, O. Facilitators of and barriers to success in nursing internship programs: A qualitative study of interns’ and faculty members’ perspectives. Nurse Educ. Today 2022, 109, 105257. [Google Scholar] [CrossRef]
- Nevin, M.; Neill, F.; Mulkerrins, J. Preparing the nursing student for internship in a pre-registration nursing program: Developing a problem based approach with the use of high fidelity simulation equipment. Nurse Educ. Pract. 2014, 14, 154–159. [Google Scholar] [CrossRef] [PubMed]
- Cheraghi, M.A.; Salasli, M.; Ahmadi, F. Factors influencing the clinical preparation of BS nursing student interns in Iran. Int. J. Nurs. Pract. 2008, 14, 26–33. [Google Scholar] [CrossRef]
- Algahtani, H.; Shirah, B.; Bukhari, H.; Alkhamisi, H.; Ibrahim, B.; Subahi, A.; Aldarmahi, A. Perceptions and attitudes of different healthcare professionals and students toward interprofessional education in Saudi Arabia: A cross-sectional survey. J. Interprof. Care 2021, 35, 476–481. [Google Scholar] [CrossRef] [PubMed]
- Guerrero, J.G.; Hafiz, A.H.; Eltohamy, N.A.E.; Gomma, N.; Al Jarrah, I. Repeated exposure to high-fidelity simulation and nursing interns’ clinical performance: Impact on practice readiness. Clin. Simul. Nurs. 2021, 60, 18–24. [Google Scholar] [CrossRef]
- Glynn, P.; Silva, S. Meeting the needs of new graduates in the emergency department: A qualitative study evaluating a new graduate internship program. J. Emerg. Nurs. 2013, 39, 173–178. [Google Scholar] [CrossRef]
- Banakhar, M.; Bamohrez, M.; Alhaddad, R.; Youldash, R.; Alyafee, R.; Sabr, S.; Sharif, L.; Mahsoon, A.; Alasmee, N. The journey of Saudi male nurses studying within the nursing profession: A qualitative study. Nurs. Rep. 2021, 11, 832–846. [Google Scholar] [CrossRef]
- Edwards, D.; Hawker, C.; Carrier, J.; Rees, C. A systematic review of the effectiveness of strategies and interventions to improve the transition from student to newly qualified nurse. Int. J. Nurs. Stud. 2015, 52, 1254–1268. [Google Scholar] [CrossRef]
- Alhamidi, S.A. Mentoring role effectiveness and satisfaction during internship training: A psychometric evaluation of Saudi nursing interns. Collegian 2022, 29, 252–262. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).