Abstract
Background and Aim: Medical students are required to complete a number of clinical rotations in hospital departments, affiliated with the Azrieli Faculty of Medicine, under the supervision of a department tutor. Our experience shows that departments receiving good scores typically also receive good feedback for their tutor. Accordingly, our aim was to assess the tutor contribution to students’ overall satisfaction from clinical rotations in hospital departments across northern Israel. Methods: Here, we recorded the students’ reported satisfaction with tutors as well as the satisfaction with clinical rotations in different departments of Galilee Medical Center (GMC) in Naharia, and Baruch Padeh Medical Center in Poria. The students’ reported satisfaction was assessed numerically and verbally using questionnaires over a period of three years. Results: We find that the students reported satisfaction with a clinical rotation is positively and significantly correlated with the student satisfaction with the tutor, and less with other factors such as hospital organization and department facilities, geographical distance from home, working hours, etc. Conclusion: Our findings suggest that medical schools can increase students’ satisfaction through investment in good tutors.
1. Background
Faculty members are naturally assumed to possess the skills of teaching, mentoring, and tutoring [1]. This assumption is not clear and several studies have challenged this view [2,3]. To improve the teaching skills of their members, several faculties have developed dedicated training programs that go beyond disciplinary expertise [4]. Such training programs extend the basic pedagogic knowledge of faculty members and improve the learning experience for both teachers and students alike [5].
As part of the requirements to become a physician, medical students must complete clinical rotations in hospitals. Successful completion of clinical rotations is paramount for building professionalism and contributes to confidence and performance in the clinic [6].
To assess teaching skills at our Faculty, students are constantly surveyed using satisfaction questionnaires [7]. Based on such student surveys, several studies have characterized important markers for successful teaching, mentoring, and tutoring. One study shows that the optimal duration of clinical rotations is around 7 weeks, based on students’ satisfaction [8]. Another study shows that student satisfaction is associated mostly with the clinical learning environment, but less with the ward premises, the ward manager, and the pedagogical atmosphere [9]. In contrast, another study shows that student satisfaction is correlated equally with the clinical learning environment, the ward premises, the ward manager, the pedagogical atmosphere, and last but not least, the relationship with the supervising tutor (i.e., mentor) [10]. The student’s satisfaction with the tutor–student relationship has been shown to contribute most to instruction rating [11]. Likewise, most students reported that the rotation was a useful educational experience and that the tutoring coach was one of the most valuable aspects of clinical rotation [12].
Teaching strategies also matter for the well-being of students. Inspiring teaching strategies, characterized by articulation, reflection, and exploration, are related to reduced burnout among medical students and an increased sense of satisfaction [13]. Mindfulness, resilience, and need satisfaction are associated with lower perceived stress [14]. Overall, medical students prioritize clarity, relevance, and competence as necessary components for effective instruction, whereas other teaching characteristics are considered luxury components [15].
In this study, we evaluated the satisfaction of MD students with the clinical rotations, the tutors that supervised them, the physicians that taught them, the hospital organization, department facilities, and distance from home, and attempted to identify correlations between these.
2. Methods
This study was conducted at the Azrieli Faculty of Medicine in Galilee, Bar Ilan University, Safed, Israel. The study was judged “exempt” by the Faculty research ethical committee, and all of the student participants signed a written informed consent form to participate in the study.
2.1. Clinical Rotation Structure
As part of the MD degree requirements, students are expected to complete mandatory clinical rotations in hospital departments selected by the Faculty. Each clinical rotation comprises a small group of MD students from our Faculty. We have two tracks in our Faculty: one track included students who studied medicine for 3 years abroad (aged from 25 to 28 years, 60% women and 40% men), and the other track included students who had received an undergraduate degree in Israel (aged 27 to 33 years, 60–70% woman and 30–40% men). The small student groups described above contained a mixture of students from the two tracks. Before clinical rotations, the students divided themselves into small groups (i.e., between 7 and 12 students) which they remained in throughout all their clinical rotations. All clinical rotations in this study were conducted in the years 2014–2016 in the departments of (1) internal medicine, (2) pediatrics, (3) OB-GYN, and (4) surgery. The clinical rotations took place at Galilee Medical Center (GMC) of Naharia and Baruch Padeh Medical Center of Poria hospitals affiliated with the Faculty of Medicine of Bar Ilan University. Each clinical rotation was directed by a tutor both administratively and academically. Clinical rotations began with an introduction by the tutor about the rotation rationale and goals. Then, the students were assigned by the tutor to assist one or more physicians in the department. For most rotations, the students were expected to arrive at 7:00 and not leave before 15:30. In addition, the students were expected to attend all planned department meetings. Once a week, the tutor provided structured lectures and briefings regarding the department. Clinical rotations were concluded with a summary and with feedback discussions. The average duration of each clinical rotation was 6 weeks. At the end of each rotation, the tutor graded the students, and the students were offered to evaluate tutors anonymously.
2.2. Tutor Role
The role of the tutor in clinical rotations was both administrative and academic. Administratively, the tutor’s role included planning curricular schedules, making sure students get lunch breaks, and solving everyday problems. Academically, the tutor’s role included bedside teaching, instruction of students during physical examinations, and tuition through new active teaching methods, such as team-based learning (TBL). The main role of the tutor was to convey clinical thought processes and skills for the practice of medicine, including history-taking, physical examination, and differential diagnosis, as well as the multidisciplinary approach to patients and their families and integration into a multidisciplinary medical team. The tutor acts as an educator, a custodian, a caretaker, a teacher, and a mentor. The tutor served as the acting director of the clinical round and was supervised by the department head. All tutors resided in the north of Israel and were experts in their field.
2.3. Clinical Rotation and Tutor Assessment
At the end of each clinical rotation, participants were requested to complete an evaluation questionnaire, assessing the perceived ability and skills of the tutor, the clinical teachers, and the head of the department, as well as the perceived satisfaction of the clinical round. The participants were additionally asked to assess to which extent the clinical rotation contributed to their skills as future physicians, and to which extent the rotation was satisfactory in terms of hospital organization and department facilities, department directors, and tutors.
To numerically assess the perceived satisfaction of the clinical rotation, our questionnaires used the Likert scale ranging from 1 to 5, corresponding to “very high”, “high”, “intermediate”, “little”, and “very little” satisfaction. To numerically assess the perceived satisfaction of the tutor, clinical teachers, and heads of departments the written assessments of our questionnaires were interpreted into a scale ranging from 1 to 3, corresponding to “bad feedback only”, “neutral feedback”, and “good feedback only” scores, respectively. For the sake of clarity, all scales of the questionnaires were provided in detail and independently analyzed by three of the authors (N.D., B.H., and L.E.). The interpreted score (good, neural, and bad feedback) was taken as the consensus, agreed upon by all three authors. In case of disaccord, then, the majority score of 2 out of 3 reviewers was taken as the consensus score. If all three reviewers provided a different score (1 good, 1 neutral, and 1 bad), then a neutral score was taken as the consensus score.
2.4. Statistical Analysis
In this study, we attempted to correlate the perceived satisfaction of clinical rotations and tutors using the Spearman coefficient factor, and the Kruskal–Wallis test was used for comparisons in more than two groups. Descriptive statistics were used to display the distribution of perceived tutor characteristics, and perceived rotation satisfaction from the questionnaires. All p-values were two-sided, and only p-values less than 0.05 were considered statistically significant. A copy of the questionnaire is shown in the Supplementary Materials (Table S1).
3. Results
3.1. Perceived Satisfaction of Clinical Rotations
In this study, we examined the performance of 102 clinical rotations in various hospitals and departments across northern Israel, using verbal and numerical questionnaires of 710 students. The number of students that responded to the questionnaires was 282 in 2014, 219 in 2015, and 209 in 2016. The perceived student satisfaction with the respective clinical rotations in this period is provided in Figure 1. The satisfaction histogram distribution is almost identical for each year of the three-year period, and no time trend was captured. The satisfaction, which was not normally distributed, indicated a p-value of 0.17 in the Kruskal–Wallis test of 2014, 2015, and 2016. Approximately half of the students were very highly satisfied, and somewhat less than a 1/3 were highly satisfied. About 15% were intermediately satisfied, while less than 10% were unsatisfied. When numerically assessed (Likert scale: 1, 2, 3, 4, and 5, corresponding to “very little”, “little”, “intermediate”, “high”, and “very high” satisfaction) the mean satisfaction was reassuringly high with a value of 4.11 out of 5. The standard deviation of the study corresponded to 1.06, and the statistical distribution corresponded to a right-skewed Gaussian bell curve. There were no differences in our results related to demographic parameters such as students, age, and gender.
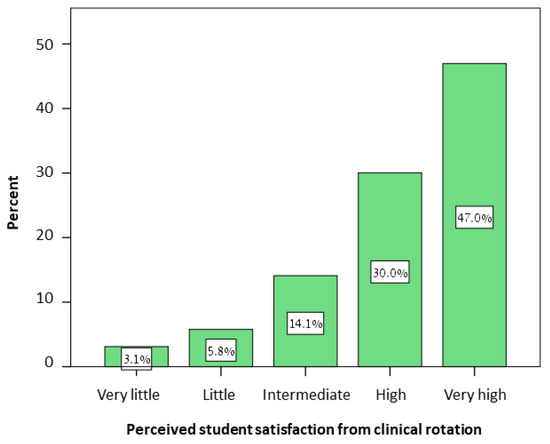
Figure 1.
Perceived satisfaction of clinical rotations. Shown is a histogram of the perceived satisfaction of students from clinical rotations.
3.2. Perceived Satisfaction with the Tutor
The reported performance of the 40 tutors of the 102 clinical rotations was evaluated based on the written assessments of the questionnaires and translated into a numerical scale. As tutors were not rated using the Likert scale, the numerical scale ranged from 1 to 3 and corresponded to “bad feedback only”, “neutral feedback”, and “good feedback only” scores, respectively. Examples of written assessments as well as their interpretation and numerical value are listed in Table 1. Note that the written assessment was translated from Hebrew. As a rule of thumb, if tutors received only positive feedback, then they got a “good feedback only” score; if tutors received both positive and negative feedback, then they obtained a “neutral feedback” score; and if tutors received only negative feedback, then they received a “negative feedback only” score. Good feedback included praiseworthy clinical knowledge (e.g., informed, familiar, proficient), and skills (qualified, accustomed, capable), as well as academic rhetorics (teacher, speaker, lecturer, explainer, orderly, explain in detail, charismatic, motivational), personal attachment (caring, giving, engaging, available, pleasant, present, patient, professional, etc.).

Table 1.
Examples of written assessments and their interpretation and numerical value.
3.3. Correlation of Satisfaction of Clinical Rotation and Satisfaction of Tutor
Figure 2 shows the perceived satisfaction of the clinical round, plotted against the interpreted tutor score. A positive, high, and significant correlation was found between the tutor score and the perceived satisfaction of clinical rounds (rs = 0.78, p < 0.01). This finding implied that 61% of the variance in student satisfaction was explained by their satisfaction with the tutor.
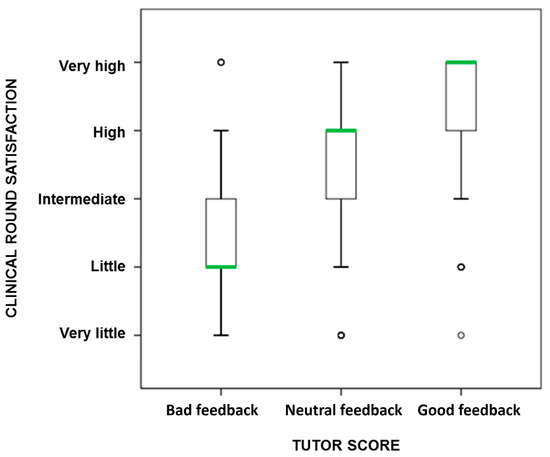
Figure 2.
Satisfaction of clinical round plotted against tutor score. Shown is the average perceived student satisfaction of clinical round plotted for each of the tutor scores: bad feedback only, neutral feedback, and good feedback only.
Interestingly, the main factor contributing to the satisfaction of a rotation was the overall satisfaction with the tutor. This trend is shown in Figure 3, where the worst tutors (i.e., “bad feedback only”) were replaced with better tutors (i.e., “neutral feedback” and “good feedback only”) halfway through the first rotations of 2014 and 2015. After the replacement, the satisfaction of the rotation correlated linearly with the satisfaction of the tutor.
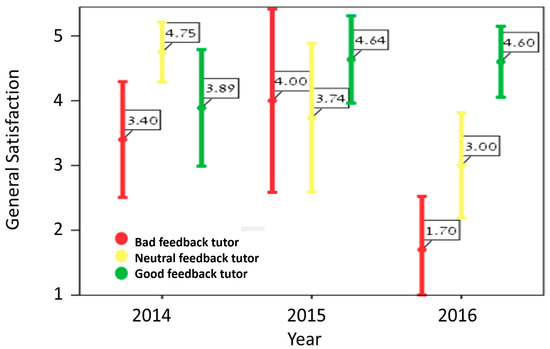
Figure 3.
The main factor contributing to perceived satisfaction of rotation is the tutor. Shown is the mean satisfaction plotted against year. Note that when a not good tutor was replaced with an excellent tutor in 2015, then the general satisfaction of a rotation became linear.
Statistically speaking, the satisfaction of a rotation could be multifactorial, and depend on other parameters than the tutor. Based on our findings, however, the main factor contributing to rotation success was the tutor. The perceived satisfaction of a rotation was not correlated with the perceived satisfaction of the other clinical teachers, department heads, hospital organizations, and department facilities (p > 0.01).
4. Discussion
In this study, we find that student satisfaction with clinical rotations is positively and significantly correlated with student satisfaction with the tutor. We do not find any correlation with hospital organizations, department facilities, and department heads. Our findings agree with earlier findings showing that tutors matter most in the satisfaction of clinical rotations [11,12]. Our findings are in partial agreement with earlier reports showing that other confounders matter less, such as the department premises (rs = 0.51), the department director (rs = 0.34), and the pedagogical atmosphere (rs = 0.38) [10]), but contrast another report showing that the aforementioned factors matter equally [9]. In all cases, however, the tutor matters. As a result, tutors are now rated using a Likert scale in all student satisfaction questionnaires of clinical rounds.
Our findings also underline desirable characteristics of tutors that increase the success of clinical rotations. Desirable tutor characteristics, as provided by our students in the good feedbacks, include praiseworthy clinical knowledge, clinical skills, academic rhetorics, and personal attachment. These characteristics are in agreement with earlier descriptions of a “good educator”, and include (a) a good communicator; (b) approachable; (c) relatable; (d) helpful; (e) friendly; (f) a subject matter expert; (g) sensitive to student needs; (h) enthusiastic; and (i) patient [16]. Likewise, ideal tutor characteristics, as perceived by pharmacy students are (a) enthusiasm; (b) subject matter experts; and (c) clear presentation [17]. Such desirable characteristics have also been reported by Arnon and Reichel who examined current and recently graduated student teachers’ perspectives to conceptualize an “image of the ideal teacher”, and summarized the ideal educator by personality and professional knowledge [18].
As a potential limitation of this study, we do not take into account confounding factors, such as the hospital prestige and tutor acclamation, based on the number of papers published, tutor salary, and tutor’s native tongue. These factors could all be important contributors to the success of clinical rotation; however, they are out of scope. Nevertheless, based on partial data, we estimate that tutor experience, tutor age, and tutor gender have little or no effect on student satisfaction (p > 0.01). Another potential limitation is that only ~40% of students responded to the questionnaires and that their opinions could not reflect the majority view. Finally, one of the potential limitations of this study is that verbal assessment is not easily translated into numbers, and that only about 75% of the students provided verbal comments.
5. Conclusions
In this study, we find that rotation satisfaction is correlated with the tutor. Since tutors of medical students could be the single most important factor for the success of clinical rotations, this study suggests devoting more resources to tutors. This is not surprising since we strive for excellence.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ime2030012/s1, Table S1: Teaching survey.
Author Contributions
N.D. and L.E. conceived the study and participated in its design and coordination. B.H. contributed to the interpretation of the data, and A.O.S. wrote the paper. All authors have read and agreed to the published version of the manuscript.
Funding
No funding was obtained for this research.
Institutional Review Board Statement
This project was judged “exempt” by the Research Ethics Committee of the Azrieli Faculty of Medicine, Bar-Ilan University.
Informed Consent Statement
The participants provided written consent to participate in the study.
Data Availability Statement
Not applicable.
Acknowledgments
The authors would like to thank all the students involved in this project. We thank the Dean of the Faculty of Medicine, Karl Skorecki, as well as the former Dean, Ran Tur-Kaspa, for their comments.
Conflicts of Interest
The authors declare no conflict of interests.
Abbreviations
Dr.—Doctor; GMC—Galilee Medical Center; Ob-gyn—Obstetrics and Gynecology.
References
- Benor, D.E. Faculty development, teacher training and teacher accreditation in medical education: Twenty years from now. Med. Teach. 2000, 22, 503–512. [Google Scholar] [CrossRef] [PubMed]
- Unterman, A.; Achiron, A.; Gat, I.; Tavor, O.; Ziv, A. A novel simulation-based training program to improve clinical teaching and mentoring skills. Isr. Med. Assoc. J. IMAJ 2014, 16, 184–190. [Google Scholar] [PubMed]
- McLean, M.; Cilliers, F.; Van Wyk, J.M. Faculty development: Yesterday, today and tomorrow. Med. Teach. 2008, 30, 555–584. [Google Scholar] [CrossRef] [PubMed]
- Steinert, Y.; Mann, K.; Centeno, A.; Dolmans, D.; Spencer, J.; Gelula, M.; Prideaux, D. A systematic review of faculty development initiatives designed to improve teaching effectiveness in medical education: BEME Guide No. 8. Med. Teach. 2006, 28, 497–526. [Google Scholar] [CrossRef] [PubMed]
- McLeod, P.J.; Steinert, Y.; Meagher, T.; Schuwirth, L.; Tabatabai, D.; McLeod, A.H. The acquisition of tacit knowledge in medical education: Learning by doing. Med. Educ. 2006, 40, 146–149. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, B.C.; Irby, D.M. Enacting the Carnegie Foundation call for reform of medical school and residency. Teach. Learn. Med. 2013, 25 (Suppl. S1), S1–S8. [Google Scholar] [CrossRef] [PubMed]
- Barash, A.; Toledano, N.; Maoz, E.; Blumberg, Y.; Dickman, N.; Karasik, D. Summing up 10 years in a new medical school: Per aspera ad astra. FASEB J. 2022, 36, S1. [Google Scholar] [CrossRef]
- González-García, A.; Díez-Fernández, A.; Leino-Kilpi, H.; Martínez-Vizcaíno, V.; Strandell-Laine, C. The relationship between clinical placement duration and students’ satisfaction with the quality of supervision and learning environment: A mediation analysis. Nurs. Health Sci. 2021, 23, 688–697. [Google Scholar] [CrossRef] [PubMed]
- Adam, A.B.; Druye, A.A.; Kumi-Kyereme, A.; Osman, W.; Alhassan, A. Nursing and midwifery students’ satisfaction with their clinical rotation experience: The role of the clinical learning environment. Nurs. Res. Pract. 2021, 2021, 7258485. [Google Scholar] [CrossRef] [PubMed]
- Alatawi, A.; Domantay, A.A.; ALatawi, M.; Qawwadi, S.; ALhiri, M.; ALbalawi, T.; Majrashi, L.; ALatawi, H. Nursing Students’ Satisfaction of the Clinical Learning Environment in Saudi Arabia. Int. J. Nurs. Didact. 2020, 10, 9–17. [Google Scholar]
- Neufeld, A.; Malin, G. How medical students’ perceptions of instructor autonomy-support mediate their motivation and psychological well-being. Med. Teach. 2020, 42, 650–656. [Google Scholar] [CrossRef] [PubMed]
- Sigler, R.; Roberts, E.; Welford, E.; Keehner, J.; Wooten, D. Evaluation of an Infectious Diseases Elective for Early Clinical Medical Students on Their Internal Medicine Clerkship. Open Forum Infect. Dis. 2022, 9, ofac120. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.K.; Yen-Ju Lin, B.; Chen, D.Y. Do teaching strategies matter? Relationships between various teaching strategies and medical students’ wellbeing during clinical workplace training. Med. Teach. 2020, 42, 39–45. [Google Scholar] [CrossRef] [PubMed]
- Neufeld, A.; Mossière, A.; Malin, G. Basic psychological needs, more than mindfulness and resilience, relate to medical student stress: A case for shifting the focus of wellness curricula. Med. Teach. 2020, 42, 1401–1412. [Google Scholar] [CrossRef] [PubMed]
- Knoster, K.; Goodboy, A.; Martin, M.; Thomay, A. What matters most? A prioritization of medical students’ preferences for effective teaching. Commun. Educ. 2021, 70, 183–200. [Google Scholar] [CrossRef]
- McLean, M. Qualities attributed to an ideal educator by medical students: Should faculty take cognizance? Med. Teach. 2001, 23, 367–370. [Google Scholar] [CrossRef] [PubMed]
- Alrakaf, S.M.; Sainsbury, E.; Rose, G.; Smith, L. Identifying achievement goals and their relationship to academic achievement in undergraduate pharmacy students. Am. J. Pharm. Educ. 2014, 78, 133. [Google Scholar] [CrossRef] [PubMed]
- Arnon, S.; Reichel, N. Who is the ideal teacher? Am I? Similarity and difference in perception of students of education regarding the qualities of a good teacher and of their own qualities as teachers. Teach. Teach. 2007, 13, 441–464. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).