Abstract
In recent decades, there has been a shift towards competency-based approaches in surgical training. The effectiveness of video-based learning (VBL) in enhancing surgical skills, particularly in the context of self-regulated learning (SR-VBL), was assessed in this study. While VBL is cost-effective, flexible, and can improve proficiency in technical skills prior to clinical practice, it is resource-challenging. SR-VBL includes many of VBL’s benefits but has utility in individual and distance settings due to its autarkic nature. This study identified and analyzed contemporary literature on SR-VBL using PRISMA guidelines, focusing on original randomized controlled studies published in international peer-reviewed journals during the COVID-19 pandemic in 2020–2022. Seven studies with 462 participants were included, with three eligible for the meta-analysis. The results showed that self-regulated video-based learning contributes to the learning of technical skills and can be applied to learners of all levels across surgical specialties. The meta-analysis revealed that improvements in validated outcome assessment scores (OSATS) were at least equal to traditional methods with a statistically significant result, though the effect was modest. Therefore, contemporary surgical training could incorporate SR-VBL for technical training to help surgeons of all levels in surgical self-assessment.
1. Introduction
Video-based learning (VBL) has become increasingly popular in higher education, surgical education included, having notably been accelerated by the COVID-19 pandemic [1,2,3,4]. VBL refers to remote instruction that uses live or prerecorded video to teach surgical skills and knowledge through a multi-sensory experience. VBL leverages auditory and visual cues for information dissemination, making it a cost-effective, flexible, and efficient method to improve proficiency in surgical skills prior to their application in clinical settings [2,3,4,5]. Mastering technical tasks before clinical application can alleviate associated stress [6]. In addition, technical mastery is beneficial to surgical outcomes [7]. While VBL has been shown to improve basic technical skills and knowledge [8,9,10], its impact on non-technical skills warrants further research [11,12]. However, it has the potential to be a powerful tool for enhancing surgical learning and increasing student satisfaction.
VBL can be used in various forms and for different purposes to enhance the learning of surgical skills. This ranges from teacher-guided VBL to more autonomous modes of learning, such as self-regulated or co-regulated VBL (SR-VBL) [13,14,15,16]. Teacher-guided VBL has been extensively studied in surgical learning and is beneficial to surgical residents of all levels, but it is typically resource-intensive [17,18,19]. Conversely, SR-VBL merely requires the recording of procedures, proving beneficial for self-assessment, proactivity, study engagement, resourcefulness, and continuous professional development. However, for learning to occur beyond merely watching a video, it is crucial to have effective and sustainable analytical tools in place [20].
Thus, while VBL presents an effective approach to surgical learning, the quality of the material used is paramount. Such material should undergo evaluation and standardization, criteria most often lacking in videos found on platforms such as YouTube [21].
Recently, the utility of SR-VBL in surgical skill learning has raised interest, especially due to its autarkic nature when healthcare environments are challenged in many ways. SR-VBL also has straightforward utility in individual and distance settings [15]. Self-assessment has proven to be a vital component of surgical training [22] and is also applicable to VBL in a self-regulated form. Reflection in surgical learning has been shown to not only improve non-technical skills, such as increased confidence and communication skills, but also technical skills [14,23,24]. In addition, reflecting on learning and thought processes improves control and promotes a quicker advancement to technical autonomy in procedures [25]. In SR-VBL, students are encouraged to take responsibility for their learning, set goals, engage in task analysis, use various strategies, reflect on their progress, and seek additional resources as needed. To be applied effectively for varied student groups and levels of learners, such learning calls for a long-term investment in cultivating self-regulated learning skills among medical students.
Despite the seemingly positive effects of SR-VBL in surgical learning, the literature is lacking in many aspects. First, terms related to SR-VBL are not used coherently, with incorrect terms such as ‘video-based coaching’, ‘video-feedback’, and ‘coaching-feedback’ being commonly used to imply aspects of SR-VBL. Second, many studies focus on highly selected groups, confounding their general applicability. Third, there is a dearth of systematic reviews addressing SR-VBL, especially considering the significant rise in the use of digital learning aids in recent years. To that end, we aimed to systematically summarize recent advancements in the utility of SR-VBL in promoting surgical learning through a systematic review and meta-analysis of randomized controlled trials, with a focus on the era during which the COVID pandemic forced most students into distance learning. Our primary outcome measure was to clarify whether SR-VBL can be used to cultivate the learning of surgical skills among less and more advanced medical learners ranging from medical students to surgical residents and whether it can be applied across multiple surgical disciplines. The secondary outcome assessed the effect of SR-VBL on technical skills with validated outcome measurement tools.
2. Materials and Methods
The literature search was conducted as per the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Two investigators (NP and SA) independently conducted searches on PubMed, ProQuest ERIC, and Cochrane databases on 17 April 2022. These databases were chosen for optimal coverage, focus on education and learning and high-quality research. The search keywords used were (video) AND (surgery) ((“video s” [All Fields] OR “videoed” [All Fields] OR “videotape recording” [MeSH Terms] OR (“videotape” [All Fields] AND “recording” [All Fields]) OR “videotape re-cording” [All Fields] OR “video” [All Fields] OR “videos” [All Fields]) AND (“surgery” [MeSH Subheading] OR “surgery” [All Fields] OR “surgical procedures, operative” [MeSH Terms] OR (“surgical” [All Fields] AND “procedures” [All Fields] AND “operative” [All Fields]) OR “operative surgical procedures” [All Fields] OR “general surgery” [MeSH Terms] OR (“general” [All Fields] AND “surgery” [All Fields]) OR “general surgery” [All Fields] OR “surgery s” [All Fields] OR “surgerys” [All Fields] OR “surgeries” [All Fields])) AND (randomizedcontrolledtrial [Filter]) with a filter for article types restricted to randomized controlled trials (RCT). The total search records were analyzed, and duplications were removed. Subsequently, the eligibility criteria were applied to screen the studies. Due to the restricted use of the appropriate terms “self-regulated video-based learning”, the literature searches were performed with broader terms, and selection was conducted in-person for the stringent inclusion/exclusion of articles.
2.1. Eligibility Criteria and Study Selection
The inclusion criteria for the studies were (Table 1): all the studies were peer-reviewed, and they applied varied modes of self-regulated video-based learning (SR-VBL) for operative interventions in surgical learning in a randomized controlled study. All studies were to include objective outcome assessments of the intervention. We included studies from 2020 onwards so as not to overlap with previous studies and to focus on the era during which the COVID pandemic forced most students into distance learning. Case reports, literature reviews, commentaries, editorials, conference abstracts, qualitative studies, and opinion articles were excluded. Studies not written in English were also excluded. For the quantitative synthesis, only studies assessing outcome with the OSATS-tool (Objective Structured Assessment of Technical Skills) were eligible [26]. The OSATS (Objective Structured Assessment of Technical Skills) is a validated assessment tool specifically designed to quantitatively measure and evaluate the technical proficiency of surgical skills in an objective manner.

Table 1.
Inclusion criteria.
2.2. Data Extraction
Search results were obtained by two independent researchers (NP and SA). Extracted information: first author’s name, publication year, article title, study period, study design, sample size, average age, number of surgeons performing the procedures, and learning outcomes. Disagreements were settled by discussion and consensus with the third author (HA). Data synthesis was independently performed by two investigators (NP and SA) using Microsoft Excel (version 16.72) spreadsheets.
2.3. Quality Assessment
The Jadad scale was used for quality assessment of the included RCTs [27]. The validated scale assesses the quality of RCTs under three domains: randomization, blinding, and withdrawals and dropouts. Using this scale, a maximum score of 5 and a minimum score of 1 can be assigned for the included studies. Two authors performed the methodological quality assessment (SA and NP). Any dispute was resolved through consensus or by discussion with a third author (HA).
2.4. Data Analysis
The baseline data were expressed as numbers, proportions, averages (mean or median), and ranges. RevMan 5.4 (Cochrane Collaboration, London, UK) was used to perform the meta-analysis. As the outcome of interest was continuous, the mean difference (with 95% CI) was calculated for each study. Subsequently, the weighted mean difference was estimated utilizing the inverse variance method. The level of heterogeneity among the studies was estimated using the I2 statistics. A random-effects model was used in the present study. A p-value of <0.05 was considered statistically significant. Artificial intelligence-based LLM software (AI Chat GPT) was used for controlling grammar and spelling after manuscript preparation.
3. Results
Altogether, we identified 3129 records, from which 510 duplicate articles were removed. The remaining 2619 records were screened for eligibility. Of these, 2585 were excluded after screening the abstracts, and the remaining 34 full texts were assessed for inclusion. From these, 27 were excluded due to ineligibility, and 7 studies were included for the systematic review, including 462 study subjects (Figure 1).
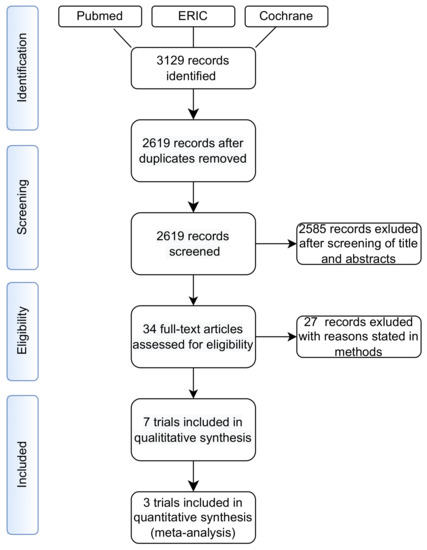
Figure 1.
Flowchart of study selection for systematic review and meta-analysis.
3.1. Summary of the Included Studies
We included seven articles for the systematic review, with 462 trainees, including both medical students and residents.
Chartrand et al. analyzed self-directed learning by video in a randomized controlled trial with 27 surgical eligible residents [28]. The residents performed an intestinal anastomosis on a cadaveric pig bowel. The group for self-directed learning was given an instructional video of the same procedure performed by an expert. Three weeks later, a second intestinal anastomosis was performed by the two groups, and the procedure was assessed using the OSATS scale. After the second procedure, all participants were provided with the expert video and completed a survey. Both groups improved their results, with the intervention group receiving higher scores, but a statistically significant difference could not be detected.
Netter et al. compared the utility of self-guided learning by video-based self-assessment (SA) in laparoscopic hysterectomy simulator settings [29]. Twenty-four gynecology residents were randomized into two groups. Both groups performed a laparoscopic hysterectomy (LH) in a virtual reality simulator. Then, both groups performed three additional laparoscopic hysterectomies in the simulator, with the SA-group rating each LH with both a generic and a procedure-specific rating scale, while the control groups watched a video demonstration of the procedure. The LH videos were blindly reviewed and rated by experts with OSATS scores. The SA group scored higher in the OSATS scores, with 17 (15–21) vs. 15 (11–17), p = 0.039.
Halim et al. assessed the effect of verbal feedback, video feedback and self-assessment on laparoscopic intracorporeal suturing skills in a prospective randomized blinded trial of 51 novices [30]. Participants were allocated into three groups (verbal feedback, video review with expert feedback and video review with self-assessment) with performance improvements in all groups. Video feedback had the best improvement in global OSATS ratings from baseline to post-feedback, p = 0.004, but the difference between the other interventions was statistically insignificant.
Seifert et al. compared the effect of different feedback modalities in a randomized prospective blinded and controlled study for procedural skills in dental students [31]. Sixty participants were randomly divided into three groups of twenty students. All groups watched an instructional video for an interdental ligature and peripheral venous catheterization. The students were then filmed performing the tasks alone, followed by feedback through either a direct expert, individualized video, or unsupervised video. The same tasks were performed after feedback interventions, and six weeks later the students participated in an objective structured clinical examination. Each feedback improved performance, p < 0.001, but no significant differences were observed between the three groups.
Yu et al. analyzed video modeling and video feedback in teaching procedural skills [32]. Twenty-five medical students were randomly allocated into two groups in a one-way blinded embedded mixed-methods study for intravenous cannulation. They were first instructed on cannulation, after which they performed cannulation on each other while being recorded. Then, the groups were either assigned to review an expert video or a video of their own performance and the expert video. The steps were repeated three times for a total of four cannulations. The time to completion was recorded. The video feedback group outperformed the direct modeling group at 126 s (93–226) vs. 345 s (131–537), with a median difference of 111 s, 95% CI 8–391, p = 0.02. The success rate was similar for groups.
Boecker et al. evaluated video-assisted peer feedback (VAPF) in a randomized controlled noninferiority trial with 251 medical students [33]. The participants were randomly allocated into two groups. In the VAPF group, participants video-recorded peers while performing a wound dressing and provided feedback through a standardized checklist; in the qualified instructor feedback group, participants received feedback from a qualified instructor. Outcome measures were the scores in an objective structured practical examination and a written exam. Noninferiority was confirmed for both outcomes.
Norris et al. prospectively evaluated the utility of educational videos in gynecology students in a randomized controlled trial [34]. Twenty-four residents were randomized to either an educational video group or a traditional residency training group. All participants completed a demographic survey and a knowledge exam prior to laparoscopic salpingo-oophorectomy (LSO). Video recordings of the surgical performance were assessed with OSATS scores and LSO-specific tools. The primary outcome measure was the difference in OSATS scores. The use of LSO videos improved knowledge and confidence, but no differences in OSATS scores were detected.
3.1.1. Methodological Quality Assessment
When utilizing the Jadad quality assessment scale, it was noted that the randomization process was not optimal in 3/7 studies (Table 2). Additionally, all included studies had performed single-blinding only. However, the information about withdrawals/dropouts (if any) was satisfactorily reported in the included trials.

Table 2.
Quality assessment of the included studies using the Jadad scale.
3.1.2. Outcome Measures
The primary outcome measures were to clarify whether (i) SR-VBL contributed to acquiring surgical skills among participants at different stages of their surgical education and (ii) whether SR-VBL could be applied across multiple surgical disciplines. In four studies, SR-VBL was applied to medical students/novices [28,29,30,31]. In all of them, self-regulated VBL proved beneficial in learning technical skills. Furthermore, noninferiority was confirmed in three studies [25,29,30], while in one study, SR-VBL proved best for improving global ratings [30]. In three studies, the effect of SR-VBL was evaluated with residents [25,26,32]. In these, noninferiority was confirmed in two studies [31,32], while one showed improved OSATS scores by SR-VBL [29]. The included studies applied SR-VBL across multiple surgical disciplines.
3.1.3. Meta-Analysis
The secondary outcome measure was to assess the quantitative effect of SR-VBL on learning surgical skills. We identified three studies eligible for meta-analysis analysis [28,29,30]. The studies of Netter et al., Chartrand et al., and Halim et al. all assessed SR-VBL with eligible control groups pre- and post-intervention with OSATS [28,29,30]. Pooling the data (Figure 2) showed a significant difference between the intervention and the control groups in terms of the OSATS scores (WMD: 3.02, 95% CI 0.82 to 5.23, p = 0.007). For this outcome, the estimated heterogeneity among the included studies was statistically insignificant (I2 = 53%, p = 0.12).
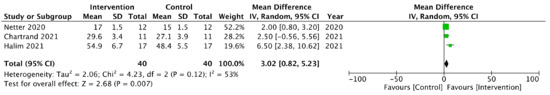
Figure 2.
Forest plot comparison between the intervention (SR-VBL) and control groups in terms of OSATS improvement.
4. Discussion
The results of this systematic review and meta-analysis demonstrate that self-regulated video-based learning (SR-VBL) contributes to the acquisition of technical skills and can therefore be beneficial for training surgeons. Our findings suggest that SR-VBL can be applied to learners at all levels, from medical students to residents, and across different surgical specialties. The meta-analysis indicated that improvements in validated outcome assessment scores (OSATS) favored SR-VBL, and while the effect size was modest, it was statistically significant.
With the COVID-19 pandemic causing widespread disruptions and lockdowns, traditional methods of in-person learning and education were severely impacted. As a result, many educational institutions and industries, including surgical education, turned to digital learning as a viable alternative to traditional in-person teaching [1,2,3,4]. The shift towards remote learning due to the pandemic played a significant role in the increasing popularity of VBL in surgical education, as it allowed for continued education and training while adhering to social distancing guidelines. This trend is likely to continue, even as the pandemic has subsided, given the numerous advantages it offers, such as cost-effectiveness, flexibility, and improved proficiency in many fields [2,3,4,5,8,9,10].
The results of this study are consistent with prior research showing that video-based learning (VBL) can in general improve the technical skills of medical students and surgical residents [17,18]. However, our findings complement these studies by demonstrating the potential benefits of SR-VBL without the need for additional coaching. Augestad et al. showed that VBL can improve technical skills, while Daniel et al. found that teacher-guided VBL for surgical residents can also enhance surgical skills [17,18]. Our study further suggests that SR-VBL may benefit all levels of surgical learners, without requiring additional guidance. SR-VBL encourages students to take responsibility for their learning, set goals, engage in task analysis, use various strategies, reflect on their progress, and seek additional resources as needed, all central processes for successful surgical careers.
Surgical procedures that utilize optical systems for enhanced visualization are particularly well-suited for SR-VBL and further modern analysis tools [35]. With the growing popularity of minimally invasive surgery, the use of SR-VBL has become even more important. To ensure that surgeons are able to benefit from SR-VBL, recording capabilities should be incorporated into surgical systems automatically. This would enable surgeons to engage in post-operative reflection, identifying areas for improvement and further enhancing their surgical skills. By integrating SR-VBL in surgical training, learners of all levels who are eligible to analyze recordings can benefit from a database of recorded operations.
Despite the educational benefits of VBL, its widespread implementation in surgical curriculums has yet to catch up. Few residents have reported using video, despite widespread interest and technical resources [17]. While teacher-guided VBL can be applied in preoperative, intraoperative, and postoperative settings, barriers to implementation remain [17,18]. These include limited resources for both students and teachers, challenges in capturing high-quality video during open surgery, and legal and ethical considerations, particularly regarding data regulation and protection in live surgery. In contrast, SR-VBL can be adopted quickly and effectively without heavy resource investment, as most trainees, surgical residents, and surgeons have access to a telecommunication device equipped with a camera capable of recording video. Nonetheless, caution must be applied, as independent VBL can only serve as a supplement to regular teaching, never a surrogate. Although the effect size of SR-VBL in the meta-analysis was modest, it was still superior to traditional methods, suggesting that better teaching effects can be achieved with less resource investment.
While the studies included in our review focused on the acquisition of technical skills through SR-VBL, prior research has shown that reflecting on learning can improve not only technical skills but also non-technical skills, such as communication and confidence [14,21,22]. Self-reflection is critical to maintaining competence consciousness and engaging in continuous professional development, and SR-VBL can be a valuable tool for cultivating both technical and non-technical surgical learning skills. Video-based learning allows learners to identify areas for improvement and maintain an awareness of competence stages within the surgical learning curricula. It also enables the identification of non-technical skills, providing opportunities for their development. Videos can be used as a resource for peer learning, enabling surgeons of all levels to analyze each other’s videos from various perspectives and learn from them.
Our study has several limitations. First, there was variable reporting of outcomes in the included studies, and a validated outcome assessment tool was used pre- and post-intervention in only a subset of the studies. Second, the mode of VBL varied between studies, and third, incomplete reporting by the included studies limited our ability to synthesize high-quality evidence. Fourth, terms for VBL are used inconsistently in the medical literature, causing confusion. The terms ‘video-feedback’ and ‘video-coaching’ have been misused in previous studies. By failing to accurately distinguish between the methods, researchers may be unable to identify the specific components that contribute to their effectiveness, which in turn may limit the generalizability of their findings. We promote the correct use of the term SR-VBL in future studies. Finally, although all studies were randomized and controlled, the randomization was not optimal, and the blinding in the studies was simple, leaving room for improvement. In addition, the study population was heterogeneous and limited, thereby introducing confounding factors into the analysis. Nonetheless, the withdrawals/dropouts were satisfactorily reported, and our study provides useful insights into the potential benefits of SR-VBL for surgical learning.
5. Conclusions
Surgical training is becoming more collaborative and interdisciplinary, emphasizing communication skills within the team and between different medical specialties. This reflects contemporary surgical care, where surgeons work within a team with a common aim of comprehensive patient care. Surgeons are no longer pure technical masters but must also be proficient in non-technical skills in order to excel, such as leadership, decision-making, and communication. SR-VBL contributes to surgical learning with objective improvements in validated outcome scores. While this study focused on self-regulated VBL for technical aspects of surgical learning, VBL can be applied to all components of surgical competence. In light of current findings, the inclusion of SR-VBL into surgical training curricula should be considered, given the minimal resource demands and the included benefits. SR-VBL strengthens the positive effects of self-assessment, self-reflection, and self-regulated learning, all of which help trainees to become better surgeons.
Author Contributions
Conceptualization, N.P.; methodology, N.P.; software, S.A.; validation, N.P., S.A. and H.A.; formal analysis, N.P.; investigation, N.P.; resources, S.A.; data curation, S.A.; writing—original draft preparation, N.P.; writing—review and editing, N.P., S.A., H.A. and K.P.; visualization, N.P.; supervision, K.P.; project administration, K.P. All authors have read and agreed to the published version of the manuscript.
Funding
N.P. received funding for this project from Jarl Walter, Karl Walter och Dorothea Olivia Perkléns minnesfond.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Study data is available from authors on reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Sablić, M.; Mirosavljević, A.; Skugor, A. Video-Based Learning (VBL)-Past, Present and Future: An Overview of the Research Published from 2008 to 2019. Technol. Knowl. Learn. 2021, 26, 1061–1077. [Google Scholar] [CrossRef]
- Youssef, S.C.; Aydin, A.; Canning, A.; Khan, N.; Ahmed, K.; Dasgupta, P. Learning Surgical Skills Through Video-Based Education: A Systematic Review. Surg. Innov. 2022, 30, 220–238. [Google Scholar] [CrossRef] [PubMed]
- Williams, T.P.; Klimberg, V.; Perez, A. Tele-education assisted mentorship in surgery (TEAMS). J. Surg. Oncol. 2021, 124, 250–254. [Google Scholar] [CrossRef]
- Tuong, M.N.E.; Winkelman, A.J.; Yang, J.H. Evaluation of the Educational Impact of the Urology Collaborative Online Video Didactics Lecture Series. Urology 2022, 167, 36–42. [Google Scholar] [CrossRef] [PubMed]
- Ahmet, A.; Gamze, K.; Rustem, M.; Sezen, K.A. Is Video-Based Education an Effective Method in Surgical Education? A Systematic Review. J. Surg. Educ. 2018, 75, 1150–1158. [Google Scholar] [CrossRef] [PubMed]
- Reznick, R.K.; MacRae, H. Teaching surgical skills—Changes in the wind. N. Engl. J. Med. 2006, 355, 2664–2669. [Google Scholar] [CrossRef]
- Fecso, A.B.; Szasz, P.; Kerezov, G.; Grantcharov, T.P. The Effect of Technical Performance on Patient Outcomes in Surgery: A Systematic Review. Ann. Surg. 2017, 265, 492–501. [Google Scholar] [CrossRef]
- Raja, B.S.; Choudhury, A.K.; Paul, S.; Rajkumar, S.; Kalia, R.B. Online educational resources for orthopaedic residency—A narrative review. Int. Orthop. 2021, 45, 1911–1922. [Google Scholar] [CrossRef]
- Mao, B.P.; Teichroeb, M.L.; Lee, T.; Wong, G.; Pang, T.; Pleass, H. Is Online Video-Based Education an Effective Method to Teach Basic Surgical Skills to Students and Surgical Trainees? A Systematic Review and Meta-analysis. J. Surg. Educ. 2022, 79, 1536–1545. [Google Scholar] [CrossRef]
- Fehervari, M.; Das, B.; Soleimani-Nouri, P.; Ahmad, M.; Fadel, M.G.; Deputy, M.; Morgan, C.; Burke, J.R.; Mason, J.D.; Nott, D.; et al. Can surgical skills be taught using technological advances online? A comparative study of online and face-to-face surgical skills training. Surg. Endosc. 2022, 36, 4631–4637. [Google Scholar] [CrossRef]
- Kyaw, B.M.; Posadzki, P.; Paddock, S.; Car, J.; Campbell, J.; Tudor Car, L. Effectiveness of Digital Education on Communication Skills Among Medical Students: Systematic Review and Meta-Analysis by the Digital Health Education Collaboration. J. Med. Internet Res. 2019, 21, e12967. [Google Scholar] [CrossRef] [PubMed]
- Gilligan, C.; Powell, M.; Lynagh, M.C.; Ward, B.M.; Lonsdale, C.; Harvey, P.; James, E.L.; Rich, D.; Dewi, S.P.; Nepal, S.; et al. Interventions for improving medical students’ interpersonal communication in medical consultations. Cochrane Database Syst. Rev. 2021, 2, CD012418. [Google Scholar] [CrossRef] [PubMed]
- Coppola, V.; Autorino, G.; Cerulo, M.; Conte, F.D.; Ricci, E.; Borgogni, R.; Cardone, R.; Escolino, M.; Esposito, C. Video-Based Coaching: An Efficient Learning and Teaching Modality for Pediatric Surgery and Pediatric Urology Training Program. J. Laparoendosc. Adv. Surg. Tech. A 2021, 31, 594–597. [Google Scholar] [CrossRef]
- Soucisse, M.L.; Boulva, K.; Sideris, L.; Drolet, P.; Morin, M.; Dube, P. Video Coaching as an Efficient Teaching Method for Surgical Residents—A Randomized Controlled Trial. J. Surg. Educ. 2017, 74, 365–371. [Google Scholar] [CrossRef] [PubMed]
- Edisherashvili, N.; Saks, K.; Pedaste, M.; Leijen, Ä. Supporting Self-Regulated Learning in Distance Learning Contexts at Higher Education Level: Systematic Literature Review. Front. Psychol. 2022, 12, 79242. [Google Scholar] [CrossRef] [PubMed]
- Dindar, M.; Malmberg, J.; Järvelä, S.; Haataja, E.; Kirschner, P. Matching self-reports with electrodermal activity data: Investigating temporal changes in self-regulated learning. Educ. Inf. Technol. 2020, 25, 1785–1802. [Google Scholar] [CrossRef]
- Augestad, K.M.; Butt, K.; Ignjatovic, D.; Keller, D.S.; Kiran, R. Video-based coaching in surgical education: A systematic review and meta-analysis. Surg. Endosc. 2020, 34, 521–535. [Google Scholar] [CrossRef]
- Daniel, R.; McKechnie, T.; Kruse, C.C.; Levin, M.; Lee, Y.; Doumoras, A.G.; Hong, D.; Eskicioglu, C. Video-based coaching for surgical residents: A systematic review and meta-analysis. Surg. Endosc. 2022, 4, 100298. [Google Scholar] [CrossRef]
- Esposito, A.C.; Coppersmith, N.A.; White, E.M.; Yoo, P.S. Video Coaching in Surgical Education: Utility, Opportunities, and Barriers to Implementation. J. Surg. Educ. 2022, 79, 717–724. [Google Scholar] [CrossRef]
- van Es, E.; Tunney, J.; Goldsmith, L.; Seago, N. A framework for the facilitation of teachers’ analysis of video. J. Teach. Educ. 2014, 65, 340–356. [Google Scholar] [CrossRef]
- Piskin, E.; Colakoglu, M.K.; Bal, A.; Oter, V.; Bostanci, E.B. Evaluation of the Quality, Educational Value and Utility of the Videos on YouTube for Laparoscopic Low Anterior Resection. Am. Surg. 2022, 88, 2380–2387. [Google Scholar] [CrossRef] [PubMed]
- Nayar, S.K.; Musto, L.; Baruah, G.; Fernandes, R.; Bharathan, R. Self-Assessment of Surgical Skills: A Systematic Review. J. Surg. Educ. 2020, 77, 348–361. [Google Scholar] [CrossRef] [PubMed]
- Trickey, A.W.; Newcomb, A.B.; Porrey, M.; Piscitani, F.; Wright, J.; Graling, P.; Dort, J. Two-Year Experience Implementing a Curriculum to Improve Residents’ Patient-Centered Communication Skills. J. Surg. Educ. 2017, 74, e124–e132. [Google Scholar] [CrossRef]
- Naik, N.D.; Abbott, E.F.; Gas, B.L.; Murphy, B.L.; Farley, D.R.; Cook, D.A. Personalized video feedback improves suturing skills of incoming general surgery trainees. Surgery 2018, 163, 921–926. [Google Scholar] [CrossRef] [PubMed]
- Ranney, S.E.; Bedrin, N.G.; Roberts, N.K.; Hebert, J.C.; Forgione, P.M.; Nicholas, C.F. Maximizing Learning in the Operating Room: Residents’ Perspectives. J. Surg. Res. 2021, 263, 5–13. [Google Scholar] [CrossRef] [PubMed]
- Reznick, R.; Regehr, G.; MacRae, H.; Martin, J.; McCulloch, W. Testing technical skill via an innovative “bench station” examination. Am. J. Surg. 1997, 173, 226–230. [Google Scholar] [CrossRef]
- Jadad, A.R.; Moore, R.A.; Carroll, D.; Jenkinson, D.; Reynolds, D.J.; Gavaghan, D.J.; McQuay, H.J. Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Control. Clin. Trials 1996, 17, 1–12. [Google Scholar] [CrossRef]
- Chartrand, G.; Soucisse, M.; Dube, P.; Trepanier, J.S.; Drolet, P.; Sideris, L. Self-directed learning by video as a means to improve technical skills in surgery residents: A randomized controlled trial. BMC Med. Educ. 2021, 21, 91. [Google Scholar] [CrossRef]
- Netter, A.; Schmitt, A.; Agostini, A.; Crochet, P. Video-based self-assessment enhances laparoscopic skills on a virtual reality simulator: A randomized controlled trial. Surg. Endosc. 2021, 35, 6679–6686. [Google Scholar] [CrossRef]
- Halim, J.; Jelley, J.; Zhang, N.; Ornstein, M.; Patel, B. The effect of verbal feedback, video feedback, and self-assessment on laparoscopic intracorporeal suturing skills in novices: A randomized trial. Surg. Endosc. 2021, 35, 3787–3795. [Google Scholar] [CrossRef]
- Seifert, L.B.; Herrera-Vizcaino, C.; Herguth, P.; Sterz, J.; Sader, R. Comparison of different feedback modalities for the training of procedural skills in Oral and maxillofacial surgery: A blinded, randomized and controlled study. BMC Med. Educ. 2020, 20, 330. [Google Scholar] [CrossRef]
- Yu, J.; Lo, C.; Madampage, C.; Bajwa, J.; O’Brien, J.; Olszynski, P.; Lucy, M. Video Modeling and Video Feedback to Reduce Time to Perform Intravenous Cannulation in Medical Students: A Randomized-Controlled Mixed-Methods Study. Can. J. Anaesth. 2020, 67, 715–725. [Google Scholar] [CrossRef] [PubMed]
- Boecker, A.H.; Bank, C.; Kim, B.S.; Aman, M.; Pears, K.H.; Klasen, M.; Lambert, S.; Sopka, S. Video-Assisted Peer Teaching for Surgical Skills Training-Innovative Potential for the Medical Curriculum and Beyond: A Randomized Controlled Trial. J. Surg. Educ. 2022, 79, 441–451. [Google Scholar] [CrossRef] [PubMed]
- Norris, S.; Papillon-Smith, J.; Gagnon, L.H.; Jacobson, M.; Sobel, M.; Shore, E.M. Effect of a Surgical Teaching Video on Resident Performance of a Laparoscopic Salpingo-oophorectomy: A Randomized Controlled Trial. J. Minim. Invasive Gynecol. 2020, 27, 1545–1551. [Google Scholar] [CrossRef] [PubMed]
- Chang, T.; Seufert, C.; Eminaga, O.; Shkolyar, E.; Hu, J.; Liao, J. Current trends in artificial intelligence application for endourology and robotic surgery. Urol. Clin. N. Am. 2021, 48, 151–160. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).