Abstract
Medical educators face many challenges instructing future medical students, specifically in the integration of learning technologies. To overcome these challenges, educators must implement learner-centered and interactive teaching strategies. Anatomical sciences are the cornerstone of medical education and provide the bedrock to layer conceptual understanding of the human body. With the “medical knowledge boom”, most medical schools have reduced the curricular time for anatomy instruction, resulting in a paucity of knowledge and issues incorporating anatomical knowledge in clinical scenarios. Modern pedagogical techniques combining AI chatbots with concurrent metacognitive frameworks can foster a deeper understanding of anatomical knowledge and analysis of clinical cases. Student reflection on the learning process allows for monitoring their progress and tailoring of learning strategies to their specific capabilities and needs. A.I. technology can aid in scaffolding knowledge with practical applications via iterative and immediate feedback in case- or problem-based learning formats. The use of textual conversations actively engages students and simulates conversations with instructors. In this communication, we advocate for the incorporation of AI technologies fused with a metacognitive framework as a medium to foster increased critical thinking and skill development that enhances comprehension. These skills are important for medical students’ lifelong learning process.
1. Introduction
Gross anatomy forms the cornerstone of medical education. However, there is widespread agreement among current instructors of anatomy that the number of actual hours spent teaching this fundamental science in overcrowded undergraduate curricula has been steadily declining. It is believed that the long-term effects of this lack of ideal anatomical knowledge will have an impact on patient safety [1]. An increase in some sorts of medico-legal cases has been attributed to an inadequate application of anatomy knowledge. This might be caused in part by the quick adoption of contemporary learning strategies of rote learning without an adequate introduction to clinical reasoning skills, the dearth of gross anatomy instructors, and the absence of well-organized teaching and learning methods to develop skills to become life-long learners [2]. Patient diagnosis often relies on anatomical and functional understanding is often the primary determinant of treatment and subsequently outcome [3]. This lack of understanding can result in misdiagnosis which puts patients at risk and directly leads to measurable harm [4]. The challenges faced by modern medical educators in relation to curriculum integration are a decreased instructor-to-student ratio, decreased face-to-face interaction, numerous ballooning topics to be covered, and the inclusion of novel technologies suitable for the Gen Z population [5]. Educational experiences that are active, contextual, integrated, technologically sound, and student-oriented lead to deeper learning. For the past two decades, medical educationists are restructuring their curricula as per modern learning theories that include components of constructive, collaborative, contextual, and self-directed learning practices [6]. Imparting this pedagogy requires the ingenious creativity of teachers and collaborative efforts from learners in creating and organizing educational content in a logical sequence. Therefore, medical educators need to look for the most sound and best practices to become self-regulated, safe, and effective doctors and retain these practices for lifelong learning [7,8,9]. In this short communication, we advocate for the development of the core concepts such that the essential knowledge is conferred appropriately to Gen Z students using modern technology-supplemented instruction. In medical education, active learning strategies such as problem-based learning (PBL) or case-based learning (CBL) aim to equip independent learners for ongoing, self-directed development through metacognitive awareness outside of the classroom. Case-based learning exposes students to real-world, complex clinical situations that call for the use of anatomical knowledge to resolve issues [10]. Much research has focused on these overlapping yet distinct instructional pedagogies, each having associated benefits and drawbacks. A thorough discussion of these methods is beyond the scope of this paper, but articles focused on their composition, utility, comparisons, and success rates abound [11,12,13,14]. Although some students perceive medical education to be an “exercise in memorizing facts” [9], successful instruction requires conceptual understanding. The concept of metacognition in medical instruction has been assumed to occur or ignored in the curriculum, even though active learning has become a key approach in anatomical instruction [15,16,17].
2. Medical Education and the Gen Z Student Population
Medical education has a necessary amount of complexity that challenges students [8] and because we cannot adjust the difficulty, we must focus on other avenues to inform and retain students [18]. This type of instruction requires appropriate pedagogical methods adherent to evidence-based practices that consider who is being taught. The present generation of students (Gen Z) as well as future students have distinctive traits and interests which influence their learning and educational experiences [19]. These students are digitally savvy and are accustomed to using technology in daily life because they were raised in a digital environment. They are skilled at using social media platforms, mobile apps, and online resources. Incorporating visual resources into anatomy learning can help engage and enhance their understanding. Compared to prior generations, Gen Z students frequently have shorter attention spans. They can better recall and understand the material if it is broken down into smaller, more manageable portions. Students in the Gen Z generation value flexibility and accessibility in their learning resources. Learning experiences that are individualized and gamified are favorably received by Gen Z students. Learners of Generation Z tend to be inquisitive and value facts-based information and instant feedback [20].
3. Incorporation of Digital Technology into Medical Education
The past two decades have seen tremendous growth in the incorporation of digital technology in anatomy learning strategies. COVID-19 has accelerated the development of digital technology where online and blended learning has become the norm of teaching on a wider scale in most medical schools across the world [21]. There is a wide range of digital technology to choose from which includes augmented reality, virtual reality, 3D modeling of the human body, 3D printed models, virtual human dissectors etc. All these technologies have been effectively implemented in medical education and are effective in providing alternate experiences to understand the human body’s complexity and understanding the relations of the internal structures. Even though these have been used effectively during early instruction, drug guides and medical calculators tend to be the most used medical technologies [22]. The impact of anatomical visualization using digital technology and learning effectiveness have controversial reports in the literature [23,24]. Although these technologies have been developed and utilized in recent years, they have lacked interaction and focus on cognitive strategies. Application of the knowledge gained through these digital aids to real-life situations needs to be aligned to help critical thinking and problem-solving skills. We postulate that this can be well conducted using an artificial intelligence chatbot (AI chatbot) integrated within a metacognitive framework focused on clinical situations.
4. Artificial Intelligence and Metacognition
4.1. Artifical Intellengence
Authentic cases delivered through an AI chatbot promote active learning by putting students in control of their own education. Learners investigate pertinent anatomical concepts, actively seek out information, and work together on their own or with peers to solve issues. While analyzing many viewpoints, assessing the evidence, and coming to well-informed judgments, this active engagement encourages critical thinking. The integration of different perspectives pushes students to consider how anatomical concepts connect to various facets of patient care. They have to think about how diseases, physiological changes, and anatomical variances may affect clinical manifestations and available treatments. This platform encourages learners to reflect on their learning process, assess their understanding, and identify areas for improvement. This reflective practice engages metacognition and thus promotes critical thinking as learners evaluate the effectiveness of their approach, consider alternative perspectives, and adjust their strategies accordingly [25]. This reflection for metacognitive purposes is best before, during, and after situations to develop the student’s understanding of their learning process [23,26] and can aid in debiasing [15]. Given that this system would be independent, students, residents, or practicing physicians can practice at any time (asynchronously), without harming patients if incorrect, and with some of the benefits of synchronous human tutoring [3,27,28].
4.2. Metacognition in Medical Education
Famed American theoretical astrophysicist Richard Feynman once discussed the difference between, “…knowing the name of something and knowing something.” which is an eloquent lead into the concept of metacognition. Very generally, metacognition can be colloquially conceptualized by the phrase “thinking about thinking” but can be understood more scientifically by “a range of executive system processes that are intimately involved in self-assessment, cognitive control, and monitoring” [15]. This more complete definition allows for a more expansive capacity that importantly includes recognition of the absence of knowledge in particular areas. This can be broken down into two main components such as knowledge of- and regulation/experiences of cognition [29,30,31]. Some have even speculated that awareness and access to specific knowledge may be arguably as important as the knowledge itself [4]. Research that supports this demonstrate a moderate correlation between change in regulation of (but not knowledge of) metacognition over the first year of medical school and academic results [7]. An analogy for this would be that you could have a million dollars in the bank (knowledge) but if you don’t know how it was earned, or how to get it out of the bank (regulation of metacognition), it is effectively useless.
The capacity to “know what you know and what you don’t know” is imperative for the process of learning and is paramount for current medical students during their education and beyond. Most students lack this ability and may outsource this from themselves to external assessment tools that provide “hard outcome measures” like assignments, e-learning activities, or exams [9]. It is not uncommon for medical instructors to be surprised by students’ negative reactions to poor performances on assessments [30] with their students bringing a color-coded textbook to demonstrate the hours they spent studying [32]. This behavior indicates that the issue may not be a lack of motivation [33] or time but one of a lack of metacognitive awareness [16]. This is summarized well as “...competence is required to identify areas of incompetency” [34]. Previous investigations have found that medical students struggle with learning as well as understanding complex content that they are responsible to learn [8,35]. Beyond this, students often struggle to transfer the knowledge from basic sciences and even simulations to the real world [31,36,37].
Even the most educated individuals are not immune to what has been coined the Dunning–Kruger effect [22,30,34], which states that people who know the least are more confident in their ability. This overconfidence may lead to a premature conclusion of a diagnosis prior to consideration of all components, negatively impacting patient outcomes [3]. One investigation found that 98 and 95 percent of first year medical students overestimated their performance in a patient encounter history and physical exam, respectively [38], and other studies have found that physicians may be unskilled in global self-assessment [39]. Training may improve this capability through simulation and exploratory experiences that encourage reflection [36]. This has implications for residency and beyond with more competent but junior physicians rating their own efficacy lower than less competent but more senior physicians; with this being more pronounced in female professionals [34,40,41]. In fact, researchers have shown that the majority of university-level learners have an inaccurate conception of how learning occurs leading to the use of poor or ineffectual strategies that result in non-durable learning that has been called the “illusion of knowing or competency” [22,30,32]. Training that includes metacognition as opposed to traditional lecture-based instruction has recently seen increased research related to medical education [3,8,15,25,26,27,31,32,35,42,43,44,45].
As current students progress through their careers, they will continue to experience many changes in their knowledge, evaluations/tests, and treatments. Most of these approaches include student-directed learning to reflect the need for autonomy and competence in the form of flipped classrooms, team-based learning, or other pedagogical methodologies [25,46]. These strategies have been found to improve learning compared to traditional lecture methods, especially in stressful environments like that of medical education, but early in the education process students may find it difficult to adopt them due to the lack of familiarity [47,48]. This lack of familiarity may not allow for larger bits of information to be “chunked” into smaller pieces placing a higher cognitive burden on the regulation of working memory and critical thinking [35]. While critical thinking ability has been shown to correlate with initial scores on medical education evaluations, it is self-regulation and metacognition that showed an ability to manage the cognitive load [35]. This also correlates with learning growth which is important for students’ success in an expanding and integrative curriculum [29,49]. Some even speculate that metacognitive strategies can mediate emotions, self-efficacy, and self-regulation and that these then influence academic performance [43,46].
While there is some discussion in the literature about which strategy is appropriate for particular subjects within medical education, all seem to have an undercurrent of metacognitive strategies [27,31,48]. Metacognitive skills that manage the learning process are not natural, inherited, or stationary but can be influenced through instruction [50]. The method of this instruction can be through classroom activities, online resources, mobile apps, virtual bodies, VR simulations, quizlets, etc. These teaching strategies have shown improvements above traditional lecture-based methods likely due to the student being an active as opposed to a passive participant in the learning process. This active vs passive interaction with the material likely engages metacognitive processes that better aid learning progression. While the learning methods focused on student-directed learning have been shown to be greatly beneficial, they can be time-consuming for both the instructor and the student. This increase in time allocation is problematic given the current and growing topics needing to be covered in medical education as well as the shrinking teacher to student ratio. Additionally, the use of these strategies may overly rely or focus on high performers and or those that feel comfortable talking in front of others [36]. Ironically, the students who may need the most assistance may be relying on others during these activities to the detriment of their comprehension and progression in the program. Thus, these pedagogical techniques engage students and aid in learning but may do so in an unbalanced manner for students and take an inordinate amount of allocated time to complete.
Given the benefits of these techniques likely due to engagement with metacognitive processes, a more explicit training that incorporates components of metacognition into its design is imperative [42]. Additionally, this should also be able to surmount the issues of uneven distribution of effect, in and out of classroom time commitment, as well as make use of emerging technologies such as Artificial Intelligence (AI). The use of AI in instruction is a current focus within education generally as well as medical education specifically. Within this focus, we advocate for an AI chatbot specifically engineered to incorporate metacognitive principles and scaffolding (i.e., individual pacing) for medical education integrating multiple domains (anatomy, physiology, disease presentation, testing, treatment, etc.…) to aid comprehension [36]. This scaffolding allows for the emphasis of specific knowledge and encourages the reflection and deeper learning that is necessary for cognitively complex problems like that of medical education [45]. The training of medical students may teach domains of knowledge as “a la carte” entrees in discrete silos but it is the interaction and integration of these that defines medical practice [25]. The use of the chatbot will allow for components explicitly necessary to train this new generation, particularly immediate feedback in an iterative and interactive technology format that they are familiar with (see Figure 1 and Figure 2 below). The iterative nature of this technology is of great benefit since the learning, especially self-regulated, is cyclical (see Figure 2 below) and can be scaffolded based upon prior knowledge and performance with students fixing their misconceptions rather than just “moving on to the next exam” [31,32]. This can enable the chatbot to fade or increase assistance allowing for a gradation of knowledge acquisition and focusing the learner on knowledge yet to be satisfactorily acquired [27,37]. The “testing” type format, as opposed to “restudying” that the chatbot would use is generative (short answer) as opposed to recognition (multiple choice) and is better for long-term memory retention.
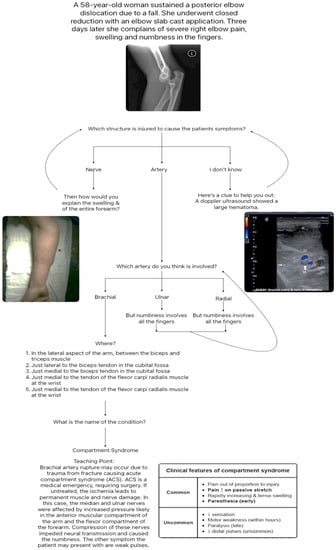
Figure 1.
This figure demonstrates a single example of a diagnostic decision tree. In this particular example students will start with partial knowledge and as they provide answers and speculations will obtain more information or hints in the form of questions to further guide them to the correct answer. In this particular case the final diagnosis is compartment syndrome. Embedded images retrieved from PM Robinson, E Griffiths and AC Watts [51] for the x-ray image, I Gedi Ibrahim and M Tahtabasi [52] for the doppler ultrasound image, and D Suvashis, M Rahul and P Lukesh [53] for the arm image.
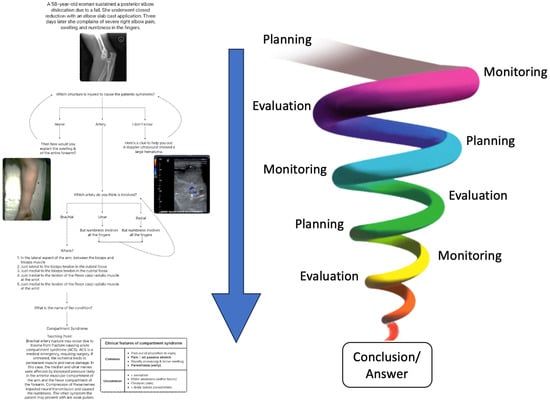
Figure 2.
This figure demonstrates the manner in which principles of metacognition including planning, monitoring, and evaluation in a cyclical fashion provide a theoretical framework to guide students through the diagnostic process. This will be both explicit and implicit within the framework of the AI chatbot application.
The combination of testing and feedback has been shown to improve learning [45] and even quadrupled retention when compared to no testing [22,54]. An added benefit is that this interaction also more closely resembles the real-world clinical environment which solidifies knowledge especially when meant to perform or assess in a similar context [26]. In addition, students will not get distracted by “lures” that are not “the best choice” which may unfortunately be incorporated into the student’s knowledge and persevere even despite correction. Misconceptions are different from a lack of knowledge in that they tend to be stronger and less easily changed [17]. Operationally, incorrect answers that have a high degree of confidence are considered misconceptions, and those with low confidence as lack of knowledge. A lack of knowledge improves over the course of instruction; however, misconceptions can persist even after traditional instruction [17]. The use of metacognition combats these perseverative misconceptions by de-biasing the individual through detaching the student a bit from the clinical decision and focusing on how they are thinking [47]. The nature of the way in which people will interact with this chatbot will be very similar and relevant to the way that information is acquired in the clinical setting. Not all information about each patient is always readily available and decisions for which assessment or test should be conducted typically rely on a set of partial or incomplete information. This parity between the training and clinical situations will allow students to bridge the gap and better adjust to the demanding clinical rotation environment [9,45].
4.3. AI Case Example Using Metacognition
In the supplied example (see Figure 1 above), a background stating that a patient presented with a broken arm is experiencing swelling and numbness in her fingers. Then a prompt asking for a differential diagnosis including all possible causes for this symptom. Out of the possible diagnoses speculated by the student, they will be asked to choose the most likely cause. Again, immediate feedback is given to the student in the form of questions that are intended to guide them to the appropriate answer. Without feedback incorrect answers with either low or high confidence from the student are almost never corrected within memory [22]. Following this, students would be asked to then indicate what type of test they would perform given the likelihood of the enumerated diagnoses. Incorrect or less correct answers could be noted immediately allowing for very quick adjustment in the choice of assessment leading to better gains in learning [3]. Correction of errors early in the process of assessment is a critical factor for learning and prevents students from spending time, energy, and cognitive effort continuing down incorrect diagnostic avenues. Following the eventual correct choice of assessment, clinically relevant information that was acquired from that test would be supplied and this would proceed in this fashion until finalization of diagnosis. A similar pattern of iterative questioning and progression would be used to identify a likely course of treatment.
In the provided example students would indicate that tingling and numbness is likely caused by nerve damage which is a related and plausible solution but ultimately incorrect. This type of instruction has been successfully used [15,36] to improve medical students’ differential diagnosis by encouraging further discussion or demonstrating a need for more research. Often medical textbooks and traditional instruction may present patient cases in an overly explicit manner lacking the ambiguity of real patient diagnosis [4]. In a case example from a gastroenterology chapter or textbook, it is very unlikely that the diagnosis would be related to anything other than the gut. Training using more ambiguous patient presentation has previously been done by incorporating metacognitive strategies through mnemonics like the TWED method (Threat, What else, Evidence, and Dispositional factors) [47] or a variety of other strategies [4]. While the patient presentation should occur in a iterative and pseudo-ambiguous fashion, the questions themselves should remain clear in their statement and appropriate in format [55]. Following the suggestion of a possible and related but incorrect differential diagnosis, a prompt would ask the student, “How do you explain the swelling” which would lead to re-evaluation from the student eventually stating that this is likely due to arterial damage.
Once the correct underlying reason is identified, then more specifics are then layered beyond that asking for the specific artery that this would be. If the incorrect artery is chosen (ulnar or radial) as an explanation, a prompt would appear that would state, “but the numbness involves all of the fingers.” This should eventually lead them to conclude that the Brachial artery is likely the cause of the swelling. Delving further they are then prompted by the question, “Where is the location of the structure?” Once identified, students will then be asked what the name of the condition was that would cause this cluster of symptoms (Compartment Syndrome). After the correct identification, more information and other teaching points about the condition, as well as the full decision tree (a variation in concept mapping) with the correct pathway, will be highlighted [3,8]. This system will also allow for elaborated, as opposed to partial feedback, which is much more powerful [22], and these hints becoming increasingly specific, is a component of successful instruction in human to human instruction [3]. One of the benefits of this type of interactive instruction is that it uses bottom-up, as opposed to top-down assessment which is more representative of the real-world experience.
The use of this AI system incorporates the theory of dual process cognition that acknowledges that we have a faster, more automatic and a slow more effortful method of processing information. The AI provides smaller and more consistent pieces of information as the case progresses. This is more necessary for the student who is using a slow and more effortful processing system as compared to automatic processing [45,47]. Some speculate that an underlying challenge of medical instruction is that the automatic system is highly developed in the instructor and there are issues when “back translating” it into the slower, segmented, and more effortful system for their students. When these students encounter new clinical cases in their rotations they will be better adapted and more prepared to engage in the automatic processing required by the fast-paced clinical environment. Strikingly, it is actually hoped that through medical education training and practice, students will transition to the fast process, making decisions by automatic pattern recognition.
The scaffolding of knowledge is an important component of the learning process. Like that of riding a bicycle or driving a car, at first you must pay attention to each and every minute aspect of the action. This focus on each individual piece, ironically may make it more difficult to perform the task as a whole. After sufficient practice, people acquire the knowledge and can perform the task but may then be unable to eloquently convey the individual components on which they were once intently focused. The use of the iterative interactive component of a chatbot can help those initially starting the process of learning and will prevent miscommunication from instructors who are immensely competent to the point that they not only do not break necessary points into smaller, more digestible “chunks” but even unintentionally gloss over lesser, albeit still necessary, components. Thus, making each of these components explicit and tangible for students that lack any conception of the structure or organization of the information [55].
As a note of caution however, the use of scaffolding and appropriate testing methods within an AI chatbot should be constructed in a way as to not interfere with the natural flow of learning, which may be a challenge [3,37]. This can be addressed strategically using this tool after students obtain sufficient topographic and systemic anatomy knowledge. The implementation of this strategy may also require training of faculty and staff in its use and student interface. Additionally, we would be remiss not to highlight the idea that these strategies are to be incorporated in addition to the more traditional methodologies of anatomy instruction. The implementation of AI as discussed in this article would never replace strategies such as in person dissection and interaction with the instructor and other students. These traditional experiences help to cultivate skills needed for interpersonal communication and the doctor–patient relationship which are still crucial and foundational to the practice of medicine. As for hands-on skills, learning technologies such as virtual reality, synthetics, simulations, and A.I. have improved leaps and bounds over the last 30 years, they are still an inferior substitution for dissection of a doner body. Maintaining a balance between tried-and-true pedagogical techniques and the inclusion of newer methodologies and evidence-based practices will be of the utmost importance moving into the 21st century and beyond.
5. Conclusions
Gen Z’s consistent exposure to digital technology has changed their learning abilities and preferences. By understanding the unique characteristics and preferences of Gen Z learners (digital natives, flexibility, instant feedback, shorter attention span, multimedia presentation, etc.), medical educators can design anatomy learning experiences that cater to their needs through enhanced engagement, technology-focused instruction, and iterative feedback. As passionate medical professionals and educators, we have observed the challenges faced by medical students when attempting to bridge the gap between theoretical knowledge and practical application. The true potential of AI chatbots lies in the integration of metacognitive frameworks for student success and plays a crucial role in their learning and development. Metacognitive strategies empower students to take greater control of their learning through planning, monitoring, and reflection. This encourages the students to understand their own learning processes and take ownership of their learning outcomes. Incorporating chatbots matches the abilities and preferences of Gen Z, facilitates self-paced learning, identifies misconceptions or roadblocks, aids in evaluation of their learning progress, and allows for necessary adjustments to gain mastery of lifelong learning skills.
Author Contributions
Conceptualization, V.T. and C.J.D.; article search, V.T. and C.J.D.; review, V.T. and C.J.D.; writing, V.T. and C.J.D.; image construction, V.T. and C.J.D.; writing, V.T. and C.J.D.; original draft preparation, review, V.T. and C.J.D.; editing V.T. and C.J.D. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Inuwa, I.M.; Tanranikanti, V.; Al-Rawahy, M.; Roychoudhry, S.; Habbal, O. “Between a Rock and a Hard Place” The discordant views among medical teachers about anatomy content in the undergraduate medical curriculum. Sultan Qaboos Univ. Med. J. 2012, 12, 19–24. [Google Scholar] [CrossRef] [PubMed]
- Porzionato, A.; Macchi, V.; Stecco, C.; Boscolo-Berto, R.; Loukas, M.; Tubbs, R.S.; De Caro, R. Clinical Anatomy and Medical Malpractice-A Narrative Review with Methodological Implications. Healthcare 2022, 10, 1915. [Google Scholar] [CrossRef]
- Feyzi-Behnagh, R.; Azevedo, R.; Legowski, E.; Reitmeyer, K.; Tseytlin, E.; Crowley, R.S. Metacognitive Scaffolds Improve Self-Judgments of Accuracy in a Medical Intelligent Tutoring System. Instr. Sci. 2014, 42, 159–181. [Google Scholar] [CrossRef]
- Leeds, F.S.; Atwa, K.M.; Cook, A.M.; Conway, K.A.; Crawford, T.N. Teaching heuristics and mnemonics to improve generation of differential diagnoses. Med. Educ. Online 2020, 25, 1742967. [Google Scholar] [CrossRef] [PubMed]
- Zheng, B. Medical Students’ Technology Use for Self-Directed Learning: Contributing and Constraining Factors. Med. Sci. Educ. 2022, 32, 149–156. [Google Scholar] [CrossRef]
- Mukhalalati, B.A.; Taylor, A. Adult Learning Theories in Context: A Quick Guide for Healthcare Professional Educators. J. Med. Educ. Curric. Dev. 2019, 6, 2382120519840332. [Google Scholar] [CrossRef]
- Hong, W.H.; Vadivelu, J.; Daniel, E.G.; Sim, J.H. Thinking about thinking: Changes in first-year medical students’ metacognition and its relation to performance. Med. Educ. Online 2015, 20, 27561. [Google Scholar] [CrossRef] [PubMed]
- Khaine, A.A.; Adefuye, A.O.; Busari, J. Utility of Concept Mapping as a Tool to Enhance Metacognitive Teaching and learning of complex concepts in undergraduate medical education. Arch. Med. Health Sci. 2019, 7, 267–272. [Google Scholar]
- Versteeg, M.; Bressers, G.; Wijnen-Meijer, M.; Ommering, B.W.C.; de Beaufort, A.J.; Steendijk, P. What Were You Thinking? Medical Students’ Metacognition and Perceptions of Self-Regulated Learning. Teach. Learn. Med. 2021, 33, 473–482. [Google Scholar] [CrossRef] [PubMed]
- Chytas, D.; Mitrousias, V.; Raoulis, V.; Banios, K.; Fyllos, A.; Zibis, A.H. A Review of the Outcomes of the Implementation of Case-Based Anatomy Learning. Cureus 2021, 13, e19179. [Google Scholar] [CrossRef] [PubMed]
- Burgess, A.; Bleasel, J.; Haq, I.; Roberts, C.; Garsia, R.; Robertson, T.; Mellis, C. Team-based learning (TBL) in the medical curriculum: Better than PBL? BMC Med. Educ. 2017, 17, 243. [Google Scholar] [CrossRef] [PubMed]
- Burgess, A.; Matar, E.; Roberts, C.; Haq, I.; Wynter, L.; Singer, J.; Kalman, E.; Bleasel, J. Scaffolding medical student knowledge and skills: Team-based learning (TBL) and case-based learning (CBL). BMC Med. Educ. 2021, 21, 238. [Google Scholar] [CrossRef] [PubMed]
- Stentoft, D. Problem-based projects in medical education: Extending PBL practices and broadening learning perspectives. Adv. Health Sci. Educ. Theory Pract. 2019, 24, 959–969. [Google Scholar] [CrossRef] [PubMed]
- Thistlethwaite, J.E.; Davies, D.; Ekeocha, S.; Kidd, J.M.; MacDougall, C.; Matthews, P.; Purkis, J.; Clay, D. The effectiveness of case-based learning in health professional education. A BEME systematic review: BEME Guide No. 23. Med. Teach. 2012, 34, e421–e444. [Google Scholar] [CrossRef]
- Colbert, C.Y.; Graham, L.; West, C.; White, B.A.; Arroliga, A.C.; Myers, J.D.; Ogden, P.E.; Archer, J.; Mohammad, Z.T.; Clark, J. Teaching metacognitive skills: Helping your physician trainees in the quest to ‘know what they don’t know’. Am. J. Med. 2015, 128, 318–324. [Google Scholar] [CrossRef]
- Naug, H.L.; Colson, N.J.; Donner, D.G. Promoting metacognition in first year anatomy laboratories using plasticine modeling and drawing activities: A pilot study of the “blank page” technique. Anat. Sci. Educ. 2011, 4, 231–234. [Google Scholar] [CrossRef]
- Versteeg, M.; Steendijk, P. Putting post-decision wagering to the test: A measure of self-perceived knowledge in basic sciences? Perspect. Med. Educ. 2019, 8, 9–16. [Google Scholar] [CrossRef]
- Lazaros, E.J.; Davidson, C.J. Increasing Student Retention in STEM. Acad. Exch. Q. 2014, 18, 119–124. [Google Scholar]
- Wells, T.; Fishman, E.K.; Horton, K.M.; Rowe, S.P. Meet Generation Z. Top 10 Trends of 2018. J. Am. Coll. Radiol. 2018, 15, 1791–1793. [Google Scholar] [CrossRef]
- Attardi, S.M.; Taylor, T.A.H.; Lerchenfeldt, S.; Pratt, R.L.; Sawarynski, K.E. Adapting Strategically to Changing Times in Health Professions Education: A Generational Workshop for Educators. MedEdPORTAL 2021, 17, 11084. [Google Scholar] [CrossRef]
- Taranikanti, V. Is COVID Era the Beginning of a Paradigm Shift in Anatomy Education? Med. Health 2020, 15, 1–2. [Google Scholar] [CrossRef]
- Yeh, D.D.; Park, Y.S. Improving Learning Efficiency of Factual Knowledge in Medical Education. J. Surg. Educ. 2015, 72, 882–889. [Google Scholar] [CrossRef] [PubMed]
- Donkin, R.; Rasmussen, R. Student Perception and the Effectiveness of Kahoot!: A Scoping Review in Histology, Anatomy, and Medical Education. Anat. Sci. Educ. 2021, 14, 572–585. [Google Scholar] [CrossRef]
- Pereira, J.A.; Pleguezuelos, E.; Meri, A.; Molina-Ros, A.; Molina-Tomas, M.C.; Masdeu, C. Effectiveness of using blended learning strategies for teaching and learning human anatomy. Med. Educ. 2007, 41, 189–195. [Google Scholar] [CrossRef] [PubMed]
- Dong, H.; Lio, J.; Sherer, R.; Jiang, I. Some Learning Theories for Medical Educators. Med. Sci. Educ. 2021, 31, 1157–1172. [Google Scholar] [CrossRef]
- Gooding, H.C.; Mann, K.; Armstrong, E. Twelve tips for applying the science of learning to health professions education. Med. Teach. 2017, 39, 26–31. [Google Scholar] [CrossRef]
- Khodaei, S.; Hasanvand, S.; Gholami, M.; Mokhayeri, Y.; Amini, M. The effect of the online flipped classroom on self-directed learning readiness and metacognitive awareness in nursing students during the COVID-19 pandemic. BMC Nurs. 2022, 21, 22. [Google Scholar] [CrossRef]
- Lazaros, E.J.; Davidson, C.J. Asynchronous online classrooms: Success for student and teacher. Acad. Exch. Q. 2014, 18, 31. [Google Scholar]
- Gonullu, I.; Artar, M. Metacognition in medical education. Educ. Health 2014, 27, 225–226. [Google Scholar] [CrossRef]
- Rhodes, M.G. Metacognition. Teach. Psychol. 2019, 46, 168–175. [Google Scholar] [CrossRef]
- Siqueira, M.A.M.; Goncalves, J.P.; Mendonca, V.S.; Kobayasi, R.; Arantes-Costa, F.M.; Tempski, P.Z.; Martins, M.A. Relationship between metacognitive awareness and motivation to learn in medical students. BMC Med. Educ. 2020, 20, 393. [Google Scholar] [CrossRef] [PubMed]
- Williams, C.A. Exam Wrappers: It Is Time to Adopt a Nursing Student Metacognitive Tool for Exam Review. Nurs. Educ. Perspect. 2021, 42, 51–52. [Google Scholar] [CrossRef] [PubMed]
- Hayat, A.A.; Shateri, K. The Role of Academic Self-Efficacy in Improving Students’ Metacognitive Learning Strategies. J. Adv. Med. Educ. Prof. 2019, 7, 205–212. [Google Scholar] [PubMed]
- Rahmani, M. Medical Trainees and the Dunning-Kruger Effect: When They Don’t Know What They Don’t Know. J. Grad. Med. Educ. 2020, 12, 532–534. [Google Scholar] [CrossRef] [PubMed]
- Iskander, M. Burnout, Cognitive Overload, and Metacognition in Medicine. Med. Sci. Educ. 2019, 29, 325–328. [Google Scholar] [CrossRef]
- Burke, H.; Mancuso, L. Social cognitive theory, metacognition, and simulation learning in nursing education. J. Nurs. Educ. 2012, 51, 543–548. [Google Scholar] [CrossRef]
- Wesiak, G.; Steiner, C.M.; Moore, A.; Dagger, D.; Power, G.; Berthold, M.; Albert, D.; Conlan, O. Iterative augmentation of a medical training simulator: Effects of affective metacognitive scaffolding. Comput. Educ. 2014, 76, 13–29. [Google Scholar] [CrossRef]
- Cleary, T.J.; Konopasky, A.; La Rochelle, J.S.; Neubauer, B.E.; Durning, S.J.; Artino, A.R., Jr. First-year medical students’ calibration bias and accuracy across clinical reasoning activities. Adv. Health Sci. Educ. Theory Pract. 2019, 24, 767–781. [Google Scholar] [CrossRef]
- Artino, A.R.; Dong, T., Jr.; DeZee, K.J.; Gilliland, W.R.; Waechter, D.M.; Cruess, D.; Durning, S.J. Achievement goal structures and self-regulated learning: Relationships and changes in medical school. Acad. Med. 2012, 87, 1375–1381. [Google Scholar] [CrossRef]
- Gude, T.; Finset, A.; Anvik, T.; Baerheim, A.; Fasmer, O.B.; Grimstad, H.; Vaglum, P. Do medical students and young physicians assess reliably their self-efficacy regarding communication skills? A prospective study from end of medical school until end of internship. BMC Med. Educ. 2017, 17, 107. [Google Scholar] [CrossRef]
- Madrazo, L.; Lee, C.B.; McConnell, M.; Khamisa, K. Self-assessment differences between genders in a low-stakes objective structured clinical examination (OSCE). BMC Res. Notes 2018, 11, 393. [Google Scholar] [CrossRef] [PubMed]
- Ali, S.; Yasmeen, R. Practice to preach self-regulation: Use of metacognitive strategies by medical teachers in their learning practices. Pak. J. Med. Sci. 2019, 35, 1642–1646. [Google Scholar] [PubMed]
- Hayat, A.A.; Shateri, K.; Amini, M.; Shokrpour, N. Relationships between academic self-efficacy, learning-related emotions, and metacognitive learning strategies with academic performance in medical students: A structural equation model. BMC Med. Educ. 2020, 20, 76. [Google Scholar] [CrossRef] [PubMed]
- Jin, M.; Ji, C. The correlation of metacognitive ability, self-directed learning ability and critical thinking in nursing students: A cross-sectional study. Nurs. Open 2021, 8, 936–945. [Google Scholar] [CrossRef] [PubMed]
- Kosior, K.; Wall, T.; Ferrero, S. The role of metacognition in teaching clinical reasoning: Theory to practice. Educ. Health Prof. 2019, 2, 108–114. [Google Scholar]
- Zheng, B.; Chang, C.; Lin, C.H.; Zhang, Y. Self-Efficacy, Academic Motivation, and Self-Regulation: How Do They Predict Academic Achievement for Medical Students? Med. Sci. Educ. 2021, 31, 125–130. [Google Scholar] [CrossRef]
- Chew, K.S.; Durning, S.J.; van Merrienboer, J.J. Teaching metacognition in clinical decision-making using a novel mnemonic checklist: An exploratory study. Singap. Med. J. 2016, 57, 694–700. [Google Scholar] [CrossRef]
- Gholami, M.; Moghadam, P.K.; Mohammadipoor, F.; Tarahi, M.J.; Sak, M.; Toulabi, T.; Pour, A.H. Comparing the effects of problem-based learning and the traditional lecture method on critical thinking skills and metacognitive awareness in nursing students in a critical care nursing course. Nurse Educ. Today 2016, 45, 16–21. [Google Scholar] [CrossRef]
- Chang, C.; Colon-Berlingeri, M.; Mavis, B.; Laird-Fick, H.S.; Parker, C.; Solomon, D. Medical Student Progress Examination Performance and Its Relationship with Metacognition, Critical Thinking, and Self-Regulated Learning Strategies. Acad. Med. 2021, 96, 278–284. [Google Scholar] [CrossRef]
- Mahdavi, M. An Overview: Metacognition in Education. Int. J. Multidiciplin. Curr. Res. 2014, 2, 529–535. [Google Scholar]
- Robinson, P.M.; Griffiths, E.; Watts, A.C. Simple elbow dislocation. Shoulder Elb. 2017, 9, 195–204. [Google Scholar] [CrossRef] [PubMed]
- Gedi Ibrahim, I.; Tahtabasi, M. Doppler ultrasound diagnosis of brachial artery injury due to blunt trauma: A Case Report. Radiol. Case Rep. 2020, 15, 1207–1210. [Google Scholar] [CrossRef] [PubMed]
- Suvashis, D.; Rahul, M.; Lukesh, P. A rare cause of open acute compartment syndrome of fore arm following stab injury. Trauma Emerg. Care 2018, 3. [Google Scholar] [CrossRef]
- Rivers, M.L. Metacognition About Practice Testing: A Review of Learners’ Beliefs, Monitoring, and Control of Test-Enhanced Learning. Educ. Psychol. Rev. 2020, 33, 823–862. [Google Scholar] [CrossRef]
- Davidson, C.J.; Lazaros, E.J. How to use cognitive psychology when testing. Acad. Exch. Q. 2014, 18, 66–71. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).