The Influence of Knee Proprioception and Strength on Lower-Limb Functional Symmetry in Healthy Adults
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
2.2. Participants
2.3. Procedures
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chamorro-Moriana, G.; Perez-Cabezas, V.; Espuny-Ruiz, F.; Torres-Enamorado, D.; Ridao-Fernández, C. Assessing Knee Functionality: Systematic Review of Validated Outcome Measures. Ann. Phys. Rehabil. Med. 2022, 65, 101608. [Google Scholar] [CrossRef] [PubMed]
- Ford, K.R.; van den Bogert, J.; Myer, G.D.; Shapiro, R.; Hewett, T.E. The Effects of Age and Skill Level on Knee Musculature Co-Contraction during Functional Activities: A Systematic Review. Br. J. Sports Med. 2008, 42, 561–566. [Google Scholar] [CrossRef] [PubMed]
- Yılmaz, O.; Soylu, Y.; Erkmen, N.; Kaplan, T.; Batalik, L. Effects of Proprioceptive Training on Sports Performance: A Systematic Review. BMC Sports Sci. Med. Rehabil. 2024, 16, 149. [Google Scholar] [CrossRef]
- Davies, W.T.; Myer, G.D.; Read, P.J. Is It Time We Better Understood the Tests We Are Using for Return to Sport Decision Making Following ACL Reconstruction? A Critical Review of the Hop Tests. Sports Med. 2020, 50, 485–495. [Google Scholar] [CrossRef]
- Lawrence, E.L.; Cesar, G.M.; Bromfield, M.R.; Peterson, R.; Valero-Cuevas, F.J.; Sigward, S.M. Strength, Multijoint Coordination, and Sensorimotor Processing Are Independent Contributors to Overall Balance Ability. BioMed Res. Int. 2015, 2015, 561243. [Google Scholar] [CrossRef] [PubMed]
- Kyritsis, P.; Bahr, R.; Landreau, P.; Miladi, R.; Witvrouw, E. Likelihood of ACL Graft Rupture: Not Meeting Six Clinical Discharge Criteria before Return to Sport Is Associated with a Four Times Greater Risk of Rupture. Br. J. Sports Med. 2016, 50, 946–951. [Google Scholar] [CrossRef] [PubMed]
- West, T.J.; Bruder, A.M.; Crossley, K.M.; Culvenor, A.G. Unilateral Tests of Lower-Limb Function as Prognostic Indicators of Future Knee-Related Outcomes Following Anterior Cruciate Ligament Injury: A Systematic Review and Meta-Analysis of 13 150 Adolescents and Adults. Br. J. Sports Med. 2023, 57, 855–863. [Google Scholar] [CrossRef]
- Guild, P.; Lininger, M.R.; Warren, M. The Association Between the Single Leg Hop Test and Lower-Extremity Injuries in Female Athletes: A Critically Appraised Topic. J. Sport Rehabil. 2020, 30, 320–326. [Google Scholar] [CrossRef]
- Undheim, M.B.; Cosgrave, C.; King, E.; Strike, S.; Marshall, B.; Falvey, É.; Franklyn-Miller, A. Isokinetic Muscle Strength and Readiness to Return to Sport Following Anterior Cruciate Ligament Reconstruction: Is There an Association? A Systematic Review and a Protocol Recommendation. Br. J. Sports Med. 2015, 49, 1305–1310. [Google Scholar] [CrossRef]
- de la Motte, S.J.; Gribbin, T.C.; Lisman, P.; Murphy, K.; Deuster, P.A. Systematic Review of the Association Between Physical Fitness and Musculoskeletal Injury Risk: Part 2—Muscular Endurance and Muscular Strength. J. Strength Cond. Res. 2017, 31, 3218–3234. [Google Scholar] [CrossRef] [PubMed]
- Varol, U.; Navarro-Santana, M.J.; Valera-Calero, J.A.; Antón-Ramírez, S.; Álvaro-Martínez, J.; Díaz-Arribas, M.J.; Fernández-de-las-Peñas, C.; Plaza-Manzano, G. Convergent Validity between Electromyographic Muscle Activity, Ultrasound Muscle Thickness and Dynamometric Force Measurement for Assessing Muscle. Sensors 2023, 23, 2030. [Google Scholar] [CrossRef] [PubMed]
- Han, J.; Waddington, G.; Adams, R.; Anson, J.; Liu, Y. Assessing Proprioception: A Critical Review of Methods. J. Sport Health Sci. 2016, 5, 80–90. [Google Scholar] [CrossRef] [PubMed]
- He, X.; Qiu, J.; Cao, M.; Ho, Y.C.; Leong, H.T.; Fu, S.-C.; Ong, M.T.-Y.; Fong, D.T.P.; Yung, P.S.-H. Effects of Deficits in the Neuromuscular and Mechanical Properties of the Quadriceps and Hamstrings on Single-Leg Hop Performance and Dynamic Knee Stability in Patients After Anterior Cruciate Ligament Reconstruction. Orthop. J. Sports Med. 2022, 10, 23259671211063893. [Google Scholar] [CrossRef]
- Gokeler, A.; Benjaminse, A.; Hewett, T.E.; Lephart, S.M.; Engebretsen, L.; Ageberg, E.; Engelhardt, M.; Arnold, M.P.; Postema, K.; Otten, E.; et al. Proprioceptive Deficits after ACL Injury: Are They Clinically Relevant? Br. J. Sports Med. 2012, 46, 180–192. [Google Scholar] [CrossRef]
- Hegedus, E.J.; McDonough, S.; Bleakley, C.; Cook, C.E.; Baxter, G.D. Clinician-Friendly Lower Extremity Physical Performance Measures in Athletes: A Systematic Review of Measurement Properties and Correlation with Injury, Part 1. The Tests for Knee Function Including the Hop Tests. Br. J. Sports Med. 2015, 49, 642–648. [Google Scholar] [CrossRef] [PubMed]
- McGrath, T.M.; Waddington, G.; Scarvell, J.M.; Ball, N.B.; Creer, R.; Woods, K.; Smith, D. The Effect of Limb Dominance on Lower Limb Functional Performance—A Systematic Review. J. Sports Sci. 2016, 34, 289–302. [Google Scholar] [CrossRef] [PubMed]
- Drigny, J.; Rolland, M.; Remilly, M.; Guermont, H.; Reboursière, E.; Hulet, C.; Gauthier, A. Knee Proprioception Four Months after Anterior Cruciate Ligament Reconstruction: Impact of Limb Dominance, Anterolateral Procedure, and Association with Readiness to Return to Sport. Phys. Ther. Sport 2024, 71, 61–68. [Google Scholar] [CrossRef]
- Greenberg, E.M.; Dyke, J.; Leung, A.; Karl, M.; Lawrence, J.T.; Ganley, T. Uninjured Youth Athlete Performance on Single-Leg Hop Testing: How Many Can Achieve Recommended Return-to-Sport Criterion? Sports Health 2020, 12, 552–558. [Google Scholar] [CrossRef] [PubMed]
- Springer, S.; Kelman, D.; Brand, M.; Gottlieb, U. Knee Position Sense: Does the Time Interval at the Target Angle Affect Position Accuracy? J. Phys. Ther. Sci. 2017, 29, 1760–1765. [Google Scholar] [CrossRef] [PubMed]
- Steidl-Müller, L.; Hildebrandt, C.; Müller, E.; Fink, C.; Raschner, C. Limb Symmetry Index in Competitive Alpine Ski Racers: Reference Values and Injury Risk Identification According to Age-Related Performance Levels. J. Sport Health Sci. 2018, 7, 405–415. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Lawrence Erlbaum Associates: Hillsdale, NJ, USA, 1988; ISBN 978-0-8058-0283-2. [Google Scholar]
- English, R.; Brannock, M.; Chik, W.T.; Eastwood, L.S.; Uhl, T. The Relationship between Lower Extremity Isokinetic Work and Single-Leg Functional Hop-Work Test. J. Sport Rehabil. 2006, 15, 95–104. [Google Scholar] [CrossRef][Green Version]
- Jones, P.A.; Bampouras, T.M. A Comparison of Isokinetic and Functional Methods of Assessing Bilateral Strength Imbalance. J. Strength Cond. Res. 2010, 24, 1553–1558. [Google Scholar] [CrossRef] [PubMed]
- Vassis, K.; Kanellopoulos, A.K.; Misiris, I.; Trigkas, P.; Spanos, S.; Poulis, I.A. Knee Isokinetic Test Scores and Functional Hop Tests Findings: Are They Related? Isokinet. Exerc. Sci. 2020, 28, 231–238. [Google Scholar] [CrossRef]
- Sueyoshi, T.; Nakahata, A.; Emoto, G.; Yuasa, T. Single-Leg Hop Test Performance and Isokinetic Knee Strength After Anterior Cruciate Ligament Reconstruction in Athletes. Orthop. J. Sports Med. 2017, 5, 2325967117739811. [Google Scholar] [CrossRef] [PubMed]
- Pincivero, D.M.; Lephart, S.M.; Karunakara, R.G. Relation between Open and Closed Kinematic Chain Assessment of Knee Strength and Functional Performance. Clin. J. Sport Med. 1997, 7, 11–16. [Google Scholar] [CrossRef]
- Bencke, J.; Strøm, M.; Curtis, D.J.; Bandholm, T.; Zebis, M.K. Differences in Thigh Muscle Activation Between Standing and Landing Exercises for Knee Injury Prevention and Rehabilitation. Int. J. Sports Phys. Ther. 2023, 18, 102–112. [Google Scholar] [CrossRef]
- Ueno, R.; Navacchia, A.; Schilaty, N.D.; Myer, G.D.; Hewett, T.E.; Bates, N.A. Hamstrings Contraction Regulates the Magnitude and Timing of the Peak ACL Loading During the Drop Vertical Jump in Female Athletes. Orthop. J. Sports Med. 2021, 9, 23259671211034487. [Google Scholar] [CrossRef]
- Strong, A.; Grip, H.; Boraxbekk, C.-J.; Selling, J.; Häger, C.K. Brain Response to a Knee Proprioception Task Among Persons With Anterior Cruciate Ligament Reconstruction and Controls. Front. Hum. Neurosci. 2022, 16, 841874. [Google Scholar] [CrossRef] [PubMed]
- Iandolo, R.; Bellini, A.; Saiote, C.; Marre, I.; Bommarito, G.; Oesingmann, N.; Fleysher, L.; Mancardi, G.L.; Casadio, M.; Inglese, M. Neural Correlates of Lower Limbs Proprioception: An fMRI Study of Foot Position Matching. Hum. Brain Mapp. 2018, 39, 1929–1944. [Google Scholar] [CrossRef]
- Strong, A.; Grip, H.; Arumugam, A.; Boraxbekk, C.-J.; Selling, J.; Häger, C.K. Right Hemisphere Brain Lateralization for Knee Proprioception among Right-Limb Dominant Individuals. Front. Hum. Neurosci. 2023, 17, 969101. [Google Scholar] [CrossRef] [PubMed]
- Galamb, K.; Szilágyi, B.; Magyar, O.M.; Hortobágyi, T.; Nagatomi, R.; Váczi, M.; Négyesi, J. Effects of Side-Dominance on Knee Joint Proprioceptive Target-Matching Asymmetries. Physiol. Int. 2018, 105, 257–265. [Google Scholar] [CrossRef] [PubMed]
- Nagai, T.; Sell, T.C.; House, A.J.; Abt, J.P.; Lephart, S.M. Knee Proprioception and Strength and Landing Kinematics During a Single-Leg Stop-Jump Task. J. Athl. Train. 2013, 48, 31–38. [Google Scholar] [CrossRef] [PubMed]
- Marini, F.; Ferrantino, M.; Zenzeri, J. Proprioceptive Identification of Joint Position versus Kinaesthetic Movement Reproduction. Hum. Mov. Sci. 2018, 62, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Proske, U.; Gandevia, S.C. The Kinaesthetic Senses. J. Physiol. 2009, 587, 4139. [Google Scholar] [CrossRef] [PubMed]
- Szafraniec, R.; Stefaniak, T.; Harmaciński, D.; Kuczyński, M. Inter-Limb Asymmetry in Force Accuracy and Steadiness Changes after a 12-Week Strength Training Program in Young Healthy Men. Symmetry 2021, 13, 2226. [Google Scholar] [CrossRef]
- Goodwin, G.M.; McCloskey, D.I.; Matthews, P.B. The Contribution of Muscle Afferents to Kinaesthesia Shown by Vibration Induced Illusions of Movement and by the Effects of Paralysing Joint Afferents. Brain J. Neurol. 1972, 95, 705–748. [Google Scholar] [CrossRef]
- Proske, U.; Gandevia, S.C. The Proprioceptive Senses: Their Roles in Signaling Body Shape, Body Position and Movement, and Muscle Force. Physiol. Rev. 2012, 92, 1651–1697. [Google Scholar] [CrossRef]
- Jami, L.; Petit, J.; Proske, U.; Zytnicki, D. Responses of Tendon Organs to Unfused Contractions of Single Motor Units. J. Neurophysiol. 1985, 53, 32–42. [Google Scholar] [CrossRef]
- Jami, L. Golgi Tendon Organs in Mammalian Skeletal Muscle: Functional Properties and Central Actions. Physiol. Rev. 1992, 72, 623–666. [Google Scholar] [CrossRef] [PubMed]
- Proske, U.; Tsay, A.; Allen, T. Muscle Thixotropy as a Tool in the Study of Proprioception. Exp. Brain Res. 2014, 232, 3397–3412. [Google Scholar] [CrossRef]
- Davies, G.; Riemann, B.; Manske, R. Current Concepts of Plyometric Exercises. Int. J. Sports Phys. Ther. 2015, 10, 760–786. [Google Scholar] [PubMed]
- Blum, K.P.; Campbell, K.S.; Horslen, B.C.; Nardelli, P.; Housley, S.N.; Cope, T.C.; Ting, L.H. Diverse and Complex Muscle Spindle Afferent Firing Properties Emerge from Multiscale Muscle Mechanics. eLife 2020, 9, e55177. [Google Scholar] [CrossRef]
- Santuz, A.; Akay, T. Muscle Spindles and Their Role in Maintaining Robust Locomotion. J. Physiol. 2023, 601, 275–285. [Google Scholar] [CrossRef] [PubMed]
- Santuz, A.; Laflamme, O.D.; Akay, T. The Brain Integrates Proprioceptive Information to Ensure Robust Locomotion. J. Physiol. 2022, 600, 5267–5294. [Google Scholar] [CrossRef]
- Gjinovci, B.; Idrizovic, K.; Uljevic, O.; Sekulic, D. Plyometric Training Improves Sprinting, Jumping and Throwing Capacities of High Level Female Volleyball Players Better Than Skill-Based Conditioning. J. Sports Sci. Med. 2017, 16, 527–535. [Google Scholar]
- Schmitt, L.C.; Paterno, M.V.; Hewett, T.E. The Impact of Quadriceps Femoris Strength Asymmetry on Functional Performance at Return to Sport Following Anterior Cruciate Ligament Reconstruction. J. Orthop. Sports Phys. Ther. 2012, 42, 750–759. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.-F.; Liu, H.; Gros, M.T.; Weinhold, P.; Garrett, W.E.; Yu, B. Biomechanical Risk Factors of Non-Contact ACL Injuries: A Stochastic Biomechanical Modeling Study. J. Sport Health Sci. 2012, 1, 36–42. [Google Scholar] [CrossRef]
- Rajula, H.S.R.; Verlato, G.; Manchia, M.; Antonucci, N.; Fanos, V. Comparison of Conventional Statistical Methods with Machine Learning in Medicine: Diagnosis, Drug Development, and Treatment. Medicina 2020, 56, 455. [Google Scholar] [CrossRef]
- Molavian, R.; Fatahi, A.; Abbasi, H.; Khezri, D. Artificial Intelligence Approach in Biomechanics of Gait and Sport: A Systematic Literature Review. J. Biomed. Phys. Eng. 2023, 13, 383–402. [Google Scholar] [CrossRef]
- Kotsifaki, A.; Korakakis, V.; Graham-Smith, P.; Sideris, V.; Whiteley, R. Vertical and Horizontal Hop Performance: Contributions of the Hip, Knee, and Ankle. Sports Health 2021, 13, 128–135. [Google Scholar] [CrossRef] [PubMed]
- Pedley, J.S.; Lloyd, R.S.; Read, P.J.; Moore, I.S.; De Ste Croix, M.; Myer, G.D.; Oliver, J.L. Utility of Kinetic and Kinematic Jumping and Landing Variables as Predictors of Injury Risk: A Systematic Review. J. Sci. Sport Exerc. 2020, 2, 287–304. [Google Scholar] [CrossRef]

| Performance | Symmetry | ||||
|---|---|---|---|---|---|
| Dominant Limb | Non-Dominant Limb | Diff (°) or LSI (%) | |||
| Isokinetic testing | Proprioception/ Kinesthesia | JPS 1 (°) | 2.66 (2.2) | 2.35 (2.49) | −0.31 (3.78) |
| JPS 2 (°) | 2.10 (1.65) | 2.51 (2.2) | 0.41 (3.25) | ||
| TTDPM (°) | 2.08 (1.2) | 3.27 (2.85) * | 1.20 (2.08) | ||
| Strength | ext 60°·s−1 (N·m·kg−1) | 2.42 (0.56) | 2.31 (0.63) * | 89.41% (14.23%) | |
| flex 60°·s−1 (N·m·kg−1) | 1.38 (0.31) | 1.42 (0.41) | 94.50% (25.66%) | ||
| ext 240°·s−1 (N·m·kg−1) | 1.61 (0.46) | 1.50 (0.37) | 95.81% (18.32%) | ||
| flex 240°·s−1 (N·m·kg−1) | 1.15 (0.39) | 1.06 (0.28) | 98.21% (25.14%) | ||
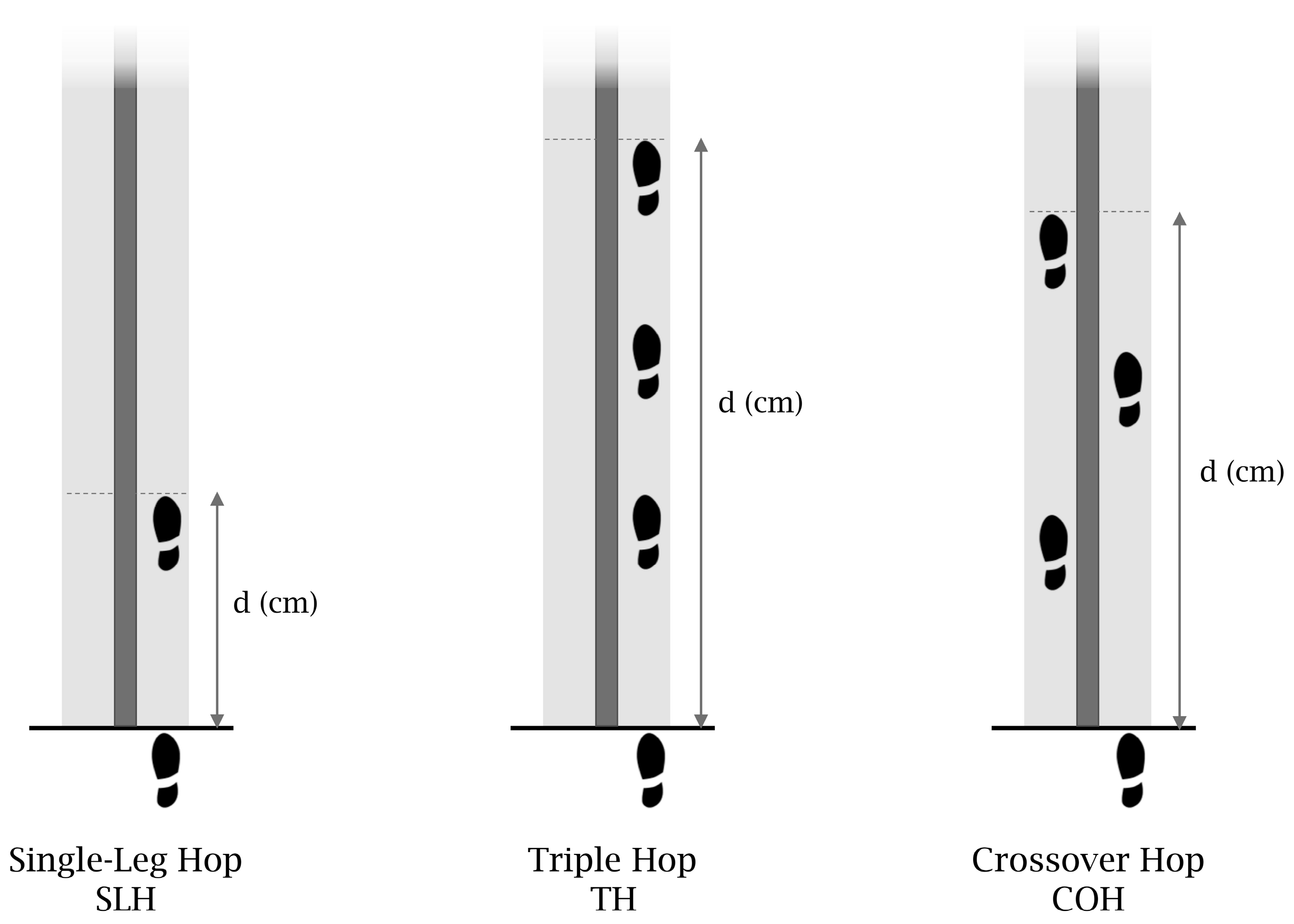
| Functional testing | Hop tests | SLH (dist/height, m) | 0.85 (0.13) | 0.83 (0.12) | 97.50% (6.94%) |
| TH (dist/height, m) | 2.51 (0.34) | 2.39 (0.35) * | 95.31% (7.45%) | ||
| COH (dist/height, m) | 2.40 (0.31) | 2.28 (0.35) * | 95.23% (9.63%) | ||
| (a) Performance | ||||
|---|---|---|---|---|
| SLH (Dist/Height, m) | TH (Dist/Height, m) | COH (Dist/Height, m) | ||
| Proprioception/Kinesthesia | ||||
| JPS 1 (°) | Pearson’s r | −0.07 | 0.00 | 0.18 |
| p-value | 0.664 | 0.985 | 0.254 | |
| JPS 2 (°) | Pearson’s r | 0.07 | 0.11 | 0.00 |
| p-value | 0.682 | 0.510 | 0.990 | |
| TTDPM (°) | Pearson’s r | −0.11 | −0.26 | −0.23 |
| p-value | 0.515 | 0.104 | 0.162 | |
| Strength | ||||
| ext 60°·s−1 (N·m·kg−1) | Pearson’s r | 0.65 ** | 0.58 ** | 0.56 ** |
| p-value | <0.001 | <0.001 | <0.001 | |
| flex 60°·s−1 (N·m·kg−1) | Pearson’s r | 0.31 | 0.19 | 0.22 |
| p-value | 0.052 | 0.229 | 0.169 | |
| ext 240°·s−1 (N·m·kg−1) | Pearson’s r | 0.70 ** | 0.69 ** | 0.66 ** |
| p-value | <0.001 | <0.001 | <0.001 | |
| flex 240°·s−1 (N·m·kg−1) | Pearson’s r | 0.35 * | 0.35 * | 0.33 * |
| p-value | 0.029 | 0.026 | 0.037 | |
| (b) Symmetry | ||||
| SLH (LSI, %) | TH (LSI, %) | COH (LSI, %) | ||
| Proprioception/Kinesthesia | ||||
| JPS 1 (AEdiff,°) | Pearson’s r | −0.53 * | −0.49 * | −0.70 ** |
| p-value | 0.017 | 0.048 | 0.001 | |
| JPS 2 (AEdiff,°) | Pearson’s r | −0.46 * | −0.37 | −0.44 * |
| p-value | 0.040 | 0.076 | 0.050 | |
| TTDPM (AEdiff,°) | Pearson’s r | −0.15 | −0.23 | −0.21 |
| p-value | 0.533 | 0.278 | 0.375 | |
| Strength | ||||
| ext 60°·s−1 (LSI, %) | Pearson’s r | 0.26 | 0.08 | 0.13 |
| p-value | 0.276 | 0.423 | 0.579 | |
| flex 60°·s−1 (LSI, %) | Pearson’s r | 0.18 | 0.02 | 0.04 |
| p-value | 0.451 | 0.928 | 0.864 | |
| ext 240°·s−1 (LSI, %) | Pearson’s r | 0.14 | 0.15 | 0.15 |
| p-value | 0.545 | 0.547 | 0.526 | |
| flex 240°·s−1 (LSI, %) | Pearson’s r | 0.13 | 0.16 | 0.13 |
| p-value | 0.594 | 0.268 | 0.597 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Drigny, J.; Rolland, M.; Gauthier, A. The Influence of Knee Proprioception and Strength on Lower-Limb Functional Symmetry in Healthy Adults. Muscles 2025, 4, 3. https://doi.org/10.3390/muscles4010003
Drigny J, Rolland M, Gauthier A. The Influence of Knee Proprioception and Strength on Lower-Limb Functional Symmetry in Healthy Adults. Muscles. 2025; 4(1):3. https://doi.org/10.3390/muscles4010003
Chicago/Turabian StyleDrigny, Joffrey, Marine Rolland, and Antoine Gauthier. 2025. "The Influence of Knee Proprioception and Strength on Lower-Limb Functional Symmetry in Healthy Adults" Muscles 4, no. 1: 3. https://doi.org/10.3390/muscles4010003
APA StyleDrigny, J., Rolland, M., & Gauthier, A. (2025). The Influence of Knee Proprioception and Strength on Lower-Limb Functional Symmetry in Healthy Adults. Muscles, 4(1), 3. https://doi.org/10.3390/muscles4010003






