Current Indications and Future Direction in Heat Therapy for Musculoskeletal Pain: A Narrative Review
Abstract
1. Introduction
2. Heat Therapy Overview
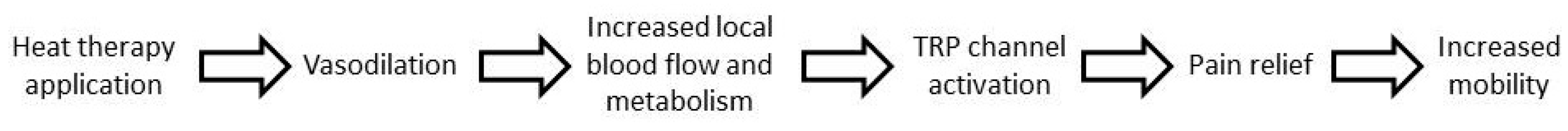
2.1. Mechanism of Action
2.2. Clinical Applications
2.3. Application Modalities
2.4. Safety
2.5. Heat Therapy versus Cold Therapy, Which and When
2.6. Specific Applications of Heat Therapy
3. Heat Therapy and Knee Pain
3.1. Knee Pain as a Multifaceted Clinical Condition
3.2. Heat Therapy for the Management of Knee Pain
3.3. Heat versus Cold Therapy in Knee Pain
4. Heat Therapy and Sport
4.1. Heat Therapy Application in Sport
4.2. Heat versus Cold Therapy in Sport
5. Discussion
6. Materials and Methods
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study. Lancet 2019, 396, 1204–1222. [Google Scholar]
- Puntillo, F.; Giglio, M.; Paladini, A.; Perchiazzi, G.; Viswanath, O.; Urits, I.; Sabbà, C.; Varrassi, G.; Brienza, N. Pathophysiology of musculoskeletal pain: A narrative review. Ther. Adv. Musculoskelet. Dis. 2021, 13, 1759720X2199506. [Google Scholar] [CrossRef] [PubMed]
- Blyth, F.M.; Briggs, A.M.; Schneider, C.H.; Hoy, D.G.; March, L.M. The Global Burden of Musculoskeletal Pain—Where to From Here? Am. J. Public Health 2019, 109, 35–40. [Google Scholar] [CrossRef] [PubMed]
- El-Tallawy, S.N.; Nalamasu, R.; Salem, G.I.; LeQuang, J.A.K.; Pergolizzi, J.V.; Christo, P.J. Management of Musculoskeletal Pain: An Update with Emphasis on Chronic Musculoskeletal Pain. Pain. Ther. 2021, 10, 181–209. [Google Scholar] [CrossRef] [PubMed]
- Kolasinski, S.L.; Neogi, T.; Hochberg, M.C.; Oatis, C.; Guyatt, G.; Block, J.; Callahan, L.; Copenhaver, C.; Dodge, C.; Felson, D.; et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Management of Osteoarthritis of the Hand, Hip, and Knee. Arthritis Rheumatol. 2020, 72, 220–233. [Google Scholar] [CrossRef] [PubMed]
- Malanga, G.A.; Yan, N.; Stark, J. Mechanisms and efficacy of heat and cold therapies for musculoskeletal injury. Postgrad. Med. 2015, 127, 57–65. [Google Scholar] [CrossRef] [PubMed]
- Papaioannou, T.G.; Karamanou, M.; Protogerou, A.D.; Tousoulis, D. Heat therapy: An ancient concept re-examined in the era of advanced biomedical technologies. J. Physiol. 2016, 594, 7141–7142. [Google Scholar] [CrossRef] [PubMed]
- Green, B.G. Temperature perception and nociception. J. Neurobiol. 2004, 61, 13–29. [Google Scholar] [CrossRef] [PubMed]
- Brederson, J.D.; Kym, P.R.; Szallasi, A. Targeting TRP channels for pain relief. Eur. J. Pharmacol. 2013, 716, 61–76. [Google Scholar] [CrossRef]
- Nadler, S.F.; Weingand, K.; Kruse, R.J. The physiologic basis and clinical applications of cryotherapy and thermotherapy for the pain practitioner. Pain. Physician 2004, 7, 395–399. [Google Scholar] [CrossRef]
- Klingler, W. Temperature effects on fascia. In Fascia—The Tensional Network of the Human Body; Schleip, R., Findley, T.W., Chaitow, L., Huijing, P., Eds.; Churchill Living: Medford, MA, USA, 2012. [Google Scholar]
- Freiwald, J.; Magni, A.; Fanlo-Mazas, P.; Paulino, E.; Sequeira de Medeiros, L.; Moretti, B.; Schleip, R.; Solarino, G. A Role for Superficial Heat Therapy in the Management of Non-Specific, Mild-to-Moderate Low Back Pain in Current Clinical Practice: A Narrative Review. Life 2021, 11, 780. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.; Reid, B.A.; Casey, C.A.; Bender, B.E.; Ro, B.; Song, Q.; Trewin, A.J.; Petersen, A.C.; Kuang, S.; Gavin, T.P.; et al. Effects of repeated local heat therapy on skeletal muscle structure and function in humans. J. Appl. Physiol. 2020, 128, 483–492. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, P.; Trajano, G.S.; Wharton, L.; Minett, G.M. Effects of passive heating intervention on muscle hypertrophy and neuromuscular function: A preliminary systematic review with meta-analysis. J. Therm. Biol. 2020, 93, 102684. [Google Scholar] [CrossRef] [PubMed]
- Deal, D.N.; Tipton, J.; Rosencrance, E.; Curl, W.W.; Smith, T.L. Ice reduces edema. A study of microvascular permeability in rats. J. Bone Jt. Surg. Am. 2002, 84, 1573–1578. [Google Scholar] [CrossRef]
- Schaser, K.D.; Vollmar, B.; Menger, M.D.; Schewior, L.; Kroppenstedt, S.N.; Raschke, M.; Lübbe, A.S.; Haas, N.P.; Mittlmeier, T. In vivo analysis of microcirculation following closed soft-tissue injury. J. Orthop. Res. 1999, 17, 678–685. [Google Scholar] [CrossRef] [PubMed]
- Merrick, M.A.; Rankin, J.M.; Andres, F.A.; Hinman, C.L. A preliminary examination of cryotherapy and secondary injury in skeletal muscle. Med. Sci. Sports Exerc. 1999, 31, 1516–1521. [Google Scholar] [CrossRef] [PubMed]
- Sapega, A.A.; Heppenstall, R.B.; Sokolow, D.P.; Graham, T.J.; Maris, J.M.; Ghosh, A.K.; Chance, B.; Osterman, A.L. The bioenergetics of preservation of limbs before replantation. The rationale for intermediate hypothermia. J. Bone Jt. Surg. Am. 1988, 70, 1500–1513. [Google Scholar] [CrossRef]
- Algafly, A.A.; George, K.P. The effect of cryotherapy on nerve conduction velocity, pain threshold and pain tolerance. Br. J. Sports Med. 2007, 41, 365–369. [Google Scholar] [CrossRef]
- Lee, S.U.; Bang, M.S.; Han, T.R. Effect of cold air therapy in relieving spasticity: Applied to spinalized rabbits. Spinal Cord. 2002, 40, 167–173. [Google Scholar] [CrossRef]
- Allan, R.; Malone, J.; Alexander, J.; Vorajee, S.; Ihsan, M.; Gregson, W.; Kwiecien, S.; Mawhinney, C. Cold for centuries: A brief history of cryotherapies to improve health, injury and post-exercise recovery. Eur. J. Appl. Physiol. 2022, 122, 1153–1162. [Google Scholar] [CrossRef]
- Kwiecien, S.Y.; McHugh, M.P. The cold truth: The role of cryotherapy in the treatment of injury and recovery from exercise. Eur. J. Appl. Physiol. 2021, 121, 2125–2142. [Google Scholar] [CrossRef]
- Wang, Y.; Li, S.; Zhang, Y.; Chen, Y.; Yan, F.; Han, L.; Ma, Y. Heat and cold therapy reduce pain in patients with delayed onset muscle soreness: A systematic review and meta-analysis of 32 randomized controlled trials. Phys. Ther. Sport 2021, 48, 177–187. [Google Scholar] [CrossRef]
- Petrofsky, J.S.; Laymon, M.; Alshammari, F.; Khowailed, I.A.; Lee, H. Use of low level of continuous heat and Ibuprofen as an adjunct to physical therapy improves pain relief, range of motion and the compliance for home exercise in patients with nonspecific neck pain: A randomized controlled trial. J. Back. Musculoskelet. Rehabil. 2017, 30, 889–896. [Google Scholar] [CrossRef]
- French, S.D.; Cameron, M.; Walker, B.F.; Reggars, J.W.; Esterman, A.J. Superficial heat or cold for low back pain. Cochrane Database Syst. Rev. 2006, 2006, CD004750. [Google Scholar] [CrossRef]
- Nadler, S.F.; Steiner, D.J.; Erasala, G.N.; Hengehold, D.A.; Hinkle, R.T.; Beth Goodale, M.; Abeln, S.B.; Weingand, K.W. Continuous low-level heat wrap therapy provides more efficacy than Ibuprofen and acetaminophen for acute low back pain. Spine (Phila Pa 1976) 2002, 27, 1012–1017. [Google Scholar] [CrossRef]
- Nadler, S.F.; Steiner, D.J.; Erasala, G.N.; Hengehold, D.A.; Abeln, S.B.; Weingand, K.W. Continuous low-level heatwrap therapy for treating acute nonspecific low back pain. Arch. Phys. Med. Rehabil. 2003, 84, 329–334. [Google Scholar] [CrossRef]
- Petrofsky, J.S.; Laymon, M.S.; Alshammari, F.S.; Lee, H. Use of Low Level of Continuous Heat as an Adjunct to Physical Therapy Improves Knee Pain Recovery and the Compliance for Home Exercise in Patients with Chronic Knee Pain: A Randomized Controlled Trial. J. Strength Cond. Res. 2016, 30, 3107–3115. [Google Scholar] [CrossRef] [PubMed]
- Petrofsky, J.; Laymon, M.; Alshammari, F.; Khowailed, I.A.; Lee, H. Continuous Low Level Heat Wraps; Faster Healing and Pain Relief during Rehabilitation for Back, Knee and Neck Injuries. World J. Prev. Med. 2015, 3, 61–72. [Google Scholar]
- McCarberg, W.; Erasala, G.; Goodale, M.; Grender, J.M.; Hengehold, D.; Donikyan, L. Therapeutic benefits of Continuous Low-level Heat wrap Therapy (CLHT) for Osteoarthritis (OA) of the knee. J. Pain. 2005, 6, 781. [Google Scholar] [CrossRef]
- Draper, D.O.; Hopkins, T.J. Increased intramuscular and intracapsular temperature via ThermaCare Knee Wrap application. Med. Sci. Monit. 2008, 14, PI7–PI11. [Google Scholar]
- Michlovitz, S.; Hun, L.; Erasala, G.N.; Hengehold, D.A.; Weingand, K.W. Continuous low-level heat wrap therapy is effective for treating wrist pain. Arch. Phys. Med. Rehabil. 2004, 85, 1409–1416. [Google Scholar] [CrossRef] [PubMed]
- Mayer, J.M.; Mooney, V.; Matheson, L.N.; Erasala, G.N.; Verna, J.L.; Udermann, B.E.; Leggett, S. Continuous low-level heat wrap therapy for the prevention and early phase treatment of delayed-onset muscle soreness of the low back: A randomized controlled trial. Arch. Phys. Med. Rehabil. 2006, 87, 1310–1317. [Google Scholar] [CrossRef] [PubMed]
- Petrofsky, J.; Batt, J.; Bollinger, J.N.; Jensen, M.C.; Maru, E.H.; Al-Nakhli, H.H. Comparison of different heat modalities for treating delayed onset muscle soreness in people with diabetes. Diabetes Technol. Ther. 2011, 13, 645–655. [Google Scholar] [CrossRef] [PubMed]
- Heiss, R.; Lutter, C.; Freiwald, J.; Hoppe, M.W.; Grim, C.; Poettgen, K.; Forst, R.; Bloch, W.; Hüttel, M.; Hotfiel, T. Advances in Delayed-Onset Muscle Soreness (DOMS)—Part II: Treatment and Prevention. Sportverletz. Sportschaden 2019, 33, 21–29. [Google Scholar] [CrossRef] [PubMed]
- Lubrano, E.; Mazas, P.F.; Freiwald, J.; Krüger, K.; Grattagliano, I.; Mur, E.; Silva, R.Q.; Maruri, G.R.; de Medeiros, L.S. An International Multidisciplinary Delphi-Based Consensus on Heat Therapy in Musculoskeletal Pain. Pain. Ther. 2023, 12, 93–110. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.S.; Annaswamy, T.M.; Yang, W.; Wang, T.G.; Kwon, D.R.; Chou, L.W. Physical Agent Modalities. In Braddom’s Physical Medicine and Rehabilitation; Elsevier: Amsterdam, The Netherlands, 2021; pp. 338–363.e6. [Google Scholar]
- Forcina, L.; Cosentino, M.; Musarò, A. Mechanisms Regulating Muscle Regeneration: Insights into the Interrelated and Time-Dependent Phases of Tissue Healing. Cells 2020, 9, 1297. [Google Scholar] [CrossRef] [PubMed]
- Lohman, E.B., 3rd; Sackiriyas, K.S.; Bains, G.S.; Calandra, G.; Lobo, C.; Nakhro, D.; Malthankar, G.; Paul, S. A comparison of whole body vibration and moist heat on lower extremity skin temperature and skin blood flow in healthy older individuals. Med. Sci. Monit. 2012, 18, CR415–CR424. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kim, W.S.; Kim, J. Exploring the impact of temporal heat stress on skeletal muscle hypertrophy in bovine myocytes. J. Therm. Biol. 2023, 117, 103684. [Google Scholar] [CrossRef] [PubMed]
- Sluka, K.A.; Christy, M.R.; Peterson, W.L.; Rudd, S.L.; Troy, S.M. Reduction of pain-related behaviors with either cold or heat treatment in an animal model of acute arthritis. Arch. Phys. Med. Rehabil. 1999, 80, 313–317. [Google Scholar] [CrossRef]
- Hotfiel, T.; Hoppe, M.W.; Heiss, R.; Lutter, C.; Tischer, T.; Forst, R.; Hammer, C.M.; Freiwald, J.; Engelhardt, M.; Grim, C. Quantifiable Contrast-Enhanced Ultrasound Explores the Role of Protection, Rest, Ice (Cryotherapy), Compression and Elevation (PRICE) Therapy on Microvascular Blood Flow. Ultrasound Med. Biol. 2021, 47, 1269–1278. [Google Scholar] [CrossRef]
- Coderre, T.J. Contribution of microvascular dysfunction to chronic pain. Front. Pain Res. 2023, 4, 1111559. [Google Scholar] [CrossRef] [PubMed]
- Hadler, N.M. Knee pain is the malady—Not osteoarthritis. Ann. Intern. Med. 1992, 116, 598–599. [Google Scholar] [CrossRef] [PubMed]
- Mandl, L.A. Osteoarthritis year in review 2018: Clinical. Osteoarthr. Cartil. 2019, 27, 359–364. [Google Scholar] [CrossRef]
- Kujala, U.M.; Taimela, S.; Antti-Poika, I.; Orava, S.; Tuominen, R.; Myllynen, P. Acute injuries in soccer, ice hockey, volleyball, basketball, judo, and karate: Analysis of national registry data. BMJ 1995, 311, 1465–1468. [Google Scholar] [CrossRef] [PubMed]
- Gage, B.E.; McIlvain, N.M.; Collins, C.L.; Fields, S.K.; Comstock, R.D. Epidemiology of 6.6 Million Knee Injuries Presenting to United States Emergency Departments from 1999 Through 2008. Acad. Emerg. Med. 2012, 19, 378–385. [Google Scholar] [CrossRef] [PubMed]
- Hunter, D.J.; McDougall, J.J.; Keefe, F.J. The Symptoms of Osteoarthritis and the Genesis of Pain. Rheum. Dis. Clin. N. Am. 2008, 34, 623–643. [Google Scholar] [CrossRef] [PubMed]
- Madi, S.; Acharya, K.; Pandey, V. Current concepts on management of medial and posteromedial knee injuries. J. Clin. Orthop. Trauma. 2022, 27, 101807. [Google Scholar] [CrossRef]
- Lavelle, E.D.; Lavelle, W.; Smith, H.S. Myofascial trigger points. Anesthesiol. Clin. 2007, 4, 841–851. [Google Scholar]
- Rahou-El-Bachiri, Y.; Navarro-Santana, M.J.; Gómez-Chiguano, G.F. Effects of Trigger Point Dry Needling for the Management of Knee Pain Syndromes: A Systematic Review and Meta-Analysis. J. Clin. Med. 2020, 9, 2044. [Google Scholar] [CrossRef]
- Gaitonde, D.Y.; Ericksen, A.; Robbins, R.C. Patellofemoral Pain Syndrome. Am. Fam. Physician 2019, 99, 88–94. [Google Scholar]
- D’Ambrosi, R.; Meena, A.; Raj, A.; Ursino, N.; Hewett, T.E. Anterior Knee Pain: State of the Art. Sport Med.—Open 2022, 8, 98. [Google Scholar] [CrossRef]
- Strauss, E.J.; Kim, S.; Calcei, J.G.; Park, D. Iliotibial band syndrome: Evaluation and management. J. Am. Acad. Orthop. Surg. 2011, 19, 728–736. [Google Scholar] [CrossRef] [PubMed]
- Qaseem, A.; Wilt, T.J.; McLean, R.M.; Forciea, M.A. Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline From the American College of Physicians. Ann. Intern. Med. 2017, 166, 514. [Google Scholar] [CrossRef]
- Hochberg, M.C.; Altman, R.D.; April, K.T.; Benkhalti, M.; Guyatt, G.; McGowan, J.; Towheed, T.; Welch, V.; Wells, G.; Tugwell, P.; et al. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res. 2012, 64, 465–474. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, L.; Hagen, K.B.; Bijlsma, J.W.; Andreassen, O.; Christensen, P.; Conaghan, P.G.; Doherty, M.; Geenen, R.; Hammond, A.; Kjeken, I.; et al. EULAR recommendations for the non-pharmacological core management of hip and knee osteoarthritis. Ann. Rheum. Dis. 2013, 72, 1125–1135. [Google Scholar] [CrossRef]
- Kim, H.; Suzuki, T.; Saito, K.; Kim, M.; Kojima, N.; Ishizaki, T.; Yamashiro, Y.; Hosoi, E.; Yoshida, H. Effectiveness of exercise with or without thermal therapy for community-dwelling elderly Japanese women with non-specific knee pain: A randomized controlled trial. Arch. Gerontol. Geriatr. 2013, 57, 352–359. [Google Scholar] [CrossRef] [PubMed]
- Ochiai, S.; Watanabe, A.; Oda, H.; Ikeda, H. Effectiveness of Thermotherapy Using a Heat and Steam Generating Sheet for Cartilage in Knee Osteoarthritis. J. Phys. Ther. Sci. 2014, 26, 281–284. [Google Scholar] [CrossRef] [PubMed]
- Ariana, M.; Afrasiabifar, A.; Najafi Doulatabad, S.; Mosavi, A.; Behnammoghadam, M. The Effect of Local Heat Therapy versus Cold Rub Gel on Pain and Joint Functions in Patients with Knee Osteoarthritis. Clin. Nurs. Res. 2022, 31, 1014–1022. [Google Scholar] [CrossRef] [PubMed]
- Aciksoz, S.; Akyuz, A.; Tunay, S. The effect of self-administered superficial local hot and cold application methods on pain, functional status and quality of life in primary knee osteoarthritis patients. J. Clin. Nurs. 2017, 26, 5179–5190. [Google Scholar] [CrossRef]
- Lin, Y.H. Effects of thermal therapy in improving the passive range of knee motion: Comparison of cold and superficial heat applications. Clin. Rehabil. 2003, 17, 618–623. [Google Scholar] [CrossRef]
- Fathi Azar, E.; Mirzaie, H.; Jamshidian, E.; Hojati, E. Effectiveness of perceptual-motor exercises and physical activity on the cognitive, motor, and academic skills of children with learning disorders: A systematic review. Child. Care Health Dev. 2023, 49, 1006–1018. [Google Scholar] [CrossRef] [PubMed]
- Sharifi, M.; Nodehi, D.; Bazgir, B. Physical activity and psychological adjustment among retirees: A systematic review. BMC Public Health 2023, 23, 194. [Google Scholar] [CrossRef] [PubMed]
- Malm, C.; Jakobsson, J.; Isaksson, A. Physical Activity and Sports-Real Health Benefits: A Review with Insight into the Public Health of Sweden. Sports 2019, 7, 127. [Google Scholar] [CrossRef]
- Conn, J.M. Sports and recreation related injury episodes in the US population, 1997–1999. Inj. Prev. 2003, 9, 117–123. [Google Scholar] [CrossRef] [PubMed]
- Emery, C.A.; Pasanen, K. Current trends in sport injury prevention. Best Pract. Res. Clin. Rheumatol. 2019, 33, 3–15. [Google Scholar] [CrossRef]
- Pasanen, K.; Parkkari, J.; Pasanen, M.; Kannus, P. Effect of a neuromuscular warm-up programme on muscle power, balance, speed and agility: A randomised controlled study. Br. J. Sports Med. 2009, 43, 1073–1078. [Google Scholar] [CrossRef] [PubMed]
- LaBella, C.R.; Huxford, M.R.; Grissom, J.; Kim, K.Y.; Peng, J.; Christoffel, K.K. Effect of Neuromuscular Warm-up on Injuries in Female Soccer and Basketball Athletes in Urban Public High Schools. Arch. Pediatr. Adolesc. Med. 2011, 165. [Google Scholar] [CrossRef] [PubMed]
- Petrofsky, J.S.; Laymon, M.; Lee, H. Effect of heat and cold on tendon flexibility and force to flex the human knee. Med. Sci. Monit. 2013, 19, 661–667. [Google Scholar] [PubMed]
- McGowan, C.J.; Pyne, D.B.; Thompson, K.G.; Rattray, B. Warm-Up Strategies for Sport and Exercise: Mechanisms and Applications. Sports Med. 2015, 45, 1523–1546. [Google Scholar] [CrossRef]
- Bishop, D. Warm up I: Potential mechanisms and the effects of passive warm up on exercise performance. Sports Med. 2003, 33, 439–454. [Google Scholar] [CrossRef]
- Kim, K.; Monroe, J.C.; Gavin, T.P.; Roseguini, B.T. Local Heat Therapy to Accelerate Recovery After Exercise-Induced Muscle Damage. Exerc. Sport Sci. Rev. 2020, 48, 163–169. [Google Scholar] [CrossRef] [PubMed]
- Heinonen, I.; Brothers, R.M.; Kemppainen, J.; Knuuti, J.; Kalliokoski, K.K.; Crandall, C.G. Local heating, but not indirect whole body heating, increases human skeletal muscle blood flow. J. Appl. Physiol. 2011, 111, 818–824. [Google Scholar] [CrossRef] [PubMed]
- Fradkin, A.J.; Zazryn, T.R.; Smoliga, J.M. Effects of warming-up on physical performance: A systematic review with meta-analysis. J. Strength. Cond. Res. 2010, 24, 140–148. [Google Scholar] [CrossRef] [PubMed]
- Warren, C.G.; Lehmann, J.F.; Koblanski, J.N. Heat and stretch procedures: An evaluation using rat tail tendon. Arch. Phys. Med. Rehabil. 1976, 57, 122–126. [Google Scholar] [PubMed]
- Oranchuk, D.J.; Flattery, M.R.; Robinson, T.L. Superficial heat administration and foam rolling increase hamstring flexibility acutely; with amplifying effects. Phys. Ther. Sport 2019, 40, 213–217. [Google Scholar] [CrossRef] [PubMed]
- Nakano, J.; Yamabayashi, C.; Scott, A.; Reid, W.D. The effect of heat applied with stretch to increase range of motion: A systematic review. Phys. Ther. Sport 2012, 13, 180–188. [Google Scholar] [CrossRef]
- Wang, Y.; Lu, H.; Li, S.; Zhang, Y.; Yan, F.; Huang, Y.; Chen, X.; Yang, A.; Han, L.; Ma, Y. Effect of cold and heat therapies on pain relief in patients with delayed onset muscle soreness: A network meta-analysis. J. Rehabil. Med. 2022, 54, jrm00258. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zanoli, G.; Albarova-Corral, I.; Ancona, M.; Grattagliano, I.; Hotfiel, T.; Iolascon, G.; Krüger, K.; Rodríguez Maruri, G. Current Indications and Future Direction in Heat Therapy for Musculoskeletal Pain: A Narrative Review. Muscles 2024, 3, 212-223. https://doi.org/10.3390/muscles3030019
Zanoli G, Albarova-Corral I, Ancona M, Grattagliano I, Hotfiel T, Iolascon G, Krüger K, Rodríguez Maruri G. Current Indications and Future Direction in Heat Therapy for Musculoskeletal Pain: A Narrative Review. Muscles. 2024; 3(3):212-223. https://doi.org/10.3390/muscles3030019
Chicago/Turabian StyleZanoli, Gustavo, Isabel Albarova-Corral, Michele Ancona, Ignazio Grattagliano, Thilo Hotfiel, Giovanni Iolascon, Karsten Krüger, and Guillermo Rodríguez Maruri. 2024. "Current Indications and Future Direction in Heat Therapy for Musculoskeletal Pain: A Narrative Review" Muscles 3, no. 3: 212-223. https://doi.org/10.3390/muscles3030019
APA StyleZanoli, G., Albarova-Corral, I., Ancona, M., Grattagliano, I., Hotfiel, T., Iolascon, G., Krüger, K., & Rodríguez Maruri, G. (2024). Current Indications and Future Direction in Heat Therapy for Musculoskeletal Pain: A Narrative Review. Muscles, 3(3), 212-223. https://doi.org/10.3390/muscles3030019






