Waist Circumference Is an Anthropometric Parameter That Identifies Women with Metabolically Unhealthy Phenotypes
Abstract
:1. Introduction
2. Materials and Methods
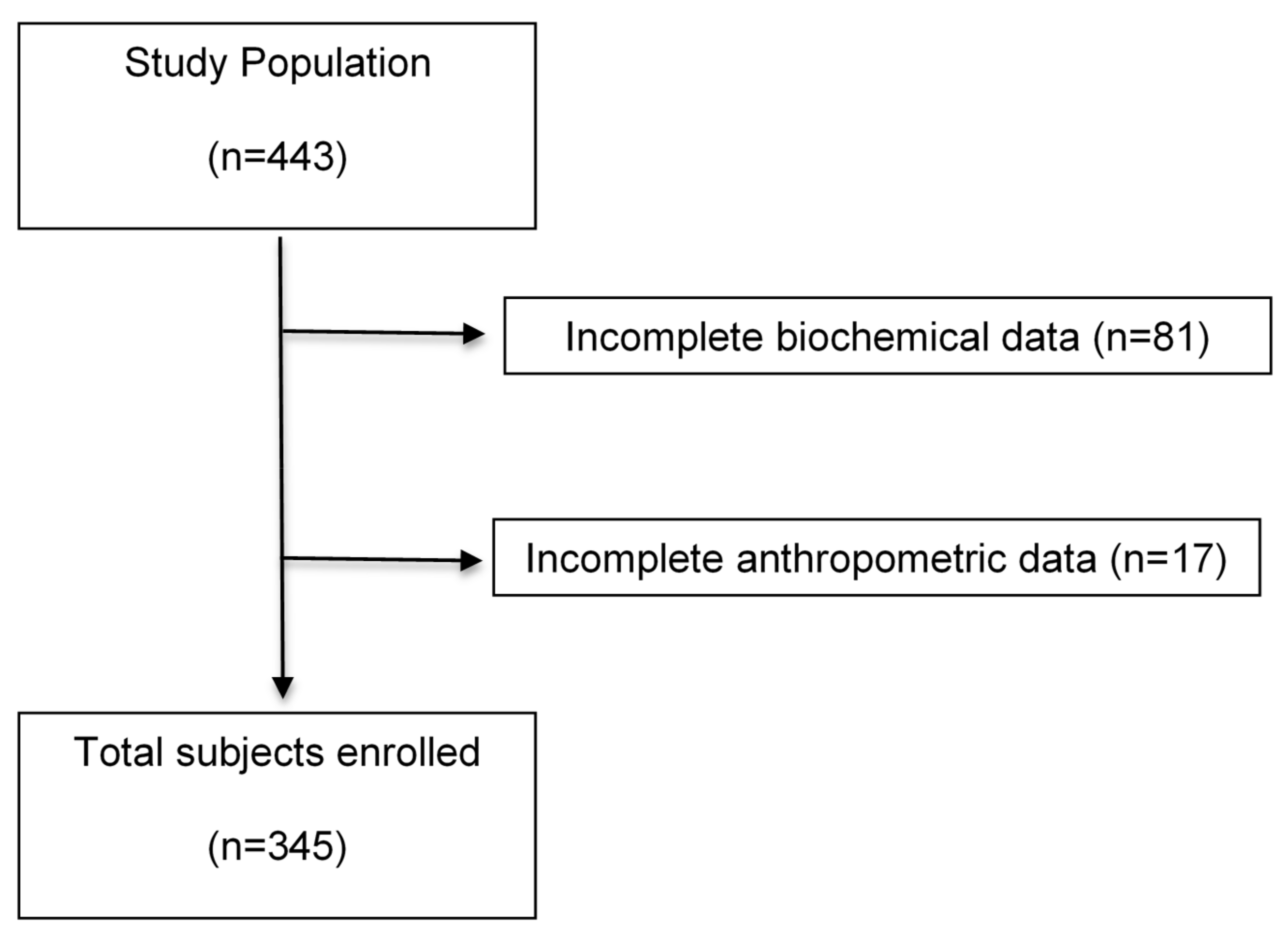
2.1. Study Population
2.2. Definition of the Metabolically Healthy Phenotype (MH) and Metabolically Unhealthy Phenotype (MUH)
2.3. Anthropometric Measurements
2.4. Biochemical Analysis
2.5. Statistical Analysis
3. Results
3.1. Prevalence of MH Phenotype
3.2. Demographic, Anthropometric, and Clinical Characteristics in MH and MUH Phenotypes
3.3. Biochemical Characteristics in MH and MUH Phenotypes
3.4. ROC Curve to Predict the MUH Phenotype Based on Anthropometric Measurements
3.5. Risk Factors Associated with the MUH Phenotype
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Obesity and Overweight. Available online: http://www.who.int/mediacentre/factsheets/fs311/en/ (accessed on 19 December 2015).
- Encuesta Nacional de Salud y Nutrición 2016. Available online: http://ensanut.insp.mx/ensanut2016/descarga_bases.php#.WoyFH-ejnIU (accessed on 27 December 2017). (In Spanish).
- Navarro, E.; Funtikova, A.N.; Fíto, M.; Schröder, H. Can metabolically healthy obesity be explained by diet, genetics, and inflammation? Mol. Nutr. Food Res. 2015, 59, 75–93. [Google Scholar] [CrossRef] [PubMed]
- Karelis, A.D.; Faraj, M.; Bastard, J.-P.; St-Pierre, D.H.; Brochu, M.; Prud’homme, D.; Rabasa-Lhoret, R. The metabolically healthy but obese individual presents a favorable inflammation profile. J. Clin. Endocrinol. Metab. 2005, 90, 4145–4150. [Google Scholar] [CrossRef] [PubMed]
- Bell, J.A.; Kivimaki, M.; Hamer, M. Metabolically healthy obesity and risk of incident type 2 diabetes: A meta-analysis of prospective cohort studies. Obes. Rev. 2014, 15, 504–515. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Samouda, H.; Ruiz-Castell, M.; Karimi, M.; Bocquet, V.; Kuemmerle, A.; Chioti, A.; Dadoun, F.; Stranges, S. Metabolically healthy and unhealthy weight statuses, health issues and related costs: Findings from the 2013-2015 European Health Examination Survey in Luxembourg. Diabetes Metab. 2017. [Google Scholar] [CrossRef] [PubMed]
- Primeau, V.; Coderre, L.; Karelis, A.D.; Brochu, M.; Lavoie, M.-E.; Messier, V.; Sladek, R.; Rabasa-Lhoret, R. Characterizing the profile of obese patients who are metabolically healthy. Int. J. Obes. 2011, 35, 971–981. [Google Scholar] [CrossRef] [PubMed]
- Lynch, L.A.; O’Connell, J.M.; Kwasnik, A.K.; Cawood, T.J.; O’Farrelly, C.; O’Shea, D.B. Are natural killer cells protecting the metabolically healthy obese patient? Obesity 2009, 17, 601–605. [Google Scholar] [CrossRef] [PubMed]
- Aguilar-Salinas, C.A.; García, E.G.; Robles, L.; Riaño, D.; Ruiz-Gomez, D.G.; García-Ulloa, A.C.; Melgarejo, M.A.; Zamora, M.; Guillen-Pineda, L.E.; Mehta, R.; et al. High adiponectin concentrations are associated with the metabolically healthy obese phenotype. J. Clin. Endocrinol. Metab. 2008, 93, 4075–4079. [Google Scholar] [CrossRef] [PubMed]
- Karelis, A.D.; Brochu, M.; Rabasa-Lhoret, R. Can we identify metabolically healthy but obese individuals (MHO)? Diabetes Metab. 2004, 30, 569–572. [Google Scholar] [CrossRef]
- Mihalache, L.; Graur, L.I.; Popescu, D.S.; Niţă, O.; Graur, M. Anthropometric parameters-predictive factors for cardio-metabolic diseases. Rev. Med. Chir. Soc. Med. Nat. Iasi 2012, 116, 794–798. [Google Scholar] [PubMed]
- Shen, W.; Punyanitya, M.; Chen, J.; Gallagher, D.; Albu, J.; Pi-Sunyer, X.; Lewis, C.E.; Gunfeld, C.; Heshka, S.; Heymsfield, S.B. Waist circumference correlates with metabolic syndrome indicators better than percentage. Fat. Obes. 2006, 14, 727–736. [Google Scholar] [CrossRef] [PubMed]
- Ahl, S.; Guenther, M.; Zhao, S.; James, R.; Marks, J.; Szabo, A.; Kidambi, S. Adiponectin levels differentiate metabolically healthy vs. unhealthy among obese and nonobese white individuals. J. Clin. Endocrinol. Metab. 2015, 100, 4172–4180. [Google Scholar] [CrossRef] [PubMed]
- What’s At-Risk or Heavy Drinking? Available online: https://www.rethinkingdrinking.niaaa.nih.gov/How-much-is-too-much/Is-your-drinking-pattern-risky/Whats-At-Risk-Or-Heavy-Drinking.aspx (accessed on 27 January 2016).
- Boonchaya-anant, P.; Apovian, C.M. Metabolically healthy obesity--does it exist? Curr. Atheroscler Rep. 2014, 16. [Google Scholar] [CrossRef] [PubMed]
- Alberti, K.G.M.M.; Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z.; Cleeman, J.I.; Donato, K.A.; Fruchart, J.C.; James, W.P.; Loria, C.M.; Smith, S.C., Jr.; et al. Harmonizing the metabolic syndrome: A joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009, 120, 1640–1645. [Google Scholar] [CrossRef] [PubMed]
- Matthews, D.R.; Hosker, J.P.; Rudenski, A.S.; Naylor, B.A.; Treacher, D.F.; Turner, R.C. Homeostasis model assessment: Insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985, 28, 412–419. [Google Scholar] [CrossRef] [PubMed]
- Friedewald, W.T.; Levy, R.I.; Fredrickson, D.S. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin. Chem. 1972, 18, 499–502. [Google Scholar] [PubMed]
- Roberts, W.C. The Friedewald-Levy-Fredrickson formula for calculating low-density lipoprotein cholesterol, the basis for lipid-lowering therapy. Am. J. Cardiol. 1988, 62, 345–346. [Google Scholar] [CrossRef]
- Zhu, N.; Pankow, J.S.; Ballantyne, C.M.; Couper, D.; Hoogeveen, R.C.; Pereira, M.; Duncan, B.B.; Schmidt, M.I. High-molecular-weight adiponectin and the risk of type 2 diabetes in the ARIC study. J. Clin. Endocrinol. Metab. 2010, 95, 5097–5104. [Google Scholar] [CrossRef] [PubMed]
- Wildman, R.P.; Muntner, P.; Reynolds, K.; McGinn, A.P.; Rajpathak, S.; Wylie-Rosett, J.; Sowers, M.R. The obese without cardiometabolic risk factor clustering and the normal weight with cardiometabolic risk factor clustering: Prevalence and correlates of 2 phenotypes among the US population (NHANES 1999–2004). Arch. Intern. Med. 2008, 168, 1617–1624. [Google Scholar] [CrossRef] [PubMed]
- Isasi, C.R.; Parrinello, C.M.; Ayala, G.X.; Delamater, A.M.; Perreira, K.M.; Daviglus, M.L.; Elder, J.P.; Marchante, A.N.; Bangdiwala, S.I.; Van Horn, L.; et al. Sex differences in cardiometabolic risk factors among Hispanic/Latino youth. J. Pediatr. 2016, 176, 121–127. [Google Scholar] [CrossRef] [PubMed]
- Goday, A.; Calvo, E.; Vázquez, L.A.; Caveda, E.; Margallo, T.; Catalina-Romero, C.; Reviriego, J. Prevalence and clinical characteristics of metabolically healthy obese individuals and other obese/non-obese metabolic phenotypes in a working population: Results from the Icaria study. BMC Public Health 2016. [Google Scholar] [CrossRef] [PubMed]
- Peppa, M.; Koliaki, C.; Papaefstathiou, A.; Garoflos, E.; Katsilambros, N.; Raptis, S.A.; Hadjidakis, D.I.; Dimitriadis, G.D. Body composition determinants of metabolic phenotypes of obesity in nonobese and obese postmenopausal women. Obesity 2013, 21, 1807–1814. [Google Scholar] [CrossRef] [PubMed]
- Chang, C.-S.; Lu, Y.-J.; Chang, H.-H.; Hsu, S.-H.; Kuo, P.-H.; Shieh, C.-C.; Yao, W.J.; Hsu, M.C.; Young, K.C.; Lin, W.Y.; et al. Role of adiponectin gene variants, adipokines and hydrometry-based percent body fat in metabolically healthy and abnormal obesity. Obes. Res. Clin. Pract. 2016. [Google Scholar] [CrossRef] [PubMed]
- Camhi, S.M.; Katzmarzyk, P.T. Differences in body composition between metabolically healthy obese and metabolically abnormal obese adults. Int. J. Obes. 2014, 38, 1142–1145. [Google Scholar] [CrossRef] [PubMed]
- Samaropoulos, X.F.; Hairston, K.G.; Anderson, A.; Haffner, S.M.; Lorenzo, C.; Montez, M.; Norris, J.M.; Scherzinger, A.L.; Chen, Y.D.; Wagenknecht, L.E. A metabolically healthy obese phenotype in hispanic participants in the IRAS family study. Obesity 2013, 21, 2303–2309. [Google Scholar] [CrossRef] [PubMed]
- Virtue, S.; Vidal-Puig, A. Adipose tissue expandability, lipotoxicity and the Metabolic Syndrome—An allostatic perspective. Biochim. Biophys. Acta 2010, 1801, 338–349. [Google Scholar] [CrossRef] [PubMed]
- Cuthbertson, D.J.; Steele, T.; Wilding, J.P.; Halford, J.C.; Harrold, J.A.; Hamer, M.; Karpe, F. What have human experimental overfeeding studies taught us about adipose tissue expansion and susceptibility to obesity and metabolic complications? Int. J. Obes. 2017, 41, 853–865. [Google Scholar] [CrossRef] [PubMed]
- Janssen, I.; Heymsfield, S.B.; Allison, D.B.; Kotler, D.P.; Ross, R. Body mass index and waist circumference independently contribute to the prediction of nonabdominal, abdominal subcutaneous, and visceral fat. Am. J. Clin. Nutr. 2002, 75, 683–688. [Google Scholar] [CrossRef] [PubMed]
- Wells, J.C.K.; Fewtrell, M.S. Measuring body composition. Arch. Dis. Child. 2006, 91, 612–617. [Google Scholar] [CrossRef] [PubMed]
- Harris, T.B.; Visser, M.; Everhart, J.; Cauley, J.; Tylavsky, F.; Fuerst, T.; Zamboni, M.; Taaffe, D.; Resnick, H.E.; Scherzinger, A.; et al. Waist circumference and sagittal diameter reflect total body fat better than visceral fat in older men and women: The Health, Aging and Body Composition Study. Ann. N. Y. Acad. Sci. 2000, 904, 462–473. [Google Scholar] [CrossRef] [PubMed]
- Zhang, N.; Chen, Y.; Guo, X.; Sun, G.; Sun, Y. The prevalence and predictors of metabolically healthy obesity in obese rural population of China: A cross-sectional study. Psychol. Health Med. 2017, 22, 303–309. [Google Scholar] [CrossRef] [PubMed]
- Phillips, C.M.; Dillon, C.; Harrington, J.M.; McCarthy, V.J.C.; Kearney, P.M.; Fitzgerald, A.P.; Perry, I.J. Defining metabolically healthy obesity: Role of dietary and lifestyle factors. PLoS ONE 2013. [Google Scholar] [CrossRef] [PubMed]
- Yoo, H.K.; Choi, E.Y.; Park, E.W.; Cheong, Y.-S.; Bae, R.A. Comparison of metabolic characteristics of metabolically healthy but obese (MHO) middle-aged men according to different criteria. Korean J. Fam. Med. 2013, 34, 19–26. [Google Scholar] [CrossRef] [PubMed]
- Doumatey, A.P.; Bentley, A.R.; Zhou, J.; Huang, H.; Adeyemo, A.; Rotimi, C.N. Paradoxical hyperadiponectinemia is associated with the metabolically healthy obese (MHO) phenotype in African Americans. J. Endocrinol. Metab. 2012, 2, 51–65. [Google Scholar] [CrossRef] [PubMed]
- Berezina, A.; Belyaeva, O.; Berkovich, O.; Baranova, E.; Karonova, T.; Bazhenova, E.; Brovin, D.; Grineva, E.; Shlyakhto, E. Prevalence, risk factors, and genetic traits in metabolically healthy and unhealthy obese individuals. Biomed. Res. Int. 2015. [Google Scholar] [CrossRef] [PubMed]
- Aprahamian, T.R.; Sam, F. Adiponectin in cardiovascular inflammation and obesity. Int. J. Inflam. 2011. [Google Scholar] [CrossRef] [PubMed]
- Heid, I.M.; Henneman, P.; Hicks, A.; Coassin, S.; Winkler, T.; Aulchenko, Y.S.; Fuchsberger, C.; Song, K.; Hivert, M.F.; Waterworth, D.M.; et al. Clear detection of ADIPOQ locus as the major gene for plasma adiponectin: Results of genome-wide association analyses including 4659 European individuals. Atherosclerosis 2010, 208, 412–420. [Google Scholar] [CrossRef] [PubMed]
- Vasseur, F.; Helbecque, N.; Dina, C.; Lobbens, S.; Delannoy, V.; Gaget, S.; Boutin, P.; Vaxillaire, M.; Leprête, F.; Dupont, S.; et al. Single-nucleotide polymorphism haplotypes in the both proximal promoter and exon 3 of the APM1 gene modulate adipocyte-secreted adiponectin hormone levels and contribute to the genetic risk for type 2 diabetes in French Caucasians. Hum. Mol. Genet. 2002, 11, 2607–2614. [Google Scholar] [CrossRef] [PubMed]
- Lim, K.I.; Yang, S.J.; Kim, T.N.; Yoo, H.J.; Kang, H.J.; Song, W.; Baik, S.H.; Choi, D.S.; Choi, K.M. The association between the ratio of visceral fat to thigh muscle area and metabolic syndrome: The Korean Sarcopenic Obesity Study (KSOS). Clin. Endocrinol. 2010, 73, 588–594. [Google Scholar] [CrossRef] [PubMed]
- Kim, T.N.; Park, M.S.; Yang, S.J.; Yoo, H.J.; Kang, H.J.; Song, W.; Seo, J.A.; Kim, S.G.; Kim, N.H.; Baik, S.H.; et al. Body size phenotypes and low muscle mass: The Korean sarcopenic obesity study (KSOS). J. Clin. Endocrinol. Metab. 2013, 98, 811–817. [Google Scholar] [CrossRef] [PubMed]
- Yu, N.; Ruan, Y.; Gao, X.; Sun, J. Systematic Review and meta-analysis of randomized, controlled trials on the effect of exercise on serum leptin and adiponectin in overweight and obese individuals. Horm. Metab. Res. 2017, 49, 164–173. [Google Scholar] [CrossRef] [PubMed]
| Variables | MH-NW | MUH-NW | p | MH-OW | MUH-OW | p | MH-O | MUH-O | p | * p |
|---|---|---|---|---|---|---|---|---|---|---|
| Demographic, anthropometric and clinical characteristics | ||||||||||
| Sex (M/F) | 23/70 | 12/28 | 0.527 | 15/42 | 22/28 | 0.067 | 3/17 | 15/70 | 1.000 | |
| Age (year) | 32.0 ± 10.7 a | 38.3 ± 12.4 | 0.005 | 37.7 ± 12.3 b | 37.8 ± 10.7 | 0.966 | 39.9 ± 13.2 b | 39.6 ± 10.8 | 0.936 | 0.005 |
| Weight (kg) | 59.1 ± 8.4 a | 63.5 ± 6.2 | 0.004 | 71.1 ± 8.4 b | 75.9 ± 8.8 | 0.006 | 84.6 ± 9.9 c | 93.2 ± 17.2 | 0.036 | <0.001 |
| BMI (kg/m2) | 21.9 ± 1.9 a | 23.1 ± 1.5 | <0.001 | 26.9 ±1.4 b | 27.2 ± 1.4 | 0.254 | 33.4 ± 2.4 c | 36.1 ± 5.4 | 0.001 | <0.001 |
| Protein mass (kg) | 11.2 ± 1.8 a | 11.5 ± 1.7 | 0.482 | 11.8 ± 2.2 a,b | 13.0 ± 2.5 | 0.033 | 12.4 ± 2.2 b | 13.5 ± 2.6 | 0.096 | 0.040 |
| Fat mass (kg) | 14.5 ± 4.3 a | 17.1 ± 3.5 | 0.001 | 23.6 ± 6.4 b | 23.6 ± 7.8 | 0.999 | 34.6 ± 6.6 c | 39.5 ± 11.3 | 0.067 | <0.001 |
| BFP (%) | 24.5 ± 6.3 a | 27.1 ± 5.8 | 0.026 | 32.4 ± 6.1 b | 30.3 ± 6.6 | 0.081 | 41.0 ± 6.7 c | 42.1 ± 6.6 | 0.492 | <0.001 |
| PM:FM ratio | 0.819 ± 0.342 a | 0.720 ± 0.273 | 0.045 | 0.544 ± 0.195 b | 0.574 ± 0.240 | 0.382 | 0.375 ± 0.126 c | 0.360 ± 0.102 | 0.562 | <0.001 |
| Waist (cm) | 74.8 ± 8.3 a | 80.8 ± 7.3 | 0.000 | 87.0 ± 7.9 b | 91.6 ± 7.1 | 0.002 | 100.5 ± 6.9 c | 107.7 ± 12.4 | 0.001 | <0.001 |
| Males | 83.2 ± 7.7 a | 86.3 ± 5.8 | 0.228 | 94.5 ± 7.0 b | 95.6 ± 5.8 | 0.595 | 103.0 ± 11.3 c | 114.9 ± 11.9 | 0.192 | <0.001 |
| Females | 72.3 ± 6.8 a | 77.7 ± 6.0 | 0.001 | 84.0 ± 6.3 b | 88.6 ± 6.4 | 0.003 | 99.6 ± 6.1 c | 106.2 ± 11.9 | 0.003 | <0.001 |
| Hip (cm) | 95.2 ± 4.8 a | 97.5 ± 3.9 | 0.011 | 103.7 ± 4.6 b | 104.8 ± 4.3 | 0.199 | 114.0 ± 6.7 c | 121.2 ± 15.0 | 0.062 | <0.001 |
| WHR | 0.78 ± 0.08 a | 0.83 ± 0.08 | 0.002 | 0.84 ± 0.08 b | 0.88 ± 0.07 | 0.019 | 0.88 ± 0.08 b | 0.88 ± 0.07 | 0.961 | <0.001 |
| SBP (mmHg) | 108.1 ± 12.6 a | 119.1 ± 17.9 | <0.001 | 110.3 ± 11.2 a,b | 121.3 ± 16.5 | <0.001 | 116.4 ± 12.0 b | 120.7 ± 13.9 | 0.204 | 0.021 |
| DBP (mmHg) | 68.1 ± 7.4 a | 72.6 ± 8.9 | 0.003 | 69.7 ± 7.9 a | 79.3 ± 11.0 | <0.001 | 75.3 ± 8.7 b | 77.9 ± 15.3 | 0.471 | 0.001 |
| Biochemical characteristics | ||||||||||
| Triglycerides (mg/dL) | 93.5 ± 30.1 a | 172.8 ± 107.3 | <0.001 | 109.3 ± 40.9 b | 205.2 ± 76.7 | <0.001 | 96.3 ± 26.8 a,b | 181.9 ± 88.2 | <0.001 | 0.021 |
| Total cholesterol (mg/dL) | 174.6 ± 29.8 | 193.6 ± 41.4 | 0.012 | 183.2 ± 39.3 | 188.7 ± 34.8 | 0.451 | 190.4 ± 32.9 | 193.9 ± 36.1 | 0.702 | 0.104 |
| HDL-c (mg/dL) | 52.1 ± 12.2 a | 40.3 ± 7.7 | <0.001 | 48.0 ± 11.0 b | 38.4 ± 12.0 | <0.001 | 46.5 ± 10.7 a,b | 38.0 ± 7.1 | 0.003 | 0.039 |
| LDL-c (mg/dL) | 105.9 ± 27.5 a | 115.4 ± 32.8 | 0.094 | 114.0 ± 34.2 a,b | 109.5 ± 30.6 | 0.484 | 125.2 ± 30.6 b | 120.2 ± 31.7 | 0.525 | 0.026 |
| VLDL-c (mg/dL) | 18.7 ± 6.1 a | 34.5 ± 21.4 | <0.001 | 21.8 ± 8.2 b | 40.4 ± 14.7 | <0.001 | 18.6 ± 5.4 a,b | 35.4 ± 15.7 | 0.000 | 0.020 |
| Glucose (mg/dL) | 83.2 ± 7.2 a | 96.6 ± 59.2 | 0.007 | 84.2 ± 8.8 a,b | 91.3 ± 10.4 | <0.001 | 88.7 ± 8.3 b | 98.0 ± 12.5 | 0.002 | 0.019 |
| Insulin (μU/mL) | 7.4 ± 4.5 | 13.3 ± 9.9 | 0.001 | 7.1 ± 3.6 | 13.7 ± 8.3 | <0.001 | 8.7 ± 3.7 | 17.5 ± 8.8 | 0.000 | 0.315 |
| HOMA-IR | 1.5 ± 1.0 | 3.0 ± 2.3 | <0.001 | 1.5 ± 0.9 | 3.1 ± 2.0 | <0.001 | 1.9 ± 0.7 | 4.3 ± 2.3 | 0.000 | 0.272 |
| CRP (mg/L) | 4.8 ± 5.0 a | 4.7 ± 4.0 | 0.369 | 8.0 ± 7.3 b | 10.9 ± 11.4 | 0.259 | 14.5 ± 9.2 c | 12.6 ± 8.5 | 0.519 | <0.001 |
| Adiponectin HMW (μg/mL) | 4.3 ± 3.1 | 3.8 ± 2.6 | 0.181 | 3.8 ± 2.0 | 2.3 ± 1.5 | <0.001 | 3.4 ± 2.3 | 2.6 ± 1.8 | 0.124 | 0.189 |
| Variable: Waist Circumference in Men | MUH-NW | MUH-OW | MUH-O |
| AUC ± SE | 0.647 ± 0.10 | 0.530 ± 0.10 | 0.744 ± 0.21 |
| 95% CI | 0.458–0.835 | 0.329–0.730 | 0.325–1.00 |
| p value | 0.156 | 0.766 | 0.193 |
| Sensibility | 71.4% | 35.7% | 66.7% |
| Specificity | 61.5% | 73.9% | 100% |
| Cut-off point (cm) | >85.5 | >92.5 | >99.0 |
| Variable: Waist Circumference in Women | MUH-NW | MUH-OW | MUH-O |
| AUC ± SE | 0.738 ± 0.05 | 0.692 ± 0.06 | 0.690 ± 0.07 |
| T95% CI | 0.633–0.842 | 0.567–0.816 | 0.552–0.807 |
| p value | <0.001 | 0.006 | 0.030 |
| Sensibility | 64.8% | 75.0% | 66.7% |
| Specificity | 76.9% | 56.7% | 69.0% |
| Cut-off point (cm) | >73.8 | >87.3 | >99.3 |
| Variable | B | p | OR | 95% CI |
|---|---|---|---|---|
| R2 Nagelkerke = 28.7% | ||||
| Sex (M = 0, F = 1) | −1.345 | 0.006 | 0.261 | 0.100–0.680 |
| Age (years) | ||||
| 18–29 | 0.011 | |||
| 30–39 | 1.167 | 0.002 | 3.212 | 1.533–6.728 |
| 40–49 | 0.745 | 0.045 | 2.214 | 1.019–4.812 |
| ≥50 | 0.911 | 0.028 | 2.486 | 1.101–5.615 |
| PM:FM ratio | −3.556 | 0.000 | 0.029 | 0.006–0.132 |
| Hypoadiponectinemia | 0.745 | 0.017 | 2.106 | 1.143–3.880 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Torres-Castillo, N.; Campos-Perez, W.; Gonzalez-Becerra, K.; Hernandez-Cañaveral, I.; Vizmanos, B.; Muñoz-Valle, J.; Martinez-Lopez, E. Waist Circumference Is an Anthropometric Parameter That Identifies Women with Metabolically Unhealthy Phenotypes. Nutrients 2018, 10, 447. https://doi.org/10.3390/nu10040447
Torres-Castillo N, Campos-Perez W, Gonzalez-Becerra K, Hernandez-Cañaveral I, Vizmanos B, Muñoz-Valle J, Martinez-Lopez E. Waist Circumference Is an Anthropometric Parameter That Identifies Women with Metabolically Unhealthy Phenotypes. Nutrients. 2018; 10(4):447. https://doi.org/10.3390/nu10040447
Chicago/Turabian StyleTorres-Castillo, Nathaly, Wendy Campos-Perez, Karina Gonzalez-Becerra, Iván Hernandez-Cañaveral, Barbara Vizmanos, José Muñoz-Valle, and Erika Martinez-Lopez. 2018. "Waist Circumference Is an Anthropometric Parameter That Identifies Women with Metabolically Unhealthy Phenotypes" Nutrients 10, no. 4: 447. https://doi.org/10.3390/nu10040447
APA StyleTorres-Castillo, N., Campos-Perez, W., Gonzalez-Becerra, K., Hernandez-Cañaveral, I., Vizmanos, B., Muñoz-Valle, J., & Martinez-Lopez, E. (2018). Waist Circumference Is an Anthropometric Parameter That Identifies Women with Metabolically Unhealthy Phenotypes. Nutrients, 10(4), 447. https://doi.org/10.3390/nu10040447







