Subcutaneous Nodules as Manifestations of Systemic Disease
Abstract
1. Introduction
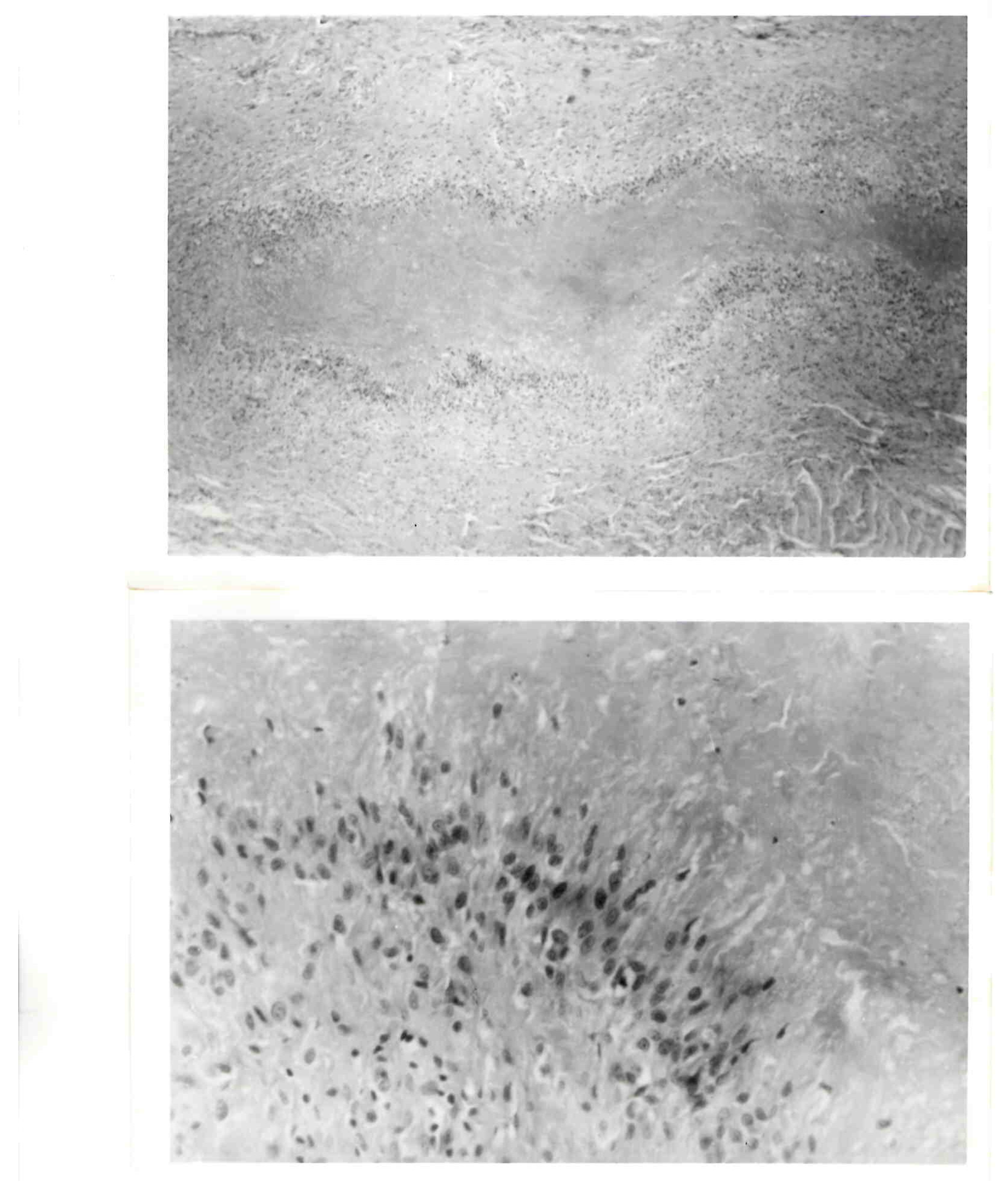
2. Rheumatoid Nodules
3. Pseudorheumatoid Nodules
4. Differential Considerations
5. Erythema Nodosum
6. Granuloma Annulare
7. Gottron’s Papules
8. Necrobiotic Nodules
9. Myositis Ossificans
10. Pancreatic-Disease-Related Nodules
11. Vasculitis/Angiitis-Related Nodules
12. Metabolic-Disease-Derived Nodules
12.1. Storage Diseases
12.2. Necrobiosis Lipoidica Diabeticorum
12.3. Gout
13. Infection—Related Nodules
13.1. Disease Specificity
13.2. Rheumatic Fever
13.3. Lyme Disease
14. Malignancy-Related Nodules
15. Dermatologic-Disease Related Nodules
16. Lymphadenopathy
17. Denouement
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Moore, C.P.; Wilkins, R.F. The subcutaneous nodule: Its significance in the diagnosis of rheumatic disease. Semin. Arthritis Rheum. 1977, 7, 63–79. [Google Scholar] [CrossRef] [PubMed]
- Bywaters, E.G.L. A variant of rheumatoid arthritis characterized by recurrent digital pad nodules and palmar fasciitis, closely resembling palindromic rheumatism. Ann. Rheum. Dis. 1949, 8, 2–30. [Google Scholar] [CrossRef] [PubMed]
- Ganda, O.P.; Caplan, H.I. Rheumatoid disease without joint involvement. JAMA 1974, 228, 338–339. [Google Scholar] [CrossRef] [PubMed]
- Highton, J.; Hessian, P.A.; Stamp, L. The rheumatoid nodule: Peripheral or central to rheumatoid arthritis? Rheumatology 2007, 46, 1385–1387. [Google Scholar] [CrossRef]
- Kaye, B.R.; Kaye, R.L.; Bobrove, A. Rheumatoid nodules: Review of the spectrum of associated conditions and proposal of a new classification, with a report of four seronegative cases. Am. J. Med. 1984, 76, 279–292. [Google Scholar] [CrossRef]
- Kim, S.; Parker, W.L.; Beckenbaugh, R.D. Atypical rheumatoid nodules: A possible precursor to a rheumatoid variant in a rheumatoid-factor-negative patient. Hand 2009, 4, 62–65. [Google Scholar] [CrossRef] [PubMed]
- MacKenzie, J.D.; Karasick, D. Imaging of rheumatoid arthritis. In Imaging of Arthritis and Metabolic Bone Disease; Weissman, B.N., Ed.; Elsevier: Amsterdam, The Netherlands, 2009; pp. 340–364. [Google Scholar]
- Nyhäll-Wåhlin, B.M.; Jacobsson, L.T.; Petersson, I.F.; Turesson, C. Smoking is a strong risk factor for rheumatoid nodules in early rheumatoid arthritis. Ann. Rheum. Dis. 2006, 65, 601–606. [Google Scholar] [CrossRef] [PubMed]
- Chua-Aguilera, C.J.; Möller, B.; Yawalkar, N. Skin manifestations of rheumatoid arthritis, juvenile idiopathic arthritis, and spondyloarthritides. Clin. Rev. Allergy Immunol. 2017, 53, 371–393. [Google Scholar] [CrossRef] [PubMed]
- Tilstra, J.S.; Lienesch, D.W. Rheumatoid Nodules. Dermatol. Clin. Granulomatous Disord. Adult Skin. 2015, 33, 361–371. [Google Scholar] [CrossRef]
- Wisnieski, J.J.; Askari, A.D. Rheumatoid nodulosis: A relatively benign rheumatoid variant. Arch. Intern. Med. 1981, 141, 615–619. [Google Scholar] [CrossRef]
- Bang, S.; Kim, Y.; Jang, K.; Paik, S.S.; Shin, S.J. Clinicopathologic features of rheumatoid nodules: A retrospectiveanalysis. Clin. Rheum. 2019, 38, 3041–3048. [Google Scholar] [CrossRef] [PubMed]
- Ziff, M. The rheumatoid nodule. Arthritis Rheum. 1990, 33, 761–767. [Google Scholar] [CrossRef]
- De Stefano, L.; Guerini, M.; Pelizza, J.; Ferracane, G.; Piccin, V.; Montecucco, C.; Bugatti, S. A case of a rheumatoid nodule on the aortic valve in a patient with rheumatoid arthritis in sustained remission with anti-TNFα. Scand. J. Rheumatol. 2023, 52, 577–579. [Google Scholar] [CrossRef]
- Lamya, W.A.; Syed, A.; Mojieb, A.-H.; Abdullah, A.-S.; Wasim, F.R. Unusual location of rheumatoid nodule case report. Ortho. Rheum. Open Access J. 2020, 16, 555939. [Google Scholar] [CrossRef]
- Patel, R.; Nand, R.; Sunderamoorthy, D. Rheumatoid nodule presenting as an indeterminate soft tissue mass in the sole of the foot. J. Surg. Case Rep. 2022, 5, rjad278. [Google Scholar] [CrossRef]
- Porko, S.; Chowdhuri, C.; Barsagade, A.K.; Priya, S.; Mustafa, M. An unusual and rare location of I intra-articular rheumatoid nodule in the elbow joint. Cureus 2023, 15, e36747. [Google Scholar] [CrossRef]
- Rozin, A.; Yigla, M.; Guralnik, L.; Keidar, Z.; Vlodavsky, E.; Rozenbaum, M. Rheumatoid lung nodulosis and osteopathy associated with leflunomide therapy. Clin. Rheumatol. 2006, 25, 384–388. [Google Scholar] [CrossRef] [PubMed]
- Upile, T.; Jerjes, W.; Sipaul, F.; Singh, S.; Hopper, C.; Wright, A.; Sandison, A. Rheumatoid nodule of the thyrohyoid membrane: A case report. J. Med. Case Rep. 2007, 1, 123. [Google Scholar] [CrossRef]
- Takashima, S.; Ota, M. Methotrexate-induced nodulosis. Can. Med. Assoc. J. 2015, 187, E327. [Google Scholar] [CrossRef][Green Version]
- Watson, P.; Simler, N.; Screaton, N.; Lillicrap, M. Management of accelerated pulmonary nodulosis following etanercept therapy in a patient with rheumatoid arthritis. Rheumatology 2008, 47, 928–929. [Google Scholar] [CrossRef][Green Version]
- Palmeiro, A.G.; Lourenço, M.H.; Miroux-Catarino, A.; Crispim, I.; Branco, J.C.; Viana, I. Drug-induced accelerated nodulosis: Review of the literature. Int. J. Dermatol. 2023, 62, 432–440. [Google Scholar] [CrossRef]
- Campbell, R. Ultrasound of soft tissue masses. In Clinical Ultrasound, 3rd ed.; Allan, P.L., Baxter, G.M., Weston, M.J., Eds.; Churchill Livingstone: London, UK, 2011; pp. 1109–1125. [Google Scholar]
- Sahu, A.K.; Kataria, S.; Gandikota, G. Added value of high-resolution ultrasound and MRI in the evaluation of rheumatologic diseases. J. Ultrasoundgr. 2023, 23, e285–e298. [Google Scholar] [CrossRef]
- Fareez, F.; Moodley, J.; Popovic, S.; Lu, J.-Q. Rheumatoid nodules: A narrative review of histopathological progression and diagnostic consideration. Clin. Rheum. 2023, 42, 1753–1765. [Google Scholar] [CrossRef]
- Dubois, E.L.; Friou, G.J.; Chandor, S. Rheumatoid nodules and rheumatoid granulomas in systemic lupus erythematosus. JAMA 1972, 220, 515–518. [Google Scholar] [CrossRef]
- Erfurt-Berge, C.; Dissemond, J.; Schwede, K.; Seitz, A.T.; Al Ghazal, P.; Wollina, U.; Renner, R. Updated results of 100 patients on clinical features and therapeutic options in necrobiosis lipoidica in a retrospective multicentre study. Eur. J. Dermatol. 2015, 25, 595–601. [Google Scholar] [CrossRef]
- Burrington, J.D. “Pseudorheumatoid” nodules in children: Report of 10 cases. Pediatrics 1970, 45, 473–478. [Google Scholar] [CrossRef]
- Doussieere, M.; Danial, J.-M.; Barthomeuf, C.; Tesson, J.-R.; Beauvillain, Q.; Goeb, V. Diagnosis of Whipple’s disease with pseudorheumatoid nodules in a patient treated with biologics for rheumatoid polyarthritis. Rheum. Adv. Pract. 2023, 7, rkad002. [Google Scholar] [CrossRef]
- Lerma, E.W.H.; Medina, M.E.; Ramírez-Madrigal, M.A.; Troche, P.F.; Ledesma, J.F.; Hurtado, M.E. Diagnosis and treatment of Weber-Christian Disease for the first contact physician. Int. J. Med. Sci. Clin. Res. Stud. 2023, 3, 829–831. [Google Scholar] [CrossRef]
- Wang, M.X.; Segaran, N.; Bhalla, S.; Pickardt, P.J.; Lubner, M.G.; Katabathina, V.S.; Ganeshan, D. Tuberous sclerosis: Current update. RadioGraphics 2021, 41, 1–8. [Google Scholar] [CrossRef]
- Inamadar, A.C.; Adya, K.A. The rash with painful and erythematous nodules. Clin. Dermatol. 2019, 37, 129–135. [Google Scholar] [CrossRef]
- Plaza, J.A.; Prieto, V.G. Inflammatory skin conditions. In Modern Surgical Pathology, 2nd ed.; Weidner, N., Cote, R.J., Weiss, L.M., Eds.; Elsevier: Amsterdam, The Netherlands, 2009; pp. 1843–1889. [Google Scholar]
- Terziroli Beretta-Piccoli, B.; Mainetti, C.; Peeters, M.A.; Laffitte, E. Cutaneous granulomatosis: A Comprehensive review. Clin. Rev. Allergy Immunol. 2018, 54, 131–146. [Google Scholar] [CrossRef]
- Weedon, D. The granulomatous reaction pattern. In Weedon’s Skin Pathology, 3rd ed.; Churchill Livingstone: London, UK, 2010; pp. 169–194. [Google Scholar]
- Pérez-Garza, D.M.; Chavez-Alvarez, S.; Ocampo-Candiani, J.; Gomez-Flores, M. Erythema nodosum: A practical approach and diagnostic algorithm. Am. J. Clin. Dermatol. 2021, 22, 367–378. [Google Scholar] [CrossRef]
- Shafiei, M.; Zadeh, F.S.; Mansoori, B.; Pyle, H.; Agim, N.; Hinojosa, J.; Doinguez, A.; Thomas, C.; Chalian, M. Imaging more than skin-deep: Radiologic and dermatologic presentations of systemic disorders. Diagnostics 2022, 12, 2011. [Google Scholar] [CrossRef]
- Alghamdi, N.; Alamrie, R.M.; Alshafie, A.Y.; Almuhaidib, S.R. Delayed recurrent erythema nodosum following COVID-19 vaccine: A case report. Cureus 2023, 15, e42776. [Google Scholar] [CrossRef]
- Ma, Y.L.; Gal, A.; Koss, M.N. The pathology of pulmonary sarcoidosis: Update. Semin. Diagn. Pathol. 2007, 24, 150–161. [Google Scholar] [CrossRef]
- Felner, E.I.; Steinberg, J.B.; Weinberg, A.G. Subcutaneous granuloma annulare: A review of 47 cases. Pediatrics 1997, 100, 965–967. [Google Scholar] [CrossRef]
- Patterson, J.W. Rheumatoid nodule and subcutaneous granuloma annulare. Am. J. Dermatopathol. 1988, 10, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Aslani, F.S.; Pouraminaee, F.; Sepaskhah, M.; Ardakani, S.K. Clinicopathologic evaluation of granuloma annulare: Study of 136 Iranian cases, south of Iran. Skin. Health Dis. 2023, 3, e299. [Google Scholar] [CrossRef]
- Stolarczyk, A.; Bawany, F.; Hernandez, S.; Scott, G.A.; Cordisco, M.R. Characterizing granuloma annulare in 73 pediatric patients. Dermatol. Res. Pract. 2023, 2023, 9267263. [Google Scholar] [CrossRef] [PubMed]
- Cao, H.; Xia, Q.; Pan, M.; Zhao, X.; Li, X.; Shi, R.; Zhou, M.; Ding, X.; Kuwana, M.; Zheng, J. Gottron papules and Gottron sign with ulceration: A distinct clinical feature in a subset of patients with classic dermatomyositis and clinically amyopathic dermatomyositis. J. Rheumatol. 2016, 43, 1735–1742. [Google Scholar] [CrossRef] [PubMed]
- Wood, A.J.; Wagner, M.V.; Abbott, J.J.; Gobson, L.E. Necrobiotic xanthogranuloma. Arch. Derm. 2009, 145, 279–284. [Google Scholar] [CrossRef] [PubMed]
- Barfield, W.R.; Holmes, R.E.; Hartsock, L.A. Heterotopic Ossification in Trauma. Orthop. Clin. N. Am. 2017, 48, 35–46. [Google Scholar] [CrossRef] [PubMed]
- Pignolo, R.J.; Foley, K.L. Nonhereditary heterotopic ossification. Implications for injury, arthropy, and aging. Clin. Rev. Bone Miner. Metab. 2005, 3, 261–266. [Google Scholar] [CrossRef]
- Ramirez-Gonzalez, A.; Castañeda-de-la-Fuente, A.; Castro-Cervantes, V.; Pineda, C.; Sandoval, H.; Hidalgo-Bravo, A. Fibrodysplasia (myositis) ossifcans progressiva (FOP). Clin. Rheum. 2022, 41, 1929–1930. [Google Scholar] [CrossRef] [PubMed]
- Shore, E.M.; Kaplan, F.S. Insights from a rare genetic disorder of extra-skeletal bone formation, fibrodysplasia ossificans progressiva (FOP). Bone 2008, 43, 427–433. [Google Scholar] [CrossRef] [PubMed]
- Rongioletti, F.; Caputo, V. Pancreatic panniculitis. G. Ital. Dermatol. Venereol. 2013, 148, 419–425. [Google Scholar]
- Selvaraj, V.; Dapaah-Afriyie, K. A Tale of Two Ps: Panniculitis Secondary to Acute Pancreatitis. Cureus 2021, 13, e20504. [Google Scholar] [CrossRef] [PubMed]
- Zundler, S.; Erber, R.; Agaimy, A.; Hartmann, A.; Kiesewetter, F.; Strobel, D.; Neurath, M.F.; Wildner, D. Pancreatic panniculitis in a patient with pancreatic-type acinar cell carcinoma of the liver—Case report and review of literature. BMC Cancer 2016, 16, 130. [Google Scholar] [CrossRef]
- Amini, S.; Jari, M. Granulomatosis with polyangiitis misdiagnosed as IgA vasculitis in a child. Case Rep. Pediatr. 2023, 2023, 9950855. [Google Scholar] [CrossRef]
- Emmi, G.; Bettiol, A.; Gelain, E.; Bajema, I.M.; Berti, A.; Burns, S.; Cid, M.C.; Cohen Tervaert, J.W.; Cottin, V.; Durante, E.; et al. Evidence-Based Guideline for the diagnosis and management of eosinophilic granulomatosis with polyangiitis. Nat. Rev. Rheumatol. 2023, 19, 378–393. [Google Scholar] [CrossRef]
- Fernandes, S.S.; Carvalho, J.; Leite, S.; Alfonso, M.; Pinto, J.; Veloso, R.; Duarte, R.; Ferreira, E.; Fraga, J. Erythema induratum and chronic hepatitis C infection. J. Clin. Virol. 2009, 44, 333–336. [Google Scholar] [CrossRef] [PubMed]
- Hammad, H.; Krausz, H.J.; Barcan, M.; Fisher, S.; Edison, N.; Ziv, M. Adult Henoch-Schönlein purpura: Comprehensive assessment of demographic, clinical, and histopathological features as predictors for systemic involvement. Dermatology 2023, 239, 609–615. [Google Scholar] [CrossRef] [PubMed]
- Hatemi, G.; Seyahi, E.; Fresko, I.; Talarico, R.; Uçar, D.; Hamuryudan, V. Behçet’s syndrome: One year in review 2023. Clin. Exp. Rheumatol. 2023, 41, 1945–1954. [Google Scholar] [PubMed]
- Kabuto, M.; Nakanishi, G.; Kimura, H.; Tanaka, T.; Fujimoto, N. Erythema induratum (nodular vasculitis) associated with Takayasu arteritis. Eur. J. Dermatol. 2017, 27, 410–412. [Google Scholar] [CrossRef] [PubMed]
- Ashaolu, O.; Ng, S.; Smale, S.; Hughes, J. Multicentric reticulohistiocytosis–A rare and disabling disease. Clin. Case Rep. 2023, 11, e7846. [Google Scholar] [CrossRef] [PubMed]
- Hannah, W.B.; Derks, T.G.; Drumm, M.L.; Grünert, S.C.; Kishnani, P.S.; Vissing, J. Glycogen storage diseases. Nat. Rev. Dis. Primers 2023, 9, 46. [Google Scholar] [CrossRef]
- Joy, N.; Sobhanakumari, K.; Mathews, H. Waxy nodules: As a cutaneous diagnostic mirror of systemic disease mimicking rheumatoid arthritis. Indian Dermatol. Online J. 2023, 14, 723–725. [Google Scholar] [CrossRef] [PubMed]
- Wilcox, W.R. Lysosomal storage disorders: The need for better pediatric recognition and comprehensive care. J. Pediatr. 2004, 144, S3–S14. [Google Scholar] [CrossRef] [PubMed]
- Zielonka, M.; Garbade, S.F.; Kölker, S.; Hoffmann, G.F.; Ries, M. A cross-sectional quantitative analysis of the natural history of Farber disease: An ultra-orphan condition with rheumatologic and neurological cardinal disease features. Genet. Med. 2018, 20, 524–530. [Google Scholar] [CrossRef]
- Punzi, L.; Galozzi, P.; Luisetto, R.; Scanu, A.; Ramonda, R.; Oliviero, F. Gout: One year in review 2023. Clin. Exp. Rheumatol. 2024, 42, 1–9. [Google Scholar] [CrossRef]
- Rothschild, B.M. Rheumatology: A Primary Care Approach; Yorke Medical Press: New York, NY, USA, 1982. [Google Scholar]
- Baffour, F.I.; Ferrero, A.; Aird, G.A.; Powell, G.M.; Adkins, M.C.; Bekele, D.I.; Johnson, M.P.; Fletcher, J.G.; Glazebrook, K.N. Evolving role of dual-energy CT in the clinical workup of gout: A retrospective study. Am. J. Roentgenol. 2022, 218, 1041–1050. [Google Scholar] [CrossRef] [PubMed]
- Resnick, D. Diagnosis of Bone and Joint Disorders; Saunders: Philadelphia, PA, USA, 2002. [Google Scholar]
- Zhong, H.; Wang, M.; Zhang, H.; Huang, Z.; Zou, B.; Zou, G.; Xie, N.; Liang, Y.; Zhu, Y.; Ma, W. Gout of feet and ankles in different stages: The potentiality of a new semiquantitative DECT scoring system in monitoring urate deposition. Medicine 2023, 102, e32722. [Google Scholar] [CrossRef] [PubMed]
- Cui, L.; Xu, Z.; Hou, H. Diagnosis and Treatment of Spinal Syphilitic Gumma. Front. Neurol. 2020, 10, 1352. [Google Scholar] [CrossRef] [PubMed]
- Taranta, A. Occurrence of rheumatic-like subcutaneous nodules without evidence of joint or heart disease. N. Engl. J. Med. 1962, 266, 13–16. [Google Scholar] [CrossRef] [PubMed]
- Woodburne, A.R.; Philpott, O.S. Nodular vasculitis. Arch. Derm. Syphilol. 1949, 60, 294–302. [Google Scholar] [CrossRef] [PubMed]
- Yamammoto, K.; Rokutanda, R. Disseminated Mycobacterium haemophilum infection mimicking rheumatoid nodules. J. Rheumatol. 2023, 50, 1193. [Google Scholar] [CrossRef]
- Butler, T. Plague Gives Surprises in the Second Decade of the Twenty-First Century. Am. J. Trop. Med. Hyg. 2023, 109, 985–988. [Google Scholar] [CrossRef] [PubMed]
- Sharma, R.; Patil, R.; Soingh, B.; Chakraborty, S.; Chandran, D.; Khama, K.; Gopinath, D.; Jairath, G.; Rialch, A.; Mal, G.; et al. Tularemia—A re-emerging disease with growing concern. Vet. Q. 2023, 43, 1–16. [Google Scholar] [CrossRef]
- Beatty, E.C. Rheumatic-like nodules occurring in nonrheumatic children. Arch. Pathol. 1959, 68, 154–159. [Google Scholar]
- Divers, T.J.; Gardner, R.B.; Madigan, J.E.; Witonsky, S.G.; Bertone, J.J.; Swinebroad, E.L.; Schutzer, S.E.; Johnson, A.L. Borrelia burgdorferi infection and lyme disease in North American horses: A consensus statement. J. Vet. Intern. Med. 2018, 32, 617–632. [Google Scholar] [CrossRef]
- España, A.; Torrelo, A.; Guerrero, A.; Suárez, J.; Rocamora, A.; Ledo, A. Periarticular fibrous nodules in Lyme borreliosis. Br. J. Dermatol. 1991, 125, 68–70. [Google Scholar] [CrossRef] [PubMed]
- Krotewicz, M.; Czarnecka, A.M.; Bloński, P.; Śledź, J.; Szostakowsik, B.; Szumera-Ciećkiewicz, A.; Bartnik, E.; Rutkowski, P. Distal and proximal epithelioid sarcoma—Differences in diagnosis and similarities in treatment. Oncol. Clin. Pract. 2024, 99119. [Google Scholar] [CrossRef]
- Macuglia, V.S.; Peruzzo, J.; Geller, A.B. Skin nodules of distal-type epithelioid sarcoma. An. Bras. Dermatol. 2023, 98, 404–406. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Jing, C.; Liu, H.; Zhao, Z.; Zhang, X.; Liiu, T.; Xu, S.; Xu, L.; Yu, S. Epithelioid sarcoma: A single-institutional retrospective cohort study of 36 cases. J. Orthopaed Surg. 2021, 29, 23094990211029349. [Google Scholar] [CrossRef] [PubMed]
- Hawryluk, E.B.; Izikson, L.; English, J.C. Non-infectious granulomatous diseases of the skin and their associated systemic diseases: An evidence-based update to important clinical questions. Am. J. Clin. Dermatol. 2010, 11, 171–181. [Google Scholar] [CrossRef] [PubMed]
- Imadojemu, S.; Rosenbach, M. Advances in inflammatory granulomatous skin diseases. Dermatol. Clin. 2019, 37, 49–64. [Google Scholar] [CrossRef]
- Horino, T.; Inotani, S.; Nakjima, H.; Ohnishi, H.; Komori, M.; Ichii, O.; Terada, Y. Pseudoxanthomatous frheumatoid nodule. Lancet Rheumatol. 2023, 5, e110. [Google Scholar] [CrossRef]
- Rodolfi, S.; Della-Torre, E.; Bongiovanni, L.; Mehta, P.; Fajgenbaum, D.C.; Selmi, C. Lymphadenopathy in the rheumatology practice: A pragmatic approach. Rheumatology 2023, 2023, kead644. [Google Scholar] [CrossRef]
| Primarily dermatologically-limited | Immunologic diseases |
|---|---|
| Granuloma annulare | Sarcoidosis |
| Erythema nodosum * | Agammaglobulinemia |
| Basal cell carcinoma | Necrobiotic xanthogranulma |
| Sebaceous/epidermal cysts | Infectious diseases |
| Xanthomas * | Rheumatic fever |
| Foreign body reaction | Erythema nodosum |
| Trauma | Subacute bacterial endocarditis |
| Myositis ossificans | Leprosy |
| Fatty tumor disorders | Tuberculosis |
| Weber-Christian disease | Fungal disease |
| Tuberous xanthomatosus | Lyme disease |
| Primarily musculoskeletal disease | Syphilis |
| Rheumatoid arthritis | Yaws |
| Juvenile inflammatory arthritis | Bejel |
| Psoriatic arthritis | Lyme |
| Jaccoud disease | Whipple’s disease |
| Inflammatory diseases | Hepatitis B |
| Pancreatitis | Vasculitis/vasculopathy diseases |
| Metabolic disorders | Polyarteritis nodosa |
| Gout | Behcet’s disease |
| Necrobiosis lipoidica diabeticorum | Granulomatous disease with antiitis |
| Deposition diseases | Henoch-Schoelein purpura |
| Amyloidosis | Churg Straus angiitis |
| Farber’s disease | Malignant disease |
| Multicentric reticulohistiocytosis | Metastatic disease |
| Collagen vascular/connective tissue diseases | Pancreatic carcinoma |
| Systemic lupus erythematosus | Sarcoma |
| Dermatomyositis | |
| Scleroderma |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rothschild, B. Subcutaneous Nodules as Manifestations of Systemic Disease. Rheumato 2024, 4, 75-87. https://doi.org/10.3390/rheumato4020007
Rothschild B. Subcutaneous Nodules as Manifestations of Systemic Disease. Rheumato. 2024; 4(2):75-87. https://doi.org/10.3390/rheumato4020007
Chicago/Turabian StyleRothschild, Bruce. 2024. "Subcutaneous Nodules as Manifestations of Systemic Disease" Rheumato 4, no. 2: 75-87. https://doi.org/10.3390/rheumato4020007
APA StyleRothschild, B. (2024). Subcutaneous Nodules as Manifestations of Systemic Disease. Rheumato, 4(2), 75-87. https://doi.org/10.3390/rheumato4020007






