Dynamic Joint Stiffness of the Knee in Post-Menopausal Women with and without Rheumatoid Arthritis
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Clinical Assessment
2.3. Gait Assessment and Data Processing
2.4. Statistical Analyses
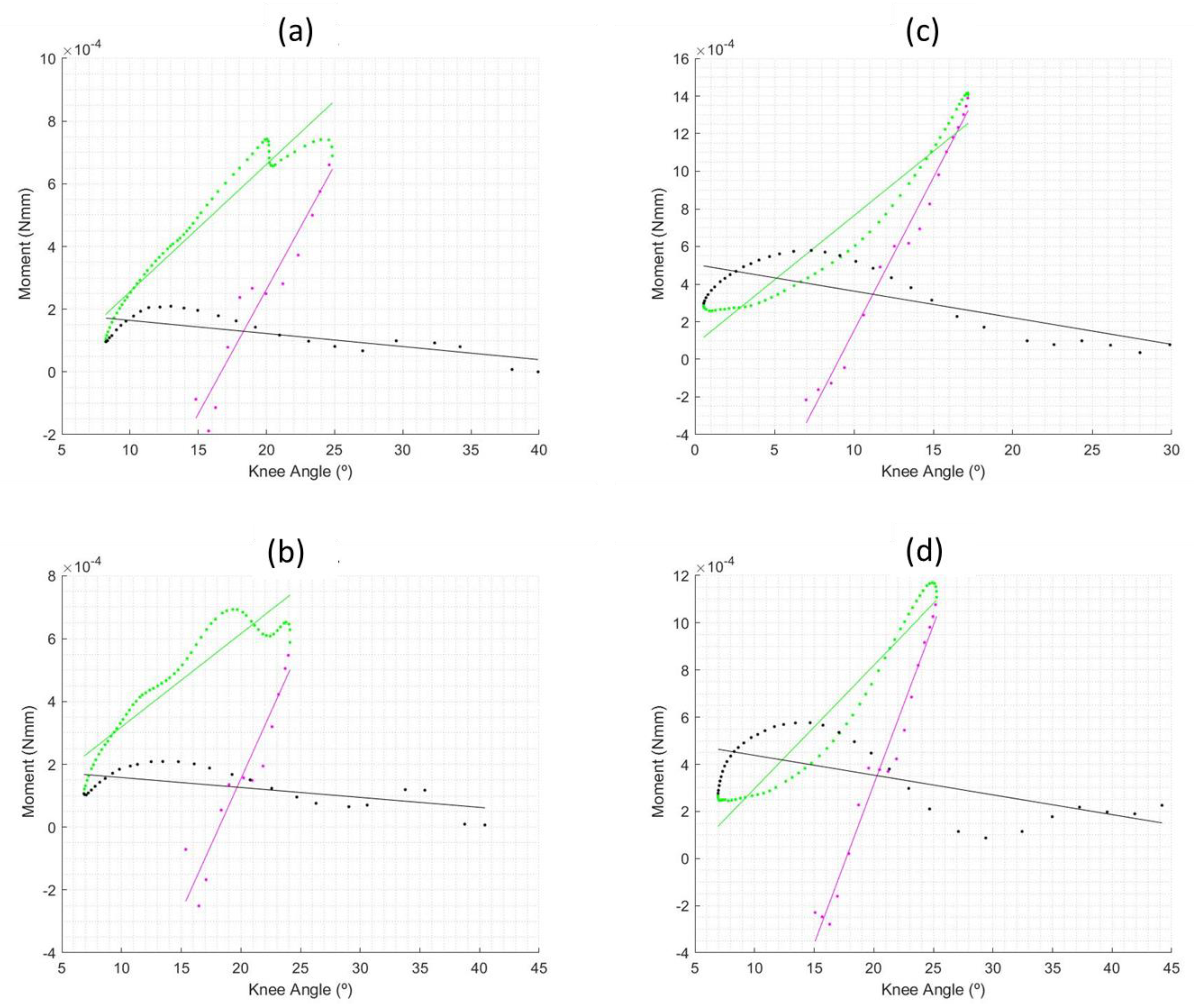
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Espanha, M.; Pascoal, A.; Correia, P.; Silva, P. Noções Fundamentais De Artrologia. In Anatomofisiologia. Tomo I. Sistema osteo-articular; Espanha, M., Ed.; Faculdade de Motricidade Humana—Serviço De Edições: Cruz Quebrada, Portugal, 1999. [Google Scholar]
- Abrantes, J. Rigidez dinâmica como indicador da estabilidade articular. In Proceedings of the XII Congresso Brasileiro de Biomecânica, São Paulo, Brazil, 30 May–2 June 2007. [Google Scholar]
- Aleixo, P.; Vaz Patto, J.; Moreira, H.; Abrantes, J. Dynamic joint stiffness of the ankle in healthy and rheumatoid arthritis post-menopausal women. Gait Posture 2018, 60, 225–234. [Google Scholar] [CrossRef] [PubMed]
- Faria, A.; Gabriel, R.; Abrantes, J.; Moreira, H.; Wood, P.; Camacho, T. The Relationship between Muscle-Tendon Unit Stiffness, Joint Stability and Posture: The Risk of Injury, Performance, Resonance and Energy Expenditure. In Posture: Types, Assessment and Control; Wright, A., Rothenberg, S., Eds.; Nova Science Publishers: New York, NY, USA, 2011; pp. 137–154. ISBN 6312317269. [Google Scholar]
- Riemann, B.; Lephart, S. The sensorimotor system, part I: The physiologic basis of functional joint stability. J. Athl. Train. 2002, 37, 71–79. [Google Scholar] [PubMed]
- Docherty, C.; Arnold, B.; Zinder, S.; Granata, K.; Gansneder, B. Relationship between two proprioceptive measures and stiffness at the ankle. J. Electromyogr. Kinesiol. 2004, 14, 317–324. [Google Scholar] [CrossRef] [PubMed]
- Aletaha, D.; Neogi, T.; Silman, A.; Funovits, J.; Felson, D.; Bingham, C.; Birnbaum, N.; Burmester, G.; Bykerk, V.; Cohen, M.; et al. 2010 Rheumatoid arthritis classification criteria: An American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum. 2010, 62, 2569–2581. [Google Scholar] [CrossRef]
- Myasoedova, E.; Davis, J.; Matteson, E.; Crowson, C. Is the epidemiology of rheumatoid arthritis changing? Results from a population-based incidence study, 1985–2014. Ann. Rheum. Dis. 2020, 79, 440–444. [Google Scholar] [CrossRef]
- Mollard, E.; Pedro, S.; Chakravarty, E.; Clowse, M.; Schumacher, R.; Michaud, K. The impact of menopause on functional status in women with rheumatoid arthritis. Rheumatology 2018, 57, 798–802. [Google Scholar] [CrossRef]
- Alpizar-Rodriguez, D.; Förger, F.; Courvoisier, D.; Gabay, C.; Finckh, A. Role of reproductive and menopausal factors in functional and structural progression of rheumatoid arthritis: Results from the SCQM cohort. Rheumatology 2019, 58, 432–440. [Google Scholar] [CrossRef]
- Stanmore, E.; Oldham, J.; Skelton, D.; O’Neill, T.; Pilling, M.; Campbell, J.; Todd, C. Risk factors for falls in adults with rheumatoid arthritis: A prospective study. Arthritis Care Res. 2013, 65, 1251–1258. [Google Scholar] [CrossRef]
- Rubenstein, L. Falls in older people: Epidemiology, risk factors and strategies for prevention. Age Ageing 2006, 35, ii37–ii41. [Google Scholar] [CrossRef]
- Weiss, R.; Wretenberg, P.; Stark, A.; Palmblad, K.; Larsson, P.; Gröndal, L.; Broström, E. Gait pattern in rheumatoid arthritis. Gait Posture 2008, 28, 229–234. [Google Scholar] [CrossRef]
- Jin, L.; Hahn, M. Modulation of lower extremity joint stiffness, work and power at different walking and running speeds. Hum. Mov. Sci. 2018, 58, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Aleixo, P.; Atalaia, T.; Abrantes, J. Dynamic Joint Stiffness: A Critical Review. In Advances in Medicine and Biology 175; Berhardt, L., Ed.; Nova Science Publishers: New York, NY, USA, 2021; pp. 1–96. ISBN 978-1-53619-083-0. [Google Scholar]
- Davis, R.; De Luca, P. Pathological gait characterization via dynamic joint stiffness. Gait Posture 1995, 3, 173. [Google Scholar] [CrossRef]
- Davis, R.; DeLuca, P. Gait caracterization via dynamic joint stiffness. Gait Posture 1996, 4, 224–231. [Google Scholar] [CrossRef]
- Gabriel, R.; Abrantes, J.; Granata, K.; Bulas-Cruz, J.; Melo-Pinto, P.; Filipe, V. Dynamic joint stiffness of the ankle during walking: Gender-related differences. Phys. Ther. Sport 2008, 9, 16–24. [Google Scholar] [CrossRef] [PubMed]
- Aleixo, P.; Vaz Patto, J.; Abrantes, J. Dynamic joint stiffness of the ankle in rheumatoid arthritis postmenopausal women fallers and non-fallers. Gait Posture 2017, 57, 324–325. [Google Scholar] [CrossRef]
- Frigo, C.; Crenna, P.; Jensen, L. Moment-angle relationship at lower limb joints during human walking at different velocities. J. Electromyogr. Kinesiol. 1996, 6, 177–190. [Google Scholar] [CrossRef]
- Galli, M.; Rigoldi, C.; Brunner, R.; Virji-Babul, N.; Giorgio, A. Joint stiffness and gait pattern evaluation in children with Down syndrome. Gait Posture 2008, 28, 502–506. [Google Scholar] [CrossRef]
- McGinnis, K.; Snyder-Mackler, L.; Flowers, P.; Zeni, J. Dynamic joint stiffness and co-contraction in subjects after total knee arthroplasty. Clin. Biomech. 2013, 28, 205–210. [Google Scholar] [CrossRef]
- Shamaei, K.; Sawicki, G.; Dollar, A. Estimation of quasi-stiffness of the human knee in the stance phase of walking. PLoS ONE 2013, 8, e59993. [Google Scholar] [CrossRef]
- Williams, D.; Brunt, D.; Tanenberg, R. Diabetic neuropathy is related to joint stiffness during late stance phase. J. Appl. Biomech. 2007, 23, 251–260. [Google Scholar] [CrossRef]
- Zeni, J.; Higginson, J. Dynamic knee joint stiffness in subjects with a progressive increase in severity of knee osteoarthritis. Clin. Biomech. 2009, 24, 366–371. [Google Scholar] [CrossRef] [PubMed]
- Safaeepour, Z.; Esteki, A.; Ghomshe, F.; Osman, N. Quantitative analysis of human ankle characteristics at different gait phases and speeds for utilizing in ankle-foot prosthetic design. Biomed. Eng. Online 2014, 13, 19. [Google Scholar] [CrossRef] [PubMed]
- Atalaia, T.; Abrantes, J.; Castro-Caldas, A. Influence of footedness on dynamic joint stiffness during the gait stance phase. J. Sci. Res. Reports 2015, 5, 175–183. [Google Scholar] [CrossRef] [PubMed]
- Harlow, S.; Gass, M.; Hall, J.; Lobo, R.; Maki, P.; Rebar, R.; Sherman, S.; Sluss, P.; De Villiers, T. Executive summary of the Stages of Reproductive Aging Workshop + 10: Addressing the unfinished agenda of staging reproductive aging Methods-Scientists from five countries and multiple disciplines evaluated data from cohort studies of midlife women and in. Menopause 2012, 19, 387–395. [Google Scholar] [CrossRef]
- Shuster, L.; Rhodes, D.; Gostout, B.; Grossardt, B.; Rocca, W. Premature menopause or early menopause: Long-term health consequences. Maturitas 2010, 65, 161–166. [Google Scholar] [CrossRef]
- Smolen, J.; Breedveld, F.; Eberl, G.; Jones, I.; Leeming, M.; Wylie, G.; Kirkpatrick, J. Validity and reliability of the twenty-eight-joint count for the assessement of rheumatoid arthritis activity. Arthritis Rheum. 1995, 38, 38–43. [Google Scholar] [CrossRef]
| With RA (n = 18) | Without RA (n = 18) | Differences | |
|---|---|---|---|
| Mean (sd) | Mean (sd) | p Value | |
| Age (years) | 64.3 (8.4) | 64.3 (7.8) | 1.000 |
| Disease duration (years) | 11.5 (10.7) | - | - |
| DAS-28 score | 4.4 (1.2) | - | - |
| Menopause duration (years) | 16.9 (8.7) | 15.0 (9.1) | 0.530 |
| Body mass (kg) | 63.7 (9.8) | 64.5 (12.6) | 0.826 |
| Height (m) | 1.52 (0.06) | 1.54 (0.06) | 0.301 |
| Body mass index (kg/m2) | 27.8 (4.8) | 27.2 (4.6) | 0.705 |
| 1st KFS | KES | 2nd KFS | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Knees | DJS | CV | R2 | CV | DJS | CV | R2 | CV | DJS | CV | R2 | CV |
| L_1 | 0.0900 (0.0085) | 9.5 | 0.985 (0.007) | 0.7 | 0.0405 (0.0027) | 6.7 | 0.981 (0.009) | 0.9 | −0.0030 (0.0020) | 67.0 | 0.294 (0.184) | 62.4 |
| L_2 | 0.0674 (0.0095) | 14.2 | 0.923 (0.028) | 3.0 | 0.0395 (0.0024) | 6.1 | 0.996 (0.002) | 0.2 | 0.0092 (0.0016) | 17.7 | 0.841 (0.072) | 8.5 |
| L_3 | 0.0183 (0.0089) | 48.4 | 0.549 (0.123) | 22.4 | 0.0289 (0.0128) | 44.4 | 0.871 (0.287) | 32.9 | 0.0034 (0.0027) | 79.9 | 0.686 (0.089) | 13.0 |
| L_4 | 0.0892 (0.0270) | 30.3 | 0.836 (0.202) | 24.2 | 0.0406 (0.0059) | 14.6 | 0.958 (0.050) | 5.2 | −0.0087 (0.0013) | 15.2 | 0.880 (0.046) | 5.2 |
| L_5 | 0.0494 (0.0031) | 6.3 | 0.982 (0.007) | 0.7 | 0.0339 (0.0039) | 11.4 | 0.985 (0.009) | 0.9 | −0.0046 (0.0007) | 14.3 | 0.656 (0.057) | 8.6 |
| L_6 | 0.1126 (0.0125) | 6.4 | 0.974 (0.007) | 0.8 | 0.0569 (0.0032) | 5.6 | 0.991 (0.006) | 0.6 | 0.0040 (0.0012) | 29.8 | 0.469 (0.102) | 21.8 |
| L_7 | 0.1278 (0.0193) | 15.1 | 0.979 (0.011) | 1.1 | 0.0529 (0.0066) | 12.4 | 0.987 (0.008) | 0.8 | −0.0042 (0.0004) | 9.9 | 0.605 (0.051) | 8.4 |
| L_8 | 0.1136 (0.0138) | 12.1 | 0.949 (0.016) | 1.7 | 0.0332 (0.0020) | 6.0 | 0.988 (0.008) | 0.8 | 0.0043 (0.0017) | 40.1 | 0.710 (0.161) | 22.6 |
| L_9 | 0.0575 (0.0148) | 25.7 | 0.830 (0.175) | 21.1 | 0.0429 (0.0265) | 61.8 | 0.907 (0.199) | 22.0 | −0.0022 (0.0027) | 123.3 | 0.265 (0.196) | 73.9 |
| L_10 | 0.0765 (0.0061) | 8.0 | 0.975 (0.014) | 1.4 | 0.0523 (0.0074) | 14.1 | 0.992 (0.008) | 0.8 | 0.0038 (0.0005) | 13.1 | 0.590 (0.061) | 10.4 |
| L_11 | 0.0409 (0.0076) | 18.6 | 0.734 (0.116) | 15.9 | 0.0478 (0.0098) | 20.5 | 0.941 (0.033) | 3.5 | 0.0102 (0.0021) | 20.2 | 0.941 (0.027) | 2.8 |
| L_12 | 0.2119 (0.1440) | 68.0 | 0.614 (0.237) | 38.6 | 0.0456 (0.0026) | 5.7 | 0.988 (0.021) | 2.1 | 0.0058 (0.0014) | 24.2 | 0.684 (0.076) | 11.1 |
| L_13 | 0.0855 (0.0085) | 10.0 | 0.935 (0.046) | 5.0 | 0.0322 (0.0185) | 57.4 | 0.860 (0.167) | 19.4 | −0.0008 (0.0022) | 279.7 | 0.307 (0.184) | 60.0 |
| L_14 | 0.1640 (0.0125) | 7.6 | 0.988 (0.006) | 0.6 | 0.0682 (0.0024) | 3.5 | 0.960 (0.012) | 1.3 | −0.0144 (0.0031) | 21.5 | 0.730 (0.049) | 6.8 |
| L_15 | 0.0924 (0.0116) | 12.5 | 0.960 (0.007) | 0.7 | 0.0423 (0.0042) | 9.9 | 0.985 (0.008) | 0.8 | −0.0081 (0.0016) | 19.8 | 0.780 (0.096) | 12.4 |
| L_16 | 0.0214 (0.0036) | 16.8 | 0.577 (0.108) | 18.8 | 0.0337 (0.0026) | 7.8 | 0.980 (0.010) | 1.0 | 0.0044 (0.0009) | 20.7 | 0.699 (0.091) | 13.0 |
| L_17 | 0.1461 (0.0532) | 36.4 | 0.748 (0.101) | 13.5 | 0.0667 (0.0272) | 40.8 | 0.877 (0.137) | 15.7 | 0.0092 (0.0010) | 11.0 | 0.878 (0.030) | 3.4 |
| L_18 | 0.0918 (0.0100) | 10.9 | 0.973 (0.013) | 1.3 | 0.0558 (0.0053) | 9.5 | 0.978 (0.007) | 0.7 | −0.0019 (0.0010) | 50.9 | 0.208 (0.095) | 45.5 |
| R_1 | 0.1359 (0.0154) | 11.3 | 0.982 (0.010) | 1.0 | 0.0557 (0.0048) | 8.6 | 0.966 (0.008) | 0.8 | −0.0143 (0.0023) | 16.0 | 0.793 (0.060) | 7.5 |
| R_2 | 0.0893 (0.0117) | 13.1 | 0.956 (0.016) | 1.7 | 0.0359 (0.0031) | 8.8 | 0.990 (0.005) | 0.5 | 0.0031 (0.0016) | 52.9 | 0.361 (0.149) | 41.4 |
| R_3 | 0.0443 (0.0039) | 8.8 | 0.882 (0.072) | 8.1 | 0.0558 (0.0165) | 29.5 | 0.977 (0.010) | 1.0 | −0.0057 (0.0013) | 21.9 | 0.739 (0.072) | 9.7 |
| R_4 | 0.0957 (0.0138) | 14.4 | 0.975 (0.007) | 0.7 | 0.0546 (0.0074) | 13.6 | 0.990 (0.003) | 0.3 | −0.0131 (0.0023) | 17.7 | 0.798 (0.074) | 9.3 |
| R_5 | 0.0625 (0.0115) | 18.4 | 0.963 (0.024) | 2.5 | 0.0251 (0.0031) | 12.2 | 0.951 (0.024) | 2.5 | 0.0018 (0.0006) | 30.3 | 0.346 (0.094) | 27.0 |
| R_6 | 0.1468 (0.0173) | 11.8 | 0.973 (0.009) | 0.9 | 0.0598 (0.0063) | 10.6 | 0.966 (0.011) | 1.2 | −0.0109 (0.0010) | 8.9 | 0.760 (0.041) | 5.4 |
| R_7 | 0.1451 (0.0122) | 8.4 | 0.963 (0.014) | 1.4 | 0.0417 (0.0027) | 6.4 | 0.982 (0.005) | 0.5 | −0.0031 (0.0014) | 43.7 | 0.336 (0.135) | 40.1 |
| R_8 | 0.1912 (0.0427) | 22.3 | 0.944 (0.019) | 2.0 | 0.0330 (0.0032) | 9.6 | 0.987 (0.012) | 1.2 | 0.0017 (0.0005) | 28.6 | 0.348 (0.094) | 27.0 |
| R_9 | 0.0738 (0.0077) | 10.4 | 0.936 (0.018) | 2.0 | 0.0467 (0.0032) | 6.9 | 0.985 (0.008) | 0.8 | −0.0080 (0.0019) | 24.2 | 0.785 (0.100) | 12.8 |
| R_10 | 0.0734 (0.0049) | 6.7 | 0.977 (0.011) | 1.2 | 0.0450 (0.0038) | 8.5 | 0.985 (0.017) | 1.8 | 0.0041 (0.0012) | 29.9 | 0.503 (0.109) | 21.8 |
| R_11 | 0.0784 (0.0420) | 53.6 | 0.859 (0.085) | 9.9 | 0.0707 (0.0114) | 16.2 | 0.969 (0.028) | 2.9 | −0.0032 (0.0015) | 45.3 | 0.611 (0.184) | 30.0 |
| R_12 | 0.5404 (0.2549) | 47.2 | 0.879 (0.111) | 12.7 | 0.0604 (0.0078) | 12.9 | 0.968 (0.027) | 2.8 | −0.0013 (0.0020) | 157.4 | 0.172 (0.119) | 69.5 |
| R_13 | 0.1046 (0.0278) | 26.6 | 0.956 (0.023) | 2.4 | 0.0437 (0.0039) | 8.9 | 0.972 (0.031) | 3.2 | −0.0054 (0.0015) | 28.2 | 0.670 (0.116) | 17.3 |
| R_14 | 0.1372 (0.0084) | 6.1 | 0.982 (0.005) | 0.5 | 0.0520 (0.0021) | 4.0 | 0.962 (0.009) | 0.9 | −0.0090 (0.0015) | 17.1 | 0.651 (0.098) | 15.0 |
| R_15 | 0.0757 (0.0166) | 21.9 | 0.948 (0.050) | 5.2 | 0.0520 (0.0081) | 15.6 | 0.980 (0.010) | 1.0 | −0.0033 (0.0015) | 44.2 | 0.442 (0.172) | 38.8 |
| R_16 | 0.0443 (0.0039) | 8.8 | 0.882 (0.072) | 8.1 | 0.0558 (0.0165) | 29.5 | 0.977 (0.010) | 1.0 | −0.0057 (0.0013) | 21.9 | 0.739 (0.072) | 9.7 |
| R_17 | 0.2953 (0.1333) | 45.2 | 0.877 (0.055) | 6.2 | 0.0525 (0.0211) | 40.1 | 0.899 (0.174) | 19.3 | 0.0036 (0.0009) | 23.3 | 0.417 (0.098) | 23.5 |
| R_18 | 0.0892 (0.0101) | 11.3 | 0.981 (0.006) | 0.6 | 0.0581 (0.0105) | 18.1 | 0.964 (0.024) | 2.5 | −0.0029 (0.0021) | 73.5 | 0.320 (0.200) | 62.5 |
| mean (sd) | 0.1133 (0.0917) | 19.5 | 0.901 (0.117) | 6.6 | 0.0476 (0.0114) | 16.6 | 0.964 * (0.357) | 4.3 * | −0.0018 * (0.0065) | 42.9 | 0.584 * (0.216) | 23.8 |
| 1st KFS | KES | 2nd KFS | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Knees | Invol. | N. | DJS | CV | R2 | CV | DJS | CV | R2 | CV | DJS | CV | R2 | CV |
| L_1 | No | 5 | 0.1087 (0.0238) | 21.9 | 0.950 (0.035) | 3.7 | 0.0608 (0.0259) | 42.7 | 0.961 (0.059) | 6.1 | −0.0244 (0.038) | 15.7 | 0.926 (0.024) | 2.5 |
| L_2 | No | 1 | 0.0347 (0.0147) | 42.4 | 0.667 (0.229) | 34.3 | −0.0200 (0.0639) | 320.0 | 0.688 (0.344) | 49.9 | −0.0139 (0.0170) | 122.6 | 0.758 (0.312) | 41.1 |
| L_3 | Yes | 3 | 0.0787 (0.0086) | 11.0 | 0.957 (0.021) | 2.2 | 0.0412 (0.0052) | 12.6 | 0.963 (0.016) | 1.7 | −0.0039 (0.0013) | 32.9 | 0.658 (0.229) | 34.8 |
| L_4 | No | 0 | 0.0799 (0.0203) | 25.4 | 0.993 (0.005) | 0.5 | 0.0422 (0.0082) | 19.3 | 0.889 (0.054) | 6.1 | −0.0093 (0.0019) | 21.0 | 0.938 (0.020) | 2.2 |
| L_5 | Yes | 8 | 0.0779 (0.0161) | 20.6 | 0.972 (0.011) | 1.1 | 0.0611 (0.0109) | 17.8 | 0.979 (0.017) | 1.7 | 0.0020 (0.0021) | 105.4 | 0.478 (0.194) | 40.5 |
| L_6 | No | 0 | 0.1020 (0.0085) | 8.4 | 0.978 (0.011) | 1.1 | 0.0253 (0.0045) | 17.8 | 0.932 (0.028) | 3.0 | −0.0066 (0.0010) | 14.7 | 0.761 (0.080) | 10.5 |
| L_7 | No | 2 | 0.0846 (0.0055) | 6.5 | 0.985 (0.009) | 0.9 | 0.0428 (0.0058) | 13.6 | 0.938 (0.046) | 4.9 | −0.0075 (0.0029) | 38.5 | 0.683 (0.138) | 20.3 |
| L_8 | Yes | 13 | 0.2011 (0.1255) | 62.4 | 0.919 (0.093) | 10.1 | 0.0754 (0.0338) | 44.8 | 0.755 (0.205) | 27.2 | −0.0445 (0.0070) | 15.8 | 0.970 (0.009) | 1.0 |
| L_9 | Yes | 3 | 0.1178 (0.0174) | 14.8 | 0.954 (0.025) | 2.6 | 0.0509 (0.0039) | 7.7 | 0.984 (0.015) | 1.5 | −0.0057 (0.0016) | 27.5 | 0.688 (0.142) | 20.6 |
| L_10 | Yes | 1 | 0.0913 (0.0072) | 7.9 | 0.987 (0.006) | 0.6 | 0.0470 (0.0053) | 11.2 | 0.980 (0.017) | 1.8 | −0.0063 (0.0020) | 31.4 | 0.872 (0.102) | 11.7 |
| L_11 | Yes | 2 | 0.2504 (0.0768) | 30.7 | 0.969 (0.020) | 2.0 | 0.0153 (0.0409) | 267.0 | 0.232 (0.097) | 41.6 | −0.0250 (0.0036) | 14.5 | 0.971 (0.014) | 1.5 |
| L_12 | No | 0 | 0.0800 (0.0184) | 22.9 | 0.864 (0.100) | 11.6 | 0.0361 (0.0040) | 11.2 | 0.981 (0.012) | 1.2 | −0.0057 (0.0024) | 42.0 | 0.701 (0.118) | 16.9 |
| L_13 | No | 6 | 0.1120 (0.0391) | 34.9 | 0.941 (0.037) | 3.9 | 0.0009 (0.0353) | 325.4 | 0.767 (0.147) | 19.2 | −0.0078 (0.0033) | 42.1 | 0.786 (0.149) | 18.9 |
| L_14 | No | 4 | 0.2049 (0.0789) | 38.5 | 0.977 (0.012) | 1.2 | 0.0683 (0.0062) | 9.1 | 0.995 (0.003) | 0.3 | −0.0012 (0.0010) | 83.1 | 0.170 (0.125) | 73.2 |
| L_15 | No | 5 | 0.1605 (0.0385) | 24.0 | 0.935 (0.063) | 6.8 | 0.0513 (0.0161) | 31.4 | 0.846 (0.214) | 25.2 | −0.0010 (0.0024) | 228.3 | 0.347 (0.244) | 70.3 |
| L_16 | Yes | 4 | 0.0639 (0.0185) | 29.0 | 0.868 (0.091) | 10.5 | 0.0257 (0.0134) | 52.2 | 0.809 (0.140) | 17.3 | 0.0001 (0.0017) | 271.6 | 0.376 (0.203) | 53.9 |
| L_17 | No | 1 | 0.1419 (0.0097) | 6.8 | 0.988 (0.018) | 1.8 | 0.0915 (0.0127) | 13.8 | 0.973 (0.013) | 1.3 | −0.0110 (0.0024) | 21.4 | 0.892 (0.032) | 3.6 |
| L_18 | No | 1 | 0.0713 (0.0229) | 32.1 | 0.872 (0.030) | 3.4 | 0.0511 (0.0107) | 20.9 | 0.976 (0.034) | 3.5 | 0.0012 (0.0012) | 103.1 | 0.347 (0.134) | 38.6 |
| R_1 | No | 5 | 0.1190 (0.0313) | 26.3 | 0.891 (0.060) | 6.8 | 0.0269 (0.0246) | 91.3 | 0.560 (0.320) | 57.2 | −0.0230 (0.0048) | 20.8 | 0.974 (0.015) | 1.5 |
| R_2 | No | 0 | 0.0986 (0.0091) | 9.2 | 0.974 (0.007) | 0.7 | 0.0302 (0.0080) | 26.6 | 0.925 (0.054) | 5.9 | −0.0108 (0.0019) | 17.4 | 0.893 (0.050) | 5.6 |
| R_3 | No | 2 | 0.0859 (0.0130) | 15.1 | 0.942 (0.043) | 4.5 | 0.0297 (0.0043) | 14.4 | 0.917 (0.051) | 5.6 | −0.0031 (0.0005) | 15.4 | 0.584 (0.074) | 12.6 |
| R_4 | Yes | 3 | 0.0889 (0.0460) | 51.7 | 0.960 (0.033) | 3.5 | 0.0165 (0.0500) | 303.2 | 0.453 (0.382) | 84.3 | −0.0213 (0.0032) | 15.1 | 0.903 (0.037) | 4.1 |
| R_5 | Yes | 8 | 0.0589 (0.0096) | 16.3 | 0.971 (0.011) | 1.1 | 0.0512 (0.0086) | 16.7 | 0.990 (0.006) | 0.6 | −0.0008 (0.0020) | 266.5 | 0.208 (0.199) | 95.7 |
| R_6 | No | 1 | 0.1718 (0.0370) | 21.5 | 0.929 (0.031) | 3.3 | 0.0201 (0.0032) | 16.1 | 0.970 (0.017) | 1.8 | 0.0004 (0.0014) | 359.5 | 0.228 (0.111) | 48.7 |
| R_7 | No | 2 | 0.0869 (0.0135) | 15.5 | 0.980 (0.003) | 0.3 | 0.0445 (0.0028) | 6.2 | 0.966 (0.011) | 1.1 | −0.0212 (0.0011) | 5.2 | 0.934 (0.033) | 3.5 |
| R_8 | Yes | 13 | 0.3206 (0.1206) | 37.6 | 0.887 (0.145) | 16.4 | 0.0639 (0.0356) | 55.6 | 0.539 (0.374) | 69.3 | −0.0482 (0.0042) | 8.7 | 0.951 (0.006) | 0.6 |
| R_9 | Yes | 2 | 0.1136 (0.0119) | 10.5 | 0.982 (0.013) | 1.3 | 0.0544 (0.0058) | 10.7 | 0.976 (0.014) | 1.4 | −0.0124 (0.0012) | 9.8 | 0.828 (0.047) | 5.7 |
| R_10 | No | 0 | 0.0805 (0.0170) | 21.1 | 0.943 (0.029) | 3.0 | 0.0342 (0.0089) | 26.0 | 0.972 (0.052) | 5.4 | 0.0050 (0.0015) | 30.0 | 0.670 (0.132) | 19.6 |
| R_11 | Yes | 2 | 0.1809 (0.0445) | 24.6 | 0.887 (0.075) | 8.5 | 0.2751 (0.2542) | 92.4 | 0.544 (0.422) | 77.5 | −0.0716 (0.0195) | 27.2 | 0.897 (0.019) | 2.1 |
| R_12 | No | 0 | 0.0835 (0.0170) | 20.3 | 0.858 (0.080) | 9.4 | 0.0326 (0.0052) | 15.8 | 0.981 (0.010) | 1.0 | −0.0005 (0.0022) | 404.2 | 0.200 (0.170) | 85.4 |
| R_13 | No | 6 | 0.0925 (0.0140) | 15.2 | 0.909 (0.060) | 6.6 | 0.0219 (0.0113) | 51.6 | 0.545 (0.196) | 35.9 | −0.0105 (0.0027) | 25.5 | 0.937 (0.038) | 4.1 |
| R_14 | No | 2 | 0.1461 (0.0210) | 14.4 | 0.952 (0.015) | 1.5 | 0.0479 (0.0048) | 9.9 | 0.995 (0.003) | 0.3 | 0.0027 (0.0009) | 33.0 | 0.363 (0.095) | 26.1 |
| R_15 | No | 5 | 0.1270 (0.0279) | 22.0 | 0.969 (0.011) | 1.2 | 0.0455 (0.0137) | 30.0 | 0.866 (0.118) | 13.7 | −0.0141 (0.0012) | 8.3 | 0.906 (0.030) | 3.3 |
| R_16 | No | 2 | 0.1089 (0.0250) | 23.0 | 0.963 (0.019) | 1.9 | 0.0348 (0.0068) | 19.6 | 0.873 (0.069) | 7.9 | −0.0048 (0.0017) | 34.8 | 0.750 (0.109) | 14.5 |
| R_17 | No | 1 | 0.1229 (0.0108) | 8.8 | 0.990 (0.004) | 0.4 | 0.0758 (0.0108) | 14.2 | 0.974 (0.016) | 1.6 | −0.0135 (0.0022) | 16.6 | 0.876 (0.044) | 5.0 |
| R_18 | No | 1 | 0.0542 (0.0097) | 18.0 | 0.874 (0.064) | 7.4 | 0.0302 (0.0060) | 19.9 | 0.980 (0.018) | 1.8 | 0.0108 (0.0011) | 9.8 | 0.972 (0.006) | 0.6 |
| mean (sd) | 3 (3) | 0.1167 (0.0579) | 22.5 | 0.934 (0.062) | 4.9 | 0.0473 (0.0446) | 57.2 | 0.852 * (0.191) | 16.3 * | −0.0113 * (0.0161) | 70.5 | 0.705 * (0.262) | 22.2 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aleixo, P.; Fernandes, O.; Patto, J.V.; Abrantes, J. Dynamic Joint Stiffness of the Knee in Post-Menopausal Women with and without Rheumatoid Arthritis. Rheumato 2023, 3, 63-73. https://doi.org/10.3390/rheumato3010005
Aleixo P, Fernandes O, Patto JV, Abrantes J. Dynamic Joint Stiffness of the Knee in Post-Menopausal Women with and without Rheumatoid Arthritis. Rheumato. 2023; 3(1):63-73. https://doi.org/10.3390/rheumato3010005
Chicago/Turabian StyleAleixo, Pedro, Orlando Fernandes, José Vaz Patto, and João Abrantes. 2023. "Dynamic Joint Stiffness of the Knee in Post-Menopausal Women with and without Rheumatoid Arthritis" Rheumato 3, no. 1: 63-73. https://doi.org/10.3390/rheumato3010005
APA StyleAleixo, P., Fernandes, O., Patto, J. V., & Abrantes, J. (2023). Dynamic Joint Stiffness of the Knee in Post-Menopausal Women with and without Rheumatoid Arthritis. Rheumato, 3(1), 63-73. https://doi.org/10.3390/rheumato3010005






