Mindful Eating Approaches to Cardiometabolic Risk Factors: Systematic Review and Meta-Analysis of Intervention Studies
Abstract
1. Introduction
2. Methods
2.1. Data Sources and Search Strategy
2.2. Eligibility Criteria
2.3. Risk of Bias
2.4. Data Extraction
2.5. Data Analysis
3. Results
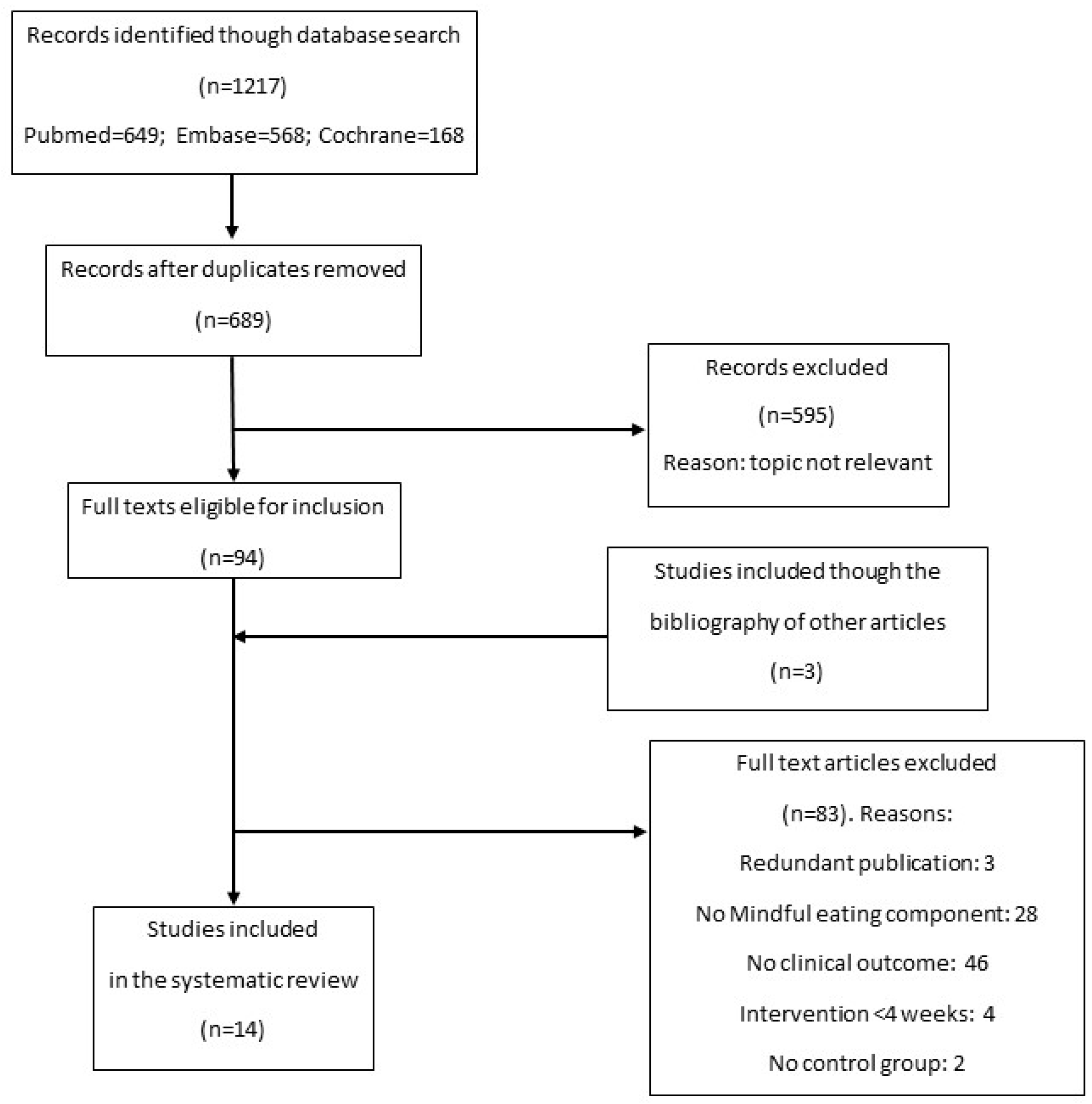
3.1. Study Selection
3.2. Characteristics of the Studies
3.3. Risk of Bias
3.4. Effect on Body Weight
3.5. Effect on Waist Circumference
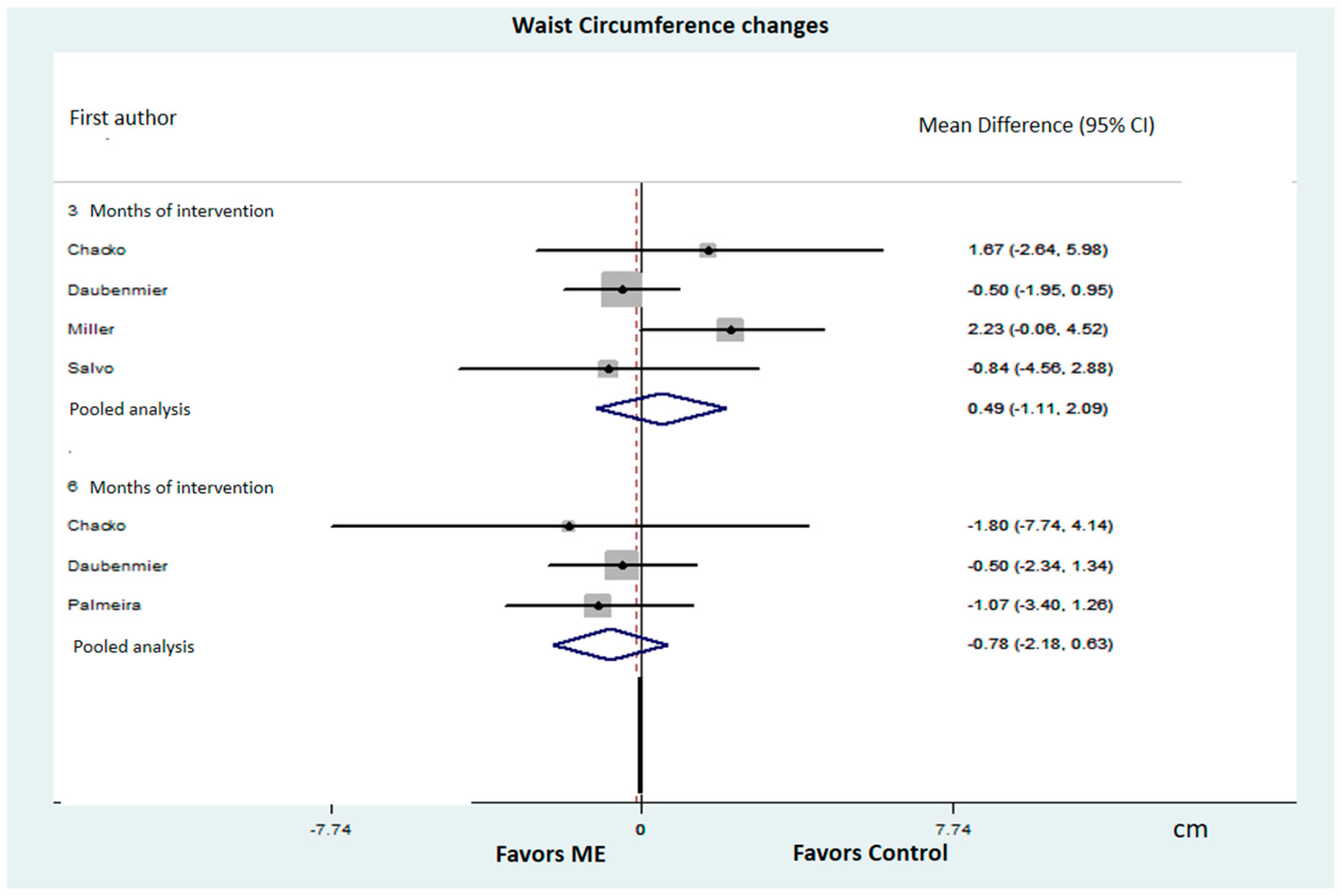
3.6. Effect on Serum Glucose
3.7. Effect on Glycated Hemoglobin
3.8. Effect on C-Reactive Protein
3.9. Effect on Psychological and Behavioral Aspects
4. Discussion
5. Strengths and Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Hofmann, S.G.; Gómez, A.F. Mindfulness-Based Interventions for Anxiety and Depression. Psychiatr. Clin. N. Am. 2017, 40, 739–749. [Google Scholar] [CrossRef] [PubMed]
- Tang, Y.Y.; Tang, R.; Posner, M.I. Mindfulness meditation improves emotion regulation and reduces drug abuse. Drug Alcohol Depend. 2016, 163, S13–S18. [Google Scholar] [CrossRef] [PubMed]
- Hilton, L.; Hempel, S.; Ewing, B.A.; Apaydin, E.; Xenakis, L.; Newberry, S.; Colaiaco, B.; Maher, A.R.; Shanman, R.M.; Sorbero, M.E.; et al. Mindfulness Meditation for Chronic Pain: Systematic Review and Meta-analysis. Ann. Behav. Med. 2017, 51, 199–213. [Google Scholar] [CrossRef] [PubMed]
- Grossman, P.; Niemann, L.; Schmidt, S.; Walach, H. Mindfulness-based stress reduction and health benefits: A meta-analysis. J. Psychosom. Res. 2004, 57, 35–43. [Google Scholar] [CrossRef] [PubMed]
- Ludwig, D.S.; Kabat-Zinn, J. Mindfulness in Medicine. JAMA 2008, 300, 1350–1352. [Google Scholar] [CrossRef] [PubMed]
- Santorelli, S. Heal Thy Self: Lessons on Mindfulness in Medicine; Harmony: New York, NY, USA, 1999. [Google Scholar]
- Iaccarino Idelson, P.; D’elia, L.; Cairella, G.; Sabino, P.; Scalfi, L.; Fabbri, A.; Galletti, F.; Garbagnati, F.; Lionetti, L.; Paolella, G.; et al. Salt and health: Survey on knowledge and salt intake related behaviour in Italy. Nutrients 2020, 12, 279. [Google Scholar] [CrossRef] [PubMed]
- Creswell, J.D.; Way, B.M.; Eisenberger, N.I.; Lieberman, M.D. Neural correlates of dispositional mindfulness during affect labeling. Psychosom. Med. 2007, 69, 560–565. [Google Scholar] [CrossRef] [PubMed]
- Dulloo, A.G.; Jacquet, J.; Montani, J.P. How dieting makes some fatter: From a perspective of human body composition autoregulation. Proc. Nutr. Soc. 2012, 71, 379–389. [Google Scholar] [CrossRef]
- Montani, J.P.; Schutz, Y.; Dulloo, A.G. Dieting and weight cycling as risk factors for cardiometabolic diseases: Who is really at risk? Obes. Rev. 2015, 16, 7–18. [Google Scholar] [CrossRef]
- Zervos, K.; Koletsi, M.; Mantzios, M.; Skopeliti, N.; Tsitsas, G.; Naska, A. An Eight-Week Mindful Eating Program Applied in a Mediterranean Population With Overweight or Obesity: The EATT Intervention Study. Psychol. Rep. 2022, 125, 1011–1040. [Google Scholar] [CrossRef]
- Godsey, J. The role of mindfulness based interventions in the treatment of obesity and eating disorders: An integrative review. Complement. Ther. Med. 2013, 21, 430–439. [Google Scholar] [CrossRef]
- Bays, J.C. Mindful Eating: A Guide to Rediscovering a Healthy and Joyful Relationship with Food; Shambhala Publications: Boulder, CO, USA, 2009. [Google Scholar]
- Kristeller, J.; Wolever, R.Q.; Sheets, V. Mindfulness-Based Eating Awareness Training (MB-EAT) for Binge Eating: A Randomized Clinical Trial. Mindfulness 2014, 5, 282–297. [Google Scholar] [CrossRef]
- Daly, P.; Pace, T.; Berg, J.; Menon, U.; Szalacha, L.A. A mindful eating intervention: A theory-guided randomized anti-obesity feasibility study with adolescent Latino females. Complement. Ther. Med. 2016, 28, 22–28. [Google Scholar] [CrossRef]
- Fuentes Artiles, R.; Staub, K.; Aldakak, L.; Eppenberger, P.; Rühli, F.; Bender, N. Mindful eating and common diet programs lower body weight similarly: Systematic review and meta-analysis. Obes. Rev. 2019, 20, 1619–1627. [Google Scholar] [CrossRef]
- Godfrey, K.M.; Gallo, L.C.; Afari, N. Mindfulness-based interventions for binge eating: A systematic review and meta-analysis. J. Behav. Med. 2015, 38, 348–362. [Google Scholar] [CrossRef] [PubMed]
- Grider, H.S.; Douglas, S.M.; Raynor, H.A. The Influence of Mindful Eating and/or Intuitive Eating Approaches on Dietary Intake: A Systematic Review. J. Acad. Nutr. Diet. 2021, 121, 709–727.e1. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions Version 6.3 (Updated February 2022); Cochrane: London, UK, 2019; Available online: www.training.cochrane.org/handbook (accessed on 30 December 2023).
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- DerSimonian, R.; Laird, N. Meta-analysis in clinical trials. Control Clin. Trials 1986, 7, 177–188. [Google Scholar] [CrossRef]
- Carpenter, K.M.; Vickerman, K.A.; Salmon, E.E.; Javitz, H.S.; Epel, E.S.; Lovejoy, J.C. A Randomized Pilot Study of a Phone-Based Mindfulness and Weight Loss Program. Behav. Med. 2019, 45, 271–281. [Google Scholar] [CrossRef]
- Chacko, S.A.; Yeh, G.Y.; Davis, R.B.; Wee, C.C. A mindfulness-based intervention to control weight after bariatric surgery: Preliminary results from a randomized controlled pilot trial. Complement. Ther. Med. 2016, 28, 13–21. [Google Scholar] [CrossRef]
- Daubenmier, J.; Moran, P.J.; Kristeller, J.; Acree, M.; Bacchetti, P.; Kemeny, M.E.; Dallman, M.; Lustig, R.H.; Grunfeld, C.; Nixon, D.F.; et al. Effects of a mindfulness-based weight loss intervention in adults with obesity: A randomized clinical trial. Obesity 2016, 24, 794–804. [Google Scholar] [CrossRef] [PubMed]
- Mason, A.E.; Epel, E.S.; Aschbacher, K.; Lustig, R.H.; Acree, M.; Kristeller, J.; Cohn, M.; Dallman, M.; Moran, P.J.; Bacchetti, P.; et al. Reduced reward-driven eating accounts for the impact of a mindfulness-based diet and exercise intervention on weight loss: Data from the SHINE randomized controlled trial. Appetite 2016, 100, 86–93. [Google Scholar] [CrossRef] [PubMed]
- Mason, A.E.; Epel, E.S.; Kristeller, J.; Moran, P.J.; Dallman, M.; Lustig, R.H.; Acree, M.; Bacchetti, P.; Laraia, B.A.; Hecht, F.M.; et al. Effects of a mindfulness-based intervention on mindful eating, sweets consumption, and fasting glucose levels in obese adults: Data from the SHINE randomized controlled trial. J. Behav. Med. 2016, 39, 201–213. [Google Scholar] [CrossRef] [PubMed]
- Miller, C.K.; Kristeller, J.L.; Headings, A.; Nagaraja, H.; Miser, W.F. Comparative Effectiveness of a Mindful Eating Intervention to a Diabetes Self-Management Intervention among Adults with Type 2 Diabetes: A Pilot Study. J. Acad. Nutr. Diet. 2012, 112, 1835–1842. [Google Scholar] [CrossRef] [PubMed]
- Palmeira, L.; Pinto-Gouveia, J.; Cunha, M. Exploring the efficacy of an acceptance, mindfulness & compassionate-based group intervention for women struggling with their weight (Kg-Free): A randomized controlled trial. Appetite 2017, 112, 107–116. [Google Scholar] [CrossRef] [PubMed]
- Radin, R.M.; Epel, E.S.; Mason, A.E.; Vaccaro, J.; Fromer, E.; Guan, J.; Prather, A.A. Impact of digital meditation on work stress and health outcomes among adults with overweight: A randomized controlled trial. PLoS ONE 2023, 18, e0280808. [Google Scholar] [CrossRef] [PubMed]
- Salvo, V.; Fernandez Curado, D.; Sanudo, A.; Kristeller, J.; Cabral Schveitzer, M.; Favarato, M.L.; Isidororo, W.; Demarzo, M. Comparative effectiveness of mindfulness and mindful eating programmes among low-income overweight women in primary health care: A randomised controlled pragmatic study with psychological, biochemical, and anthropometric outcomes. Appetite 2022, 177, 106131. [Google Scholar] [CrossRef] [PubMed]
- Smith, B.W.; Shelley, B.M.; Sloan, A.L.; Colleran, K.; Erickson, K. A Preliminary Randomized Controlled Trial of a Mindful Eating Intervention for Post-menopausal Obese Women. Mindfulness 2018, 9, 836–849. [Google Scholar] [CrossRef]
- Spadaro, K.C.; Davis, K.K.; Sereika, S.M.; Gibbs, B.B.; Jakicic, J.M.; Cohen, S.M. Effect of mindfulness meditation on short-term weight loss and eating behaviors in overweight and obese adults: A randomized controlled trial. J. Complement. Integr. Med. 2018, 15, 20160048. [Google Scholar] [CrossRef]
- Youngwanichsetha, S.; Phumdoung, S.; Ingkathawornwong, T. The effects of mindfulness eating and yoga exercise on blood sugar levels of pregnant women with gestational diabetes mellitus. Appl. Nurs. Res. 2014, 27, 227–230. [Google Scholar] [CrossRef]
- Carrière, K.; Khoury, B.; Günak, M.M.; Knäuper, B. Mindfulness-based interventions for weight loss: A systematic review and meta-analysis. Obes. Rev. 2018, 19, 164–177. [Google Scholar] [CrossRef] [PubMed]
- Rogers, J.M.; Ferrari, M.; Mosely, K.; Lang, C.P.; Brennan, L. Mindfulness-based interventions for adults who are overweight or obese: A meta-analysis of physical and psychological health outcomes. Obes. Rev. 2017, 18, 51–67. [Google Scholar] [CrossRef] [PubMed]
- Hofman, W.; Nordgren, L.F. The Psychology of Desire; The Guilford Press: New York, NY, USA, 2016. [Google Scholar]


| Author (Year), Study Design, Country | Study Population Age (Years) | Primary Outcomes | Secondary Outcomes | INT and Follow-Up Duration (Weeks) | Short Description of INT N. of Participants (% Female) | Short Description of CG N. of Participants (% Female) | Main Results |
|---|---|---|---|---|---|---|---|
| Carpenter, 2019 [22] RCT USA | 69 OB adults Age: 47.3 ± 2.4 | Feasibility and acceptability of ME program | WL, Improvement in the approach towards food | INT = 24 Follow-up = 0 | Mind your Weight (MYW): 11 phone calls with mindfulness and ME practices 46 (92%) | Weight Talk: 11 phone calls with counselling based on NIH guidelines + unlimited support phone calls. 23 (92%) |
|
| Chacko, 2016 [23] RCT USA | 18 OB adults 1–5 years post-bariatric surgery Age: 53.9 ± 6.7 | Weight gain prevention and improvements in eating behavior, psychosocial factors, HbA1c, adiponectin, hs-CRP, IL-6, TNF-α | INT = 10 Follow-up = 24 | Mindfulness-Based Intervention (MBI): 10 × 90 min group sessions based on mindfulness (MBSR) and ME (MB-EAT) + ½ day of meditation practice + homework assignment 9 (90%) | Standard care: 1 × 1 h session with a dietitian on nutrition and physical activity guidelines and on strategies to prevent weight gain and improve lifestyle. 9 (78%) |
| |
| Daly, 2016 [15] RCT USA | 23 OB female adolescents Age: 15.4 ± 1.4 | BMI reduction, mindfulness improvement | INT = 6 Follow-up = 10 | Mindful Eating Intervention (MEI): 6 × 90 min group sessions ME, behavioral skills, motivational inputs and information on nutrition and PA 8 (100%) | Standard care: One visit with prescription of diet and PA. 15 (100%) | At 6 weeks:
| |
| Daubenmier, 2016 [24] RCT USA | 194 OB adults Age: 47 ± 13 | WL maintenance at 18 months | Reduction in WC, GLU, TRIG, HDL, LDL, HOMA-IR, HbA1c, hs-CRP, BP | INT = 22 Follow-up = 72 | 16 × 2.5 h sessions (12 weekly + 3 bimonthly + 1 monthly + 1 × 6.5 h session) with GL on nutrition, PA + training based on mindfulness (MBSR and MBCT) and ME (MB-EAT) 100 (79%) | Same protocol, replacing mindfulness and ME with nutrition and PA information, strength training and weight loss discussions. 94(86%) |
|
| Kristeller, 2014 [14] RCT USA | 92 adults with BED Age: 46.6 | Reduction in frequency and dimensions of binge episodes | BMI reduction | INT = 12 Follow-up = 28 | Mindfulness-Based Eating Awareness Training (MB-EAT): 9 × 2 h weekly group sessions + 3 monthly sessions based on mindfulness meditations, ME practices, awareness exercises on physical and emotional hunger and on satiety and homework 39 (82%) |
|
|
| Mason, 2016 [25] RCT USA | 194 OB adults Age: 47 ± 13 | Reduction in the use of food as compensation and in psychological stress | WL | INT = 22 Follow-up = 72 | 5.5-month program based on ME (MB-EAT) and nutrition and PA guidelines (12 × 2.5 h weekly group sessions + 3 bi-monthly + 1 × 6.5 h session) 100 (79%) | Same protocol, replacing mindfulness and ME with nutrition and PA information, muscle relaxation and weight loss discussions. 94 (86%) |
|
| Mason, 2016 [26] RCT USA | 194 OB adults Age: 47 ± 13 | Reduction in sweet consumption and in basal blood glucose at 6 months | Maintenance of results after 12 months, improvement of a more conscious approach towards sweet consumption | INT = 22 Follow-up = 48 | 5.5-month program based on MB-EAT and nutrition and PA guidelines (12 × 2.5 h weekly group sessions + 3 bimonthly + 1 × 6.5 h session) 100 (79%) | Same protocol, replacing mindfulness and ME with nutrition and PA information, muscle relaxation and weight loss discussions. 94 (86%) | At 6 and 12 months:
|
| Miller, 2012 [27] RCT USA | 52 OV diabetic adults Age: 54 ± 8 | Weight loss, BMI reduction | Reduction in WC, HA1c, basal blood glucose, insulin | INT = 12 Follow-up = 24 | MB-EAT-D: 10 × 2.5 h weekly group session + 1 monthly session on ME (MB-EAT) adapted to diabetes 27 (63%) | Smart choices (DSME): Same structure, replacing ME with standard information protocol on diabetes. 25 (64%) |
|
| Palmeira, 2017 [28] RCT Portugal | 73 OV/OB women Age: 42.0 ± 8.5 | Improved quality of life, reduction in weight-related stigma and binge and emotional eating | Reduction in BMI, WC, tot. CHOL and general health and PA improvement | INT = 14 Follow-up = 10 | Kg-free: Standard treatment + 10 × 2.5 h weekly group sessions + 2 sessions every 2 months with meditation, mindfulness and ME practices, self-compassion and kindness + psycho-educational interventions 36 (100%) | Standard treatment: Visits with medical doctors and nutritionists, giving personalized dietetic recommendations + PA prescriptions. 37 (100%) |
|
| Radin, 2023 [29] RCT USA | 161 OV/OB participants with mild/ moderate stress Age: 38 ± 11 | Perceived stress, tolerance for food cravings | Reduction in BMI, WC and binge eating | INT = 8 Follow-up = 0 | Meditation (MED): Participants were provided with a digital meditation app and invited to use it at least for 10 min/day 38 (71%) Meditation + Healthy eating (MED + HE) 40 (68%) | Healthy eating (HE): 1 × 50 min nutritional counselling session + 3 booster phone calls + invitation to follow a digital mindful eating program once/week × 8 weeks with audio exercises inspired by MB-EAT. 41 (83%) Waiting list 42 (67%) |
|
| Salvo, 2022 [30] RCT Brasil | 133 OW/OB women Age: 40.4 ± 10.7 | Improvement of eating behavior | Biochemical control (GLU, TRIG, HbA1c, insulin, tot. CHOL, HDL, LDL, serum cortisol and hs-CRP), body composition improvement, weight and WC reduction | INT = 10 Follow-up = 12 | MB-EAT-SP (MB-EAT adapted to Sao Paulo population) 10 weekly group sessions on mindful meditation, ME practices, awareness of satiety and hunger, homework and greater acceptance regarding eating and weight 45 (100%) Mindfulness-based health promotion (MBHP) + TAU: 10 weekly group sessions based on mindful meditations, mini-meditations, walking meditations and homework 40 (100%) | Treatment as usual (TAU): According to OV/OB rate and of presence of co-morbidities, different actions were planned: from a care plan to achieve a normal BMI range to a dietary prescription and/or behavioral or pharmaco-therapy. 48 (100%) |
|
| Smith, 2018 [31] RCT USA | 36 Post-menopausal OB women Age: 58.5 ± 4.5 | Reduction in BMI, WHR, IL-6, hs-CRP | BED reduction | INT = 6 Follow-up = 48 | MEAL: 6 × 2 h weekly group sessions based on ME(MB-EAT) 18 (100%) | Active control: 6 × 2 h weekly group sessions based on nutritional counselling, goal setting and group support. 18 (100%) |
|
| Spadaro, 2017 [32] RCT USA | 46 OV/OB adults Age: 45.2 ± 8.2 | Weight loss | Caloric intake reduction, improvement in eating behaviors PA and mindfulness | INT = 24 Follow-up = 0 | Standard behavioral WL program + mindfulness and ME: weekly group session for 6 months on nutrition, PA, behavioral changes + 30 min ME practices 22 (90.9%) | Standard behavioral weight loss program, with the same structure as MEI but without mindfulness and ME. 24 (83.3%) |
|
| Youngwanichesetha, 2014 [33] RCT Thailand | 170 women with G-diab Age: 31 ± 5 | Reduction in basal GLU, post-prandial GLU and HbA1c | INT = 8 Follow-up = 0 | Standard diabetes care + 2 × 50 min yoga and ME + encouragement to practice 5 days/week × 8 weeks 85 (100%) | Standard diabetes care 85 (100%) |
|
| Author | Mean Body Weight (kg) ± SD or BMI Change (kg/m2) in MEI Group | Mean Body Weight (kg) ± SD or BMI Change (kg/m2) in Control Group | p |
|---|---|---|---|
| Carpenter, 2019 [22] | At 6 months: −2.4 ± 4.4 kg | At 6 months: −2.6 ± 3.2 kg | 0.68 |
| Chacro, 2016 [23] | At 3 months: +1.0 ± 1.76 kg At 6 months: +2.3 ± 3.5 kg | At 3 months: −0.1 ± 2.4 kg At 6 months: +0.3 ± 2.1 kg | 0.27 0.15 |
| Daly, 2016 [15] | At 1.5 months: −1.1 kg/m2 At 2.5 months: −1.4 kg/m2 | At 1.5 months: +0.72 kg/m2 - | 0.001 |
| Daubenmier, 2016 [24] | At 3 months: −3.9 ± 0.4 kg At 6 months: −5.2 ± 0.6 kg At 12 months: −5.1 ± 0.8 kg At 18 months: −5.0 ± 0.9 kg | At 3 months: −3.3 ± 0.4 kg At 6 months: −4.0 ± 0.7 kg At 12 months: −3.0 ± 0.8 kg At 18 months: −3.2 ± 1.0 kg | 0.34 0.19 0.06 0.2 |
| Kristeller, 2014 [14] | At 1 month: −0.1 kg/m2 At 4 months: +0.5 kg/m2 | At 1 month: −0.5 kg/m2 At 4 months: −0.02 kg/m2 | >0.05 >0.05 |
| Mason, 2016 [25] | At 6 months: −5.6 kg At 12 months: −5.46 kg At 18 months: −5.2 kg | At 6 months: −4.8 kg At 12 months: −4.16 kg At 18 months: −4.35 kg | >0.05 >0.05 >0.05 |
| Miller, 2012 [27] | At 3 months: −1.78 kg At 6 months: −1.53 kg | At 3 months: −3.25 kg At 6 months: −2.92 kg | >0.05 >0.05 |
| Palmeira, 2017 [28] | At 6 months: −0.54 ± 0.92 kg/m2 | At 6 months: −0.07 ± 0.76 kg/m2 | 0.022 |
| Radin, 2023 [29] | At 2 months: −0.66 kg/m2 | At 2 months: +0.06 kg/m2 | 0.29 |
| Smith, 2018 [31] | At 1.5 months: −3.25 kg At 4 months: −4.41 kg At 9 months: −6.09 kg At 12 months: 7.26 kg | At 1.5 months: −3.62 kg At 4 months: −5.2 kg At 9 months: −6.62 kg At 12 months: −6.31 kg | >0.05 >0.05 >0.05 >0.05 |
| Spadaro, 2017 [32] | At 3 months: −5 kg At 6 months: −6.9 kg | At 3 months: −5.1 kg At 6 months: −4.1 kg | >0.05 0.03 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Iaccarino Idelson, P.; D’Elia, L.; Strazzullo, P. Mindful Eating Approaches to Cardiometabolic Risk Factors: Systematic Review and Meta-Analysis of Intervention Studies. Dietetics 2024, 3, 271-288. https://doi.org/10.3390/dietetics3030022
Iaccarino Idelson P, D’Elia L, Strazzullo P. Mindful Eating Approaches to Cardiometabolic Risk Factors: Systematic Review and Meta-Analysis of Intervention Studies. Dietetics. 2024; 3(3):271-288. https://doi.org/10.3390/dietetics3030022
Chicago/Turabian StyleIaccarino Idelson, Paola, Lanfranco D’Elia, and Pasquale Strazzullo. 2024. "Mindful Eating Approaches to Cardiometabolic Risk Factors: Systematic Review and Meta-Analysis of Intervention Studies" Dietetics 3, no. 3: 271-288. https://doi.org/10.3390/dietetics3030022
APA StyleIaccarino Idelson, P., D’Elia, L., & Strazzullo, P. (2024). Mindful Eating Approaches to Cardiometabolic Risk Factors: Systematic Review and Meta-Analysis of Intervention Studies. Dietetics, 3(3), 271-288. https://doi.org/10.3390/dietetics3030022





