Preliminary Study on Associated Risk Factors of Mortality Due to COVID-19 Pandemic in Malaysia †
Abstract
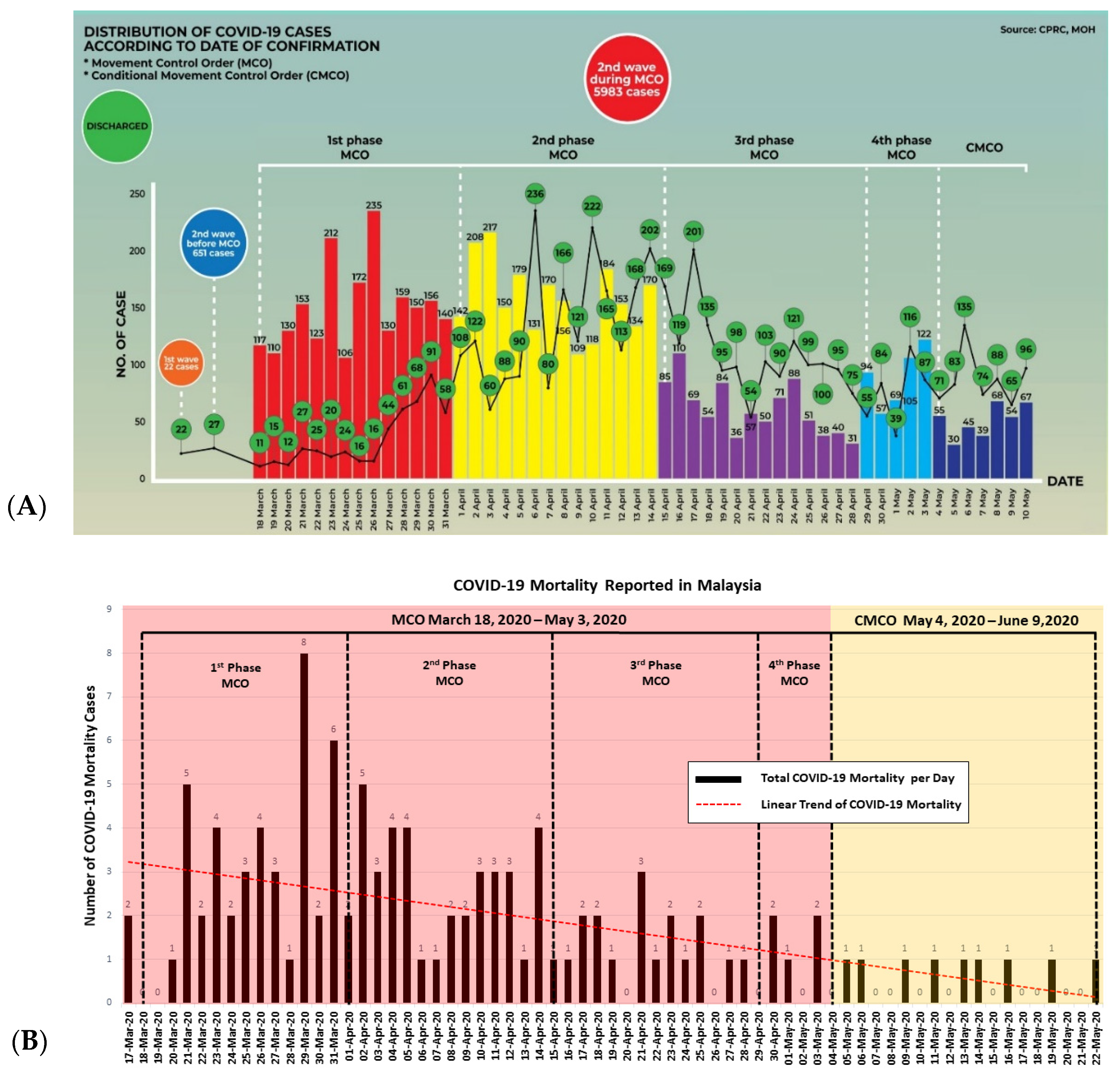
:1. Introduction
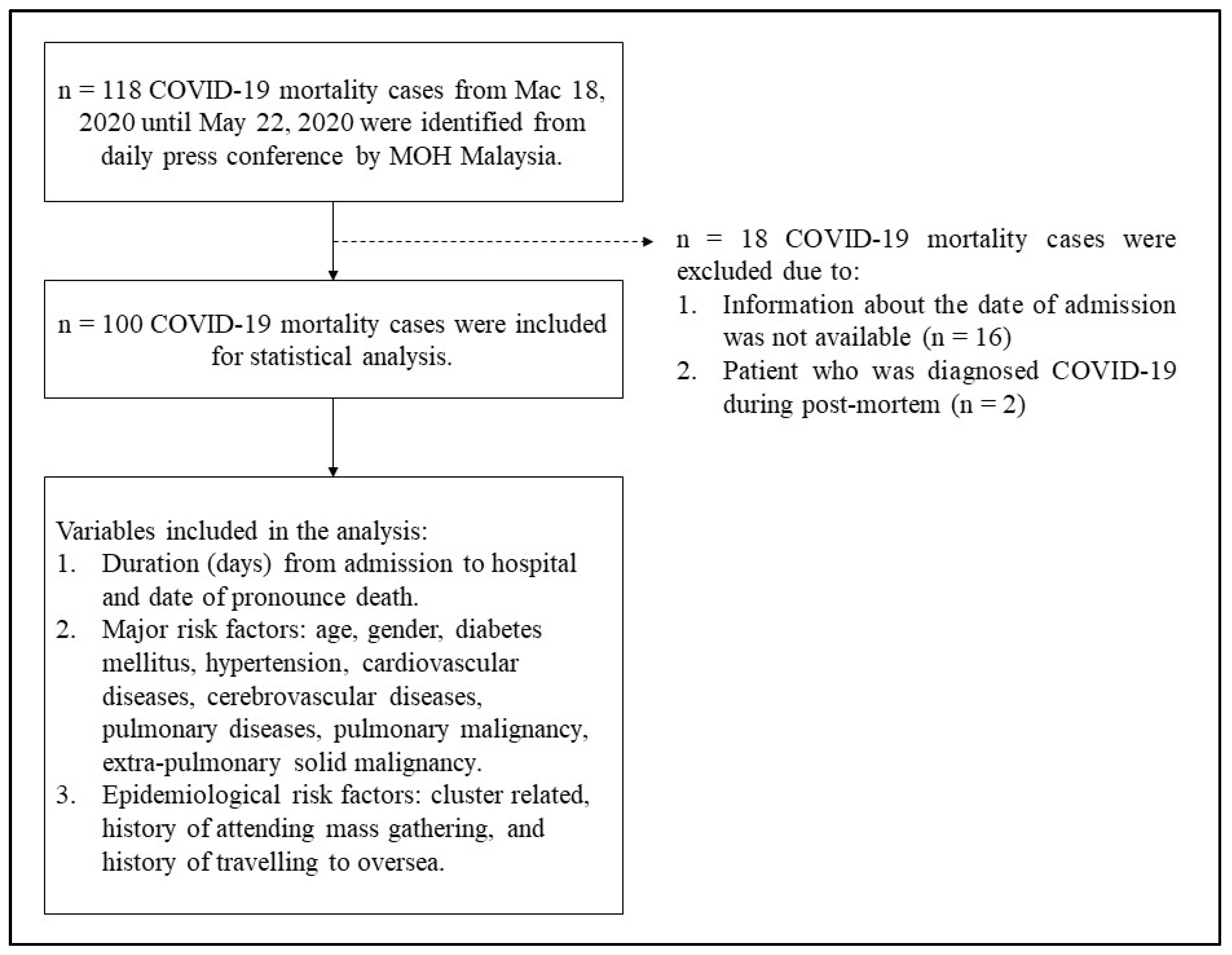
2. Methodology
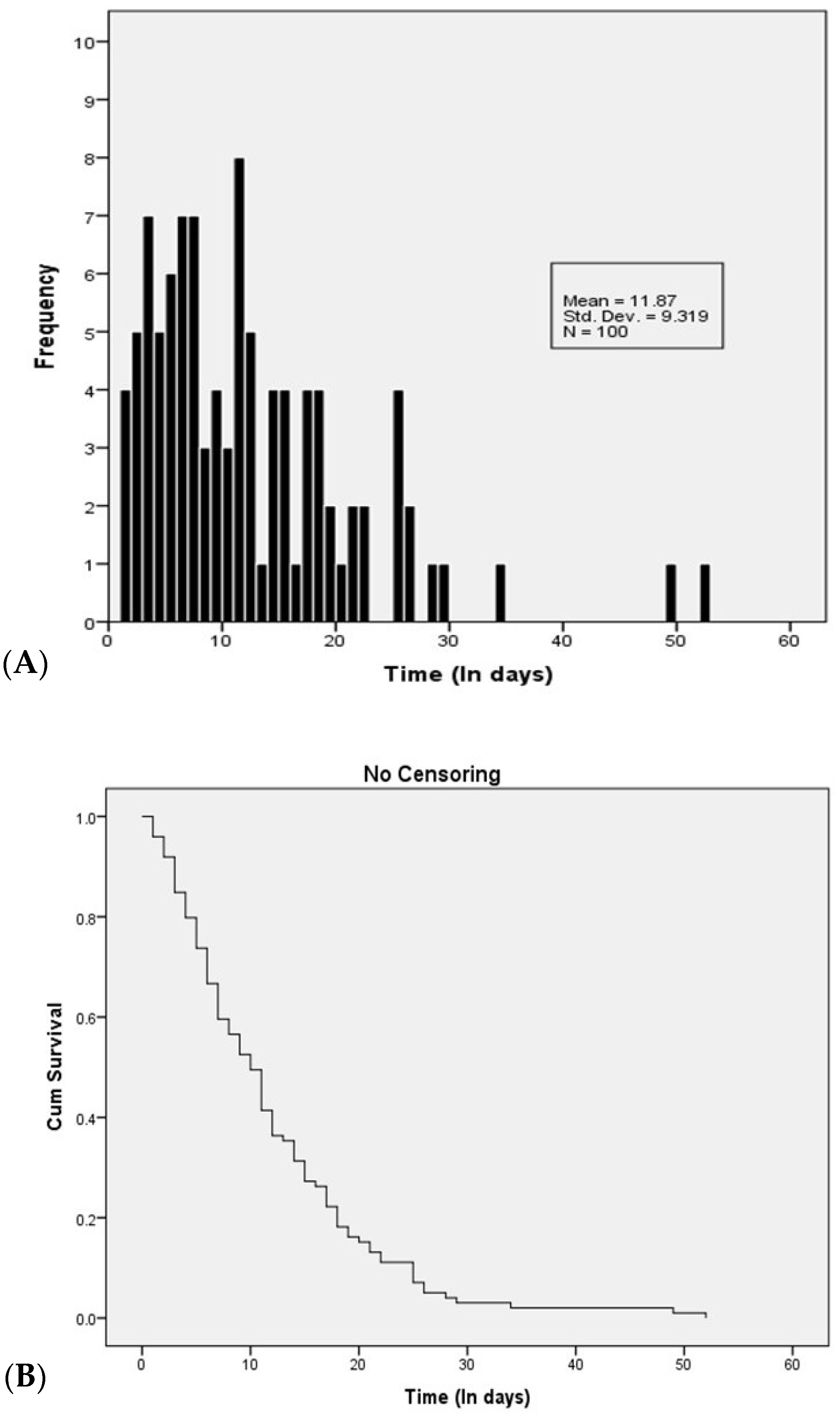
3. Results
4. Discussion
5. Limitation
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Ethics Approval and Consent to Participate
Availability of Data and Materials
Abbreviations
| BMI | Body mass index |
| CHEST | American College of Chest Physicians |
| CMCO | Conditional Movement Control Order |
| COVID-19 | Coronavirus Disease 2019 |
| CPRC | Crisis Preparedness and Response Centre |
| HSB | Sungai Buloh General Hospital |
| MCO | Movement Control Order |
| MERS-CO | Middle East Respiratory Syndrome Coronavirus |
| MOH | Ministry of Health |
| HR | Hazard ratio |
| ICD | International Classification of Disease |
| OR | Odds ratio |
| PHEIC | Public Health Emergency of International Concern |
| PUI | Person under surveillance |
| RNA | Ribonucleic acid |
| SARS-COV | Severe acute respiratory syndrome coronavirus |
| SD | Standard deviation |
| SPSS | Statistical Package for the Social Sciences |
| WHO | World Health Organization |
| UKM | University Kebangsaan Malaysia (National University of Malaysia) |
References
- Centers for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19). Available online: https://www.cdc.gov/coronavirus/2019-ncov/cdcresponse/about-COVID-19.html (accessed on 6 October 2020).
- Zhu, Z.; Lian, X.; Su, X.; Wu, W.; Marraro, G.A.; Zeng, Y. From SARS and MERS to COVID-19: A brief summary and comparison of severe acute respiratory infections caused by three highly pathogenic human coronaviruses. Respir. Res. 2020, 21, 1–14. [Google Scholar] [CrossRef]
- Lai, C.-C.; Shih, T.-P.; Ko, W.-C.; Tang, H.-J.; Hsueh, P.-R. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and corona virus disease-2019 (COVID-19): The epidemic and the challenges. Int. J. Antimicrob. Agents 2020, 55, 105924. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.R.; Cao, Q.D.; Hong, Z.S.; Tan, Y.Y.; Chen, S.D.; Jin, H.J.; Tan, K.S.; Wang, D.Y.; Yan, Y. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak–an update on the status. Mil. Med. Res. 2020, 7, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Abd El-Aziz, T.M.; Stockand, J.D. Recent progress and challenges in drug development against COVID-19 coronavirus (SARS-CoV-2)-an update on the status. Infect. Genet. Evol. 2020, 83, 104327. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control. Total Confirmed Deaths Due to COVID-19. 31 December 2019–6 October 2020. Available online: https://ourworldindata.org/grapher/total-COVID-deaths-region?tab=table&time=2020-01-11..2020-10-06 (accessed on 6 October 2020).
- Ministry of Health Malaysia. Director General of Health Press Statement 5 October 2020-Current Situation of Coronavirus Disease 2019 (COVID-19) in Malaysia. Available online: https://kpkesihatan.com/2020/10/05/kenyataan-akhbar-kpk-5-oktober-2020-situasi-semasa-jangkitan-penyakit-coronavirus-2019-COVID-19-di-malaysia/ (accessed on 14 June 2020).
- Ministry of Health Malaysia. Director General of Health Press Statement 25 January 2020-Detection of New Cases Confirmed Infected 2019 Novel Coronavirus (2019-nCoV) in Malaysia. Available online: https://kpkesihatan.com/2020/01/25/kenyataan-akhbar-kpk-25-januari-2020-pengesanan-kes-baharu-yang-disahkan-dijangkiti-2019-novel-coronavirus-2019-ncov-di-malaysia/ (accessed on 6 October 2020).
- Mat, N.F.C.; Edinur, H.A.; Razab, M.K.A.A.; Safuan, S. A single mass gathering resulted in massive transmission of COVID-19 infections in Malaysia with further international spread. J. Travel Med. 2020, 27, 1–4. [Google Scholar] [CrossRef]
- Ministry of Health Malaysia. Director General of Health Press Statement 13 March 2020-Current Situation of Coronavirus Disease 2019 (COVID-19) in Malaysia. Available online: https://kpkesihatan.com/2020/03/13/kenyataan-akhbar-kpk-13-mac-2020-situasi-semasa-jangkitan-penyakit-coronavirus-2019-COVID-19-di-malaysia/ (accessed on 6 October 2020).
- Ministry of Health Malaysia. Directed General of Health Press Statement 7 April 2020-Current Situation of Coronavirus Disease 2019 (COVID-19) in Malaysia. Available online: https://kpkesihatan.com/2020/04/07/kenyataan-akhbar-kpk-7-april-2020-situasi-semasa-jangkitan-penyakit-coronavirus-2019-COVID-19-di-malaysia/ (accessed on 6 October 2020).
- Zheng, Z.; Peng, F.; Xu, B.; Zhao, J.; Liu, H.; Peng, J.; Li, Q.; Jiang, C.; Zhou, Y.; Liu, S.; et al. Risk factors of critical & mortal COVID-19 cases: A systematic literature review and meta-analysis. J. Infect. 2020, 81, e16–e25. [Google Scholar] [CrossRef]
- Li, X.; Xu, S.; Yu, M.; Wang, K.; Tao, Y.; Zhou, Y.; Shi, J.; Zhou, M.; Wu, B.; Yang, Z.; et al. Risk factors for severity and mortality in adult COVID-19 inpatients in Wuhan. J. Allergy Clin. Immunol. 2020, 146, 110–118. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.; Li, R.; Lu, Z.; Huang, Y. Does comorbidity increase the risk of patients with COVID-19: Evidence from meta-analysis. Aging 2020, 12, 6049. [Google Scholar] [CrossRef]
- Grasselli, G.; Greco, M.; Zanella, A.; Albano, G.; Antonelli, M.; Bellani, G.; Bonanomi, E.; Cabrini, L.; Carlesso, E.; Castelli, G.; et al. Risk factors associated with mortality among patients with COVID-19 in intensive care units in Lombardy, Italy. JAMA Intern. Med. 2020, 180, 1345–1355. [Google Scholar] [CrossRef]
- Wu, Y.-C.; Chen, C.-S.; Chan, Y.-J. The outbreak of COVID-19: An overview. J. Chin. Med. Assoc. 2020, 83, 217. [Google Scholar] [CrossRef]
- Chen, S.; Yang, J.; Yang, W.; Wang, C.; Bärnighausen, T. COVID-19 control in China during mass population movements at New Year. Lancet 2020, 395, 764–766. [Google Scholar] [CrossRef] [Green Version]
- Zhang, L.; Zhu, F.; Xie, L.; Wang, C.; Wang, J.; Chen, R.; Jia, P.; Guan, H.Q.; Peng, L.; Chen, Y.; et al. Clinical characteristics of COVID-19-infected cancer patients: A retrospective case study in three hospitals within Wuhan, China. Ann. Oncol. 2020, 31, 894–901. [Google Scholar] [CrossRef] [PubMed]
- Westblade, L.F.; Brar, G.; Pinh, L.C.; Paid, D.; Rajan, M.; Martin, P.; Goyal, P.; Sepulveda, J.L.; Zhang, L.; George, G.; et al. SARS-CoV-2 viral load predicts mortality in patients with and without cancer who are hospitalized with COVID-19. Cancer Cell 2020, 38, 661–671. [Google Scholar] [CrossRef]
- Mehta, V.; Goel, S.; Kabarriti, R.; Cole, D.; Goldfinger, M.; Acuna-Villaorduna, A.; Pradhan, K.; Thota, R.; Reissman, S.; Sparano, J.A.; et al. Case fatality rate of cancer patients with COVID-19 in a New York hospital system. Cancer Discov. 2020, 10, 935–941. [Google Scholar] [CrossRef] [PubMed]
- Department of Statistics Malaysia. Demographic Statistics First Quarter 2020, Malaysia. Released by Dato’ Sri Dr. Mohd Uzir Mahidin, Chief Statistician Malaysia, Department of Statistics Malaysia. Available online: https://www.dosm.gov.my/v1/index.php?r=column/cthemeByCat&cat=430&bul_id=aFYzVjJ3anNyQytHZGxzcUZxTG9Ydz09&menu_id=L0pheU43NWJwRWVSZklWdzQ4TlhUUT09 (accessed on 14 June 2020).
- Ministry of Health Malaysia. Guidelines COVID-19 Management No. 5/2020 Update on 24 March 2020. Available online: http://www.umk.edu.my/covid19/doc/Garispanduan-COVID19-Edisi-5_2020.pdf (accessed on 14 June 2020).
- Ministry of Health Malaysia. The List of District Health Office in Malaysia. Available online: https://www.moh.gov.my/index.php/database_stores/store_view/5?items=25&page=1 (accessed on 14 June 2020).
- Ministry of Health Malaysia. From the Desk of the Director-General of Health Malaysia. Available online: https://kpkesihatan.com/ (accessed on 6 October 2020).
- European Centre for Disease Prevention and Control. Our World in Data. Case Fatality Rate of the Ongoing COVID-19 Pandemic. Available online: https://ourworldindata.org/coronavirus-data-explorer?zoomToSelection=true&time=2020-03-14..latest&country=OWID_WRL~BRN~MYS~THA~VNM~IDN~PHL~GBR~USA®ion=World&cfrMetric=true&interval=total&aligned=true&hideControls=true&smoothing=0&pickerMetric=location&pickerSort=asc (accessed on 6 October 2020).
- Ministry of Health Malaysia. From the Desk of the Director-General of Health Malaysia-The Malaysian Response to COVID-19: Building Preparedness for ‘Surge Capacity’, Testing Efficiency, and Containment. Available online: https://kpkesihatan.com/2020/06/16/the-malaysian-response-to-COVID-19-building-preparedness-for-surge-capacity-testing-efficiency-and-containment/ (accessed on 18 August 2020).
- Ministry of Health Malaysia. Press Release Ministry of Health Malaysia. Current Situation During Coronavirus Disease Infection 2019 (COVID-19) in Malaysia 31 March 2020. Available online: https://www.moh.gov.my/index.php/database_stores/attach_download/337/1410 (accessed on 18 August 2020).
- Ministry of Health Malaysia. Press Release Ministry of Health Malaysia. Current Situation During Coronavirus Disease Infection 2019 (COVID-19) in Malaysia 7 April 2020. Available online: https://www.moh.gov.my/index.php/database_stores/attach_download/337/1431 (accessed on 18 August 2020).
- Promislow, D.E.L. A Geroscience Perspective on COVID-19 Mortality. J. Gerontol. Ser. A 2020, 75, e30–e33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, C.; Chen, X.; Cai, Y.; Zhou, X.; Xu, S.; Huang, H.; Zhang, L.; Zhou, X.; Du, C.; Zhang, Y.; et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern. Med. 2020, 180, 934–943. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Institute for Public Health Malaysia. National Health and Morbidity Survey (NHMS) 2019. Non-Communicable Diseases, Healthcare Demand, and Health Literacy: Key Findings. Available online: http://iku.moh.gov.my/images/IKU/Document/REPORT/NHMS2019/Infographic_Booklet_NHMS_2019-English.pdf (accessed on 6 October 2020).
- Moser, J.A.S.; Galindo-Fraga, A.; Ortiz-Hernández, A.A.; Gu, W.; Hunsberger, S.; Galán-Herrera, J.F.; Guerrero, M.L.; Ruiz-Palacios, G.M.; Beigel, J.H.; La Red ILI 002 Study Group; et al. Underweight, overweight, and obesity as independent risk factors for hospitalization in adults and children from influenza and other respiratory viruses. Influenza Other Respir. Viruses 2019, 13, 3–9. [Google Scholar] [CrossRef]
- Ong, S.W.X.; Young, B.E.; Leo, Y.-S.; Lye, D.C. Association of Higher Body Mass Index With Severe Coronavirus Disease 2019 (COVID-19) in Younger Patients. Clin. Infect. Dis. 2020, 71, 2300–2302. [Google Scholar] [CrossRef]
- Lighter, J.; Phillips, M.; Hochman, S.; Sterling, S.; Johnson, D.; Francois, F.; Stachel, A. Obesity in patients younger than 60 years is a risk factor for COVID-19 hospital admission. Clin. Infect. Dis. 2020, 71, 896–897. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Luo, J.; Rizvi, H.; Preeshagul, I.R.; Egger, J.V.; Hoyos, D.; Bandlamudi, C.; McCarthy, C.G.; Falcon, C.J.; Schoenfeld, A.J.; Arbour, K.C.; et al. COVID-19 in patients with lung cancer. Ann. Oncol. 2020, 31, 1386–1396. [Google Scholar] [CrossRef]
- Dai, M.; Liu, D.; Liu, M.; Zhou, F.; Li, G.; Chen, Z.; Zhang, Z.; You, H.; Wu, M.; Zheng, Q.; et al. Patients with cancer appear more vulnerable to SARS-COV-2: A multicenter study during the COVID-19 outbreak. Cancer Discov. 2020, 10, 783–791. [Google Scholar] [CrossRef] [PubMed]
- Kabarriti, R.; Brodin, N.P.; Maron, M.I.; Tomé, W.A.; Halmos, B.; Guha, C.; Kalnicki, S.; Garg, M.K.; Ohri, N. Extent of prior lung irradiation and mortality in COVID-19 patients with a cancer history. Adv. Radiat. Oncol. 2020, 5, 707–710. [Google Scholar] [CrossRef]
- Singh, A.P.; Berman, A.T.; Marmarelis, M.E.; Haas, A.R.; Feigenberg, S.J.; Braun, J.; Ciunci, C.A.; Bauml, J.M.; Cohen, R.B.; Kucharczuk, J.C.; et al. Management of lung cancer during the COVID-19 pandemic. JCO Oncol. Pract. 2020, 16, 579–586. [Google Scholar] [CrossRef] [PubMed]
- Mazzone, P.J.; Gould, M.K.; Arenberg, D.A.; Chen, A.C.; Choi, H.K.; Detterbeck, F.C.; Farjah, F.; Fong, K.M.; Iaccarino, J.M.; Janes, S.M.; et al. Management of lung nodules and lung cancer screening during the COVID-19 pandemic: CHEST expert panel report. Chest 2020, 158, 406–415. [Google Scholar] [CrossRef] [PubMed]
- Burki, T.K. Cancer guidelines during the COVID-19 pandemic. Lancet Oncol. 2020, 21, 629–630. [Google Scholar] [CrossRef]
- Xu, Y.; Liu, H.; Hu, K.; Wang, M. Clinical recommendations on lung cancer management during the COVID-19 pandemic. Thorac. Cancer 2020, 11, 2067–2074. [Google Scholar] [CrossRef]
- Ebrahim, S.H.; Memish, Z.A. COVID-19–the role of mass gatherings. Travel Med. Infect. Dis. 2020, 34, 101617. [Google Scholar] [CrossRef]
- Parnell, D.; Widdop, P.; Bond, A.; Wilson, R. COVID-19, networks and sport. Manag. Sport Leis. 2020, 25, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Ministry of Health Malaysia. Director General of Health Press Statement 18 July 2020-Current Situation of Coronavirus Disease 2019 (COVID-19) in Malaysia. Available online: https://kpkesihatan.com/2020/07/08/kenyataan-akhbar-kpk-8-julai-2020-situasi-semasa-jangkitan-penyakit-coronavirus-2019-COVID-19-di-malaysia/ (accessed on 16 August 2020).
- Studdert, D.M.; Hall, M.A.; Mello, M.M. Partitioning the Curve—Interstate Travel Restrictions During the COVID-19 Pandemic. N. Engl. J. Med. 2020, 383, e83. [Google Scholar] [CrossRef]
- Chinazzi, M.; Davis, J.T.; Ajelli, M.; Gioannini, C.; Litvinova, M.; Merler, S.; y Piontti, A.P.; Mu, K.; Rossi, L.; Sun, K.; et al. The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak. Science 2020, 368, 395–400. [Google Scholar] [CrossRef] [Green Version]
- Anzai, A.; Kobayashi, T.; Linton, N.M.; Kinoshita, R.; Hayashi, K.; Suzuki, A.; Yang, Y.; Jung, S.M.; Miyama, T.; Akhmetzhanov, A.R.; et al. Assessing the impact of reduced travel on exportation dynamics of novel coronavirus infection (COVID-19). J. Clin. Med. 2020, 9, 601. [Google Scholar] [CrossRef] [Green Version]
- Kraemer, M.U.; Yang, C.H.; Gutierrez, B.; Wu, C.H.; Klein, B.; Pigott, D.M.; Du Plessis, L.; Faria, N.R.; Li, R.; Hanage, W.P.; et al. The effect of human mobility and control measures on the COVID-19 epidemic in China. Science 2020, 368, 493–497. [Google Scholar] [CrossRef] [Green Version]
- Tang, K.H.D. Movement control as an effective measure against COVID-19 spread in Malaysia: An overview. J. Public Health 2020, 28, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Gill, B.S.; Jayaraj, V.J.; Singh, S.; Mohd Ghazali, S.; Cheong, Y.L.; Md Iderus, N.H.; Sundram, B.M.; Aris, T.B.; Mohd Ibrahim, H.; Hong, B.H.; et al. Modelling the Effectiveness of Epidemic Control Measures in Preventing the Transmission of COVID-19 in Malaysia. Int. J. Environ. Res. Public Health 2020, 17, 5509. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, N.; Bauer, G. Apparent difference in fatalities between Central Europe and East Asia due to SARS-COV-2 and COVID-19: Four hypotheses for possible explanation. Med. Hypotheses 2020, 144, 110160. [Google Scholar] [CrossRef]
- Gonzalez-Reiche, A.S.; Hernandez, M.M.; Sullivan, M.J.; Ciferri, B.; Alshammary, H.; Obla, A.; Fabre, S.; Kleiner, G.; Polanco, J.; Khan, Z.; et al. Introductions and early spread of SARS-CoV-2 in the New York City area. Science 2020, 369, 297–301. [Google Scholar] [CrossRef]
- Toyoshima, Y.; Nemoto, K.; Matsumoto, S.; Nakamura, Y.; Kiyotani, K. SARS-CoV-2 genomic variations associated with mortality rate of COVID-19. J. Hum. Genet. 2020, 65, 1075–1082. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health Malaysia. Director General of Health Press Statement 5 April 2020-Current Situation of Coronavirus Disease 2019 (COVID-19) in Malaysia. Available online: https://kpkesihatan.com/2020/04/05/kenyataan-akhbar-kpk-5-april-2020-situasi-semasa-jangkitan-penyakit-coronavirus-2019-COVID-19-di-malaysia/ (accessed on 6 October 2020).
- Department of Personal Data Protection Malaysia. Act 709, Personal Data Protection Act. Available online: https://www.pdp.gov.my/jpdpv2/assets/2019/09/Personal-Data-Protection-Act-2010.pdf (accessed on 6 October 2020).
- Department of Personal Data Protection Malaysia. Federal Government Gazette. P.U. (A) 335, Personal Data Protection Regulations 2013. Available online: https://www.pdp.gov.my/jpdpv2/assets/2019/09/Peraturan-peraturan_Perlindungan_Data_Peribadi.pdf (accessed on 6 October 2020).
| Parameter | n (%) | Mean ± SD |
|---|---|---|
| Mortality cases according to state | ||
| Federal Territory of Kuala Lumpur | 27 (27.00) | |
| Johor state | 17 (17.00) | |
| Sarawak state | 14 (14.00) | |
| Selangor state | 9 (9.00) | |
| Negeri Sembilan state | 8 (8.00) | |
| Other states | 25 (25.00) | |
| Age group | ||
| 60 years old and below | 31 (31.00) | |
| More than 60 years old | 69 (69.00) | |
| Age (years) | 64.01 ± 14.91 | |
| Gender | ||
| Male | 78 (78.00) | |
| Female | 22 (22.00) | |
| Diabetes Mellitus | ||
| Yes | 43 (43.0) | |
| No | 57 (57.00) | |
| Hypertension | ||
| Yes | 52 (52.00) | |
| No | 48 (48.00) | |
| Cardiovascular Diseases | ||
| Yes | 21 (21.00) | |
| No | 79 (79.00) | |
| Cerebrovascular Diseases | ||
| Yes | 3 (3.00) | |
| No | 97 (97.00) | |
| Pulmonary Diseases | ||
| Yes | 1 (1.00) | |
| No | 99 (99.00) | |
| Pulmonary Malignancy | ||
| Yes | 1 (1.00) | |
| No | 99 (99.00) | |
| Extra-Pulmonary Solid Malignancy | ||
| Yes | 5 (5.00) | |
| No | 95 (95.00) | |
| Established Cluster– Related | ||
| Yes | 23 (23.00) | |
| No | 77 (77.00) | |
| Mass Gathering–Related | ||
| Yes | 15 (15.00) | |
| No | 85 (85.00) | |
| Travelling to Overseas–Related | ||
| Yes | 5 (5.00) | |
| No | 95 (95.00) |
| Group (Parameter) | Mean | Median | Log Rank | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | Survival Time | Standard Error | 95% CI | Survival Time | Standard Error | 95% CI | Statistic | df | Sig. | |
| Age Group | 7.178 | 1 | 0.007 * | |||||||
| 60 years old and below | 31 | 8.74 | 1.66 | 5.50, 11.99 | 6.00 | 0.93 | 4.18, 7.82 | |||
| More than 60 years old | 69 | 13.28 | 1.09 | 11.13, 15.42 | 11.00 | 0.83 | 9.37, 12.63 | |||
| Gender | 0.099 | 1 | 0.753 | |||||||
| Male | 78 | 12.09 | 1.07 | 9.99, 14.19 | 10.00 | 1.20 | 7.64, 12.36 | |||
| Female | 22 | 11.09 | 1.90 | 7.37, 14.81 | 6.00 | 2.01 | 2.06, 9.94 | |||
| Diabetes Mellitus | 2.738 | 1 | 0.098 | |||||||
| Yes | 43 | 13.77 | 1.48 | 10.93, 16.60 | 12.00 | 1.87 | 8.33, 15.67 | |||
| No | 57 | 10.44 | 1.19 | 8.10, 12.78 | 7.00 | 1.68 | 3.71, 10.29 | |||
| Hypertension | 2.818 | 1 | 0.093 | |||||||
| Yes | 52 | 13.44 | 1.28 | 10.93, 15.96 | 11.00 | 1.31 | 8.43, 13.57 | |||
| No | 48 | 10.17 | 1.33 | 7.57, 12.77 | 7.00 | 1.15 | 4.74, 9.26 | |||
| Cardiovascular Diseases | 0.166 | 1 | 0.684 | |||||||
| Yes | 21 | 12.24 | 1.90 | 8.52, 15.96 | 11.00 | 2.84 | 5.44, 16.56 | |||
| No | 79 | 11.77 | 1.07 | 9.67, 13.87 | 10.00 | 1.03 | 7.99, 12.01 | |||
| Cerebrovascular Diseases | 1.615 | 1 | 0.204 | |||||||
| Yes | 3 | 21.00 | 2.31 | 16.47, 25.53 | 21.00 | 3.27 | 14.60, 27.40 | |||
| No | 97 | 11.59 | 0.95 | 9.74, 13.44 | 10.00 | 1.09 | 7.86, 12.14 | |||
| Pulmonary Disease | 1.310 | 1 | 0.252 | |||||||
| Yes | 1 | 26.00 | 0.00 | 26.00, 26.00 | 26.00 | - | - | |||
| No | 99 | 11.73 | 0.93 | 9.90, 13.55 | 10.00 | 1.00 | 8.05, 11.95 | |||
| Pulmonary Malignancy | 4.349 | 1 | 0.037 * | |||||||
| Yes | 1 | 3.00 | 0.00 | 3.00, 3.00 | 3.00 | - | - | |||
| No | 99 | 11.96 | 0.94 | 10.12, 13.80 | 10.00 | 1.00 | 8.05, 11.95 | |||
| Extra-Pulmonary Solid Malignancy | 0.825 | 1 | 0.364 | |||||||
| Yes | 5 | 8.40 | 3.74 | 1.08, 15.72 | 3.00 | 1.10 | 0.85, 5.15 | |||
| No | 95 | 12.05 | 0.96 | 10.17, 13.94 | 10.00 | 0.98 | 8.09, 11.91 | |||
| Established Cluster Related | 0.898 | 1 | 0.343 | |||||||
| Yes | 23 | 10.48 | 1.29 | 7.96, 13.00 | 10.00 | 1.20 | 7.65, 12.35 | |||
| No | 77 | 12.29 | 1.15 | 10.04, 14.53 | 10.00 | 1.46 | 7.13, 12.87 | |||
| Mass Gathering Related | 6.883 | 1 | 0.009 * | |||||||
| Yes | 15 | 7.67 | 0.81 | 6.08, 9.25 | 7.00 | 0.97 | 5.11, 8.89 | |||
| No | 85 | 12.61 | 1.07 | 10.52, 14.71 | 1.00 | 1.32 | 8.42, 13.58 | |||
| Travelling to Overseas Related | 7.218 | 1 | 0.007 * | |||||||
| Yes | 4 | 4.50 | 1.76 | 1.06, 7.49 | 2.00 | 3.00 | 0.00, 7.88 | |||
| No | 96 | 12.18 | 0.96 | 10.30, 14.05 | 11.00 | 0.97 | 9.10, 12.90 | |||
| Parameter | B | SE | Wald | df | Sig. | Exp (B) | 95% CI for Exp (B) |
|---|---|---|---|---|---|---|---|
| Age Group | 0.463 | 0.279 | 2.745 | 1 | 0.098 | 1.589 | 0.919, 2.747 |
| Gender | −0.079 | 0.269 | 0.085 | 1 | 0.770 | 0.924 | 0.546, 1.566 |
| Diabetes Mellitus | 0.032 | 0.268 | 0.014 | 1 | 0.906 | 1.032 | 0.610, 1.746 |
| Hypertension | −0.066 | 0.265 | 0.061 | 1 | 0.805 | 0.936 | 0.557, 1.575 |
| Cardiovascular Disease | 0.115 | 0.282 | 0.167 | 1 | 0.682 | 1.122 | 0.646, 1.952 |
| Cerebrovascular Disease | −0.585 | 0.611 | 0.918 | 1 | 0.338 | 0.557 | 0.168, 1.844 |
| Pulmonary Disease | 0.893 | 1.046 | 0.728 | 1 | 0.394 | 2.442 | 0.314, 18.983 |
| Pulmonary Malignancy | 1.707 | 1.081 | 2.492 | 1 | 0.114 | 5.512 | 0.662, 45.899 |
| Extra Pulmonary Solid Malignancy | 0.772 | 0.530 | 2.126 | 1 | 0.145 | 2.165 | 0.767, 6.112 |
| Established Cluster Related | 0.544 | 0.377 | 2.085 | 1 | 0.149 | 1.723 | 0.823, 3.606 |
| Mass Gathering Related | −1.234 | 0.467 | 6.978 | 1 | 0.008 * | 3.434 | 1.375, 8.579 |
| Travelling to Overseas Related | 0.811 | 0.628 | 1.668 | 1 | 0.197 | 2.251 | 0.657, 7.711 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wahil, M.S.A.; Jaafar, M.H.; Ismail, R.; Chua, S.P.; Jeevananthan, C.; Sandhu, R.S.; Madrim, M.F.; Haddi, A.A.A. Preliminary Study on Associated Risk Factors of Mortality Due to COVID-19 Pandemic in Malaysia. Med. Sci. Forum 2021, 4, 8. https://doi.org/10.3390/ECERPH-3-09022
Wahil MSA, Jaafar MH, Ismail R, Chua SP, Jeevananthan C, Sandhu RS, Madrim MF, Haddi AAA. Preliminary Study on Associated Risk Factors of Mortality Due to COVID-19 Pandemic in Malaysia. Medical Sciences Forum. 2021; 4(1):8. https://doi.org/10.3390/ECERPH-3-09022
Chicago/Turabian StyleWahil, Mohd Shahrol Abd, Mohd Hasni Jaafar, Rohaya Ismail, Su Peng Chua, Chandrika Jeevananthan, Rakesh Singh Sandhu, Mohd Faizal Madrim, and Ammar Amsyar Abdul Haddi. 2021. "Preliminary Study on Associated Risk Factors of Mortality Due to COVID-19 Pandemic in Malaysia" Medical Sciences Forum 4, no. 1: 8. https://doi.org/10.3390/ECERPH-3-09022
APA StyleWahil, M. S. A., Jaafar, M. H., Ismail, R., Chua, S. P., Jeevananthan, C., Sandhu, R. S., Madrim, M. F., & Haddi, A. A. A. (2021). Preliminary Study on Associated Risk Factors of Mortality Due to COVID-19 Pandemic in Malaysia. Medical Sciences Forum, 4(1), 8. https://doi.org/10.3390/ECERPH-3-09022






