1. Introduction
The coronavirus disease 2019 (COVID-19) pandemic has resulted in over 244 million known infections and 4.9 million deaths as of October 2021 [
1] and has had a tremendous impact on the world’s society and economy in a relatively short period of time. Until vaccines or therapeutic medications for COVID-19 become fully available, many countries and regions are forced to adopt physical distancing measures, such as self-quarantine, lockdowns, and/or stay-at-home orders/requests to prevent the spread of the disease. However, measures that restrict people’s activities may cause unintended health problems owing to a reduction in exercise, as well as mental health problems because of a lack of social contact. In particular, Japanese people are susceptible to so-called “peer pressure” and tend to voluntarily restrict their activities even in the absence of strict regulations, which may make them more likely to be adversely affected by countermeasures than by infectious diseases themselves.
The incidence of heat stroke is a growing health problem that is increasing with global warming. In Japan, older adults account for a high proportion of heat stroke patients, and most of these cases arise in the home [
2]. One of the best ways to prevent heat stroke indoors is to use proper air conditioning. However, sustained cooling in a closed room can lead to poor indoor ventilation and increase the risk of respiratory infections, such as COVID-19. In early summer 2020, concerns were raised that a request to not go outside and the wearing of face masks to prevent transmission might increase the incidence of heat stroke; however, this relationship has not been investigated. In this study, we analyzed emergency transport data from Tottori Prefecture, where the number of COVID-19 cases has been low, to evaluate the indirect effect of COVID-19 measures on the incidence of heat stroke in a provincial prefecture of Japan.
2. Materials and Methods
This study was conducted with data from Tottori Prefecture, which is located in western Japan and has the smallest population (551,402 in October 2020) of all the 47 prefectures in the country. The daily number of new COVID-19 cases and the date on which the COVID-19 Tottori Alert (the warning system of Tottori Prefecture) was issued were obtained from Tottori Prefecture’s COVID-19 website.
The number of daily ambulance transports for heat stroke was obtained from the Department of Health and Welfare of Tottori Prefecture, which identified a total of 426 of these cases from April to October 2020. A total of 1465 heat stroke cases from April to October for the years 2017 to 2019 combined were selected as the control group. The following parameters were compared between the control cases and the 2020 heat stroke cases: mean age, age structure, and whether the heat stroke occurred at home, at work (excluding agriculture work), during exercise (indoors and outdoors), outside (excluding work, events, and tourism), during agricultural work, while watching an outdoor event, during tourist activities, or under other circumstances. The patient’s medical condition and diagnosis were determined by the emergency room physician based on the International Classification of Diseases, 10th revision (T67: Effects of heat and light), when the patient arrived at the hospital.
The Japan Meteorological Agency provided air temperature data for Tottori City, the capital of Tottori Prefecture.
Descriptive statistics, one-way analysis of variance, and the χ2 test were used in the analysis, and the significance level was set at 5%. The analyses were conducted in SPSS version 24.0 (IBM-SPSS, Armonk, NY, USA).
The study was approved by the Tottori University Ethics Committee (No. 18A024).
3. Results
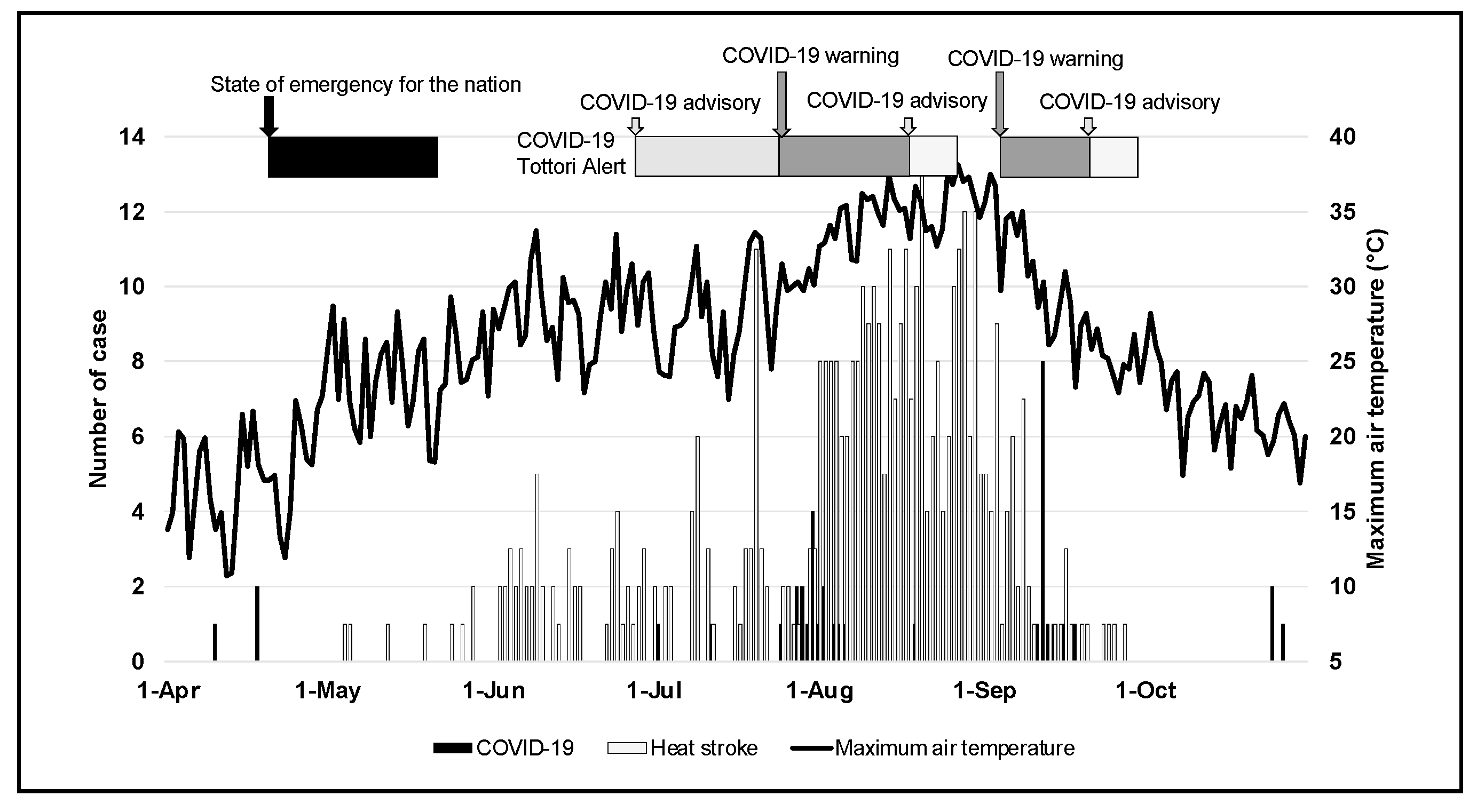
The first COVID-19 case in Tottori Prefecture was reported on 10 April 2020, and a total of 38 cases were reported by the end of October 2020. As of the end of October 2020, Tottori Prefecture ranked 46th in Japan for the number of COVID-19 cases (the 45th ranking prefecture had 68.35 cases per million people). In response to the growing number of COVID-19 cases, the Japanese government declared a state of emergency on 16 April 2020, which was lifted on 14 May 2020. Although the Japanese government requested people to quarantine themselves, this was a voluntary measure. Tottori Prefecture issued COVID-19 Tottori Alerts in response to the outbreak of cases in the prefecture, but these were requests to residents and were not enforceable. A COVID-19 Tottori Alert was issued on the following dates: “Advisory”, 2–14 July 2020 (Eastern District); 12–25 July (Western District); 25–28 July (Eastern District); 21 August–2 September (Western District); 22 September–2 October (Western District), and “Warning”, 29 July (Eastern District); 30 July–20 August (Prefecture-wide); 12–22 September (Prefecture-wide).
Figure 1 shows the daily number of new cases of COVID-19 and the issuance of local government alerts in Tottori Prefecture.
The average minimum and maximum temperatures in Tottori City from April to October for the years 2017 to 2019 are shown in
Table 1. In 2020, the average July temperature was lower than in previous years; the average August temperature was higher than usual and was the highest ever recorded in Tottori City.
The mean age (±standard deviation) of heat stroke-related emergency transport patients from 2017–2020 was 60.0 ± 27.9, 57.4 ± 27.9, 57.6 ± 26.9, and 66.2 ± 24.0 years, respectively. The mean age in 2020 was significantly higher than in previous years (
Table 2). In 2020, the percentage of those under 18 was 8.0%, which was lower than in previous years (14.9–18.0%), and the percentage of those over 75 was 47.7%, which was higher than in previous years (35.6–44.2%). Regarding the circumstances of heat stroke, in 2020, 36.9% of all incidents occurred in the person’s residence, which was higher than in previous years (26.6–29.3%), and 11.3% were associated with exercise, which was lower than in previous years (18.2–20.4%). In 2020, the percentage of heat stroke cases associated with agricultural work (17.1%) was also higher than in other years (8.1–12.5%) (
Table 3).
According to information from the Fire Department, there were no cases of heat stroke transport associated with mask-wearing.
4. Discussion
The proportion of elderly people among all the heat stroke patients has been high in Tottori Prefecture [
3]. The current study found that this trend was amplified in 2020. In addition, the frequency of heat stroke cases arising in residences was higher than in previous years. The typical circumstance of a heat stroke incident in Japan is an elderly person suffering from heat stroke at home. This trend became more obvious in 2020, presumably owing to the indirect effect of the COVID-19 voluntary restrictions. In Japan, due to constitutional and legal restrictions, the government could not legally enforce lockdown measures. Nevertheless, the government’s declaration of a state of emergency and local government requests for infection control measures led many citizens to limit their activities [
4]. In Japan, the number of COVID-19 cases is extremely low compared to Western countries, and in particular, Tottori Prefecture has one of the lowest incidence rates in Japan (only 38 cases were reported during the observation period of this study). Therefore, it is unlikely that COVID-19 directly affects heat stroke or any other diseases. Nonetheless, the change in the rate of heat stroke incidence can be attributed to the indirect effects of COVID-19, namely, infection control measures, such as restrictions on going out. In another report [
5], the overall risk of heat stroke transport in Japan decreased under the pandemic, but the risk by generation was not mentioned. This study suggests that there may be a potential increased risk of heat stroke among the older generation.
An increasing number of studies have investigated the physical and mental effects of voluntary isolation during the COVID-19 pandemic, and it does not seem to have a positive effect on the body or mental health [
6,
7,
8]. In Japan, physical activity among the elderly has reportedly decreased during the COVID-19 pandemic [
9]. Although it is not clear whether older people who refrain from going out are more susceptible to heat stroke, vulnerability to heat stress may have increased due to reduced physical strength resulting from lack of outdoor activity. In addition, the reduction in opportunities to go outside during the summer season could have prevented adaptation to the hot environment, and this may have increased the risk of heat stroke among the elderly [
10]. In contrast to these theories, the percentage of heat stroke cases associated with agricultural work was also higher in 2020 than in other years. This was partly due to the fact that many of Japan’s farmers are older: the average age of Japanese farmers is 67.8 years, and 94.9% were 65 years or older in 2020 [
11]. In fact, in this study (2017 to 2020), 86.8% of those transported for heat stroke due to agricultural work were 65 years old or older (64.9% of those 75 years old or older). Agriculture has to be performed outside if necessary, even in extremely hot environments, hence the relatively high percentage of elderly people as a result of the decrease in heat stroke among the young generation in 2020. Agriculture is one of the occupations with a high risk of heat stroke [
11] and, given the aging of Japan’s farm workers, it is even more important to address this issue.
By contrast, the proportion of heat stroke transport cases under the age of 18 in 2020 was lower than in previous years. There were also lower numbers of heat stroke cases associated with exercise. This may have been because most sporting events for school children, which are primarily held in the summer, were canceled in 2020 to prevent the spread of the infection. Because most heat stroke cases in young people are related to exertion, strenuous exercise in a hot environment can be a problem in Japan. This point was made clear by the COVID-19 pandemic, but it is hoped that it will provide an opportunity to reassess the future of sports under extreme heat conditions [
12].
There were concerns about the impact of face masks on heat stroke before the summer of 2020. However, according to the information obtained from Tottori Prefecture, there were no reports of heat stroke caused by face masks during the investigated time period. The physiological changes induced by the use of face masks in healthy individuals, even during exercise, are negligible [
13]; therefore, the impact of face masks on heat stroke is likely to be limited. However, the effects on people with severe cardiopulmonary disease are not well understood, and future research is needed to determine the impact of face masks on the older population, a high-risk group for heat stroke.
There are several limitations to this study. Because it included only 4 years of data, it is difficult to say definitively whether 2020 was an aberration. Thus, it is necessary to monitor the incidence of heat stroke in the future. Another limitation is that there are no accurate data on how many people restricted themselves from leaving the residence during the government’s request for self-quarantine. Once accurate figures become available, we will be able to assess the risks and benefits of voluntary quarantine aiming to limit the spread of infection.
5. Conclusions
COVID-19 control measures, such as stay-at-home requests and the cancellation of events, may have contributed to slowing the transmission of the disease. However, restricting outings may further increase heat stroke risk for those who are typically more susceptible to heat stroke that occurs at home.
Author Contributions
Conceptualization, S.O.; methodology, S.O.; validation, S.O., Y.K., S.F.I., T.M. and H.A.; formal analysis, S.O.; investigation, S.F.I., T.M. and H.A.; resources, S.O.; data curation, S.O.; writing (original draft preparation), S.O.; writing (review and editing), S.O.; visualization, S.O.; supervision, Y.K.; project administration, S.O. and Y.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Tottori University Ethics Committee (No. 18A024, approved on 29 May 2018, updated on 29 June 2021).
Informed Consent Statement
Informed consent was obtained in the form of opt-out on the website/posting in Tottori Prefectural Office.
Data Availability Statement
The data presented in this study are available on request from authors.
Acknowledgments
The ambulance transport data in this study were provided by the Department of Health and Welfare of the Tottori Prefectural Government. We thank Katherine Thieltges, from Edanz Group (
https://en-author-services.edanz.com/, accessed on 27 October 2021) for editing a draft of this manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Johns Hopkins University of Medicine. COVID-19 Resource Center. Available online: https://coronavirus.jhu.edu/map.html (accessed on 27 October 2021).
- Miyake, Y. Characteristics of elderly heat illness patients in Japan—Analysis from Heatstroke STUDY 2010. Nihon Rinsho 2013, 71, 1065–1073. (In Japanese) [Google Scholar] [PubMed]
- Fujitani, Y.; Otani, S.; Majbauddin, A.; Amano, H.; Masumoto, T.; Kurozawa, Y. Impact of maximum air temperature on ambulance transports owing to heat stroke during spring and summer in Tottori Prefecture, Japan: A time-stratified case-crossover analysis. Yonago Acta Med. 2019, 62, 47–52. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ministry of Health, Labour and Welfare. Nationwide Survey to Counter COVID-19. Available online: https://www.mhlw.go.jp/stf/newpage_13101.html (accessed on 27 December 2020). (In Japanese)
- Hatakeyama, K.; Ota, J.; Takahashi, Y.; Kawamitsu, S.; Seposo, X. Effect of the COVID-19 pandemic on heatstroke-related ambulance dispatch in the 47 prefectures of Japan. Sci. Total Environ. 2021, 768, 145176. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Shuai, L.; Yu, H.; Wang, Z.; Qiu, M.; Lu, L.; Cao, X.; Xia, W.; Wang, Y.; Chen, R. Acute stress, behavioural symptoms and mood states among school-age children with attention-deficit/hyperactive disorder during the COVID-19 outbreak. Asian J. Psychiatry 2020, 51, 102077. [Google Scholar] [CrossRef] [PubMed]
- Pan, K.-Y.; Kok, A.A.L.; Eikelenboom, M.; Horsfall, M.; Jörg, F.; Luteijn, R.A.; Rhebergen, D.; Oppen, P.V.; Giltay, E.J.; Penninx, B.W.J.H. The mental health impact of the COVID-19 pandemic on people with and without depressive, anxiety, or obsessive-compulsive disorders: A longitudinal study of three Dutch case-control cohorts. Lancet Psychiatry 2020, 8, 121–129. [Google Scholar] [CrossRef]
- Almandoz, J.P.; Xie, L.; Schellinger, J.N.; Mathew, M.S.; Gazda, C.; Ofori, A.; Kukreja, S.; Messiah, S.E. Impact of COVID-19 stay-at-home orders on weight-related behaviours among patients with obesity. Clin. Obes. 2020, 10, e12386. [Google Scholar] [CrossRef] [PubMed]
- Yamada, M.; Kimura, Y.; Ishiyama, D.; Otobe, Y.; Suzuki, M.; Koyama, S.; Kikuchi, T.; Kusumi, H.; Arai, H. Effect of the COVID-19 epidemic on physical activity in community-dwelling older adults in Japan: A cross-sectional online survey. J. Nutr. Health Aging 2020, 24, 948–950. [Google Scholar] [CrossRef] [PubMed]
- Ioannou, L.G.; Gkikas, G.; Mantzios, K.; Tsoutsoubi, L.; Flouris, A.D. Risk assessment for heat stress during work and leisure. In Toxicological Risk Assessment and Multi-System Health Impacts from Exposure; Tsatsakis, A.M., Ed.; Elsevier: Amsterdam, The Netherlands, 2021; pp. 375–385. [Google Scholar]
- Ministry of Agriculture, Forestry and Fisheries. Statistics on Agricultural Labor Force. Available online: https://www.maff.go.jp/j/tokei/sihyo/data/08.html (accessed on 27 October 2021). (In Japanese)
- Takinami, Y.; Maeda, S. Ambulance dispatches to schools during a 5-year period in Fukui Prefecture. Acute Med. Surg. 2017, 4, 46–51. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hopkins, S.R.; Dominelli, P.B.; Davis, C.K.; Guenette, J.A.; Luks, A.M.; Molgat-Seon, Y.; Sa, R.C.; Sheel, A.W.; Swenson, E.R.; Stickland, M.K. Face masks and the cardiorespiratory response to physical activity in health and disease. Ann. Am. Thorac. Soc. 2021, 18, 399–407. [Google Scholar] [CrossRef] [PubMed]
| Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).