Responses of Italian Public Hospitals to COVID-19 Pandemic: Analysis of Supply and Demand of Hospital ICU Beds †
Abstract
:1. Introduction
- the strengthening of human resources. To address the urgent needs deriving from the diffusion of COVID-19, the entities of the National Health Service have been authorized to re-determine the plans of personnel needs and proceed with the consequent recruitment of health personnel. The increase in personnel concerned the hospital units most affected by the emergency (such as infectious and tropical diseases, emergency medicine, internal medicine, ICUs);
- the establishment of temporary health areas. Hospitals have activated temporary health areas both inside and outside of the structures, for the management of the COVID-19 emergency;
- the suspension of hospitalizations and non-urgent outpatient activities. For priority management of the coronavirus emergency, hospitals have been authorized to suspend or remodel non-urgent hospitalization and outpatient activities;
- the increase in beds. The emergency from COVID-19 required the immediate strengthening of the ICUs, especially in the most affected regions. The circular of 29 February 2020 n. 2619 of the Ministry of Health (whose recommendations were subsequently regulated by the decree-law of 9 March 2020) underlined the urgent need for the regions to prepare an emergency plan to guarantee suitable levels of treatment through an adequate number of intensive care beds. Subsequently, the circular of the Ministry of Health of 1 March 2020 n. 2627 (whose recommendations were subsequently regulated by decree-law n. 18 of 17 March 2020) required that, in the shortest possible time, an interregional cooperation model coordinated at the national level was activated, with the involvement of public and private accredited structures. At the regional level, the model envisaged an increase of 50 percent in the number of beds in ICUs and 100 percent in the pulmonary and infectious disease units.
2. Materials and Methods
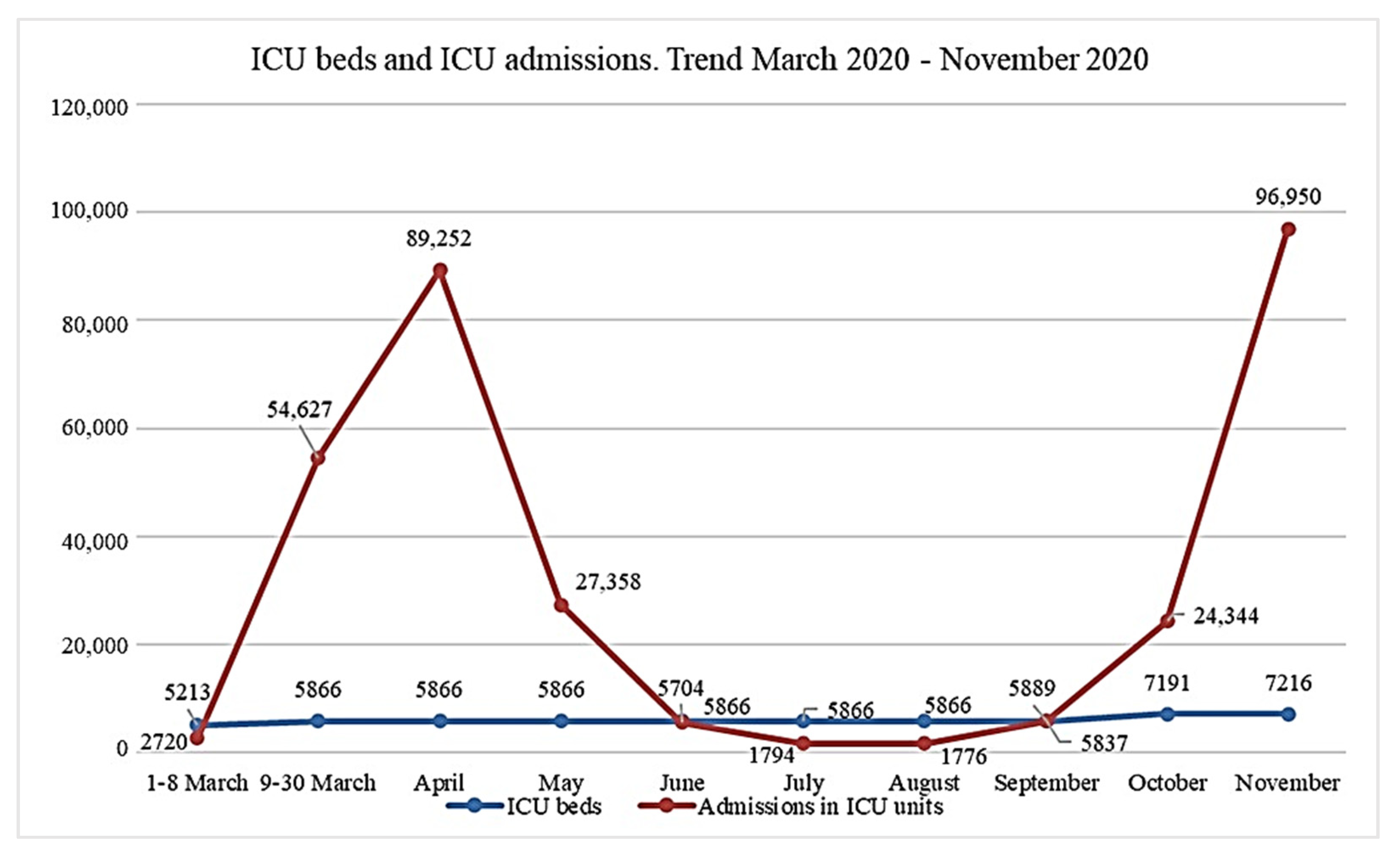
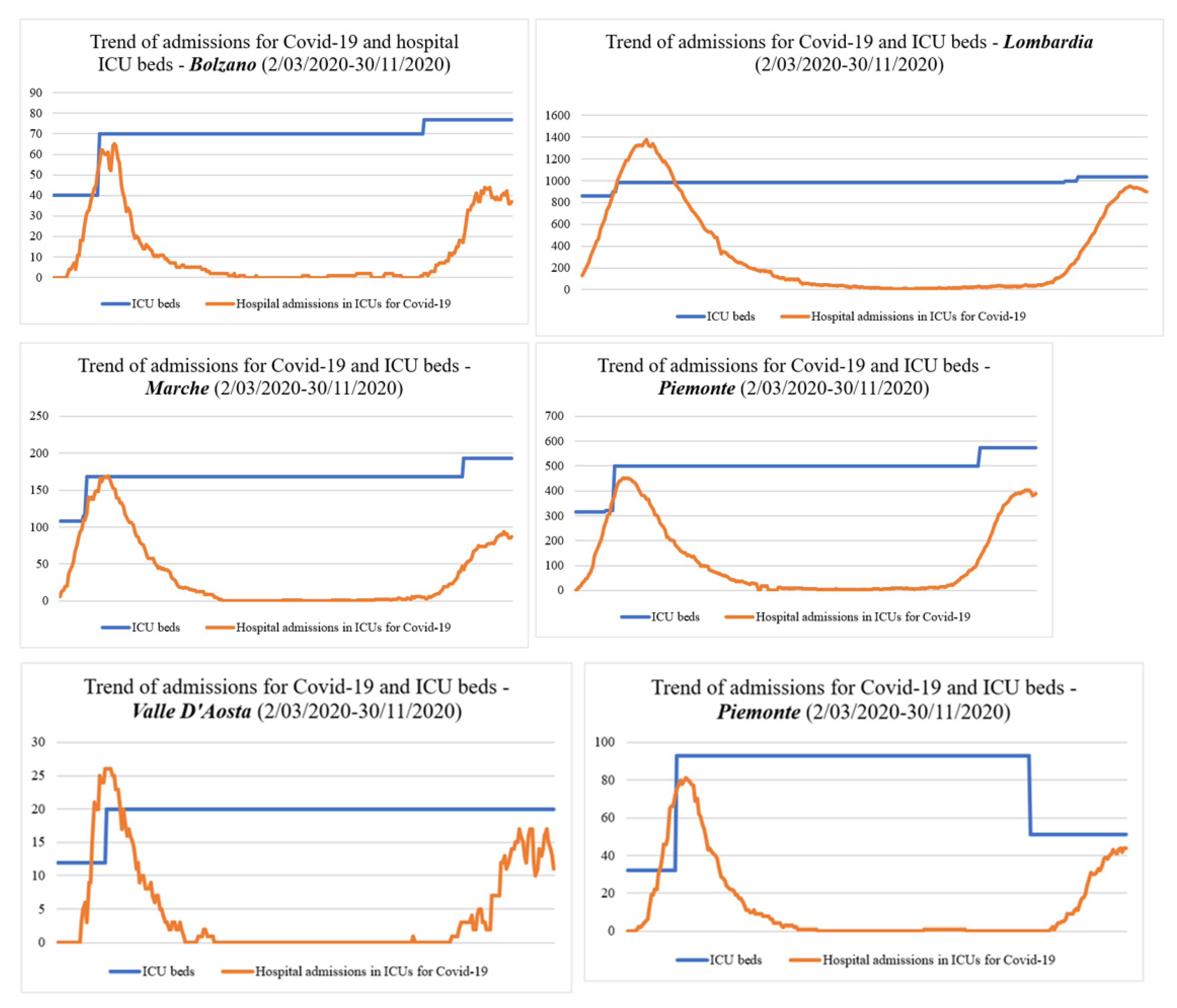
3. Results
4. Discussion and Conclusions
- deep changes have been made in the public healthcare offering, with a significant reduction in beds and health personnel (this is one of the reasons why hospitals found themselves unprepared to face such an important health emergency [11]);
- responsibilities for healthcare have been decentralized to regions, though the central government still retains a key role in ensuring all citizens have uniform access to health services throughout the country [12]. During the COVID-19 emergency, the central government directly intervened by introducing specific measures with a direct impact on the healthcare system and hospital management.
Supplementary Materials
Funding
Conflicts of Interest
References
- Lai, C.C.; Shih, T.P.; Ko, W.C.; Tang, H.J.; Hsueh, P.R. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and corona virus disease-2019 (COVID-19): The epidemic and the challenges. Int. J. Antimicrob. Agents 2020, 55, 105924. [Google Scholar] [CrossRef] [PubMed]
- Remuzzi, A.; Remuzzi, G. COVID-19 and Italy: What next? Lancet 2020, 395, 1225–1228. [Google Scholar] [CrossRef]
- Bontempi, E. The Europe second wave of COVID-19 infection and the Italy “strange” situation. Environ. Res. 2020, 193, 110476. [Google Scholar] [CrossRef] [PubMed]
- Carinci, F. Covid-19: Preparedness, decentralisation, and the hunt for patient zero. BMJ 2020, 368, 799. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Albarello, F.; Pianura, E.; Di Stefano, F.; Cristofaro, M.; Petrone, A.; Marchioni, L.; Campioni, P.; Eskild, P.; Zumla, A.; Ippolito, G.; et al. 2019-novel Coronavirus severe adult respiratory distress syndrome in two cases in Italy: An uncommon radiological presentation. Int. J. Infect. Dis. 2020, 93, 192–197. [Google Scholar] [CrossRef] [PubMed]
- Möhlenkamp, S.; Thiele, H. Ventilation of COVID-19 patients in intensive care units. Herz 2020, 45, 329–331. [Google Scholar] [CrossRef] [PubMed]
- DECRETO-LEGGE 9 Marzo 2020, n. 14. Disposizioni Urgenti per il Potenziamento del Servizio Sanitario Nazionale in Relazione All’emergenza COVID-19. (20G00030) (GU Serie Generale n.62 del 09-03-2020). Available online: https://www.gazzettaufficiale.it/eli/id/2020/03/09/20G00030/sg (accessed on 1 November 2020).
- DECRETO-LEGGE 17 Marzo 2020, n. 18 Misure di Potenziamento del Servizio Sanitario Nazionale e di Sostegno Economico per Famiglie, Lavoratori e Imprese Connesse All’emergenza Epidemiologica da COVID-19. (20G00034) (GU Serie Generale n.70 del 17-03-2020). Available online: https://www.gazzettaufficiale.it/eli/id/2020/03/17/20G00034/sg (accessed on 1 November 2020).
- Mackay, M.; Lee, M. Choice of models for the analysis and forecasting of hospital beds. Health Care Manag. Sci. 2005, 8, 221–230. [Google Scholar] [CrossRef] [PubMed]
- Anessi-Pessina, E.; Cantù, E. Whither managerialism in the Italian national health service? Int. J. Health Plan. Manag. 2006, 21, 327–355. [Google Scholar] [CrossRef] [PubMed]
- Mattiuzzi, C.; Lippi, G. Which lessons shall we learn from the 2019 novel coronavirus outbreak? Ann. Transl. Med. 2020, 8, 48. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization, Regional Office for Europe. European Observatory on Health Systems and Policies. In Italy: Health System Review; Ferre, F., de Belvis, A.G., Valerio, L., Longhi, S., Lazzari, A., Fattore, G., Ricciardi, W., Maresso, A., Eds.; World Health Organization, Regional Office for Europe: Geneva, Switzerland, 2014. [Google Scholar]
| Measures for the Containment and Management of the COVID-19 Emergency | Strengthening Measures of the National Health Service | ||||||
|---|---|---|---|---|---|---|---|
| Decree-Law of 23 February 2020 | Prime Minister’s Decree of 1 March 2020 | Decree-Law of 2 March 2020 | Prime Minister’s Decree of 4 March 2020 | Prime Minister’s Decree of 8 March 2020 | Decree-Law of 8 March 2020 | Decree-Law of 9 March 2020 | Decree-Law of 17 March 2020 |
| Urgent measures for the containment and management of the epidemiological emergency from COVID-19. | Further implementing provisions of the decree-law of 23 February 2020, n. 6, containing urgent measures regarding the containment and management of the epidemiological emergency from COVID-19. | Urgent support measures for families, workers and businesses related to the epidemiological emergency caused by COVID-19. | Further implementing provisions of the decree-law of 23 February 2020, n. 6, containing urgent measures regarding the containment and management of the epidemiological emergency from COVID-19, applicable on the whole national territory. | Further implementing provisions of the decree-law of 23 February 2020, n. 6, containing urgent measures regarding the containment and management of the epidemiological emergency from COVID-19. | Extraordinary and urgent measures to counteract the epidemiological emergency from COVID-19 and contain the negative effects on the judicial activity. | Urgent provisions for the strengthening of the National Health Service in relation to the COVID-19 emergency. | Strengthening measures of the National Health Service and economic support for families, workers and businesses connected to the epidemiological emergency from COVID-19. |
| Regions | Periods | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1–8 March | 9–30 March | April | May | June | July | August | September | October | November | ||
| ABRUZZO | Min | 0.00% | 0.00% | 14.68% | 2.75% | 0.00% | 0.00% | 0.92% | 0.92% | 4.59% | 21.62% |
| Max | 0.00% | 65.14% | 69.72% | 14.68% | 5.50% | 1.83% | 1.83% | 4.59% | 19.59% | 52.03% | |
| Mean | 0.00% | 37.28% | 42.42% | 6.87% | 2.45% | 0.41% | 0.95% | 3.24% | 10.05% | 39.39% | |
| BASILICATA | Min | 0.00% | 0.00% | 6.25% | 0.00% | 0.00% | 0.00% | 0.00% | 1.56% | 0.00% | 15.07% |
| Max | 0.00% | 29.69% | 29.69% | 6.25% | 1.56% | 0.00% | 1.56% | 3.13% | 9.59% | 41.10% | |
| Mean | 0.00% | 12.04% | 17.76% | 2.02% | 0.42% | 0.00% | 0.15% | 1.61% | 3.48% | 28.40% | |
| BOLZANO | Min | 0.00% | 0.00% | 18.57% | 5.71% | 0.00% | 0.00% | 0.00% | 0.00% | 0.00% | 22.08% |
| Max | 0.00% | 127.50% | 92.86% | 15.71% | 5.71% | 1.43% | 2.86% | 2.86% | 23.38% | 57.14% | |
| Mean | 0.00% | 55.28% | 52.66% | 9.86% | 1.95% | 0.18% | 1.01% | 1.43% | 7.84% | 48.44% | |
| CALABRIA | Min | 0.00% | 0.00% | 4.26% | 0.71% | 0.00% | 0.00% | 0.00% | 0.00% | 0.66% | 7.24% |
| Max | 0.00% | 16.31% | 13.48% | 2.84% | 0.71% | 0.71% | 0.71% | 2.63% | 7.24% | 34.87% | |
| Mean | 0.00% | 8.93% | 7.57% | 1.30% | 0.17% | 0.05% | 0.59% | 1.51% | 3.03% | 21.32% | |
| CAMPANIA | Min | 0.00% | 1.87% | 6.79% | 1.17% | 0.00% | 0.00% | 0.23% | 0.94% | 8.90% | 33.66% |
| Max | 1.64% | 42.39% | 31.15% | 7.03% | 1.64% | 1.41% | 1.17% | 9.13% | 33.27% | 44.95% | |
| Mean | 0.23% | 15.57% | 17.74% | 3.91% | 0.58% | 0.28% | 0.49% | 4.18% | 18.85% | 37.60% | |
| EMILIA ROMAGNA | Min | 3.56% | 20.04% | 45.88% | 12.69% | 0.00% | 0.67% | 0.67% | 2.00% | 2.45% | 23.45% |
| Max | 16.70% | 78.17% | 83.52% | 44.32% | 12.03% | 2.23% | 2.45% | 5.12% | 22.20% | 45.83% | |
| Mean | 9.23% | 51.13% | 68.78% | 27.44% | 4.11% | 1.65% | 1.26% | 3.71% | 10.77% | 39.04% | |
| FRIULI VENEZIA GIULIA | Min | 0.00% | 0.79% | 8.66% | 0.79% | 0.00% | 0.00% | 0.00% | 1.57% | 1.57% | 21.14% |
| Max | 0.79% | 47.24% | 48.03% | 4.72% | 3.15% | 1.57% | 2.36% | 4.72% | 20.57% | 32.57% | |
| Mean | 0.22% | 24.95% | 23.49% | 1.96% | 0.66% | 0.43% | 1.80% | 3.18% | 8.45% | 27.50% | |
| LAZIO | Min | 0.00% | 1.44% | 20.65% | 10.23% | 0.00% | 1.62% | 1.08% | 1.44% | 7.63% | 21.84% |
| Max | 1.44% | 27.65% | 36.45% | 18.85% | 10.05% | 2.33% | 1.62% | 8.44% | 22.22% | 42.03% | |
| Mean | 0.87% | 11.84% | 32.68% | 13.72% | 5.52% | 1.85% | 1.34% | 3.81% | 13.75% | 33.73% | |
| LIGURIA | Min | 0.54% | 9.14% | 37.10% | 4.30% | 0.00% | 0.00% | 0.00% | 2.69% | 11.29% | 27.27% |
| Max | 5.91% | 94.09% | 96.24% | 38.71% | 3.76% | 1.61% | 1.61% | 12.90% | 27.27% | 58.85% | |
| Mean | 2.38% | 55.87% | 65.65% | 18.26% | 1.42% | 0.33% | 0.57% | 7.35% | 16.08% | 48.69% | |
| LOMBARDIA | Min | 14.78% | 51.22% | 61.55% | 17.29% | 4.27% | 0.71% | 0.92% | 2.14% | 3.56% | 40.35% |
| Max | 46.45% | 135.30% | 140.49% | 57.27% | 16.99% | 4.17% | 2.03% | 3.87% | 37.84% | 91.60% | |
| Mean | 30.17% | 102.54% | 104.18% | 31.45% | 8.42% | 2.52% | 1.30% | 3.00% | 12.99% | 75.15% | |
| MARCHE | Min | 5.56% | 43.52% | 28.57% | 5.36% | 0.00% | 0.00% | 0.00% | 0.60% | 1.79% | 21.76% |
| Max | 37.96% | 100.00% | 100.60% | 27.38% | 5.36% | 0.60% | 0.60% | 2.38% | 27.98% | 48.70% | |
| Mean | 19.84% | 83.29% | 61.25% | 14.07% | 0.85% | 0.23% | 0.27% | 1.15% | 9.01% | 38.84% | |
| MOLISE | Min | 0.00% | 10.53% | 5.26% | 0.00% | 0.00% | 0.00% | 0.00% | 0.00% | 0.00% | 14.71% |
| Max | 10.53% | 47.37% | 42.11% | 10.53% | 10.53% | 0.00% | 0.00% | 3.23% | 17.65% | 41.18% | |
| Mean | 4.51% | 30.14% | 18.95% | 7.13% | 3.86% | 0.00% | 0.00% | 1.83% | 3.23% | 24.51% | |
| PIEMONTE | Min | 0.63% | 15.77% | 39.88% | 11.62% | 0.00% | 1.00% | 0.40% | 1.20% | 2.40% | 31.13% |
| Max | 14.20% | 112.50% | 90.78% | 36.27% | 10.82% | 2.20% | 1.20% | 2.40% | 30.26% | 70.26% | |
| Mean | 6.67% | 69.11% | 68.06% | 22.23% | 4.73% | 1.46% | 0.81% | 1.66% | 12.71% | 59.23% | |
| PUGLIA | Min | 0.00% | 0.65% | 13.73% | 3.59% | 0.00% | 0.00% | 0.00% | 1.96% | 3.92% | 23.58% |
| Max | 0.98% | 34.64% | 51.96% | 13.07% | 3.59% | 0.00% | 1.63% | 4.90% | 23.58% | 57.45% | |
| Mean | 0.33% | 12.49% | 24.81% | 8.25% | 0.92% | 0.00% | 0.69% | 3.20% | 10.40% | 44.42% | |
| SICILIA | Min | 0.00% | 0.00% | 7.79% | 1.70% | 0.00% | 0.00% | 0.73% | 2.43% | 4.87% | 22.45% |
| Max | 0.00% | 19.46% | 18.49% | 7.30% | 1.95% | 0.97% | 2.43% | 4.62% | 20.75% | 43.03% | |
| Mean | 0.00% | 9.50% | 12.37% | 3.65% | 0.95% | 0.34% | 1.59% | 3.54% | 11.71% | 35.57% | |
| SARDEGNA | Min | 0.00% | 0.00% | 13.01% | 1.63% | 0.00% | 0.00% | 0.00% | 4.07% | 12.57% | 23.89% |
| Max | 0.00% | 19.51% | 25.20% | 10.57% | 0.81% | 0.00% | 2.44% | 17.07% | 22.22% | 42.22% | |
| Mean | 0.00% | 8.54% | 18.62% | 6.45% | 0.30% | 0.00% | 0.26% | 11.76% | 17.56% | 33.65% | |
| TOSCANA | Min | 0.00% | 2.39% | 28.19% | 6.04% | 0.00% | 0.00% | 0.00% | 1.57% | 4.92% | 37.61% |
| Max | 1.86% | 62.52% | 66.00% | 27.74% | 5.59% | 1.12% | 1.57% | 5.37% | 35.43% | 64.78% | |
| Mean | 0.91% | 40.15% | 48.05% | 14.64% | 2.71% | 0.32% | 0.71% | 3.80% | 15.04% | 55.56% | |
| TRENTO | Min | 0.00% | 6.25% | 23.33% | 2.22% | 0.00% | 0.00% | 0.00% | 0.00% | 0.00% | 10.00% |
| Max | 6.25% | 225.00% | 90.00% | 21.11% | 3.33% | 0.00% | 1.11% | 1.11% | 10.00% | 48.89% | |
| Mean | 1.34% | 96.79% | 56.70% | 9.53% | 0.67% | 0.00% | 0.72% | 0.11% | 2.08% | 34.30% | |
| UMBRIA | Min | 0.00% | 2.86% | 22.86% | 1.43% | 0.00% | 0.00% | 0.00% | 2.86% | 4.29% | 47.42% |
| Max | 2.86% | 67.14% | 68.57% | 18.57% | 2.86% | 1.43% | 2.86% | 8.57% | 46.84% | 80.41% | |
| Mean | 1.84% | 37.34% | 45.57% | 6.68% | 1.67% | 0.23% | 0.78% | 4.76% | 21.88% | 66.74% | |
| VALLE D’AOSTA | Min | 0.00% | 0.00% | 20.00% | 0.00% | 0.00% | 0.00% | 0.00% | 0.00% | 0.00% | 50.00% |
| Max | 0.00% | 216.67% | 130.00% | 15.00% | 0.00% | 0.00% | 0.00% | 5.00% | 35.00% | 85.00% | |
| Mean | 0.00% | 91.36% | 67.00% | 5.97% | 0.00% | 0.00% | 0.00% | 0.17% | 15.00% | 69.00% | |
| VENETO | Min | 2.83% | 10.32% | 19.00% | 1.00% | 0.00% | 0.00% | 0.67% | 1.33% | 2.42% | 16.00% |
| Max | 9.51% | 69.64% | 59.33% | 18.33% | 1.00% | 0.50% | 1.17% | 3.50% | 14.91% | 38.79% | |
| Mean | 5.64% | 42.25% | 36.75% | 6.52% | 0.17% | 0.29% | 0.90% | 2.29% | 6.04% | 28.67% | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Giancotti, M. Responses of Italian Public Hospitals to COVID-19 Pandemic: Analysis of Supply and Demand of Hospital ICU Beds. Med. Sci. Forum 2021, 4, 16. https://doi.org/10.3390/ECERPH-3-09019
Giancotti M. Responses of Italian Public Hospitals to COVID-19 Pandemic: Analysis of Supply and Demand of Hospital ICU Beds. Medical Sciences Forum. 2021; 4(1):16. https://doi.org/10.3390/ECERPH-3-09019
Chicago/Turabian StyleGiancotti, Monica. 2021. "Responses of Italian Public Hospitals to COVID-19 Pandemic: Analysis of Supply and Demand of Hospital ICU Beds" Medical Sciences Forum 4, no. 1: 16. https://doi.org/10.3390/ECERPH-3-09019
APA StyleGiancotti, M. (2021). Responses of Italian Public Hospitals to COVID-19 Pandemic: Analysis of Supply and Demand of Hospital ICU Beds. Medical Sciences Forum, 4(1), 16. https://doi.org/10.3390/ECERPH-3-09019






