Abstract
Introduction: The “migrant” term indicates a resident born in a country other than the host country. Resident foreigners made up 8.4% of the total Italian population in 2020. The Sicilian trend reflects the national one, with 190,974 resident foreigners as of 1th January 2020. The aim of this study was to identify the presence of tumors in foreign patients residing in the RTI’s provinces of interest in 2003–2017 and to analyze the clinical-biological variables. Materials and Methods: We analyzed 3541 foreign patients with tumors (out of a total of 160,912 patients) residing in the RTI’s provinces of interest in 2003–2017. Foreign patients were identified by tax code. Tumors are described ((number and percentage). Results: Of the 3541 foreign patients, 36% were male and 64% were female. They resided in the provinces of Catania (42.6%), Messina (29.9%), Siracusa (20.7%), and Enna (6.6%). They came from Europe (57%), Africa (22.4%), the Americas (12.03%), Asia (5.08%), and Oceania (1.80%); 0.3% were stateless. The average age was 58 for males and 54.4 for females. The number of tumors (excluding non-melanoma skin tumors) was 3715. Sixty-two males and 98 females had one or more multiple tumors. In foreign females, the three most common tumors were breast (28%), thyroid (9%), and cervical (6%) tumors. Most breast cancers were diagnosed as stage T1 (35%) or T2 (26%). In foreign males, the three most common tumors were lung (13%), bladder (12%), and prostate (11%) tumors. Conclusions: The growing presence of foreign citizens in the provinces studied calls for more attention on oncology-related problems and more careful surveillance of changes in incidence and mortality by the RTI.
1. Introduction
The “migrant” term indicates a resident born in a country other than the host country. In 2019, migrants made up 3.5% of the world population, i.e., 272 million, while according to ISTAT (Italian Institute of Statistics) data, regular migrants in the 27 European Union countries represented 10.1% of the entire population [1].
In the post-war period, Italy had a high rate of emigration; recently, however, it has had a high rate of immigration as a final destination or intermediate destination in the passage to other European countries. In 2020, Italy’s total resident population of 59,641,488 was made up of 5,039,637 foreigners (8.4%), of which 48.3% were men, 51.7% were women, and 20.3% were minors.
The number of foreign citizens in Italy is high and is growing rapidly, rising from 4.2% of total residents in 2005 to 8.4% in 2020. Most (58.3%) resided in northern Italy, 24.8% resided in central Italy, 12.1% resided in southern Italy, and only 4.8% resided in the Italian isles.
Their countries of origin can be classified into two categories: those whose development is very similar to Italy’s (PSA); and those with strong migratory pressure (PFPM), including countries of Central and Eastern Europe, Africa, Asia, and Central and South America. Among resident foreigners in Italy, 49.6% were European citizens, 22% were from Africa, 21% were from Asia, 7.3% were from the Americas, 0.04% were from Oceania, and 0.01% were stateless. The top 10 countries of origin were Romania (22.7%), Albania (8.4%), Morocco (8.2%), China (5.7%), Ukraine (4.5%), the Philippines (3.1%), India (3%), Bangladesh (2.8%), Egypt (2.5%), and Pakistan (2.4%); the remaining 36.5% was represented by all other countries.
The Sicilian trend reflects the national one (both in terms of citizenship and of countries of origin), with 190,974 foreigners residing in the Sicilian provinces as of 1 January 2021 (Figure 1, Table 1).
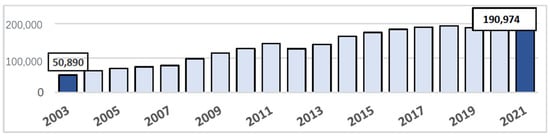
Figure 1.
Sicilian trend for resident foreigners as of 1 January 2021.

Table 1.
Distribution of foreign citizens in the Sicilian provinces.
A gradual increase occurred from 2003 to 2021 in the four provinces belonging to the Integrated Cancer Registry (RTI), with a total of about 34,000 migrants belonging to Catania, 28,000 to Messina, 15,000 to Siracusa, and 4000 to Enna (Figure 2). The presence of foreign citizens has social, political, humanitarian, and cultural implications; has consequences on public health; and presents an oncological risk (an ability to identify the risk factors causing the onset of cancer pathologies in order to understand if they are inherent to the patient or acquired in the host country) which also influences access to prevention and treatment services. The aim of this work is to identify the presence of tumors in foreign patients residing in the RTI’s provinces of interest (Catania, Messina, Siracusa and Enna) in 2003–2017 and to analyze the clinical-biological variables (sex, age, origin, location, and histotype).
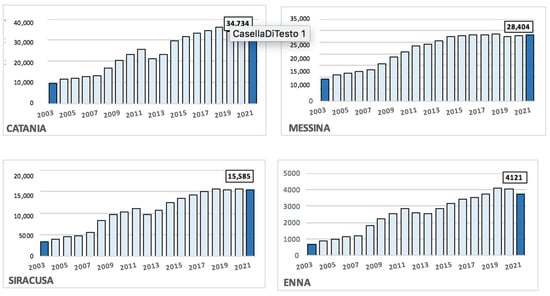
Figure 2.
Foreign population trends in the provinces of interest of the RTI (Catania, Messina, Siracusa, and Enna).
2. Materials and Methods
We analyzed 3541 foreign patients with cancer residing in the provinces of Catania, Messina, Siracusa and Enna and belonging to the Integrated Cancer Registry in 2003–2017; there was a total of 3715 tumors, given that 62 males and 98 females had one or more multiple tumors.
Foreign patients were identified by their tax code; for foreign patients, the twelfth letter is a “Z” and is followed by three digits indicating country of origin.
From our database, we selected all patients who have the letter “Z” as the twelfth letter of their tax codes; we excluded patients without a tax code because it was not possible to identify them either as foreigners or as Italians.
We calculated the percentage of tumors (excluding non-melanoma skin tumors) by gender and topography in the RTI’s provinces of interest (Catania, Messina, Siracusa and Enna) in 2003–2017. For the three most common cancers in both male and female foreign patients, we analyzed age groups, morphologies, and staging.
3. Results
From 2003 to 2017, in the provinces of interest of the RTI (CT, ME, SR, EN), there were about 160,912 patients with cancer; 3541 were foreign patients (2.2%) and were distributed as follows: 1511 in Catania (42.6%), 1060 in Messina (29.9%), 733 (20.7%) in Siracusa, and 236 (6.6%) in Enna. 57% (2023) of the patients came from Europe, 22.4% (795) came from Africa, 12.03% (426) came from America, 5.08% (180) came from Asia, 1.80% (64) came from Oceania, and 0.3% (12) were stateless. The average age was 58 years for foreign males and 54 years for foreign females.
The top 10 countries with the highest rates of migration were Germany (792—22.36%), Libya (426—12.03%), Romania (345—9.74%), Switzerland (215—6.07%), the United States of America (140—3.95%), Argentina (109—3.07%), Poland (108—3.04%), Venezuela (93—2.62%), the Philippines (86—2.42%), and Tunisia (81—2.28%); 3541 foreigners resided in the provinces of interest of the RTI, of which 2269 (64%) were female and 1272 (36%) were male. The total number of tumors (excluding non-melanomatous skin tumors) in migrant patients belonging to the RTI was 3715. Of these, 2375 were in females and 1340 were in males.
Women were predominantly from Europe (1436—63%), followed by Africa (337—15%), the Americas (289—13%), Asia (120—5%), Oceania (42—2%), and Russia (37—2%), while 7 (0.3%) were stateless.
Males were predominantly from Europe (565—25%), followed by Africa (451—20%), the Americas (165—7%), Asia (60—3%), Oceania (22—1%), and Russia (4—0.1%), while 5 (0.2%) were stateless.
In foreign females belonging to the RTI, the 10 most common tumor locations were the breasts (679 cases—28.5%), thyroid (207—8.7%), cervix (154—6.4%), colon (138—5.8%), haematopoietic system and endothelial reticulum (135—5.6%), lungs (118—4.9%), uterine body (111—4.6%), ovaries (74—3.1%), brain and other parts of the CNS (71—2.9%), and meninges (69—2.9%).
In foreign males belonging to the RTI, the 10 most common tumor locations were the lungs (180 cases—13.4%), bladder (158—11.7%), prostate (154—11.4%), haematopoietic system and endothelial reticulum (100—7.4%), colon (86—6.4%), lymphnodes (59—4.4%), brain and other parts of the CNS (54—4.02%), stomach (47—3.5%), testes (45—3.3%), and liver and intrahepatic biliary tract (37—2.7%).
Then, we examined the clinical-biological variables of the three most common tumor locations for both females and males. In foreign women, breast cancer was the most common (679 cases—28%), followed by the thyroid (207—9%) and the cervix (154—6%). For breast cancer, the most frequent histotype was the “non-special type” carcinoma (497 cases—73%), followed by special histotypes (lobular, mucinous, papillary), and finally the rarer forms. We divided the patients by age group. We know that breast cancer shows an increasing incidence until menopause (50–55 years of age). It then reaches a plateau, and a further increase occurs after 60 years of age. This trend is also evident in foreign women. We then evaluated the extent of the disease. “T” is the size of the tumor; most cases of breast cancer were in stage T1 or T2 and were therefore still at an early stage. However, if we examine the subdivision of the T1 stage, we see that most of the tumors were between T1c and were therefore >1 cm in size (Figure 3).
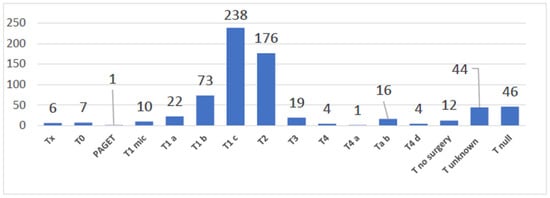
Figure 3.
Rates of breast cancer in foreign women belonging to the RTI.
The most frequent histotype for the thyroid, as per the literature, was papillary carcinoma (173 cases—83%), followed by follicular, medullary, sclerosing, and anaplastic carcinomas. Thyroid cancer has a peak incidence between the ages of 50 and 60. In foreign women, we see a bias in the younger age groups (Figure 4).
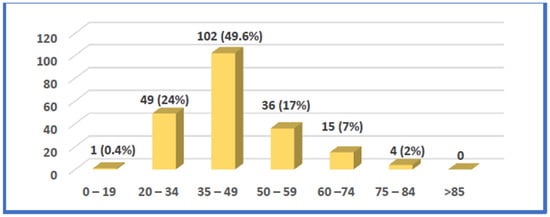
Figure 4.
The age groups of foreign women with thyroid cancer registered by the RTI.
As per the literature, the most frequent histotype for cervical cancer is squamous cell carcinoma (135 cases—88%), followed by adenocarcinoma and mixed forms. Normally, the invasive forms have a peak incidence around 50 years of age, while the intraepithelial forms have a peak incidence around 30 years of age. In foreign women, there is an incidence of invasive forms even in the younger age groups (Figure 5).
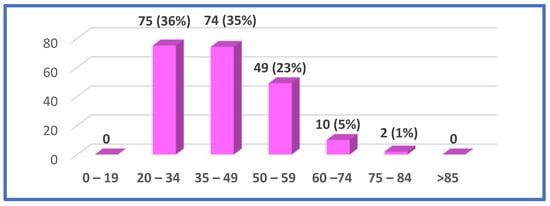
Figure 5.
The age groups of foreign women with cervix cancer registered by the RTI.
The three most common cancers in foreign men were lung cancer (180 cases—13%), followed by bladder cancer (158—12%) and prostate cancer (154—11%).
As per the literature, the most frequent histotype for the lungs was non-small cell carcinoma (104 cases—58%), followed by small-cell carcinoma and carcinoid, adenosquamous, mucoepidermoid, and solid carcinomas, etc. Incidence of lung carcinoma peaks between the ages of 50 and 60. Moreover, in the case of foreign men, there is a bias in the younger age groups (Figure 6).
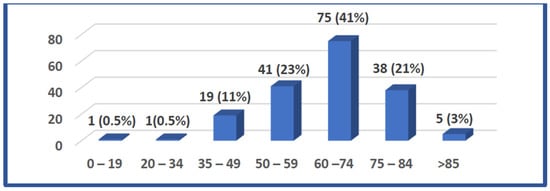
Figure 6.
The age groups of foreign men with lung cancer registered by the RTI.
Regarding the bladder, papillary urothelial carcinoma is the most frequent type (113 cases—71%), followed by urothelial, squamous-cell, transitional-cell, and sarcomatoid carcinomas. Normally, the peak of incidence is between 60 and 70 years of age; incidence occurs exclusively over 45 years of age. Moreover, for bladder cancer, we see a bias in the younger age groups (Figure 7).
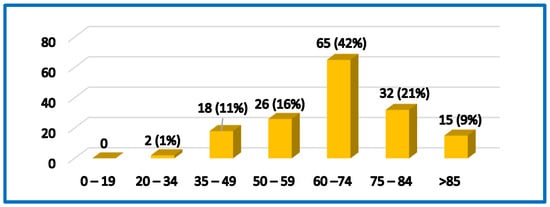
Figure 7.
The age groups of foreign men with bladder cancer registered by the RTI.
As per the literature data for the prostate, the most frequent carcinoma is adenocarcinoma. Generally, the onset is in old age and is rarely under the age of 40. This is also true in foreign patients.
The 2003–2017 incidence trends in both female and male patients with cancers are constant, with only a slight increase in the incidence of breast cancer.
4. Conclusions and Discussion
Our study shows that most foreigners with cancer belonging to the Integrated Cancer Register and residing in its provinces of interest (Catania, Messina, Siracusa, and Enna) come from Eastern Europe; it also shows that the percentage of resident males from Africa with carcinoma is higher than for females from Africa.
The histopathological characteristics of carcinomas are consistent with the literature data, but for breast cancer, even if it is diagnosed at an early stage of cancerogenesis, stage T1c and T2 carcinomas (tumors > 1 cm in size) prevail. This incidence could be caused by the fact that some women may arrive in Italy with breast cancer or may be treated too late.
Finally, for all cancers except the prostate, there is a bias in the younger age groups. Bibliographic data shows that the data on cancer and risk factors in the foreign population are insufficient. Normally, the risk of cancer is lower in migrant populations and the incidence is lower in foreigners who come from countries with strong migratory pressure than it is for those who come from highly developed countries and from Italy (based on analysis of the registers of Toscana and Piemonte), with the exception of viral carcinomas of the cervix and liver. Cervical cancer, for example, could be linked to pre-existing HPV infections whose prevalence is high in the countries of South America, Africa, and Eastern Europe (PFPM), which are the areas from which most of Italy’s migrants arrive.
There are several factors that can affect the health of migrant populations and ethnic minorities [2]. The causes could be inherent to the individuals or related to the country of origin or host country (or to the countries they passed through travelling to the host country). The risk factors can be related to the socio-economic context, i.e., the environment where the migrants live. It can also be related to behavioral characteristics. A diet rich in processed or ready-to-eat foods (because healthy foods are expensive), ignorance of the dangers of Western food, obstacles and inequalities in the education system, underpaid work and poor safety measures in the workplace, reduced accessibility to health services, inadequate prevention programs, poor participation in community activities, and lack of health promotion; these are all determinants that can affect the health of migrants. The growing presence of foreign citizens in our country requires greater attention to oncological problems. The response of the national health service must aim for greater involvement of the foreign population in screening programs, the only source of secondary prevention accessible to this most disadvantaged part of the population, and for more careful surveillance by the RTI of changes in incidence and mortality.
Author Contributions
Conceptualization and original draft preparation, A.A.M.T.; writing, review and editing, R.R.; data acquisition, C.S. and E.I.; data acquisition and interpretation, A.I.; data analysis and interpretation, A.A.D.P.; methodology, data analysis, A.M.; project administration, M.F. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki. The study did not require ethical approval. The present analysis was considered a secondary analysis of data already collected for the purposes of the RTI and, as such, it was covered by the same consent statements and privacy provisions of the RTI, already obtained previously; therefore, a further request to the Ethics Committee was not deemed necessary under present national laws.
Informed Consent Statement
Patient consent was waived as the present analysis was a secondary analysis of data, covered by the same consent statements and privacy provisions of the RTI that had previously been obtained.
Data Availability Statement
The data that support the findings of our study are available on request from the Integrated Cancer Registry (RTI CT-ME-EN). Further information is available from the corresponding author upon request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Andamento della Popolazione con Cittadinanza Straniera. Dati ISTAT. Available online: http://dati.istat.it/Index.aspx?DataSetCode=DCIS_POPSTRCIT1 (accessed on 1 March 2023).
- Manneschi, G.; Crocetti, E.; Puliti, D.; Zappa, M.; Sacchetti, C.; Paci, E. L’incidenza dei tumori in cittadini nati in Italia e immigrati di prima generazione. Epidemiol. Prev. 2011, 35, 292–296. [Google Scholar] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).