Abstract
Surgical site infections (SSI) are one of the main healthcare-related infections in developing nations. Regardless of upgrades in surgical strategy and the utilization of best disease avoidance techniques, SSI stayed the significant reason for medical clinic obtained infections. Subsequently, the target of this paper was to describe risk factors for SSI and the utilization of antibiotics to decrease the risk involved for the SSI. SSI is a possibly morbid and expensive complications of medical procedures. In this way, an underlying pursuit recognized various titles distributed in 2012–2022. Extracted data, including design of study and procedure, revealed combined occurrence and time taken as post-surgery until the beginning of SSI, and probabilities proportions and associated inconstancy for all variables considered in univariate and additionally multivariable investigations. In a wide survey of available works, risk factors for SSI were portrayed as depicting decreased wellness, patient fragility, medical procedure length, and intricacy. The occurrence of SSI was high in the review set. There were critical quantities of contributing variables to the event of surgical site infections. Recognition of risk factors habitually connected with SSI considers the identification of such patients with the best requirement for ideal protective actions to be recognized and pre-treatment before medical procedure.
1. Introduction
Medical care related diseases are considered the most well-known and deadliest occasions undermining the well-being of patients. They drag out the length of clinic stays and increase medical care costs worldwide [1]. A surgical site infection (SSI) is an infection that occurs following an obtrusive method [2]. SSI is one of the most well-known and genuine causes of hospitalization from obtained contaminations around the world [3]. According to the “Centre for Disease Control and Prevention” (CDC), SSI is characterized as “post-operative contaminations that create in 30 days after any careful surgical procedure or the span of one year of any implants” [4]. If we look at the worldwide data, around 300 million medical procedures are carried out annually. This rising number of medical procedures consequently means an increase in the frequency of postoperative injury diseases on surgical sites [5]. A new report distributed by the World Health Organization (WHO) that SSI is one of the common hospital-acquired infections (HAI) in low- and middle-income countries. These effects were dependent upon 33% of patients who have gone through surgery.
Despite the fact that SSI recurrence is lower in developed nations, it remains the second-most common sort of HAI in the USA [6]. Notwithstanding enhancements in operating room preparation, instrument cleansing strategies, better surgical procedures, and the best endeavors of contamination anticipation systems, SSI remains a significant reason for HAI and rates are expanding universally, even in clinics with up-to-date offices and standard conventions of preoperative preparation and anti-microbial prophylaxis. In addition, in emerging nations where assets are restricted, even fundamental life-saving tasks—such as appendectomies and cesarean sections—are related to high contamination rates and mortality [7]. Surgical wound infection results disrupted host–microorganism balance that prompts colonization of the microbes on the surgical site. Therefore, healing of surgical wounds is incredibly impacted, and fundamental reactions likewise will show [8]. Utilizing anti-antibiotics before incision of surgery is viewed as a compelling method in forestalling SSIs, which are among the most well-known preventable post-medical procedure difficulties including HAIs [9]. A parenteral prophylaxis specialist range with comparing expected microscopic organisms on specific destinations of medical procedures has been recommended as of late to diminish SSI rates proficiently [10]. This study was led to identifying the SSI rate and to distinguish risk factors for SSI among surgical patients. An improved comprehension of indicators could further develop disease control by antibiotics in post-surgical patient infections.
2. Methodology
The current systematic review was made according to the Preferred Reporting Items for Systematic Reviews (PRISMA) revealing rules and statements. We looked at PubMed/Medline, Cochrane Library, Embase, and ScienceDirect. The search included the keywords “incidence of surgical site infection”, “prevalence of surgical site infection”, “surgical site infection”, and “utilization of antibiotics in post-operative infection”. The selection involved articles distributed in the English language, other language articles were removed. Articles distributed in the last decade were only considered. All of the authors have gathered the articles according to these consideration standards. After the assortment and aggregation of articles, the authors explored and included articles for information extraction. The journals collected for the study were published in a peer-reviewed journal and all the papers have an International Standard Serial Number (ISSN).
3. Results and Discussion
SSI is one of the fastest-growing concerns in the medical sector. Prevention and control of the SSI is an important aspect of the reduction in medical care costs and, as of now, it is increasingly important as pressure from the COVID-19 pandemic is paralyzing the medical sector. There has been an increased use of antibiotics among patients with SSI in the last decade. Antibiotics help in the control of the spreading tendency in the case of SSI in surgical patients. The current systemic review is intended to distinguish the epidemiological features and risk factors for the growth of SSI and the uses of antibiotics to overcome them.
In order to understand the utilization of antibiotics, a systemic PRISMA review was performed of the incidence and risk aspects for SSI among surgical patients. The following figure (flow chart of PRISMA as shown in Figure 1) sums up the information extraction process for this systematic review. The number of articles included and barred in the various stages because of the information extraction measures is depicted. These articles were distributed in peer-reviewed journals over the past 10 years. At first, there were around 312 articles selected in this survey. Consequently, after rejection from each stage on the basis of inclusion/exclusion criteria, an sample of 26 full-text articles was evaluated for evidence synthesis as shown in Table 1.
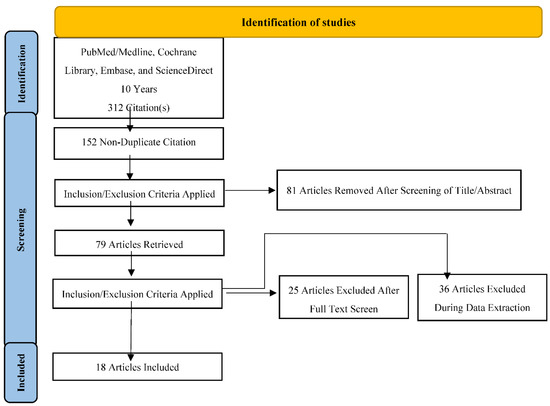
Figure 1.
PRISMA flow chart.

Table 1.
Summary of major outcomes in the SSI.
In spite of the best exertion from our examination group for this systematic review, certain constraints should be considered while deciphering this systematic review. Initially, the current review only included English-language articles. Subsequently, discoveries of non-English articles are not considered for audit, this systematic review may not be pertinent for worldwide targets.
The sample sizes of most of the articles in this survey are small. Furthermore, around 33% of included investigations are case-control studies. Thus, the chance of perplexing predisposition should be considered while deciphering this systematic review.
4. Conclusions
The event rate of SSI among post-operative patients is extremely high, particularly in developing nations. This prompts a double burden on the medical services conveyance settings. The layout of operating rooms, deficient ventilation norms, inadequate staffing, unrestrained traffic in the operating rooms, absence of information about contamination control actions, or more all, obliviousness about disease control exercise account for the high SSI rates. The usage of antibiotics in the case of SSI helps in the faster recovery of the patients but improper usage and maltreatment of antibiotics results in SSIs with multi-resistant microbes. Henceforth, it is fundamental to incorporate a severe contamination control strategy, and fair utilization of antibiotic practices to be executed.
Author Contributions
D.K.M., S.M., A.T., V.D., S.Y., and S.U.: conceptualization, methodology, data collection, writing—original draft preparation; D.K.M., S.M., A.T., V.D., S.Y., and S.U.: writing—reviewing and editing. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data available in a publicly accessible repository that does not issue DOIs. Publicly available datasets were analyzed in this study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Allegranzi, B.; Bagheri Nejad, S.; Combescure, C.; Graafmans, W.; Attar, H.; Donaldson, L.; Pittet, D. Burden of endemic health-care-associated infection in developing countries: Systematic review and meta-analysis. Lancet 2011, 377, 228–241. [Google Scholar] [CrossRef]
- Horan, T.C.; Gaynes, R.P.; Martone, W.J.; Jarvis, W.R.; Emori, T.G. CDC definitions of nosocomial surgical site infections, 1992: A modification of CDC definitions of surgical wound infections. Infect. Control Hosp. Epidemiol. 1992, 13, 606–608. [Google Scholar] [CrossRef] [PubMed]
- Lewis, S.S.; Moehring, R.W.; Chen, L.F.; Sexton, D.J.; Anderson, D.J. Assessing the relative burden of hospital-acquired infections in a network of community hospitals. Infect. Control Hosp. Epidemiol. 2013, 34, 1229–1230. [Google Scholar] [CrossRef] [PubMed]
- Berríos-Torres, S.I.; Umscheid, C.A.; Bratzler, D.W.; Leas, B.; Stone, E.C.; Kelz, R.R.; Reinke, C.E.; Morgan, S.; Solomkin, J.S.; Mazuski, J.E.; et al. Centers for Disease Control and Prevention Guideline for the Prevention of Surgical Site Infection. JAMA Surg. 2017, 152, 784–791. [Google Scholar] [CrossRef] [PubMed]
- Weiser, T.G.; Haynes, A.B.; Molina, G.; Lipsitz, S.R.; Esquivel, M.M.; Uribe-Leitz, T.; Fu, R.; Azad, T.; Chao, T.E.; Berry, W.R.; et al. Size and distribution of the global volume of surgery in 2012. Bull. World Health Organ. 2016, 94, 201–209f. [Google Scholar] [CrossRef] [PubMed]
- Kamat, U.S.; Fereirra, A.M.A.; Kulkarni, M.S.; Motghare, D.D. A prospective study of surgical site infections in a teaching hospital in Goa. Indian J. Surg. 2008, 70, 120–124. [Google Scholar] [CrossRef] [PubMed]
- Dinda, V.; Gunturu, R.; Kariuki, S.; Hakeem, A.; Raja, A.; Andrew, K. Pattern of pathogens and their sensitivity isolated from surgical site infections at the Aga Khan University Hospital, Nairobi, Kenya. Ethiop. J. Health Sci. 2013, 23, 141–149. [Google Scholar]
- Robson, M.C. Wound infection. A failure of wound healing caused by an imbalance of bacteria. Surg. Clin. N. Am. 1997, 77, 637–650. [Google Scholar] [CrossRef]
- Mangram, A.J.; Horan, T.C.; Pearson, M.L.; Silver, L.C.; Jarvis, W.R. Guideline for Prevention of Surgical Site Infection, 1999. Centers for Disease Control and Prevention (CDC) Hospital Infection Control Practices Advisory Committee. Am. J. Infect. Control 1999, 27, 3–132, 97–132; quiz 3–4; discussion 96. [Google Scholar] [CrossRef]
- Umscheid, C.A.; Mitchell, M.D.; Doshi, J.A.; Agarwal, R.; Williams, K.; Brennan, P.J. Estimating the proportion of healthcare-associated infections that are reasonably preventable and the related mortality and costs. Infect. Control Hosp. Epidemiol. 2011, 32, 101–114. [Google Scholar] [CrossRef] [PubMed]
- Wakeman, D.; Livingston, M.H.; Levatino, E.; Juviler, P.; Gleason, C.; Tesini, B.; Wilson, N.A.; Pegoli, W., Jr.; Arca, M.J. Reduction of surgical site infections in pediatric patients with complicated appendicitis: Utilization of antibiotic stewardship principles and quality improvement methodology. J. Pediatr. Surg. 2022, 57, 63–73. [Google Scholar] [CrossRef] [PubMed]
- AlGamdi, S.S.; Alawi, M.; Bokhari, R.; Bajunaid, K.; Mukhtar, A.; Baeesa, S.S. Risk factors for surgical site infection following spinal surgery in Saudi Arabia: A retrospective case-control study. Medicine 2021, 100, e25567. [Google Scholar] [CrossRef]
- Li, Z.; Li, H.; Lv, P.; Peng, X.; Wu, C.; Ren, J.; Wang, P. Prospective multicenter study on the incidence of surgical site infection after emergency abdominal surgery in China. Sci. Rep. 2021, 11, 7794. [Google Scholar] [CrossRef] [PubMed]
- Brennfleck, F.W.; Bachmeier, T.; Simet, W.; Zeman, F.; Junger, H.H.G.; Schlitt, H.J.; Dahlke, M.H.; Brunner, S.M. Surgical Site Infections and their economic significance in hepatopancreatobiliary surgery: A retrospective incidence, cost, and reimbursement analysis in a German centre of the highest level of care. Int. Wound J. 2021, 18, 17–23. [Google Scholar] [CrossRef] [PubMed]
- Alshammari, L.T.; Alkatheer, S.A.; AlShoaibi, M.B.; Alomran, A.A.; Almulhim, S.N.; Aljindan, R.Y.; Aljehani, Y.M.; Alkharsah, K.R. Surgical site infections in a tertiary hospital over 10 years. The effect of hospital accreditation strategy implementation. Saudi Med. J. 2020, 41, 971–976. [Google Scholar] [CrossRef] [PubMed]
- Rouse, T.; Nascu, P.; Dawson, C.; Morris, E. Incidence of surgical site infections after caesarean sections in a community hospital. Can. J. Infect. Control 2019, 34, 30–34. [Google Scholar] [CrossRef]
- Mekhla, F.R.B. Determinants of superficial surgical site infections in abdominal surgeries at a Rural Teaching Hospital in Central India: A prospective study. J. Fam. Med. Prim. Care 2019, 8, 2258–2263. [Google Scholar]
- Azeze, G.G.; Bizuneh, A.D. Surgical site infection and its associated factors following cesarean section in Ethiopia: A cross-sectional study. BMC Res. Notes 2019, 12, 288. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.; Thompson, D.; Innocent, S.; Narbad, V.; Selway, R.; Barkas, K. Risk factors for surgical site infections in neurosurgery. Ann. R. Coll. Surg. Engl. 2019, 101, 220–225. [Google Scholar] [CrossRef]
- Mirzashahi, B.; Tonkaboni, A.; Chehrassan, M.; Doosti, R.; Kharazifard, M.J. The role of poor oral health in surgical site infection following elective spinal surgery. Musculoskelet. Surg. 2019, 103, 167–171. [Google Scholar] [CrossRef]
- Torres, S.; Perdiz, L.B.; Medeiros, E.A. Incidence of surgical site infection after craniotomy: Comparison between three months and twelve months of epidemiological surveillance. Braz. J. Infect. Dis. Off. Publ. Braz. Soc. Infect. Dis. 2018, 22, 433–437. [Google Scholar] [CrossRef] [PubMed]
- Negi, V.; Pal, S.; Juyal, D.; Sharma, M.K.; Sharma, N. Bacteriological Profile of Surgical Site Infections and Their Antibiogram: A Study From Resource Constrained Rural Setting of Uttarakhand State, India. J. Clin. Diagn. Res. 2015, 9, DC17–DC20. [Google Scholar] [CrossRef] [PubMed]
- Lubega, A.; Joel, B.; Justina, L.N. Incidence and Etiology of Surgical Site Infections among Emergency Postoperative Patients in Mbarara Regional Referral Hospital, South Western Uganda. Surg. Res. Pract. 2017, 2017, 6365172. [Google Scholar] [CrossRef]
- Carvalho, R.L.R.d.; Campos, C.C.; Franco, L.M.d.C.; Rocha, A.D.M.; Ercole, F.F. Incidence and risk factors for surgical site infection in general surgeries. Rev. Lat. Am. Enfermagem. 2017, 25, e2848. [Google Scholar] [CrossRef] [PubMed]
- Pathak, A.; Mahadik, K.; Swami, M.B.; Roy, P.K.; Sharma, M.; Mahadik, V.K.; Lundborg, C.S. Incidence and risk factors for surgical site infections in obstetric and gynecological surgeries from a teaching hospital in rural India. Antimicrob. Resist. Infect. Control 2017, 6, 66. [Google Scholar] [CrossRef]
- Kumar, A.; Thakur, A. Prevalence of surgical site infection in general surgery in a tertiary care centre in India. Int. Surg. J. 2017, 4, 3101–3106. [Google Scholar] [CrossRef]
- Morikane, K.; Honda, H.; Suzuki, S. Factors Associated With Surgical Site Infection Following Gastric Surgery in Japan. Infect. Control Hosp. Epidemiol. 2016, 37, 1167–1172. [Google Scholar] [CrossRef]
- Dessie, W.; Mulugeta, G.; Fentaw, S.; Mihret, A.; Hassen, M.; Abebe, E. Pattern of Bacterial Pathogens and Their Susceptibility Isolated from Surgical Site Infections at Selected Referral Hospitals, Addis Ababa, Ethiopia. Int. J. Microbiol. 2016, 2016, 2418902. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).