Abstract
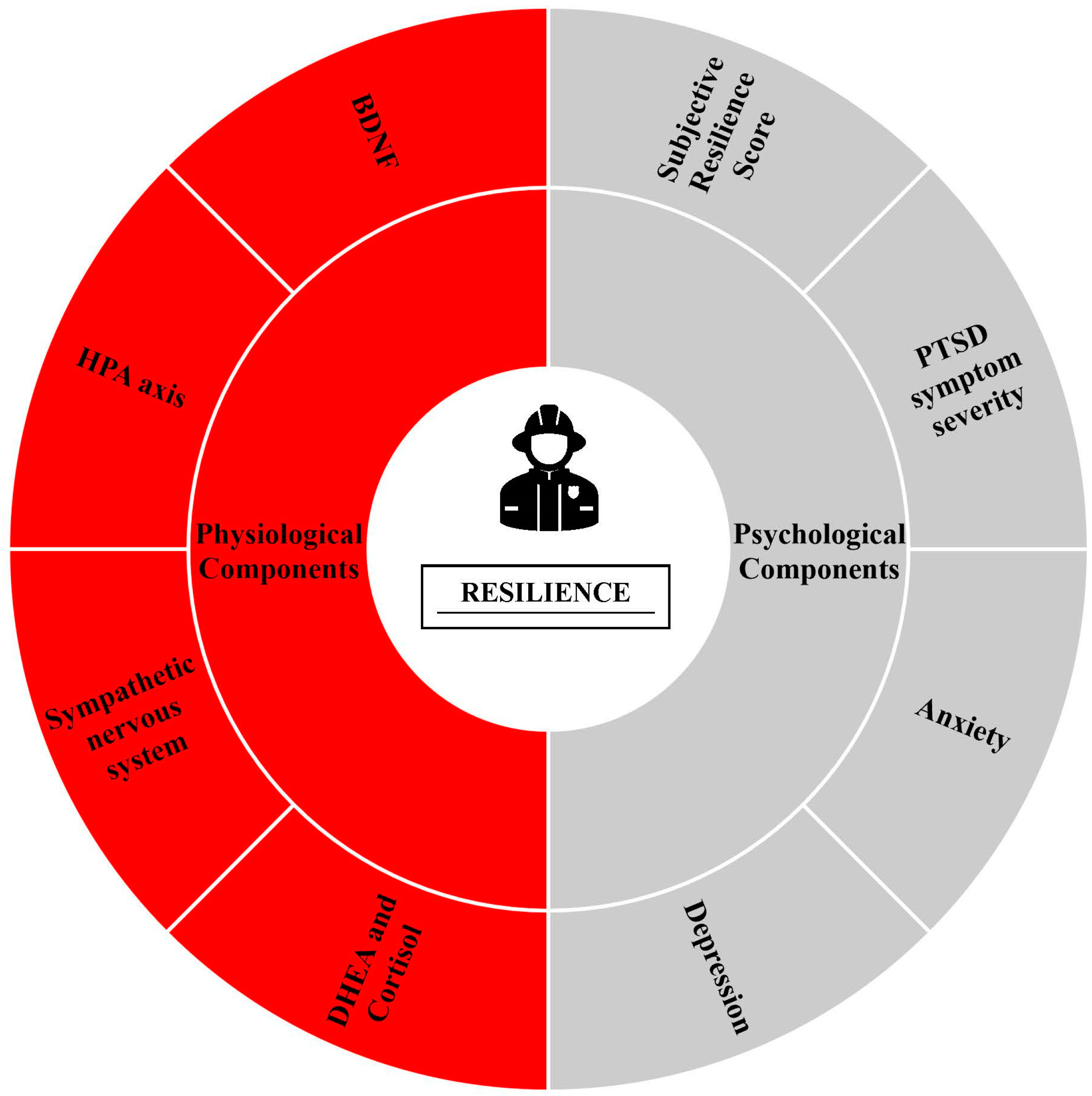
Firefighters are exposed to dangerous and often traumatic events due to the nature of their occupational demands. This repeated exposure to trauma combined with stressful work demands increases their risk for negative physiological and psychological health outcomes. The high prevalence of adverse health outcomes highlights the need for interventions to improve resiliency in firefighters. Resiliency is the ability to reduce the effect of crisis, rebound from adversity, and recover to pre-stimulus homeostasis. When traumatic exposures are unavoidable, as is the case with firefighters, it is important to buffer the resulting consequences on health. While resilience has a genetic component, interventions targeting physiological, psychological, and social components have been successful at improving resilience. These factors are of specific interest as increases in resilience have been linked to improved PTSD symptomology/severity, depression, anxiety, autonomic nervous system activation, hypothalamus–pituitary axis balance, and brain-derived neurotrophic factor. Therefore, the purpose of this review is to identify physiological and psychological components associated with resiliency and discuss strategies that may improve those components to ultimately increase resiliency in firefighters. The strategies discussed include exercise, social support, and mindfulness.
Keywords:
resilience; firefighters; PTSD; mindfulness; exercise; social support; stress; heart rate variability; cortisol; BDNF 1. Introduction
The work life and occupational demands of firefighters are often physiologically and psychologically stressful, dangerous, and traumatic [1]. Work life consists of 24 h work shifts every three days, which dramatically impacts sleep health and, therefore, overall health. The on-duty occupational demands place firefighters at high risk for injury, with death occurring in 80–100 firefighters in the United States yearly. Occupational risks may occur from a combination of demands such as maneuvering through hazardous environments, physical exhaustion from the required workload in addition to wearing heavy, unbreathable full personal protective equipment, mental stress from working to rescue people in need, and cognitive challenges such as quick decision-making to take appropriate steps to safely respond to an emergency [2]. Repetitive exposure to these stressors places firefighters at high risk for longer-term mental health conditions, such as posttraumatic stress disorder (PTSD), and physiological health conditions, such as cancer and cardiovascular disease [3,4].
Firefighters are in a unique position that predisposes them to the development of PTSD. In fact, the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) includes occupational indirect exposure to aversive details of trauma, such as a firefighter would be exposed to when responding to a traumatic call, as one of the four category A criteria [5]. Firefighters are also subject to experiencing the other three criteria in the line of duty: direct exposure, witnessing the trauma, and learning that the trauma happened to a close relative or close friend [2].
Possessing a high level of resilience is essential for firefighters as it increases the likelihood of being able to maintain good health throughout a career that consists of repeated physiological and psychological stress. Resilience is defined in multiple similar statements, which include the following: (1) the ability to withstand, recover, and grow in the face of stressors and changing demands, (2) a psychological coping mechanism that fosters one’s ability to recover from adversity, (3) the ability to maintain a positive adaptation in the face of adversity, and (4) the ability to remain in a biopsychospiritual homeostasis following disruptive and adverse events [6,7,8,9]. Subjective individual reports demonstrate a positive relationship between resiliency and physical, mental, and emotional health [9,10,11]. By nature of their duty, firefighters cannot limit their exposure to traumatic moments; therefore, resiliency is a vital trait to ensure long-term health among firefighters.
Psychological measures associated with resilience are typically assessed with subjective questionnaires. The U.S. Air Force assessed the validity of the Connor-Davidson Resilience Scale (CD-RISC) and demonstrated strong consistency and validity, which lends to the popularity of the CD-RISC as a common resiliency measure [12]. The CD-RISC is a 25-item self-rating 5-point Likert scale with an outcome score of 0 to 100. The questions revolve around components of resilience, such as adaptability, confidence, and fear. Higher scores are associated with greater levels of psychological resilience [9]. Other psychological measures associated with resilience include depression, anxiety, and PTSD symptom severity. Research has demonstrated a negative relationship between resilience and the severity of these mental illness symptoms [13]. The following questionnaires have been found valid and reliable in assessing symptom severity for depression, anxiety, and PTSD: 9-item Patient Health Questionnaire (PHQ-9), 7-item General Anxiety Disorder Screener (GAD-7), and PTSD Checklist (PCL-5), respectively [14,15,16].
Multiple physiological factors have been associated with resilience, including autonomic nervous system function and hypothalamic–pituitary–adrenocortical (HPA) axis activation. The HPA axis, which releases cortisol, and the sympathetic nervous system, which releases epinephrine and norepinephrine, are two primary systems that regulate the body’s response to stressors. In a healthy individual, these systems work to stimulate the body to meet the physiological demands of the stressor via cardiovascular, nervous, and musculoskeletal interactions [17]. For instance, when these systems are activated during times of stress, physiological responses include increased blood pressure, heart rate, cognitive function, breakdown of energy stores, and inflammatory responses from the immune system. Once the stressful situation is over, it is important for the body to end the stress response and return to homeostasis; otherwise, a continued stress response may cause health problems [18]. Heart rate variability and systemic vascular resistance return to baseline are common ways to assess individuals’ ability to return to homeostasis. However, if the body does not return to homeostasis after the stressful situation has ended, a continued release of cortisol and sympathetic activation may promote inflammation and reduced heart rate variability [19]. This overactive and prolonged stress response may leave the immune system weak and defenseless to infections and conditions such as cancer [20].
The adrenal cortex also releases the hormone dehydroepiandrosterone (DHEA) in response to stress exposure to balance the physiological effects of cortisol [19]. DHEA provides anti-inflammatory effects and neuroprotection as it compensates for the effects of cortisol [19,21]. If cortisol release continues, even after exposure to the stressor, the immune system may become suppressed, which is detrimental to health [20]. DHEA may prevent the harmful effects of cortisol [21]. A high DHEA-to-cortisol ratio has been shown to correlate with better performance during stressful military exercises and may reduce the severity of PTSD [22,23]. In addition to DHEA, brain-derived neurotrophic factor (BDNF) may increase resilience to stress as it promotes neural adaptations to environmental demands via synaptic plasticity [23,24,25]. BDNF levels in the hippocampus have been found to be similar to circulating plasma BDNF levels [26]. Like DHEA, BDNF functions to attenuate harmful effects resulting from chronic cortisol release [27]. In depressed individuals, BDNF levels are reduced when exposed to chronic stress [24]. Therefore, circulating DHEA and BDNF are physiological markers related to higher levels of resilience.
Resilience to stress has been associated with normal stress responses that are activated and then terminated shortly after the stressor is over; therefore, those that report higher resilience levels tend to have a higher DHEA-to-cortisol ratio, higher BDNF levels, less resting sympathetic activation, which increases heart rate variability, and lower levels of inflammation. These measures are used as objective biomarkers of resiliency. Subjective measures include questionnaires associated with psychological measures of resilience, including anxiety, depression, and PTSD symptom severity. This review paper seeks to find applicable lifestyle strategies that firefighters can implement to improve resilience. Exercise, mindfulness, and social support were chosen as they have been shown to improve many of the psychological and physiological markers associated with resilience, as shown in Figure 1. By improving these markers, firefighters may be able to better handle the chronic physiological, mental, and emotional stress that they experience as part of their daily occupational demands.
Figure 1.
Physiological and psychological components of resilience in firefighters.
2. Strategies to Improve Components of Resilience
2.1. Exercise
Exercise, physical activity, and physical fitness all play a vital role with respect to an individual’s health. As firefighters are often required to perform physical work, it is important to differentiate between the above terms. Physical activity is the accumulation of all bodily movements performed throughout the day. For firefighters, this includes the physical work required by their occupation. Exercise is a specific type of physical activity in that it is planned and performed to achieve a specific goal (i.e., strength, agility, endurance). Finally, physical fitness is the health and skill-related aspects that permit an individual to achieve movement-related goals [28]. As exercise is designed to improve one or more aspects of physical fitness, it is classified as a physical stressor. According to the World Health Organization, stress is experienced anytime one is subjected to physical, emotional, or psychological strain [29]. During exercise, one is subjecting oneself to physical strain that exceeds the strain one experiences under homeostasis.
As mentioned above, resilience is a combination of aspects associated with overcoming stress, psychological adversity, and disruptive events. As exercise results in the increased production of reactive oxygen species, exercise is a physiological stressor [30]. However, it is important to identify the two main types of stress: distress and eustress. Distress refers to an external stressor that results in potential harm or negative feelings, while eustress is associated with positive feelings brought on by overcoming challenges [31]. Thus, individuals who exercise regularly are constantly exposing themselves to stressful situations and then overcoming that stress. This is known as exposure therapy, which is a common therapy tool used to help individuals overcome their fears associated with PTSD, anxiety, and panic disorders [32]. Hence, it follows that regular exercisers who expose themselves to eustress may demonstrate a natural resistance to increased traumatic occupational stress (i.e., distress). This is of specific interest to first responders who experience occupational stress every working day.
A recent study has highlighted six domains that have a direct impact on resilience in firefighters: physical health, physical fitness, mental health, lifestyle, job-related competencies, and demographic status [33]. Exercise has been well-documented to improve physical health, physical fitness, and mental health. [34,35]. Childs and de Wit (2014) assessed the protective benefits of regular exercise on the stress response to a social stress test [36]. While regular exercisers and non-exercisers reported similar physiological responses (i.e., heart rate, blood pressure, cortisol), non-exercisers exhibited a significantly greater decline in positive affect. Given the impact exercise has on specific domains of resilience, exploring exercise as a potential mechanism to improve resilience seems warranted.
A recent study has highlighted the potential that exercise has for improving measures of resilience. Zhang et al. (2022) conducted a correlational study on physical activity levels, resilience, and negative emotional states [37]. Their results indicate that negative emotional states were negatively correlated with physical activity levels and resilience. Individuals who reported more physical activity exhibited significantly better emotional states relative to those with lower physical activity levels. Additionally, individuals with higher resilience exhibited significantly healthier emotional states relative to those with lower resilience. Further, resilience and physical activity were positively correlated. Thus, individuals who exercise more frequently score higher on resilience measures [37]. While many studies examining exercise and resilience are correlational, numerous animal studies have explored exercise interventions to target resilience. The potential for exercise interventions to improve measures of resilience cannot be overstated, especially as first responders have shown little progress in resilience from pre-incident education. Specifically, a recent review shows no evidence that psychoeducation or pre-employment screening programs help build resilience in first responders [38].
2.1.1. Exercise & Psychological Components of Resilience
Heydari et al. (2021) identified mental health as one of the six domains that directly impact resilience in firefighters [33]. This is not surprising as there has been a significant increase in the number of reported mental illness cases from 2008 to 2018 (i.e., over 7.8 million more reported cases) [39]. While the general population is at risk for developing a mental illness, there is an overwhelming need to explore mental health in high-risk populations. Emergency workers, such as firefighters, are often exposed to life-threatening, traumatic events. The nature of first responders leads to the incidence of high stress, anxiety, depression, and PTSD. It has been reported that over 50 percent of firefighter mortality rates were due to stress and exhaustion [40]. Further, there is a significant body of literature linking firefighters to higher-than-normal levels of stress [41].
As exercise has been well-documented to improve specific domains of mental health, it follows that we should explore exercise as a potential treatment to improve resilience in firefighters. Exercise has been successful in the treatment of anxiety and depression, sleep quality, stress, and symptoms of PTSD [42,43,44,45,46]. While many of the exercise-induced benefits on mental health are moderate, the potential for exercise to moderately improve numerous pillars of mental health cannot be overstated [47]. Further, not only has exercise been successful at reducing symptoms of mental illnesses, but it also functions to protect against mental health relapse [48].
2.1.2. Exercise and Physiological Components of Resilience
During the stress response, the body releases hormones aimed at protecting the body and preparing the body for “fight or flight”. Specifically, the adrenal glands will release cortisol, which will result in elevated heart rate and blood pressure. While this is a normal and healthy response to stress, a prolonged stress response can lead to serious health consequences. Therefore, it is vital to explore mechanisms to reduce the stress response and permit the body to return to homeostasis when the external stressor is removed [20].
The effects of acute exercise on cortisol have been well documented. As exercise is a stressor, individuals respond to exercise with an increase in circulating cortisol. There is evidence that higher-intensity exercise elicits significantly greater levels of salivary and serum cortisol [49]. Additionally, there is evidence that current fitness levels may mitigate cortisol release. Zschucke et al. (2015) had highly trained or sedentary men complete a moderate-intensity treadmill exercise bout [50]. Their results indicated that highly trained men released significantly less cortisol to the same physical stressors as sedentary men. This evidence suggests that an increase in physical fitness/health may help firefighters cope with occupational stress, especially physical occupational stress, by releasing less cortisol.
While there may be some protective benefits following acute exposure to physical stress, many firefighters live with chronic stress. Chronic exposure to stress, whether it be physical, emotional, or mental, can lead to increased resting levels of circulating cortisol. This is often observed in individuals living with PTSD, major depressive disorder (MDD), and/or generalized anxiety disorder (GAD). A recent review and meta-analysis indicated that exercise can significantly reduce cortisol levels in individuals living with MDD [51]. Additionally, chronic exercise has been associated with lower serum cortisol and reduced risk of comorbidities in older populations [52]. Firefighters with increased fitness levels may experience both a decrease in acute cortisol release during stressful events and a reduced resting cortisol level. These protective measures could have significant implications on firefighter’s long-term health.
As mentioned above, DHEA acts to protect the body from excess cortisol by promoting anti-inflammatory effects. Specifically, a high DHEA-to-cortisol ratio is particularly effective at reducing numerous risk factors associated with exposure to stressful events. Regular exercise may significantly improve the DHEA-to-cortisol ratio. Heaney, Carroll, and Phillips (2014) reported that individuals living with higher stress show a significantly greater DHEA-to-cortisol ratio when participating in regular exercise relative to individuals with high stress who do not participate in regular exercise [53]. Additionally, they report that individuals with higher stress severity are at an increased risk for lower DHEA-to-cortisol ratios. Further, Heaney, Carroll, and Phillips (2014) reported a significant increase in DHEA immediately following an acute bout of aerobic exercise [53]. Given the above evidence, both acute and chronic exercise may improve the DHEA-to-cortisol, especially in individuals living with higher stress. As firefighters have been linked to higher-than-usual stress levels, it is logical that exercise would have significant implications on their DHEA-to-cortisol ratios.
Another factor that influences the return to homeostasis following exposure to physical stress is heart rate recovery (HRR). Individuals with abnormal HRR experience an increased risk for all-cause mortality [54]. Exercise interventions have been effective at both improving HRR and decreasing all-cause mortality. Jolly, Brennan, and Cho (2011) classified individuals as having normal HRR or abnormal HRR [55]. Following a 12-week exercise intervention, overall HRR improved, and individuals who went from abnormal to normal HRR demonstrated similar all-cause mortality risk factors to healthy individuals at baseline.
BDNF may also increase resilience to stressful events. One of the mechanisms to increase circulating levels of BDNF is exercise. Szuhany, Bugatti, and Otto (2015) conducted a meta-analysis to determine the effects an acute bout of exercise has on plasma and serum BDNF levels [56]. Their results indicate that exercise has a moderate effect on BDNF levels. While the evidence is limited, chronic aerobic exercise has been shown to reduce resting serum and plasma BDNF [57]. While most studies on exercise and BDNF have been conducted on healthy individuals, Szuhany and Otto (2020) showed similar effects for individuals living with depression [58]. This is of particular interest as firefighters are at an increased risk for numerous mental health conditions. Given the current body of literature on BDNF and exercise, it appears that both healthy and at-risk firefighters will benefit from the exercise-enhanced BDNF changes.
Finally, exercise has been associated with improved HPA axis functioning. The HPA axis is fundamental for the regulation and control of the stress response. During a stressful event, the HPA axis is activated to release adrenocorticotropic hormone (ACTH), which stimulates the release of cortisol. Traustadóttir et al. (2004) accessed changes in ACTH in a group of young, older, and older-fit women [59]. Their results indicate that aging is associated with a decreased functioning of the HPA axis, but regular exercise can temper these changes. Specifically, older-fit women recovered from exercise faster, as indicated by the slope of ACTH, relative to older-unfit women. Chronic exposure to exercise (i.e., eustress) may help the HPA axis both release less ACTH and recover from elevated ACTH levels faster following exposure to a stressful event. This is of particular interest to firefighters who are exposed to occupational stressors often. The faster these individuals can recover from elevated hormone release following adverse events, the better the outcome for their overall health and wellness.
2.1.3. Intervention
When developing an exercise program, multiple variables are incorporated, including frequency (i.e., the number of exercise sessions per week), intensity (i.e., level of energy demand during exercise), duration (i.e., the length of the exercise session), and mode (i.e., the type of exercise being done). However, these variables differ between the interventions utilized in the cited studies of this review that found improvements in components related to resilience. This demonstrates the flexibility in exercise program design as there are many paths to improve physical fitness and overall health. When highly trained individuals were compared to sedentary individuals, the highly trained group demonstrated a lower cortisol response to a stress task; however, both groups showed reduced cortisol responses to the stress task after completing 30 min of moderate-intensity exercise compared with 30 min of no exercise [50]. This study demonstrates two important overall factors when starting to design a program to improve components of resiliency: (1) the primary goal is to transition the individual from sedentary to increasingly more trained over time, and (2) every bout of exercise is important as it acutely reduces the release of the stress hormone, cortisol, in response to stressful situations in both trained and untrained individuals. While this study focused on moderate-intensity aerobic exercise, significant health improvements directly impacting factors of resilience have been shown following resistance exercise [46], various aerobic exercise intensities [47], and circuit training [44].
Ji et al. conducted a randomized, controlled trial that compared three frequencies and two intensities of exercise training for 6 weeks on components of resilience, including anxiety and depression. The frequency groups included two low-frequency (one time per week), two moderate-frequency (two times per week), and two high-frequency (three times per week) groups. The two groups per frequency were then randomized to complete either low-intensity exercise (<59% maximal heart rate) or high-intensity exercise (60–95% maximal heart rate). The exercise sessions were 60 min in duration, including a warm-up and cool-down and consisted of circuit-style training with resistance and aerobic exercises. This study demonstrated that there was a dose-response effect of both exercise intensity and frequency on improvements in anxiety and depression, with intensity having a greater effect [44]. Although other studies demonstrate improvements in components of resilience when exercising at a frequency of three times per week [36], at least an hour per week [53], or following the American College of Sports Medicine guidelines [46,58], these studies did not compare various frequencies and intensities in effectiveness similar to Ji et al. Therefore, when designing an exercise program, it may be beneficial to start with higher intensities (60–95% maximal heart rate) at lower frequencies (one day per week) and progressively increase exercise frequency (three days per week) and duration (60 min). However, as mentioned previously, there is flexibility in exercise programs as long as the program continues to increase overall physical fitness and training status [50].
2.2. Mindfulness
Mindfulness is defined as paying attention in the present moment nonjudgmentally [60]. It is possible to increase attention to the present moment through mindfulness training practices. Example techniques used in mindfulness training programs include guided meditation, body scan exercises, and mindful stretching through yoga [61]. Mindfulness training involves exercising full attention to all forms of sensory experiences in the moment, which then shifts the focus from external to internal stimuli through muscular contraction, breathing, and internal sensations. Mindfulness alters physiological pathways such as hormonal and nervous signaling, which may ultimately improve the resilience of firefighters [62,63]. These physiological alterations that occur during mindfulness training will be discussed and related to components of resilience.
2.2.1. Mindfulness and Psychological Components of Resilience
Mindfulness training has been shown to be a successful tool in improving psychological impairments associated with lower levels of resilience, such as depression, anxiety, stress, and PTSD symptom severity. Subjective questionnaires demonstrate improvements in resilience from mindfulness training. For instance, firefighters and law enforcement showed increased resilience and associated decreased job burnout after going through a Mindfulness-Based Resilience Training intervention [64]. Higher mindfulness scores were also associated with reduced reactivity to daily stress in urban firefighters, including more positive affect and less loneliness on days of increased work and partner stress [65]. Furthermore, specific mindfulness facets including ‘description’ (i.e., labeling and expressing in words our experiences), ‘conscious actions’ (i.e., actions after synthesizing the information from the present moment), and ‘non-reactivity’ (i.e., detaching, accepting, and not reacting to negative thoughts and emotions) were shown to be predictive of resilience in active duty and veteran service members [66].
Mindfulness training has been effective at reducing depression and anxiety symptoms, which are often related to low levels of resilience. An 8-week mindfulness program reduced ruminative thinking, a risk factor for depression, in individuals with mood disorders compared to a group that did not go through the program [67]. College students also demonstrated that mindfulness skills may reduce ruminative thinking, which may alleviate depressive symptoms [68]. To further understand mindfulness-related protection against rumination, Paul et al. (2013) used a magnetic resonance imaging technique to measure neural and behavioral changes during stress-inducing and mindfulness tasks [69]. The study showed that ‘non-reactivity’ is a key facet of mindfulness to protect against rumination and the risk of depression. In addition to the ‘non-reactivity’ facet of mindfulness, the mindfulness facet ‘description’, as defined above, has been found to be beneficial in dealing with negative emotional reactivity to help reduce the risk for depression [70]. In addition to stress and depression, large sample studies have shown mindfulness to be negatively associated with anxiety [71,72]. A randomized control trial including individuals diagnosed with generalized anxiety disorder (GAD) demonstrated significant reductions in subjective anxiety as well as stress reactivity during a stress challenge after participating in an 8-week mindfulness program [72]. Anxiety and stress were also shown to be significantly reduced in female college students after participating in a 3-week mindfulness intervention compared with a group that did not participate [73].
PTSD is common in firefighters and associated with lower levels of resilience, as previously mentioned. Smith et al. assessed urban firefighters for levels of mindfulness, PTSD symptoms, depressive symptoms, and other health symptoms via subjective questionnaires and found that higher levels of mindfulness were associated with fewer PTSD and depressive symptoms in this population [74]. This finding is important as Stanley et al. demonstrated that greater PTSD symptoms are associated with a higher risk of suicide in firefighters; however, certain facets of mindfulness reduced this risk, including ‘conscious actions’ and ‘non-judging of inner experience’ (i.e., empathy for oneself). However, they found a positive association between the mindfulness facet of ‘observation’ (i.e., perceiving the internal and external world around us) and the risk for suicide [75]. The relationship between PTSD symptom severity and pain-related disability in firefighters was found to be moderated by mindfulness; those with higher levels of mindfulness did not show an association between PTSD symptom severity and pain-related disability, whereas those with lower levels of mindfulness did show a significant association between those two variables [76]. According to subjective evaluations of mindfulness, mindfulness is effective at predicting PTSD, job stress, and job burnout in firefighters and, therefore, should be implemented as a training tool to improve these psychological factors that may lead to a healthier life throughout this mentally taxing occupation [77].
2.2.2. Mindfulness and Physiological Components of Resilience
As the mind and the rest of the body are highly connected, mindfulness training also affects many physiological components related to resilience, such as the autonomic nervous system and stress hormones. The sympathetic nervous system, known as the fight or flight system, becomes chronically stimulated in individuals dealing with extreme daily stress, such as those with PTSD [78]. An overactivation of the sympathetic nervous system can lead to cardiovascular strain and risk for cardiovascular disease [79]. Mindfulness training has been shown to reduce daily stress-related sympathetic activation in healthy individuals compared with a control group that did not participate in mindfulness training. Firefighters are also at an increased risk of kidney disease and increased blood pressure due to chronic occupational heat exposure [80]. Park et al. examined mindfulness training in a group of hypertensive men with chronic kidney disease and showed a significant reduction in systolic, diastolic, mean arterial blood pressure, heart rate and muscle sympathetic nerve activity. They suggested that the improved blood pressure was mediated by the reduction in sympathetic activity occurring from the mindfulness training [63].
Physiological markers of stress include the stress hormones cortisol and DHEA and their ratio. These may be examined to objectively identify improvements in stress outside of subjective questionnaires. Studies often use cortisol as a biological marker to validate self-reports of stress [81]. An 8-week mindfulness training program led to decreased morning cortisol levels and improved self-reported sleep for individuals considered novices at mindfulness training [82]. Moreover, a randomized controlled study of nursing students demonstrated decreased serum cortisol levels and perceived stress after receiving five mindfulness training sessions compared with a control group that just sat quietly [83]. DHEA secretion may moderate stress by offsetting the effects of cortisol. A randomized controlled trial in individuals with self-reported stress demonstrated that a 12-week mindfulness training program increased plasma levels of DHEA in the experimental group [84]. Higher levels of mindfulness are associated with a strong negative relationship between DHEA level and subjective physical symptom severity, which suggests that a person’s mindfulness level may predict their perception of their health [85]. A randomized controlled study also examined an 8-week mindfulness training program using a guided body scan versus the control of listening to an audiobook to determine possible alterations in the cortisol/DHEA ratio. The mindfulness training program led to decreased levels of cortisol and cortisol/DHEA ratio with increased levels of DHEA compared to the control group [62].
BDNF, a physiological marker of resilience, has also been shown to benefit from mindfulness training. A systematic review that included randomized controlled trials concluded that mindfulness training using either exercise- or meditation-based interventions resulted in increased peripheral blood BDNF levels [86]. A short period of mindfulness training demonstrated increased serum BDNF levels and decreased oxidative stress compared to controls that simply rested [87]. Similarly, a short period of mindfulness training increased BDNF levels in addition to reducing cortisol and oxidative stress in patients with primary open-angle glaucoma [88]. These studies demonstrate that mindfulness training is useful for improving physiological markers of resilience, such as sympathetic activation and levels of cortisol, DHEA, and BDNF in both healthy and diseased populations.
2.2.3. Intervention
Physiological and psychological benefits result from both acute and long-term mindfulness training. The majority of the cited studies in this review that demonstrate positive effects on components of resilience use an 8-week Mindfulness-Based Stress Reduction (MBSR) course that originated with Kabat-Zinn at the University of Massachusetts Medical Center’s Stress Reduction Clinic [60,64,67,72,84]. The standardized 8-week MBSR course is conducted by a trained specialist and consists of one 2 h course per week, a day-long retreat, and daily homework to listen to a pre-recorded 45 min guided meditation [60]. The practices used in the weekly course included breath-awareness, body-scanning, and gentle Hatha yoga [72]. Variations to fit study populations were used, such as providing strategies to manage stress related to police work in a law enforcement population [64], allowing for self-guided meditation instead of pre-recorded guided meditation for the homework [67], shortening the retreat to half a day [67,72], and shortening the homework to 20 min of meditation [72].
If time and resources allow it, we suggest incorporating the 8-week MBSR course as the mindfulness training strategy for firefighters, as it has been well-researched with controlled trials. For instance, in a three-armed randomized, controlled trial, the MBSR program demonstrated greater increases in plasma levels of DHEAS when compared with the control group, as well as an 8-week locally developed stress reduction program (LSR) that consisted of similar sessions and homework but with a deeper focus on the cognitive-behavioral component with a psychologist [84]. However, if time and resources do not allow for the incorporation of the MBSR course, short and less intensive mindfulness training strategies have been found to be beneficial for improving components of resilience, such as 30 min weekly sessions with a trained meditation specialist [83], listening to a 20 min long pre-recording of a guided body scan for 8 weeks [62], and an 8 h Mindfulness-Based Flow Practice weekend course [87]. Adding in a single, short mindfulness session is better than leaving mindfulness training completely out. For instance, a single 14 min mindfulness session that used a pre-recorded guided mindfulness meditation, which included breathing awareness (i.e., observing their breathing without changing it), body scanning (i.e., perceiving any sensations throughout the body), and self-compassion (i.e., think and repeat positive self-phrases), resulted in acute improvements in blood pressure, sympathetic nerve activity, and respiratory rate compared with 14 min of controlled breathing alone and 14 min of an education session on blood pressure in hypertensive males with chronic kidney disease [63].
2.3. Social Support
Social support is the multi-faceted construct of beneficial resources provided by social relationships that better allow individuals to respond to stress. This support can come from various sources in one’s life, such as family, friends, or colleagues [18,89,90]. This support can be tangible support (e.g., assistance completing a task or providing shelter) or intangible support, such as emotional components (e.g., love and affection [18,89,90]. Of particular importance are one’s perceptions of their available social support. Independent of the quantifiable level of social support that may be represented by the number of family members or coworkers, perceived social support addresses one’s belief that support will be available to them when needed [91].
2.3.1. Social Support and Psychological Components of Resilience
A cross-sectional study found that firefighters with lower perceptions of social support had greater levels of MDD, GAD, and PTSD after experiencing job-related stress [90]. Moreover, the increased risk of suicide among wilderness firefighters, attributed in part to their diminished social connections, highlights the importance of firefighters’ social connections [92]. A longitudinal study evaluated firefighter’s Daily Stress Index and social support [93]. At the conclusion of the study, the Beck Depression Inventory was used to evaluate depression. At the 3- and 6-month follow-up, increased social support buffered the impact of the DSI impact on depressed mood.
Firefighters’ occupation places them not only in harm’s way personally but also exposes them to tragic situations on a regular basis, which increases their risk of developing PTSD. Social support acts as a buffer to protect individuals from developing PTSD. Specifically, higher levels of perceived support compared with lower levels are associated with fewer PTSD symptoms, intrusive rumination, and perception of entrapment in response to the same number of traumatic events [91]. Similarly, the feeling of belonging among firefighters has also shown significant decreases in symptoms of re-experiencing, numbing, hyperarousal, and avoidance [92]. As mentioned, social support can come from a variety of personal relationships. Stanley et al. (2019) investigated what source of support has the strongest association with decreased PTSD symptoms. Three sources were investigated: supervisor, coworker, and family/friends, while PTSD was evaluated using the PCL-5. All three sources showed a significant correlation with decreased overall PTSD severity. Increased supervisor and coworker support also had a significant association with a decrease in all four clusters of PTSD symptoms (i.e., re-experiencing, avoidance, numbing, and hyperarousal) [92]. These results further highlight the benefit of workplace support for firefighters.
2.3.2. Social Support and Physiological Components of Resilience
Social support is not only beneficial to psychological outcomes but physiological ones as well. As explained, chronic stress can lead to maladaptive sympathetic activation, resulting in elevated cortisol, blood pressure, heart rate and a failure to return to homeostasis. While increases in cortisol, heart rate and blood pressure are normal sympathetic system responses to stress, heightened and prolonged elevations can be pathological. In studies where individuals participate in a public speaking or arithmetic task, there is less of an increase in cortisol for participants who perceived that they had support than participants who did not [18].
Another study showed that those with higher perceived social support demonstrated a faster return to baseline in blood pressure and vascular resistance after an arithmetic task. Failure to recover may indicate an overactive sympathetic response and pose a greater risk of developing hypertension [94]. Heart rate variability is used as an indication of vagal influence and has previously been shown to decrease with higher levels of work-related rumination. This suggests that higher rumination disrupts emotional regulation and creates cardiovascular health risks [95]. A study by Gerteis et al. in 2016 explored the protective cardiac effects of social support [96]. In this study, they found that individuals having thoughts of rumination had greater heart rate variability when they perceived their social support to be higher. The proposed mechanism underlying this relationship is the ability of social support to mediate the parasympathetic vagal withdrawal associated with ruminating thoughts [96].
In addition to being cardioprotective, social support is neuroprotective as well. In a study investigating the risk of stroke and social support, participants who had someone available to listen to them had a lower risk of subsequent stroke at follow-up compared with those who did not have someone available. Likewise, the risk of dementia was lower when associated with higher levels of emotional support and the availability of someone to listen. This neuroprotection may be mediated in part by BDNF. Participants who had had higher available social support had higher levels of BDNF, and conversely, those with social isolation had lower levels of BDNF [97].
2.3.3. Intervention
Given that social support is beneficial to firefighters’ development of resiliency, interventions that can increase social support offer fire departments the ability to positively impact firefighters’ health. While all sources of social support are beneficial, support from coworkers and supervisors demonstrates the greatest benefit on mental health outcomes [98,99]. Because workplace support can have such a large impact on the resiliency of firefighters, fire department leadership has a practical opportunity to improve the well-being of firefighters [90,98]. Importantly, leadership should aim to create an environment that welcomes seeking help and speaking about traumatic events while dispelling notions that such behavior will be viewed as a weakness [90,91,98].
We propose implementing critical incident stress debriefing to foster social support and camaraderie. Debriefing provides a space to build community among firefighters by elaborating upon shared experiences [100]. This also offers an opportunity for firefighters to process the event in a supportive environment, further promoting posttraumatic growth [100]. Although the benefits of this practice have been expressed in the literature and used by some professions, it remains underutilized by fire departments across the country. A survey of firefighters found that while firefighters were exposed to trauma regularly, only about half of them participated in debriefing [101]. The firefighters who attended debriefing sessions after stressful incidences displayed greater posttraumatic growth and fewer PTSD symptoms [101]. These positive outcomes from debriefing are attributed largely in part to the increase in social support perceived by firefighters after debriefing [101]. Implementing interventions to increase social support builds resiliency to improve both physiological and psychological health outcomes in firefighters. A summary of suggested exercise, mindfulness, and social support interventions according to the presented literature in this review is included in Table 1.

Table 1.
Summary of suggested interventions to improve components of resilience in firefighters.
3. Conclusions
The life of a firefighter is marked by significant physiological and psychological stressors, including sleep disruption, exposure to hazardous environments, and the constant risk of injury or death. These challenges place firefighters at high risk for both short-term and long-term health conditions, including PTSD, cancer, and cardiovascular disease. Resilience is a critical trait for firefighters to possess to cope with the relentless stress they encounter. Resiliency may be defined as the ability to withstand and adapt to stressors. Exercise, mindfulness, and social support are valuable tools that can create a holistic approach to enhancing firefighters’ ability to withstand the ongoing stress they face. Implementing strategies to bolster these tools can contribute to the well-being and long-term health of firefighters, mitigating the risk of mental and physiologic health conditions associated with their profession.
Author Contributions
Conceptualization, A.M.H.-W.; writing—original draft preparation, A.M.H.-W., B.K.H., D.R.G., and A.A.K.; writing—review and editing, A.M.H.-W., B.K.H., D.R.G., and A.A.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Straud, C.; Henderson, S.N.; Vega, L.; Black, R.; Van Hasselt, V. Resiliency and posttraumatic stress symptoms in firefighter paramedics: The mediating role of depression, anxiety, and sleep. Traumatology 2018, 24, 140. [Google Scholar] [CrossRef]
- Perroni, F.; Guidetti, L.; Cignitti, L.; Baldari, C. Psychophysiological responses of firefighters to emergencies: A review. Open Sports Sci. J. 2014, 7 (Suppl.-1, M3), 8–15. [Google Scholar] [CrossRef]
- Vogt, D.S.; King, D.W.; King, L.A. Risk pathways for PTSD: Making sense of the literature. In Handbook of PTSD: Science and Practice, 2nd ed.; Guilford Press: New York, NY, USA, 2014; pp. 146–165. [Google Scholar]
- Del Ben, K.S.; Scotti, J.R.; Chen, Y.C.; Fortson, B.L. Prevalence of posttraumatic stress disorder symptoms in firefighters. Work Stress 2006, 20, 37–48. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5; American Psychiatric Association: Washington, DC, USA, 2013; Volume 5. [Google Scholar]
- Silverman, M.N.; Deuster, P.A. Biological mechanisms underlying the role of physical fitness in health and resilience. Interface Focus. 2014, 4, 20140040. [Google Scholar] [CrossRef] [PubMed]
- Rutter, M. Psychosocial resilience and protective mechanisms. Am. J. Orthopsychiatry 1987, 57, 316–331. [Google Scholar] [CrossRef]
- Britt, T.W.; Sinclair, R.R.; McFadden, A.C. Introduction: The meaning and importance of military resilience. In Building Psychological Resilience in Military Personnel; American Psychological Association: Washington, DC, USA, 2013; pp. 3–17. [Google Scholar] [CrossRef]
- Connor, K.M.; Davidson, J.R. Development of a new resilience scale: The Connor-Davidson Resilience Scale (CD-RISC). Depress. Anxiety 2003, 18, 76–82. [Google Scholar] [CrossRef] [PubMed]
- Bonanno, G.A. Loss, trauma, and human resilience: Have we underestimated the human capacity to thrive after extremely aversive events? Am. Psychol. 2004, 59, 20–28. [Google Scholar] [CrossRef]
- Hu, T.; Zhang, D.; Wang, J. A meta-analysis of the trait resilience and mental health. Pers. Individ. Differ. 2015, 76, 18–27. [Google Scholar] [CrossRef]
- Bezdjian, S.; Schneider, K.G.; Burchett, D.; Baker, M.T.; Garb, H.N. Resilience in the United States Air Force: Psychometric properties of the Connor-Davidson Resilience Scale (CD-RISC). Psychol. Assess. 2017, 29, 479–485. [Google Scholar] [CrossRef]
- Shrivastava, A.; Desousa, A. Resilience: A psychobiological construct for psychiatric disorders. Indian J. Psychiatry 2016, 58, 38–43. [Google Scholar] [CrossRef]
- Kocalevent, R.D.; Hinz, A.; Brähler, E. Standardization of the depression screener patient health questionnaire (PHQ-9) in the general population. Gen. Hosp. Psychiatry 2013, 35, 551–555. [Google Scholar] [CrossRef] [PubMed]
- Löwe, B.; Decker, O.; Müller, S.; Brähler, E.; Schellberg, D.; Herzog, W.; Herzberg, P.Y. Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Med. Care. 2008, 46, 266–274. [Google Scholar] [CrossRef]
- Weathers, F.W.; Litz, B.T.; Herman, D.S.; Huska, J.A.; Keane, T.M. The PTSD Checklist (PCL): Reliability, Validity, and Diagnostic Utility; Annual Convention of the International Society for Traumatic Stress Studies: San Antonio, TX, USA, 1993; Volume 462. [Google Scholar]
- Sapolsky, R.M. Stress hormones: Good and bad. Neurobiol. Dis. 2000, 7, 540–542. [Google Scholar] [CrossRef]
- Ozbay, F.; Johnson, D.C.; Dimoulas, E.; Morgan, C.A.; Charney, D.; Southwick, S. Social support and resilience to stress: From neurobiology to clinical practice. Psychiatry 2007, 4, 35–40. [Google Scholar] [PubMed]
- Russo, S.J.; Murrough, J.W.; Han, M.H.; Charney, D.S.; Nestler, E.J. Neurobiology of resilience. Nat. Neurosci. 2012, 15, 1475–1484. [Google Scholar] [CrossRef]
- Sapolsky, R.M.; Romero, L.M.; Munck, A.U. How do glucocorticoids influence stress responses? Integrating permissive, suppressive, stimulatory, and preparative actions. Endocr. Rev. 2000, 21, 55–89. [Google Scholar] [CrossRef]
- Charney, D.S. Psychobiological mechanisms of resilience and vulnerability: Implications for successful adaptation to extreme stress. Am. J. Psychiatry 2004, 161, 195–216. [Google Scholar] [CrossRef]
- Rasmusson, A.M.; Vythilingam, M.; Morgan, C.A., 3rd. The neuroendocrinology of posttraumatic stress disorder: New directions. CNS Spectr. 2003, 8, 651–667. [Google Scholar] [CrossRef]
- Ledford, A.K.; Dixon, D.; Luning, C.R.; Martin, B.J.; Miles, P.C.; Beckner, M.; Bennett, D.; Conley, J.; Nindl, B.C. Psychological and Physiological Predictors of Resilience in Navy SEAL Training. Behav. Med. 2020, 46, 290–301. [Google Scholar] [CrossRef]
- Taliaz, D.; Loya, A.; Gersner, R.; Haramati, S.; Chen, A.; Zangen, A. Resilience to chronic stress is mediated by hippocampal brain-derived neurotrophic factor. J. Neurosci. 2011, 31, 4475–4483. [Google Scholar] [CrossRef]
- Linz, R.; Puhlmann, L.M.C.; Apostolakou, F.; Mantzou, E.; Papassotiriou, I.; Chrousos, G.P.; Engert, V.; Singer, T. Acute psychosocial stress increases serum BDNF levels: An antagonistic relation to cortisol but no group differences after mental training. Neuropsychopharmacology 2019, 44, 1797–1804. [Google Scholar] [CrossRef]
- Karatsoreos, I.N.; McEwen, B.S. Psychobiological allostasis: Resistance, resilience and vulnerability. Trends Cogn. Sci. 2011, 15, 576–584. [Google Scholar] [CrossRef]
- Rothman, S.M.; Mattson, M.P. Activity-dependent, stress-responsive BDNF signaling and the quest for optimal brain health and resilience throughout the lifespan. Neuroscience 2013, 239, 228–240. [Google Scholar] [CrossRef] [PubMed]
- Caspersen, C.J.; Powell, K.E.; Christenson, G.M. Physical activity, exercise, and physical fitness: Definitions and distinctions for health-related research. Public. Health Rep. 1985, 100, 126–131. [Google Scholar] [PubMed]
- Fahmy, H.; Tarun, D. Mental Health Atlas 2020; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Powers, S.K.; Deminice, R.; Ozdemir, M.; Yoshihara, T.; Bomkamp, M.P.; Hyatt, H. Exercise-induced oxidative stress: Friend or foe? J. Sport. Health Sci. 2020, 9, 415–425. [Google Scholar] [CrossRef] [PubMed]
- Little, L.M.; Simmons, B.L.; Nelson, D.L. Health among leaders: Positive and negative affect, engagement and burnout, forgiveness and revenge. J. Manag. Stud. 2007, 44, 243–260. [Google Scholar] [CrossRef]
- American Psychological Association. Ethical Principles of Psychologists and Code of Conduct (2002, Amended Effective 1 June 2010, and 1 January 2017). Available online: https://www.apa.org/ethics/code/ (accessed on 30 July 2023).
- Heydari, A.; Ostadtaghizadeh, A.; Khorasani-Zavareh, D.; Ardalan, A.; Ebadi, A.; Mohammadfam, I.; Shafaei, H. Building Resilience in Firefighters: A Systematic Review. Iran. J. Public. Health 2022, 51, 1546–1558. [Google Scholar] [CrossRef] [PubMed]
- Miller, K.R.; McClave, S.A.; Jampolis, M.B.; Hurt, R.T.; Krueger, K.; Landes, S.; Collier, B. The health benefits of exercise and physical activity. Curr. Nutr. Rep. 2016, 5, 204–212. [Google Scholar] [CrossRef]
- Penedo, F.J.; Dahn, J.R. Exercise and well-being: A review of mental and physical health benefits associated with physical activity. Curr. Opin. Psychiatry 2005, 18, 189–193. [Google Scholar] [CrossRef]
- Childs, E.; de Wit, H. Regular exercise is associated with emotional resilience to acute stress in healthy adults. Front. Physiol. 2014, 5, 161. [Google Scholar] [CrossRef]
- Zhang, Z.; Wang, T.; Kuang, J.; Herold, F.; Ludyga, S.; Li, J.; Hall, D.L.; Taylor, A.; Healy, S.; Yeung, A.S.; et al. The roles of exercise tolerance and resilience in the effect of physical activity on emotional states among college students. Int. J. Clin. Health Psychol. 2022, 22, 100312. [Google Scholar] [CrossRef] [PubMed]
- Wild, J.; Greenberg, N.; Moulds, M.L.; Sharp, M.L.; Fear, N.; Harvey, S.; Wessely, S.; Bryant, R.A. Pre-incident Training to Build Resilience in First Responders: Recommendations on What to and What Not to Do. Psychiatry 2020, 83, 128–142. [Google Scholar] [CrossRef]
- SAMHSA; Center for Behavioral Health Statistics and Quality. National Survey on Drug Use and Health, 2008–2018. Available online: https://www.samhsa.gov/data/release/2018-national-survey-drug-use-and-health-nsduh-releases (accessed on 30 July 2023).
- Dowdall-Thomae, C.; Gilkey, J.; Larson, W.; Arend-Hicks, R. Elite firefighter/first responder mindsets and outcome coping efficacy. Int. J. Emerg. Ment. Health 2012, 14, 269–281. [Google Scholar]
- Fraess-Phillips, A.; Wagner, S.; Harris, L.R. Firefighters and traumatic stress: A review. Int. J. Emerg. Serv. 2017, 6, 67–80. [Google Scholar] [CrossRef]
- Carek, P.J.; Laibstain, S.E.; Carek, S.M. Exercise for the treatment of depression and anxiety. Int. J. Psychiatry Med. 2011, 41, 15–28. [Google Scholar] [CrossRef]
- Jayakody, K.; Gunadasa, S.; Hosker, C. Exercise for anxiety disorders: Systematic review. Br. J. Sports Med. 2014, 48, 187–196. [Google Scholar] [CrossRef] [PubMed]
- Ji, C.; Yang, J.; Lin, L.; Chen, S. Physical Exercise Ameliorates Anxiety, Depression and Sleep Quality in College Students: Experimental Evidence from Exercise Intensity and Frequency. Behav. Sci. 2022, 12, 61. [Google Scholar] [CrossRef]
- Gerber, M.; Pühse, U. Review article: Do exercise and fitness protect against stress-induced health complaints? A review of the literature. Scand. J. Public. Health 2009, 37, 801–819. [Google Scholar] [CrossRef]
- Rosenbaum, S.; Sherrington, C.; Tiedemann, A. Exercise augmentation compared with usual care for post-traumatic stress disorder: A randomized controlled trial. Acta Psychiatr. Scand. 2015, 131, 350–359. [Google Scholar] [CrossRef] [PubMed]
- Ensari, I.; Greenlee, T.A.; Motl, R.W.; Petruzzello, S.J. Meta-analysis of acute exercise effects on state anxiety: An update of randomized controlled trials over the past 25 years. Depress. Anxiety 2015, 32, 624–634. [Google Scholar] [CrossRef] [PubMed]
- Babyak, M.; Blumenthal, J.A.; Herman, S.; Khatri, P.; Doraiswamy, M.; Moore, K.; Craighead, W.E.; Baldewicz, T.T.; Krishnan, K.R. Exercise treatment for major depression: Maintenance of therapeutic benefit at 10 months. Psychosom. Med. 2000, 62, 633–638. [Google Scholar] [CrossRef]
- VanBruggen, M.D.; Hackney, A.C.; McMurray, R.G.; Ondrak, K.S. The relationship between serum and salivary cortisol levels in response to different intensities of exercise. Int. J. Sports Physiol. Perform. 2011, 6, 396–407. [Google Scholar] [CrossRef] [PubMed]
- Zschucke, E.; Renneberg, B.; Dimeo, F.; Wüstenberg, T.; Ströhle, A. The stress-buffering effect of acute exercise: Evidence for HPA axis negative feedback. Psychoneuroendocrinology 2015, 51, 414–425. [Google Scholar] [CrossRef] [PubMed]
- Beserra, A.H.N.; Kameda, P.; Deslandes, A.C.; Schuch, F.B.; Laks, J.; Moraes, H.S. Can physical exercise modulate cortisol level in subjects with depression? A systematic review and meta-analysis. Trends Psychiatry Psychother. 2018, 40, 360–368. [Google Scholar] [CrossRef] [PubMed]
- Corazza, D.I.; Sebastião, É.; Pedroso, R.V.; Andreatto, C.; Gomes de Melo Coelho, R.; Gobbi, S.; Teodorov, E.; Ferreira Santos-Galduróz, R. Influence of chronic exercise on serum cortisol levels in older adults. Eurapa 2014, 11, 25–34. [Google Scholar] [CrossRef]
- Heaney, J.L.; Carroll, D.; Phillips, A.C. Physical activity, life events stress, cortisol, and DHEA: Preliminary findings that physical activity may buffer against the negative effects of stress. J. Aging Phys. Act. 2014, 22, 465–473. [Google Scholar] [CrossRef]
- Cole, C.R.; Blackstone, E.H.; Pashkow, F.J.; Snader, C.E.; Lauer, M.S. Heart-rate recovery immediately after exercise as a predictor of mortality. N. Engl. J. Med. 1999, 341, 1351–1357. [Google Scholar] [CrossRef]
- Jolly, M.A.; Brennan, D.M.; Cho, L. Impact of exercise on heart rate recovery. Circulation 2011, 124, 1520–1526. [Google Scholar] [CrossRef]
- Szuhany, K.L.; Bugatti, M.; Otto, M.W. A meta-analytic review of the effects of exercise on brain-derived neurotrophic factor. J. Psychiatr. Res. 2015, 60, 56–64. [Google Scholar] [CrossRef]
- Dinoff, A.; Herrmann, N.; Swardfager, W.; Liu, C.S.; Sherman, C.; Chan, S.; Lanctôt, K.L. The Effect of Exercise Training on Resting Concentrations of Peripheral Brain-Derived Neurotrophic Factor (BDNF): A Meta-Analysis. PLoS ONE 2016, 11, e0163037. [Google Scholar] [CrossRef]
- Szuhany, K.L.; Otto, M.W. Assessing BDNF as a mediator of the effects of exercise on depression. J. Psychiatr. Res. 2020, 123, 114–118. [Google Scholar] [CrossRef]
- Traustadóttir, T.; Bosch, P.R.; Cantu, T.; Matt, K.S. Hypothalamic-pituitary-adrenal axis response and recovery from high-intensity exercise in women: Effects of aging and fitness. J. Clin. Endocrinol. Metab. 2004, 89, 3248–3254. [Google Scholar] [CrossRef]
- Kabat-Zinn, J. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain and Illness; Delacorte: New York, NY, USA, 1990. [Google Scholar]
- Schuman-Olivier, Z.; Trombka, M.; Lovas, D.A.; Brewer, J.A.; Vago, D.R.; Gawande, R.; Dunne, J.P.; Lazar, S.W.; Loucks, E.B.; Fulwiler, C. Mindfulness and Behavior Change. Harv. Rev. Psychiatry 2020, 28, 371–394. [Google Scholar] [CrossRef]
- Schultchen, D.; Messner, M.; Karabatsiakis, A.; Schillings, C.; Pollatos, O. Effects of an 8-week body scan intervention on individually perceived psychological stress and related steroid hormones in hair. Mindfulness 2010, 10, 2532–2543. [Google Scholar] [CrossRef]
- Park, J.; Lyles, R.H.; Bauer-Wu, S. Mindfulness meditation lowers muscle sympathetic nerve activity and blood pressure in African-American males with chronic kidney disease. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2014, 307, R93–R101. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, J.B.; Bergman, A.L.; Christopher, M.; Bowen, S.; Hunsinger, M. Role of resilience in mindfulness training for first responders. Mindfulness 2017, 8, 1373–1380. [Google Scholar] [CrossRef] [PubMed]
- Smith, B.W.; Ford, C.G.; Steffen, L.E. The role of mindfulness in reactivity to daily stress in urban firefighters. Mindfulness 2019, 10, 1603–1614. [Google Scholar] [CrossRef]
- Rice, V.; Boykin, G.; Jeter, A.; Villarreal, J.; Overby, C.; Alfred, P. The relationship between mindfulness and resiliency among active duty service members and military veterans. In Proceedings of the Human. Factors and Ergonomics Society Annual Meeting, San Diego, CA, USA, 1 October 2013; SAGE Publications: Sage, CA, USA; Los Angeles, CA, USA; Volume 57, pp. 1387–1391. [Google Scholar]
- Ramel, W.; Goldin, P.R.; Carmona, P.E.; McQuaid, J.R. The effects of mindfulness meditation on cognitive processes and affect in patients with past depression. Cogn. Ther. Res. 2004, 28, 433–455. [Google Scholar] [CrossRef]
- Barnes, S.M.; Lynn, S.J. Mindfulness skills and depressive symptoms: A longitudinal study. Imagin. Cogn. Pers. 2010, 30, 77–91. [Google Scholar] [CrossRef]
- Paul, N.A.; Stanton, S.J.; Greeson, J.M.; Smoski, M.J.; Wang, L. Psychological and neural mechanisms of trait mindfulness in reducing depression vulnerability. Soc. Cogn. Affect. Neurosci. 2013, 8, 56–64. [Google Scholar] [CrossRef]
- Barnhofer, T.; Duggan, D.S.; Griffith, J.W. Dispositional mindfulness moderates the relation between neuroticism and depressive symptoms. Pers. Individ. Dif. 2011, 51, 958–962. [Google Scholar] [CrossRef]
- Sharma, P.K.; Kumra, R. Relationship between mindfulness, depression, anxiety and stress: Mediating role of self-efficacy. Pers. Individ. Diff. 2022, 186, 111363. [Google Scholar] [CrossRef]
- Hoge, E.A.; Bui, E.; Marques, L.; Metcalf, C.A.; Morris, L.K.; Robinaugh, D.J.; Worthington, J.J.; Pollack, M.H.; Simon, N.M. Randomized controlled trial of mindfulness meditation for generalized anxiety disorder: Effects on anxiety and stress reactivity. J. Clin. Psychiatry 2013, 74, 786–7892. [Google Scholar] [CrossRef] [PubMed]
- Call, D.; Miron, L.; Orcutt, H. Effectiveness of brief mindfulness techniques in reducing symptoms of anxiety and stress. Mindfulness 2014, 5, 658–668. [Google Scholar] [CrossRef]
- Smith, B.W.; Ortiz, J.A.; Steffen, L.E.; Tooley, E.M.; Wiggins, K.T.; Yeater, E.A.; Montoya, J.D.; Bernard, M.L. Mindfulness is associated with fewer PTSD symptoms, depressive symptoms, physical symptoms, and alcohol problems in urban firefighters. J. Consult. Clin. Psychol. 2011, 79, 613–617. [Google Scholar] [CrossRef] [PubMed]
- Stanley, I.H.; Boffa, J.W.; Tran, J.K.; Schmidt, N.B.; Joiner, T.E.; Vujanovic, A.A. Posttraumatic stress disorder symptoms and mindfulness facets in relation to suicide risk among firefighters. J. Clin. Psychol. 2019, 75, 696–709. [Google Scholar] [CrossRef]
- Lebeaut, A.; Zegel, M.; Healy, N.A.; Rogers, A.H.; Buser, S.J.; Vujanovic, A.A. PTSD Symptom Severity, Pain Intensity, and Pain-Related Disability Among Trauma-Exposed Firefighters: The Moderating Role of Mindfulness. Mindfulness 2022, 13, 786–798. [Google Scholar] [CrossRef]
- Golestani, E.; Sadri Damirchi, E.; Jabbari, S. The Role of Mindfulness in Predicting Symptoms of Post-traumatic stress Disorder, Job stress and Job burnout in Tabriz firefighters. Knowl. Res. Appl. Psych. 2021, 22, 174–184. [Google Scholar]
- Lipov, E. Post traumatic stress disorder (PTSD) as an over activation of sympathetic nervous system: An alternative view. J. Trauma. Treat. 2013, 3, 1222. [Google Scholar] [CrossRef]
- Harris, K.F.; Matthews, K.A. Interactions between autonomic nervous system activity and endothelial function: A model for the development of cardiovascular disease. Psychosom. Med. 2004, 66, 153–164. [Google Scholar] [CrossRef] [PubMed]
- Chapman, C.L.; Hess, H.W.; Lucas, R.A.I.; Glaser, J.; Saran, R.; Bragg-Gresham, J.; Wegman, D.H.; Hansson, E.; Minson, C.T.; Schlader, Z.J. Occupational heat exposure and the risk of chronic kidney disease of nontraditional origin in the United States. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2021, 321, R141–R151. [Google Scholar] [CrossRef] [PubMed]
- Matousek, R.H.; Dobkin, P.L.; Pruessner, J. Cortisol as a marker for improvement in mindfulness-based stress reduction. Complement. Ther. Clin. Pract. 2010, 16, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Brand, S.; Holsboer-Trachsler, E.; Naranjo, J.R.; Schmidt, S. Influence of mindfulness practice on cortisol and sleep in long-term and short-term meditators. Neuropsychobiology 2012, 65, 109–118. [Google Scholar] [CrossRef]
- Alhawatmeh, H.N.; Rababa, M.; Alfaqih, M.; Albataineh, R.; Hweidi, I.; Abu Awwad, A. The Benefits of Mindfulness Meditation on Trait Mindfulness, Perceived Stress, Cortisol, and C-Reactive Protein in Nursing Students: A Randomized Controlled Trial. Adv. Med. Educ. Pract. 2022, 13, 47–58. [Google Scholar] [CrossRef] [PubMed]
- Jørgensen, M.A.; Pallesen, K.J.; Fjorback, L.O.; Juul, L. Effect of Mindfulness-Based Stress Reduction on dehydroepiandrosterone-sulfate in adults with self-reported stress. A randomized trial. Clin. Transl. Sci. 2021, 14, 2360–2369. [Google Scholar] [CrossRef] [PubMed]
- O’Loughlin, R.E.; Zuckerman, M. Mindfulness as a moderator of the relationship between dehydroepiandrosterone and reported physical symptoms. Pers. Individ. Diff. 2008, 44, 1193–1202. [Google Scholar] [CrossRef]
- Gomutbutra, P.; Yingchankul, N.; Chattipakorn, N.; Chattipakorn, S.; Srisurapanont, M. The Effect of Mindfulness-Based Intervention on Brain-Derived Neurotrophic Factor (BDNF): A Systematic Review and Meta-Analysis of Controlled Trials. Front. Psychol. 2020, 11, 2209. [Google Scholar] [CrossRef]
- Gomutbutra, P.; Srikamjak, T.; Sapinun, L.; Kunaphanh, S.; Yingchankul, N.; Apaijai, N.; Shinlapawittayatorn, K.; Phuackchantuck, R.; Chattipakorn, N.; Chattipakorn, S. Effect of intensive weekend mindfulness-based intervention on BDNF, mitochondria function, and anxiety. A randomized, crossover clinical trial. Compr. Psychoneuroendocrinol. 2022, 11, 100137, Erratum in Compr. Psychoneuroendocrinol. 2022, 11, 100141. [Google Scholar] [CrossRef] [PubMed]
- Dada, T.; Mittal, D.; Mohanty, K.; Faiq, M.A.; Bhat, M.A.; Yadav, R.K.; Sihota, R.; Sidhu, T.; Velpandian, T.; Kalaivani, M.; et al. Mindfulness Meditation Reduces Intraocular Pressure, Lowers Stress Biomarkers and Modulates Gene Expression in Glaucoma: A Randomized Controlled Trial. J. Glaucoma 2018, 27, 1061–1067. [Google Scholar] [CrossRef]
- Southwick, S.M.; Sippel, L.; Krystal, J.; Charney, D.; Mayes, L.; Pietrzak, R. Why are some individuals more resilient than others: The role of social support. World Psychiatry 2016, 15, 77–79. [Google Scholar] [CrossRef] [PubMed]
- Kshtriya, S.; Kobezak, H.M.; Popok, P.; Lawrence, J.; Lowe, S.R. Social support as a mediator of occupational stressors and mental health outcomes in first responders. J. Community Psychol. 2020, 48, 2252–2263. [Google Scholar] [CrossRef]
- Lee, J.S. Perceived social support functions as a resilience in buffering the impact of trauma exposure on PTSD symptoms via intrusive rumination and entrapment in firefighters. PLoS ONE 2019, 14, e0220454. [Google Scholar] [CrossRef]
- Stanley, I.H.; Hom, M.A.; Gai, A.R.; Joiner, T.E. Wildland firefighters and suicide risk: Examining the role of social disconnectedness. Psychiatry Res. 2018, 266, 269–274. [Google Scholar] [CrossRef] [PubMed]
- Roy, M.P.; Steptoe, A. Daily stressors and social support availability as predictors of depressed mood in male firefighters. Work Stress 1994, 8, 210–219. [Google Scholar] [CrossRef]
- Roy, M.P.; Steptoe, A.; Kirschbaum, C. Life events and social support as moderators of individual differences in cardiovascular and cortisol reactivity. J. Pers. Soc. Psychol. 1998, 75, 1273–1281. [Google Scholar] [CrossRef] [PubMed]
- Cropley, M.; Plans, D.; Morelli, D.; Sütterlin, S.; Inceoglu, I.; Thomas, G.; Chu, C. The Association between Work-Related Rumination and Heart Rate Variability: A Field Study. Front. Hum. Neurosci. 2017, 11, 27. [Google Scholar] [CrossRef]
- Gerteis, A.K.; Schwerdtfeger, A.R. When rumination counts: Perceived social support and heart rate variability in daily life. Psychophysiology 2016, 53, 1034–1043. [Google Scholar] [CrossRef] [PubMed]
- Salinas, J.; Beiser, A.; Himali, J.J.; Satizabal, C.L.; Aparicio, H.J.; Weinstein, G.; Mateen, F.J.; Berkman, L.F.; Rosand, J.; Seshadri, S. Associations between social relationship measures, serum brain-derived neurotrophic factor, and risk of stroke and dementia. Alzheimers Dement. 2017, 3, 229–237. [Google Scholar] [CrossRef]
- Stanley, I.H.; Hom, M.A.; Chu, C.; Dougherty, S.P.; Gallyer, A.J.; Spencer-Thomas, S.; Shelef, L.; Fruchter, E.; Comtois, K.A.; Gutierrez, P.M.; et al. Perceptions of belongingness and social support attenuate PTSD symptom severity among firefighters: A multistudy investigation. Psychol. Serv. 2019, 16, 543–555. [Google Scholar] [CrossRef] [PubMed]
- Setti, I.; Lourel, M.; Argentero, P. The role of affective commitment and perceived social support in protecting emergency workers against burnout and vicarious traumatization. Traumatology 2016, 22, 261–270. [Google Scholar] [CrossRef]
- Donovan, N. Peer support facilitates post-traumatic growth in first responders: A literature review. Trauma 2022, 24, 277–285. [Google Scholar] [CrossRef]
- Sattler, D.N.; Boyd, B.; Kirsch, J. Trauma-exposed firefighters: Relationships among posttraumatic growth, posttraumatic stress, resource availability, coping and critical incident stress debriefing experience. Stress Health 2014, 30, 356–365. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).